Back to Journals » Open Access Emergency Medicine » Volume 14
Orbital Floor Blowout Fracture Reconstruction Using Moldable Polymethyl Methacrylate: A Report of Two Cases and Their Imaging Findings
Authors AlSubaie MF, Al-Sharydah AM , Nassim HM, Alhawsawi A
Received 1 February 2022
Accepted for publication 13 May 2022
Published 25 May 2022 Volume 2022:14 Pages 223—232
DOI https://doi.org/10.2147/OAEM.S359173
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Majed Fehaid AlSubaie,1,2 Abdulaziz Mohammad Al-Sharydah,3 Hala M Nassim,1 Abrar Alhawsawi1
1Department of Ophthalmology, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Khobar City, Eastern Province, Saudi Arabia; 2Department of Ophthalmology, Dhahran-Eye-Specialist-Hospital, Al Jamiah, Dhahran City, Eastern Province, Saudi Arabia; 3Department of Diagnostic and Interventional Radiology, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Khobar City, Eastern Province, Saudi Arabia; 4College of Medicine, Ophthalmology Department, Jeddah University, Jeddah, Saudi Arabia
Correspondence: Majed Fehaid AlSubaie, Department of Ophthalmology, Dhahran-Eye-Specialist-Hospital, Al Jamiah, Dhahran City, Eastern Province, Saudi Arabia, P.O. Box: 31952, Email [email protected]
Background: Blowout fracture is defined as an internal orbital fracture that does not involve the orbital rim. This type of fracture results in the loss of tissue and disruption of the structure of the orbital wall. The symptoms and signs include pain, enophthalmos, diplopia, orbital emphysema, and ecchymosis. The surgeon’s main goal is to reconstruct the orbit in the best possible manner to achieve optimal anatomy and functionality of the orbit wall postoperatively. There is no consensus regarding the best material for use in surgical orbital reconstruction, despite the commercial availability of several biological and manufactured materials. Moreover, material selection is often based on the practitioner’s preferences/experience and patient safety. This study reported two cases of orbital fracture reconstruction using moldable methyl polymethacrylate as a bone surrogate. This material has already been used in dentistry, neurosurgery, and orthopedic surgery and is potentially hazard-free for orbit surgery.
Case Presentation: Two victims of motor vehicle collisions presented with blowout orbital fractures. Cross-sectional imaging revealed inferior fractures involving the orbital wall. High-resolution tomographic modeling was used to plan surgical orbital floor reconstruction using moldable polymethyl methacrylate material. The short-term outcome of the implant appeared favorable at the one-year follow-up, based on regular patient monitoring and cross-sectional imaging assessment. Postoperative improvement with positive clinical outcomes was observed during both patients’ follow-up visits.
Conclusion: Moldable polymethyl methacrylate can be used safely and effectively for reconstructive surgeries for the management of blowout orbital fractures. This new technique ensured a satisfactory short-term postoperative orbital configuration and tolerance and good esthetic and functional results without adverse effects. This customizable product is affordable and easy to fabricate.
Keywords: implant, trauma, oculoplasty, magnetic resonance imaging, computed tomography
Introduction
Blowout fracture (BOF) refers to an internal orbital wall fracture not involving the orbital rim. The hallmarks of BOF are diplopia and enophthalmos, and other presentations include pain, hypesthesia, subcutaneous emphysema, and eyelid ecchymosis.1,2
The management of BOF is challenging for cosmetic surgeons.2,3 The current lack of an ideal implant makes the choice of implant difficult.4
Orbital floor BOF typically results from blunt trauma that pushes the globe posteriorly, causing an increase in the pressure within the orbital chamber.5 Although the diagnosis can be made clinically, cross-sectional imaging, including computed tomography (CT) or magnetic resonance imaging (MRI), should be performed for confirmation, especially in patients with suspected BOF, and is paramount to guiding the management plan.5 Surgical correction is usually performed by repositioning all the herniated tissues into the orbit and placing an implant to avoid tissue movement into the maxillary sinus.5 Numerous materials have reportedly been used for orbital fracture reconstruction, including porous polyethylene, polydioxanone, and autologous calvarial bone grafting.4 The primary aim of surgery is to restore the optimal anatomical and functional structure of the orbit as much as possible.4
Moldable polymethyl methacrylate (PMMA) is an acrylic polymer discovered in the 1930s. It has found wide application in the biomedical field as a bone substitute, spherical implant for evisceration or enucleation, and artificial intraocular lenses, with a comprehensive safety and efficacy profile.6,7
This case series describes the effective use of PMMA for the oculoplastic restoration after BOF for two patients without considerable loss of bony or soft tissues. The patients were successfully treated with single, incident-free, subciliary incision-based orbital reconstruction. Moreover, their cross-sectional imaging characteristics on CT and MRI were also highlighted.
Materials and Methods
Study Setting
The study was conducted at King Fahd Hospital of the University (KFHU), a tertiary-care university teaching hospital with 650 beds, located in the Eastern Province of Saudi Arabia.
Imaging Studies
Image Acquisition
Orbital MRI studies were performed using a 3-T whole-body system (Magnetom Skyra; Siemens Medical Solutions, Erlangen, Germany) with a 20-channel phased-array head coil. Orbital CT studies were acquired using a 128-slice dual-source CT system (Somatom Definition FLASH, Siemens Healthcare, Forchheim, Germany) with a 64-channel multidetector CT scanner.
Image Interpretations
A board-certified diagnostic and interventional radiologist (AS) conducted, reviewed, and reported the imaging studies.
Informed Consent and Follow-Up
Consent was obtained from the patients specifically for the publication of this case series. The patients’ clinical assessment at the mid-term 1-year follow-up revealed adequate orbital volume correction without any migration, extrusion of the implant, or infection. Subjectively, patients were delighted with the postoperative results, and continue to undergo regular follow-up visits to our clinic, without active complaints.
Case Presentation
Clinical Case One
A 27-year-old Saudi man, a victim of an MVC, was referred to the oculoplastic department with complaints of left eye pain, swelling, and diplopia 1 day post-trauma. On examination, visual acuity was normal for both eyes, but left eye emphysema, periorbital ecchymosis, swollen eyelids, and enophthalmos with mild limitation of lid elevation were observed. The other gazes were full. The right eye was unaffected, and the results of other routine ophthalmological examinations were normal, including intraocular pressure, slit-lamp, and dilated fundus examinations.
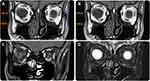
The bone algorithm on non-enhanced CT of the orbit revealed a displaced fracture involving the left lamina papyracea, medial orbital wall, and left inferior orbital wall. The fractures were associated with a small, displaced bone fragment, abnormal superior orientation of the globe, orbital fat herniation, and tethered inferior rectus muscle. Moreover, periorbital swelling/bruising and lacerations of the skin were noted (Figure 1).
Initial management was provided, including cold compression, nasal decongestion, analgesics, and advice to avoid nasal blowing. At the 1-week follow-up, the patient complained of enophthalmos. Surgical intervention was suggested by the surgeon (Table 1), and written informed consent was obtained from the patient after explaining the benefits and risks of the procedure.
 |
Table 1 Proposed Criteria for Surgical Treatment of Orbital Floor Fractures |
Surgery was performed through a subciliary incision. Oculoplasty was performed using the Codman kit (CODMAN: 43–1280), which consists of two complete assemblies of the polymeric powder component, liquid monomer component, and plastic sheath. All procedures were performed according to the manufacturer’s recommendations (Figure 2).
Postoperative MRI scans were used to evaluate the size and shape of the implant (Figure 3).
The patient was followed up at 2 days, 1 week, and 3 months postoperatively to assess the implant, and post-operative complications. The patient showed esthetically and functionally acceptable results at follow-up. After one year, there was no diplopia, complete extraocular motility, and normal findings on Hertel exophthalmometry (22.5, right eye; 22, left eye) (Figure 4).
Clinical Case Two
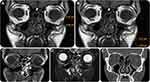
A 28-year-old male victim of an MVC promptly approached our oculoplastic department with complaints of diplopia, periorbital pain, and swelling in the right eye. On examination, the right eye showed limited elevation and diplopia on upward gaze. The patient also experienced numbness above his right cheek. However, full eye movement was possible in all directions. The left eye was unaffected, and further routine eye examinations were unremarkable. CT was performed, which revealed a comminuted fracture involving the floor of the right orbit associated with fat herniation, entrapment of the lower rectal muscle, and swelling of the soft tissues. The optic nerve seemed intact (Figure 5).
As in the first case, conservative management was provided initially, and the surgeon suggested surgical treatment after 1 week, after obtaining written informed consent from the patient. The synthetic materials commonly used in oculoplastic reconstruction are summarized in Table 2.
 |
Table 2 A Summary of Commonly Used Synthetic Materials in Oculoplastic Reconstruction2,3 |
This surgery was also performed through a subciliary incision. Codman cranioplasty was utilized for reconstruction (CODMAN: 43–1280).
Postoperative MRI scans were used to assess the size and shape of the implant (Figure 6).
The follow-up regimen was similar to the first case. The patient’s clinical condition improved over the immediate post-surgical course without the occurrence of adverse events. Similarly, after a year, diplopia was absent, with normal ocular motility, and normal Hertel exophthalmometry findings (17, right eye; 17 left eye) (Figure 7).
Discussion
Numerous types of implant materials reported by previous studies have been used clinically for reconstruction following orbital floor fracture. They can be grouped mainly into organic and fabricated/synthetic materials. Organic materials are classified into auto-graft (eg, bone or cartilage), allograft (eg, Lyophilized Dura Mater, Demineralized Human Bone), or xenograft implants. Fabricated/synthetic materials are classified into absorbable (eg, polymers) or non-absorbable (eg, porous polyethylene, titanium, bioactive glass, silicone, nylon, Teflon, and Seprafilm) implants (Table 2).4,8,9
However, the choice of ideal graft material remains controversial, and depends primarily on the operator’s preference and individual judgment for each patient, to ensure that it elicits good results with fewer complications. The three most commonly used materials for orbital floor reconstruction in clinical practice are autologous calvarial bone graft, porous polyethylene, and polydioxanone.4 Bone graft is still considered the gold standard by several surgeons.4,9
This case report demonstrated the benefits of using moldable PMMA materials, a new type of oculoplastic implant, which can be used safely and effectively to repair orbital floor fractures. To the best of our knowledge, reconstruction of an orbital floor BOF with this material has not previously been reported in literature.
Groth et al reported nine patients with complex orbitofacial defects secondary to trauma, who underwent reconstruction using custom, heat-cured PMMA implants and described the long-term efficacy of using PMMA as a substitute material for implants.10
CRANIOPLASTIC® is an acrylic derivative of PMMA, which is widely used in neurosurgery, dentistry, and orthopedics to replace missing bone.9,11–13 It is commonly used as an orbital sphere implant in anophthalmia to provide more volume to the orbit.14
PMMA is considered an advantageous material in several fields as it does not cause donor-site complications, since it is an immunologically inert synthetic material.4 Allergic reactions to PMMA can occur, albeit rarely.4 Additionally, it offers ease of fabrication (of the implant) and can be shaped according to the size and shape of the bony defect with real-time adjustability; therefore, it can be used for small and large defects, unlike the available absorbable materials that cannot be used in large defects.4 PMMA also does not require any hardware for rigid fixation.4
However, the disadvantages of fabricating large implants using PMMA include time-consuming manipulation.10,15 Besides, the adjacent soft tissues are exposed to the heat of polymerization and residual monomer.16 Once the PMMA resin begins to polymerize and generate heat, these implants must be removed from the molding to prevent deformation and damage to the contour.10,16 However, these issues can be overcome using several techniques, such as performing the fabrication and implantation of PMMA implant procedures separately, including molding of the defect, fabrication of a negative cast from the mold, and implant production using heat polymerization,15 duplication of the original bone flap using a molding technique or as a template for the direct shaping of metal plates. The molding time can be reduced by limiting model fabrication to the defected bone and its proximal structures. The final implant can be modeled intra-operatively within minutes.10,17
The use of intraoperative CT scan during the repair of orbitozygomatic fractures was first reported in 1999.18 Orbital BOF can be identified on MRI with clinically acceptable accuracy.19 Recent investigations by Cooper et al suggest that MRI is comparable to CT for imaging isolated orbital BOF, as evidenced by all BOFs maintaining an average fracture boundary deviation of 1.13 mm or less from the gold standard, CT.19 Another recent cohort study examined the diagnostic accuracy of CT and MRI to assess the integrity of the orbital wall in pathological states. Both modalities were on par with the gold standard; however, imaging assessment of orbital wall integrity leads to a comparably higher number of false-positive findings. In such cases, BOF can be confirmed easily via intraoperative exploration.19 Moreover, pre- and postoperative three-dimensional (3D) cross-sectional imaging has become standard for all patients with craniomaxillofacial trauma. Intraoperative 3D scanning is a relatively recent innovation,18 which is very useful, as correct positioning of implants can be adequately evaluated on 3D imaging.18
Limitations
This study, which reflects recent experiences with a new technique to manage facial fractures with appropriate visual and functional results, has multiple limitations; furthermore, our study is a case series and cannot be used to draw general conclusions. Thus, we recommend further studies with this type of implant, and suggest commercial manufacturing of a moldable PMMA material (CRANIOPLASTIC®) with a roughed surface to decrease the probability of implant movement. The lack of long-term outcomes is also a possible limitation, since it is unknown if the PMMA implant would undergo deterioration (PMMA is susceptible to polymerization shrinkage). The allergenic potential of PMMA is also a limitation. Finally, the operator’s experience is a factor in the manipulation of this material, which would affect the generalizability of the findings.
Conclusion
Subject to the limitations of a small series of two clinical cases, it suffices to conclude that moldable PMMA is a readily available material that can be potentially used to manage BOF in oculoplastic surgeries. It is a customizable material, which can be manipulated effortlessly, that allows for a shorter intraoperative time, small surgical wound, quicker recovery, and greater affordability. However, further studies are needed to investigate and validate its long-term safety and effectiveness. PMMA implants were noted to provide a satisfactory level of orbital configuration and patient tolerance in the short term, while ensuring good cosmetic and functional outcomes with relatively fewer adverse effects.
Abbreviations
MRI, Magnetic resonance imaging; CT, Computed tomography; PMMA, polymethyl methacrylate; BOF, Blowout fracture.
Data Sharing Statement
Not applicable. This is a case review of publicly available information.
Ethics Approval and Informed Consent
The article, in its entirety and detail, does not include disclosing the identity of individuals or information indicating them. It presents two reported cases in a retrospective series of two clinical cases without analysis. This medical/educational report is intended to develop or contribute to generalizable knowledge and does not represent the development, testing, or formulation of a research hypothesis. The article generally does not need to be reviewed by the Imam Abdulrahman Bin Faisal University Institutional Review Board.
Consent for Publication
Consent for publication of the manuscript and related patient information has been obtained by the Ophthalmology Department, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University. Consent for publication of the case details and images has been obtained from both patients.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Cruz AAV, Eichenberger GC. Epidemiology and management of orbital fractures. Curr Opin Ophthalmol. 2004;15(5):416–421. doi:10.1097/01.icu.0000136113.56288.87
2. Felding UNA. Blowout fractures-clinic, imaging and applied anatomy of the orbit. Dan Med J. 2018;65(3):B5459.
3. Jordan DR, Onge PS, Anderson RL, et al. Complications associated with alloplastic implants used in orbital fracture repair. Ophthalmology. 1992;99(10):1600–1608. doi:10.1016/S0161-6420(92)31760-9
4. Avashia YJ, Sastry A, Fan KL, et al. Materials used for reconstruction after orbital floor fracture. J Craniofac Surg. 2012;23(7):S49–S55. doi:10.1097/SCS.0b013e31825aada1
5. Gart MS, Gosain AK. Evidence-based medicine: orbital floor fractures. Plast Reconstr Surg. 2014;134(6):1345–1355. doi:10.1097/PRS.0000000000000719
6. Ali U, Karim KJBA, Buang NA. A review of the properties and applications of poly (methyl methacrylate) (PMMA). Polymer Reviews. 2015;55(4):678–705. doi:10.1080/15583724.2015.1031377
7. Muñoz XM, Bonardi JP, Silva LF, et al. Cranioplasty with poly-methyl methacrylate resin. J Craniofac Surg. 2017;28(1):294–295. doi:10.1097/SCS.0000000000003226
8. Mok D, Lessard L, Cordoba C, Harris PG, Nikolis A. A review of materials currently used in orbital floor reconstruction. Can J Plast Surg. 2004;12(3):134–140. doi:10.1177/229255030401200302
9. Groth MJ, Bhatnagar A, Clearihue WJ, Goldberg RA, Douglas RS. Long-term efficacy of biomodeled polymethyl methacrylate implants for orbitofacial defects. Arch Facial Plast Surg. 2006;8(6):381–389. doi:10.1001/archfaci.8.6.381
10. Unterhofer C, Wipplinger C, Verius M, et al. Reconstruction of large cranial defects with poly-methyl-methacrylate (PMMA) using a rapid prototyping model and a new technique for intraoperative implant modeling. Neurol Neurochir Pol. 2017;51(3):214–220. doi:10.1016/j.pjnns.2017.02.007
11. Rosentritt M, Raab P, Hahnel S, Stöckle M, Preis V. In-vitro performance of CAD/CAM-fabricated implant-supported temporary crowns. Clin Oral Investig. 2017;21(8):2581–2587. doi:10.1007/s00784-017-2057-7
12. Gibon E, Córdova LA, Lu L, et al. The biological response to orthopedic implants for joint replacement. II: polyethylene, ceramics, PMMA, and the foreign body reaction. J Biomed Mater Res B Appl Biomater. 2017;105(6):1685–1691. doi:10.1002/jbm.b.33676
13. Schellini SA, El Dib R, Limongi RM, Mörschbächer R. Anophthalmic socket: choice of orbital implants for reconstruction. Arq Bras Oftalmol. 2015;78:260–263. doi:10.5935/0004-2749.20150068
14. Khoo SC, Nabil S, Nordin R, et al. Intraoperative computed tomography scan for orbital fracture reconstruction. J Craniofac Surg. 2019;30(7):2159–2162. doi:10.1097/SCS.0000000000005667
15. Cooper P, Schechter B, Jacobs G, Rubin R, Wille R. A pre-formed methyl methacrylate cranioplasty. Surg Neurol. 1977;8(3):219–221.
16. Gronet PM, Waskewicz GA, Richardson C. Preformed acrylic cranial implants using fused deposition modeling: a clinical report. J Prosthet Dent. 2003;90(5):429–433. doi:10.1016/j.prosdent.2003.08.023
17. Gliese M, Handel G, Brawanski A. A simple and cosmetically ideal method large cranioplasty. Zentralbl Neurochir. 2000;61(3):155–157. doi:10.1055/s-2000-10999
18. Cooper T, Schmutz B, Hsu E, Lynham A. Magnetic resonance imaging for three-dimensional printing of the bony orbit: is clinical use imminent? Int J Oral Maxillofac Surg. 2020;49(4):483–490. doi:10.1016/j.ijom.2019.07.011
19. Meerwein CM, Pazahr S, Soyka MB, Hüllner MW, Holzmann D. Diagnostic accuracy of computed tomography and magnetic resonance imaging compared to surgical exploration for anterior skull base and medial orbital wall infiltration in advanced sinonasal tumors. Head Neck. 2020;42(8):2002–2012. doi:10.1002/hed.26129
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.