Back to Journals » Clinical Ophthalmology » Volume 16
Open-Label Extension Study Comparing Latanoprost 0.005% Without vs With Benzalkonium Chloride in Open-Angle Glaucoma or Ocular Hypertension
Authors Shen Lee B , Malhotra R, Sall K , Mitchell B, Peace J
Received 24 March 2022
Accepted for publication 30 June 2022
Published 19 July 2022 Volume 2022:16 Pages 2285—2293
DOI https://doi.org/10.2147/OPTH.S367756
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Bridgitte Shen Lee,1 Ranjan Malhotra,2 Kenneth Sall,3 Brittany Mitchell,4 James Peace5
1Vision Optique, Houston, TX, USA; 2Ophthalmology Associates, St. Louis, MO, USA; 3Sall Research Medical Center, Inc., Artesia, CA, USA; 4Medical Affairs North America, Sun Pharmaceutical Industries, Inc., Princeton, NJ, USA; 5Peace Eyecare, Inglewood, CA, USA
Correspondence: Bridgitte Shen Lee, Vision Optique, 5158 Buffalo Speedway, Houston, TX, 77005, USA, Tel +1 713-838-2020, Fax +1 713-838-2030, Email [email protected]
Purpose: To evaluate the long-term safety of latanoprost benzalkonium chloride (BAK)-free vs currently marketed latanoprost 0.005% ophthalmic solution containing BAK (referred to as reference), to treat open-angle glaucoma (OAG) or ocular hypertension (OHT).
Patients and Methods: This phase 3, multicenter, open-label, nonrandomized, single group assignment, safety study included patients who previously completed a phase 3 noninferiority study. Patients self-administered 1 drop of latanoprost BAK-free nightly for 36 weeks in the affected eye(s). Intraocular pressure (IOP), visual acuity (VA), and slit lamp biomicroscopy were assessed predose at baseline and Days 28, 56, 84, 112, 140, and 168; dilated ophthalmoscopy and visual field (VF) at baseline and Day 168. Adverse events (AEs) were recorded throughout the study.
Results: A total of 161 patients who previously received latanoprost BAK-free (n = 80) or reference (n = 81) were enrolled. Latanoprost BAK-free maintained lowered IOP for both the study and nonstudy eye in all patients relative to baseline throughout the study. Clinically significant retinal or optic nerve changes were identified in 5 patients (1 mild-to-moderate change, prior latanoprost BAK-free; 4 mild changes, prior reference). No clinically important changes were identified for VA, slit lamp biomicroscopy, and VF measurements. Ocular AEs occurred in 66 (82.5%) vs 74 (91.4%) patients on prior latanoprost BAK-free and reference, respectively; the most frequent being eye pain (50.0% vs 64.2%) and ocular hyperemia (47.5% vs 54.3%). Most AEs were mild. There were 5 serious systemic AEs in 5 patients (n = 3, prior latanoprost BAK-free; n = 2, prior reference); all were considered unrelated or not likely related to treatment. One patient (prior reference) discontinued due to follicular conjunctivitis. There were no deaths or serious ocular AEs.
Conclusion: Latanoprost BAK-free was well tolerated. These findings support the chronic use of latanoprost BAK-free to treat OAG or OHT.
Clinical Trial Registration Number: NCT00945958.
Keywords: adverse events, intraocular pressure, preservative, prostaglandin, safety, tolerability
Introduction
Glaucoma, a chronic, progressive optic neuropathy, is one of the leading causes of vision impairment and blindness.1,2 Increased intraocular pressure (IOP) is a major risk factor for developing open-angle glaucoma (OAG); therefore, reduction of IOP is an essential part of glaucoma management and can slow disease progression.2 Prostanoid selective prostaglandin F receptor agonists, such as latanoprost, decrease IOP by increasing the outflow of aqueous humor.3 Latanoprost 0.005% ophthalmic solution (Xalatan®, Pfizer Inc., New York, NY, USA) is indicated to reduce elevated IOP in patients with OAG or ocular hypertension (OHT).4 In this original latanoprost formulation, 0.02% benzalkonium chloride (BAK) is used as a preservative.4 However, it has long been recognized that chronic use of preservatives such as BAK has the potential to decrease the stability of the precorneal tear film, resulting in decreased epithelial cell integrity, inflammation, and conjunctival scarring.5 Additionally, benzalkonium salts have moderate sensitizing potential, which can lead to allergies and delayed hypersensitivity reactions.5 All of these potential adverse events (AEs) are of concern for glaucoma patients requiring chronic medical treatment.
Latanoprost 0.005% ophthalmic emulsion without BAK (Xelpros™, Sun Pharmaceutical Industries, Inc., Cranbury, NJ, USA) was approved in 2018 by the US Food and Drug Administration (FDA) for reduction of elevated IOP in patients with OAG or OHT, using potassium sorbate 0.47% as a preservative rather than BAK.6,7 In a phase 3 noninferiority study lasting 12 weeks, latanoprost BAK-free showed IOP reduction similar to that of latanoprost with BAK in patients with OAG or OHT.8 The distribution of AEs was similar between the groups and primarily consisted of ocular events, most commonly eye pain and ocular hyperemia.8 While these results are promising, it is also important to demonstrate that the safety of latanoprost 0.005% BAK-free is maintained beyond the 12 weeks evaluated in the noninferiority study, due to the chronic and progressive nature of glaucoma and the necessity of long-term treatment.
Here, we report the results of the 36-week extension of the phase 3 noninferiority trial (NCT00945958), focused on characterizing the long-term safety of latanoprost 0.005% BAK-free vs the currently marketed latanoprost 0.005% ophthalmic solution containing BAK (referred to as reference) in patients with OAG or OHT.
Materials and Methods
Study Design and Participants
This was a multicenter, open-label, nonrandomized, single group assignment, safety study adhering to the Declaration of Helsinki and the International Council for Harmonisation Consolidated Guideline E6 for Good Clinical Practice, and in accordance with Institutional Review Board (IRB) regulations (US 21 CFR Part 56.103). The study protocol was reviewed and approved by Schulman Associates IRB, Cincinnati, OH, and IRB, St. John’s Hospital, Springfield, MO. All patients provided written informed consent before enrollment.
The study population included patients ≥18 years of age with OHT or primary OAG and unmedicated IOP ≥22 mmHg with ≤5 mmHg intereye difference. Key inclusion criteria included an Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuity (VA) of 1.00 or better and a visual field (VF) defect defined as Humphrey Swedish Interactive Threshold Algorithm (SITA) mean deviation <−20 dB and no central point depression to 0 dB. Key exclusion criteria included central corneal thickness >620 μm or any abnormality preventing stable applanation tonometry, known lack of response to topical ophthalmic prostaglandin analogs, history of allergic hypersensitivity or poor tolerance to study compound components, and intraocular conventional or laser surgery within 6 months of study or refractive surgery in the study eye within 3 months of study. Patients were eligible to enroll in the open-label extension if they participated in the 12-week treatment phase of the phase 3 noninferiority study where they received latanoprost BAK-free or the reference of latanoprost with BAK. To be eligible, patients must have completed the treatment phase of the study without any major protocol violation.
All open-label participants self-administered 1 drop of latanoprost BAK-free once nightly (at approximately 8 PM) for 36 weeks in the affected eye(s). A total of 10 study visits were conducted over 36 weeks: visit 1 (Week 1), visit 2 (Week 4 ± 2 days), visit 3 (Week 8 ± 2 days), visit 4 (Week 12 ± 2 days), visit 5 (Week 16 ± 2 days), visit 6 (Week 20 ± 2 days), visit 7 (end-of-evaluations [EOE] visit, Week 24 ± 2 days), visit 8 (Week 28 ± 2 days), visit 9 (Week 32 ± 2 days), and visit 10 (end-of-study visit, Week 36 ± 2 days). Follow-up continued until the end of the study or until AE resolution, whichever occurred later.
Assessments
No efficacy endpoints were evaluated in this study. Safety assessments including IOP measurement, VA evaluation (best corrected) using an ETDRS chart, slit lamp biomicroscopy, and assessment of conjunctival hyperemia (ORA Redness Scale #6.0b) were completed predose at baseline and on Days 28, 56, 84, 112, 140, and 168. Dilated ophthalmoscopy, corneal endothelial cell count (noncontact specular microscope), VF, and changes in iris and eyelash pigmentation/color and eyelash length, density, and thickness (standardized digital camera) were evaluated at baseline and on Day 168. Vital signs including resting pulse rate and seated blood pressure were measured on Days 1, 28, 56, 84, 112, 140, and 168. Observed AEs were recorded throughout the study, including severity and suspected relationship to study treatment as judged by the investigator. At each study visit, the study medication bottle was weighed before dispensing and after return of the medication to the site to estimate dosing compliance. Patients also used a diary to record whether they had administered their daily evening dose of study medication, and any occurrent AE.
Intraocular pressure was measured in each eye using a Goldmann applanation tonometer at 8 AM, 10 AM, and 4 PM (± 30 minutes) relative to the required time points. Measurements were taken in triplicate at an interval of 1 minute. The mean of the triplicate readings was recorded as the IOP measurement for that time point, with significant mean changes from baseline assessed. LogMAR VA was calculated as follows: LogMAR VA = base logMAR + (N x 0.02), where base logMAR reading was the last line in which at least one letter was read correctly by the patient and N was the total number of letters missed up to and including the last line read. The number and percentage of patients with no change, loss or gain of 1 line, loss or gain of 2 lines, and loss or gain of >2 lines from baseline were analyzed. Clinically, a decrease in VA of ≥2 LogMAR lines (0.1 = 1 LogMAR line) from baseline was reported as an AE. Slit lamp biomicroscopy evaluated the lid and lid margin, conjunctiva, cornea, iris, anterior chamber, lens, and vitreous. The cornea, anterior chamber, and lens were rated on a 3-point scale ranging from 0 to 2 units (0 = absence of any pathology, 1 = evidence of previously active pathology now quiet and/or structural change now stable, or 2 = evidence of active pathology or active structural change). Any clinically significant increase of one or more units from baseline was reported as an AE. A 4-point scale ranging from 0 to 3 units was used to assess conjunctival hyperemia (0 = none, 1 = mild, 2 = moderate, or 3 = severe). A clinically significant change from baseline was defined as an increase of one or more units from the maximum hyperemia score recorded at any time point after baseline; an AE was reported for any clinically significant increase. For dilated ophthalmoscopy, changes to the retina, macula, choroid, optic nerve, and optic disc pallor were examined and rated by severity category (none, mild, moderate, or severe). A clinically significant increase of one or more units from baseline was reported as an AE; cup-to-disc ratio was also recorded. Visual field was measured using Humphrey field analyzer 24-2/30-2 threshold tests (SITA standard), and VF reliability was established at ≤33% fixation loss. Iris color was classified according to a color scheme ranging from 1 (blue/grey) to 10 (brown [Asian]). Any change in pigmentation grade in the iris and eyelashes at the time of withdrawal from study treatment was compared with baseline, verified from photographs, and graded as none, weak, moderate, marked, or no information. Eyelashes were also graded in this way for change in color, length, density, or thickness. Any confirmed iris pigmentation change from baseline was reported as an AE. Systolic blood pressure, diastolic blood pressure, and pulse rate values and any changes from baseline were monitored.
Statistical Analysis
The enrollment goal for this open-label extension was to have a sufficient number of patients to obtain safety data from ≥100 patients for 36 weeks. The safety population included all patients who enrolled and received ≥1 dose of study medication. Statistical programming and analyses were performed using SAS Version 9.2. Descriptive statistics (n, mean, standard deviation, median, maximum, minimum, 95% confidence intervals) were provided for continuous variables. Numbers and percentages were provided for categorical variables. Change from baseline was derived for vital signs and ophthalmic parameters (IOP, VA, slit lamp biomicroscopy, conjunctival hyperemia, dilated ophthalmoscopy, and iris and eyelash evaluations) for the study eye and nonstudy eye. For patients who received latanoprost BAK-free in the phase 3 study, their baseline measurements were the baseline measurements for the phase 3 study (prior to receiving the first dose of latanoprost BAK-free). Baseline measurements for patients who received reference phase 3 treatment were the measurements taken on Day 1 of the current study (end-of-study visit for the phase 3 study).
Results
Patients
A total of 161 patients completed the phase 3 treatment phase and were enrolled in the extension; 80 had received prior latanoprost BAK-free and 81 received prior reference (Figure 1). All patients were included in the safety analysis population. Patient demographics and baseline characteristics are summarized in Table 1, showing that the groups who had received latanoprost BAK-free and reference were similar, with the most notable difference in the proportions of Caucasian patients (67.5% and 75.3%, respectively).
 |
Table 1 Patient Demographics and Baseline Characteristics |
 |
Figure 1 Patient disposition. Abbreviation: BAK, benzalkonium chloride. Notes: aThese patients withdrew consent at the end-of-evaluations visit (visit 7). |
During the trial, 86 (53%) patients discontinued the study, with the majority (n = 71) withdrawing their consent at EOE visit 7 (after which there were no additional assessments other than AE monitoring). Of the enrolled patients, 149 received at least 24 weeks of latanoprost BAK-free treatment having completed EOE visit 7, which met the FDA’s recommendation of providing safety data for at least 100 patients for ≥6 months.
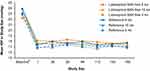
Ophthalmic Examinations and Additional Analyses
Treatment with latanoprost BAK-free maintained reductions in IOP for all patients throughout the study, for both the study eye (Figure 2) and the nonstudy eye. In the study eye for the prior latanoprost BAK-free group, mean IOP before any phase 3 treatment was approximately 22–24 mmHg, compared to approximately 17–18 mmHg at the extension trial EOE visit. For the prior reference group, mean IOP was approximately 16–17 mmHg at baseline (Day 1 of the extension trial) and 16–18 mmHg at the EOE visit.
The number of patients with clinically significant changes in severity of conjunctival hyperemia was small and remained relatively constant in the study (for the study eye, it ranged from 12 to 17 in the latanoprost BAK-free group and from 5 to 14 in the prior reference group). For retinal assessments, 5 clinically significant changes in severity related to the retina or optic nerve at the EOE visit were identified: 1 mild-to-moderate change in the latanoprost BAK-free group and 4 mild changes in the prior reference group. Eyelash density AEs (all of mild severity) increased in a small number of patients from baseline to EOE visit (from 3 to 9 in the latanoprost BAK-free group and from 6 to 12 in the prior reference group). Eyelash length also increased in a small number of patients in the prior reference group (from 9 with mild severity at baseline to 12 with mild severity and 1 with moderate severity at the EOE visit) but not in the latanoprost BAK-free group (the number of patients with mild severity remained the same [n = 8]). For eyelash thickness, 2 patients in the prior reference group had mild eyelash thickness at baseline, increasing to 6 patients at the EOE visit; in the prior latanoprost BAK-free group, 4 patients had mild eyelash thickness at baseline, decreasing to 3 patients at the EOE visit.
For systolic blood pressure, 20 patients in the prior reference group and 19 in the prior latanoprost BAK-free group had potentially clinically significant values at the EOE visit. There were no potentially clinically significant findings for any patients for diastolic blood pressure or resting pulse.
No important findings were identified for the other safety measures, including VA, eye lid and margin, cornea, anterior chamber, lens, cup disc ratio, VF, iris, and corneal endothelial cell count parameters.
Treatment-Emergent Adverse Events
A total of 1720 treatment-emergent AEs (TEAEs) were reported among 143 (88.8%) patients. Of these, 893 TEAEs occurred in the prior latanoprost BAK-free group and 827 in the prior reference group.
A total of 1640 ocular TEAEs were reported among 140 patients (Tables 2 and 3), of which 1390 (85%) were mild in severity, 216 (13%) were moderate, and 34 (2%) were severe. The incidence of most ocular TEAEs was similar between the prior latanoprost BAK-free and reference groups (Table 3). However, more ocular TEAEs judged as severe by the investigator were identified in the prior reference group, including those that were both severe and treatment-related (Table 2). One patient in the reference group discontinued the trial due to an ocular AE of follicular conjunctivitis.
 |
Table 2 Treatment-Emergent Adverse Events |
 |
Table 3 Ocular Treatment-Emergent Adverse Events ≥5% in at Least One Group |
A total of 80 systemic TEAEs were reported by 42 patients (26.1%), with a similar distribution based on prior treatment (Table 2). Infections and infestations were the most frequently reported systemic TEAEs, with 23 TEAEs reported by 19 patients; 12 patients reported TEAEs in the prior latanoprost BAK-free group and 7 in the reference group. Specific systemic AEs with an incidence >2% were influenza (2.5%) and nausea (2.5%) in the reference group, and VF defect (3.9%), tooth infection (2.5%), and peripheral edema (2.5%) in the latanoprost BAK-free group. There were no ocular serious AEs reported, and 5 serious systemic AEs were reported: orchitis, carotid artery stenosis, and syncope in the latanoprost BAK-free group and tension headache and peripheral vascular disorder in the reference group (Table 2). All serious systemic AEs were considered to be unrelated or unlikely to be related to study treatment and all resolved without sequelae with no deaths reported during the study.
Discussion
This extension trial was conducted to investigate the long-term safety of latanoprost BAK-free ophthalmic solution when administered once daily in an adult population with OAG or OHT, evaluating both safety and tolerability. The most frequently reported ocular TEAE was eye pain. Many of the less frequently reported ocular TEAEs were generally similar between the prior treatment groups and/or occurred in small numbers. No serious ophthalmic AEs were reported, and none of the serious systemic AEs were considered likely to be related to study drug treatment. Regarding IOP, latanoprost BAK-free treatment maintained reductions in IOP for all patients throughout the study. Few notable safety findings were identified during ophthalmic exams or additional analyses. The number of at least potentially clinically significant changes in severity was small, and these occurred for a small number of safety/ophthalmic parameters, with no safety concerns identified.
The current findings are consistent with other recent publications that collectively support the safety, tolerability, and high rates of patient satisfaction and self-reported quality of life with BAK-free latanoprost formulations, including preservative-free formulations.8–15 Results of the 12-week primary phase 3 study comparing latanoprost 0.005% without vs with BAK in OAG or OHT, which enrolled 578 patients, demonstrated that substantial reductions from baseline in IOP were maintained for the duration of the study in the latanoprost BAK-free group.8 TEAEs were mostly mild with comparable incidence between treatment groups, and no significant safety concerns were found for ocular TEAEs (eye pain, ocular and conjunctival hyperemia, VA, eye lid and margin, cornea, anterior chamber, eye pruritus, VF, and iris and eyelash changes) in patients receiving BAK-free latanoprost.8 A post hoc pooled analysis of 3 randomized controlled clinical trials and 2 international real-world evidence observational studies including 3610 total patients, which compared patient tolerance and efficacy of preservative-free and preservative-containing latanoprost formulations, found that patients receiving preservative-free latanoprost had reductions in conjunctival hyperemia and ocular surface disease composite score as compared with patients receiving latanoprost with preservatives.15 Similar reductions from baseline in IOP were found for both formulations. In the open-label RELIEF study of 140 adults with glaucoma or OHT who had stable IOP after ≥3 months of latanoprost with BAK monotherapy and switched to preservative-free latanoprost, IOP-lowering efficacy was maintained over the 90-day study.13 Based on both objective and subjective measures, the RELIEF study found that the preservative-free formulation was associated with statistically significant reductions in conjunctival hyperemia, as well as improvements in blepharitis, tear breakup time, corneal and conjunctival epithelial fluorescein staining, and patient-rated assessments of tolerability.13 Topical AEs were limited to single reports of mild-to-moderate stinging, foreign body sensation, palpebral edema, and increased dry eye sensation. No serious AEs or treatment-related systemic AEs were reported.13 While glaucoma requires chronic treatment, the 36-week extension trial results reported here are noteworthy; it should also be noted that patients who previously completed the latanoprost BAK-free arm in the phase 3 noninferiority study received this treatment for a total of 48 weeks.
Limitations of this extension study include the relatively small patient population, as well as the lack of assessment of perceptions of patient satisfaction and patient-reported quality of life. Future studies may enroll larger numbers of patients, as well as incorporate patient-reported measures to allow comparison of subjective tolerability between treatment groups.
Conclusions
Long-term administration of latanoprost BAK-free appears to be safe and well tolerated. These findings support the long-term use of latanoprost BAK-free as treatment for primary OAG or OHT.
Abbreviations
AE, adverse event; BAK, benzalkonium chloride; EOE, end-of-evaluations; ETDRS, Early Treatment Diabetic Retinopathy Study; FDA, Food and Drug Administration; IOP, intraocular pressure; IRB, Institutional Review Board; MedDRA, Medical Dictionary for Regulatory Activities; OAG, open-angle glaucoma; OHT, ocular hypertension; SITA, Swedish Interactive Testing Algorithm; TEAE, treatment-emergent adverse event; VA, visual acuity; VF, visual field.
Data Sharing Statement
Data and other documents will be made available after publication, with no end date, to anyone who submits a reasonable request to the study sponsor. Contact information for the study sponsor can be found at www.SunPharma.com/USA.
Ethics Statement
Written informed consent was obtained from all patients prior to study initiation. This study was conducted in accordance with the ethical guidelines of the latest revision of the Declaration of Helsinki, and in accordance with Institutional Review Board (IRB) regulations (US 21 CFR Part 56.103). The study protocol was reviewed and approved by Schulman Associates IRB, Cincinnati, OH, and IRB, St. John’s Hospital, Springfield, MO.
Acknowledgments
Sun Pharma Advanced Research Company, Ltd., participated in the design, conduct, monitoring, data collection, data management, and data analysis of the study. Writing and editorial support were provided by Jennifer Masucci, VMD, of AlphaBioCom, LLC, and were funded by Sun Pharmaceutical Industries, Inc.
Author Contributions
All authors have made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or all of these areas. All authors have critically reviewed and agreed on all versions of the article before submission. All authors have agreed on the journal to which the article will be submitted and agree to take responsibility and be accountable for the contents of the article.
Funding
This study was sponsored and funded by Sun Pharma Advanced Research Company, Ltd.
Disclosure
BSL reports consultant fees from Lumenis, MacuHealth, and Santen Pharmaceutical Co., Ltd; research fees from Johnson & Johnson Vision, Kala Pharmaceuticals, and SightGlass; and speaker fees from Lumenis, RVL Pharmaceuticals, and Sun Pharmaceutical Industries, Inc. RM reports consultant fees from Abbott Laboratories, Alcon, Allergan, Bausch & Lomb, BioD, InSite Vision, Katena Products, Nicox, OASIS Medical, Shire, and TearScience; and speaker and other fees from Abbott Laboratories, Alcon, Allergan, Bausch & Lomb, BioD, InSite Vision, Katena Products, Nicox, OASIS Medical, Shire, and TearScience. KS reports consultant fees from Cloudbreak; Kala Pharmaceuticals; and Sun Pharmaceuticals Industries, Inc.; and personal fees from Allysta Pharmaceuticals; Betaliq; Cloudbreak; Glaukos; Inotek Pharma; Kala Pharmaceuticals; Kowa; La Roche; Novaliq; Ocular Therapeutix; Santen Pharmaceutical Co., Ltd; Sun Pharmaceutical Industries, Inc.; Tearsolutions; Topcon; and Valeant. BM is an employee of Sun Pharmaceutical Industries, Inc. The authors report no other conflicts of interest in this work.
References
1. Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221–e1234. doi:10.1016/s2214-109x(17)30393-5
2. Prum BE, Rosenberg LF, Gedde SJ, et al. Primary open-angle glaucoma Preferred Practice Pattern® guidelines. Ophthalmology. 2016;123(1):P41–P111. doi:10.1016/j.ophtha.2015.10.053
3. Winkler NS, Fautsch MP. Effects of prostaglandin analogues on aqueous humor outflow pathways. J Ocul Pharmacol Ther. 2014;30(2–3):102–109. doi:10.1089/jop.2013.0179
4. Xalatan (latanoprost ophthalmic solution) 0.005% full prescribing information. Pfizer Inc.; 2014.
5. Pisella PJ, Pouliquen P, Baudouin C. Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. Br J Ophthalmol. 2002;86:418–423. doi:10.1136/bjo.86.4.418
6. Xelpros (latanoprost ophthalmic emulsion) 0.005% full prescribing information. Sun Pharmaceutical Industries, Inc.; 2020.
7. Xelpros (latanoprost ophthalmic emulsion) 0.005% NDA approval letter; 2018.
8. Wirta D, Malhotra R, Peace J, et al. Noninferiority study comparing latanoprost 0.005% without versus with benzalkonium chloride in open-angle glaucoma or ocular hypertension. Eye Contact Lens. 2021. Publish ahead of print. doi:10.1097/icl.0000000000000860
9. Aptel F, Pfeiffer N, Schmickler S, et al. Noninferiority of preservative-free versus BAK-preserved latanoprost-timolol fixed combination eye drops in patients with open-angle glaucoma or ocular hypertension. J Glaucoma. 2019;28(6):498–506. doi:10.1097/IJG.0000000000001248
10. Economou MA, Laukeland HK, Grabska-Liberek I, Rouland JF. Better tolerance of preservative-free latanoprost compared to preserved glaucoma eye drops: the 12-month real-life FREE study. Clin Ophthalmol. 2018;12:2399–2407. doi:10.2147/OPTH.S176605
11. Hollo G, Katsanos A, Boboridis KG, Irkec M, Konstas AGP. Preservative-free prostaglandin analogs and prostaglandin/timolol fixed combinations in the treatment of glaucoma: efficacy, safety and potential advantages. Drugs. 2018;78(1):39–64. doi:10.1007/s40265-017-0843-9
12. Lopes NLV, Gracitelli CPB, Chalita MR, Faria NVL. Ocular surface evaluation after the substitution of benzalkonium chloride preserved prostaglandin eye drops by a preservative-free prostaglandin analogue. Med Hypothesis Discov Innov Ophthalmol. 2019;8(1):52–56.
13. Misiuk-Hojlo M, Pomorska M, Mulak M, et al. The RELIEF study: tolerability and efficacy of preservative-free latanoprost in the treatment of glaucoma or ocular hypertension. Eur J Ophthalmol. 2019;29(2):210–215. doi:10.1177/1120672118785280
14. Munoz Negrete FJ, Lemij HG, Erb C. Switching to preservative-free latanoprost: impact on tolerability and patient satisfaction. Clin Ophthalmol. 2017;11:557–566. doi:10.2147/OPTH.S126042
15. Harasymowycz P, Hutnik C, Rouland JF, et al. Preserved versus preservative-free latanoprost for the treatment of glaucoma and ocular hypertension: a post hoc pooled analysis. Adv Ther. 2021;38(6):3019–3031. doi:10.1007/s12325-021-01731-9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.