Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Nutrition and Non-Nutrition-Related Challenges Predict Time to Death in Long-Term Care Residents: A Retrospective Chart Review
Authors Morrison-Koechl J , Liu SH, Banerjee A, Heckman G, Keller H
Received 25 April 2023
Accepted for publication 8 August 2023
Published 20 September 2023 Volume 2023:16 Pages 2823—2837
DOI https://doi.org/10.2147/JMDH.S417344
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jill Morrison-Koechl,1 Sheng Han Liu,1 Albert Banerjee,2 George Heckman,3,4 Heather Keller1,4
1Department of Kinesiology & Health Sciences, University of Waterloo, Waterloo, Ontario, Canada; 2Department of Gerontology, St. Thomas University, Fredericton, New Brunswick, Canada; 3Schlegel-UW Research Institute for Aging, Waterloo, Ontario, Canada; 4School of Public Health Sciences, University of Waterloo, Waterloo, Ontario, Canada
Correspondence: Jill Morrison-Koechl, Department of Kinesiology & Health Sciences, University of Waterloo, 200 University Ave W, Waterloo, Ontario, N2L 3G1, Canada, Email [email protected]
Purpose: Signals of end-of-life decline observed in daily habits, such as mealtime participation, are important for moving towards comfort-focused goals of care in the final months of life of long-term care (LTC) residents. It is unclear how eating issues observed in real-time in LTC homes are used as indicators of suspected end of life. The study quantifies nutrition and key non-nutrition related signals (eg, general decline, unstable vitals) documented to describe end-of-life decline and the subsequent time to death.
Patients and Methods: A retrospective chart review identified the first documented conversation where end-of-life decline was considered by members of the care team (eg, nurses, physicians, dietitian, family member) for 76 randomly selected decedents from 9 LTC homes in southwestern Ontario, Canada. Time (days) to death was calculated. A directed content analysis of the free-text description of the suspected end-of-life decline was used to categorize signals. Cox proportional hazards regression analysis tested the risk of mortality associated with each categorized signal.
Results: Time to death of residents (mean age = 88 ± 7 years; 60% female) from the first documentation of potential end-of-life decline ranged from 0 days to over 2 years prior to death (median = 27.5 days). Seven nutrition-related and 18 non-nutrition related signals were identified. Swallowing difficulty (HR = 2.99; 95% CI = 1.41, 6.33), cognitive decline (HR = 0.40; 95% CI = 0.20, 0.77), delirium (HR = 13.23; 95% CI = 1.57, 111.69), and cancer (HR = 0.18; 95% CI = 0.07, 0.48) were associated with time to death.
Conclusion: This study provides insight into the signals used by care providers in LTC to suspect that residents are declining towards the end of life and identifies four signals that were associated with time to death. When identified by care providers as indicators of end-of-life decline, swallowing difficulty and delirium predicted a shorter time to death, while cancer and cognitive decline predicted a longer time to death. Recognition of nutrition and non-nutrition related signals may be leveraged to systematically introduce timely comfort care conversations.
Plain Language Summary: This study is part of a larger project exploring the experience of older adults living in residential long-term care (LTC) facilities around nutrition-related challenges (eg, refusing to eat, weight loss) in the final months of life. It is well known that residents experience more complex nutrition-related challenges with proximity to the end of life and that such challenges are associated with increased risk of death. Furthermore, LTC staff rely on observable signals, including nutrition-related challenges, to indicate that residents in their care are experiencing end-of-life decline and to reorient goals of care to emphasize comfort. As such, we carried out this study to identify how common nutrition-related challenges observed in residents may be leveraged to introduce comfort conversations between LTC staff, residents, and their family caregivers. To accomplish this, we performed an in-depth review of resident charts of 76 deceased LTC residents. In our review, we identified the point at which the LTC staff first noted a decline in the residents’ health that potentially indicated end-of-life decline. We took detailed notes of the circumstances surrounding the suspected decline and categorized the reasons given. Our study describes these documented reasons (ie, ‘signals’), which included seven nutrition-related challenges, only one of which (ie, swallowing difficulty) was associated with shorter time to death. From these findings, we can conclude that goals of care should be reassessed when LTC residents experience swallowing difficulty, while the other identified signals (eg, food refusal) may prompt LTC staff to initiate comfort-focused conversations despite uncertain imminence of death.
Keywords: time to death, dysphagia, delirium, LTC
Introduction
Residents of long-term care (LTC) in Canada represent some of the oldest and frailest members of society, with many complex health, cognitive, and functional impairments that increase the risk of mortality. The LTC population is characterized by a high level of cognitive impairment affecting at least 90% of residents,1 and approximately 75% of residents have three or more comorbidities, including cardiovascular disorders and diabetes among other conditions.2 Multimorbidity contributes to an increased risk of functional decline which, combined with age-associated sarcopenia and frailty, leads to increased vulnerability to complications such as pain, delirium, weakness, and dysphagia (ie, swallowing difficulty).3,4 Given the high prevalence of frailty in the LTC population, with estimates ranging up to 75% of residents internationally,5,6 these complications are also common among residents of LTC. Evidence suggests that LTC residents experience a high prevalence of dysphagia and swallowing difficulties, with estimates ranging from 7% to 40% according to one systematic review.7 Further compounding these vulnerabilities, cognitive impairment, multimorbidity, frailty, and their associated challenges hinder adequate food intake and increase the risk of malnutrition,7–9 which is estimated to affect over half of LTC residents10 and contributes to an increased risk of mortality.11
As a result of such complex physical and functional challenges, many residents live their final months and days of life in the LTC home.12,13 An estimated 25% of residents in Ontario LTC homes die within one year of admission14 and approximately 20% of admitted residents are discharged due to death each year, according to publicly reported Canadian data.15 Given the high rate of mortality, the demand for comfort-focused approaches to care in LTC is growing.16–18 Such approaches become increasingly important as residents experience changes in health, function, and cognitive status that increase the complexity of care needs and severity of their conditions. Yet, very few decedents in Canadian LTC homes receive specialist palliative care.19,20 Integrated palliative (ie, comfort-focused) approaches to care, though undergoing rapid development in the Canadian LTC landscape, are still limited by many challenges.18
Early initiation of comfort care practices has been demonstrated to decrease burdensome interventions and improve quality of life of persons living with dementia and other life-limiting conditions, and to decrease costs associated with accessing acute care services.17,19,21 Imminent or obvious end-of-life decline should not be a prerequisite for initiating comfort approaches to care. However, commonly cited barriers to implementing early comfort-focused care such as complexity of symptoms, unclear prognosis, and variable condition-related trajectories towards end-of-life22–27 indicate that care providers do look for signs or signals of decline before initiating goals of care conversations. While previous theory suggests that end-of-life trajectories differ by diagnostic category (ie, cancer, organ failure, and frailty/dementia),28,29 these categories have not been useful in distinguishing end-of-life decline among older adults living in residential and LTC facilities,22,30 likely due to the complexity of health conditions and functional changes found among residents in these settings. As such, alternative opportunities for introducing comfort-focused goals of care are needed.
Signals of end-of-life decline that are observable in daily habits and routines of LTC residents have been identified and regarded as fundamental to initiating high-quality palliative end-of-life care.25,31–33 A Swedish study of multidisciplinary healthcare professionals working in LTC found that early signals were subtle, and although not immediately obvious, could be identified with some reflection from care staff.31 Another study had Dutch nursing home physicians list signs and symptoms that would indicate a life expectancy of 6 weeks or less; little/no fluid and food intake, generalized weakness, and respiratory problems were most commonly reported as the top symptoms.25 Categorization of observed and recorded signs and symptoms that lead to suspected end-of-life decline, from a care provider perspective, has not been done to confirm these findings. The timing of such signals in relation to death may also inform strategies for initiating earlier comfort-focused care conversations.
Eating challenges are common in LTC residents and become more prominent in many residents in the final months of life.34 Most prognostic tools used to indicate the risk of 6-month mortality include at least one item such as malnutrition, weight loss, and/or reduced food intake,17,35 highlighting the relevance of eating challenges as a signal of terminal decline. In addition to the use of prognostic tools, daily observations of residents’ changing habits and behaviors surrounding food and fluid may be useful to initiate conversations and to support the decision to transition towards end-of-life care goals. Decreased food/fluid intake, refusal to eat, and dysphagia have been cited by healthcare providers to signal terminal decline in practice,25,31,33 yet it is not known if these challenges predict time to death. Studies of signals of end-of-life decline have been qualitative31–33 or do not consider timing to death after the signs are recognized.25 It is unclear how eating issues observed in real-time in LTC homes, from the viewpoint of the care provider, are used as indicators of suspected end of life.
This study is exploratory and aims to better understand the transition to end-of-life care goals for LTC residents from a multidisciplinary perspective with a particular focus on nutrition-related signals. To meet these objectives, a retrospective chart review was used to identify the point at which care providers first documented potential end-of-life decline and the factors surrounding this event.36,37 A retrospective chart review was advantageous for this purpose because it allowed for efficient collection of data on deceased residents and an unbiased account of the care providers’ perspective of the important signals that led them to consider that the resident was experiencing end-of-life decline. The study is led by two objectives: 1) to describe the nutrition-related and other (ie, non-nutrition) challenges that led care providers to suspect the end-of-life phase was starting for residents and 2) to investigate whether any of the identified challenges, when flagged to indicate potential end-of-life decline, consistently predicted a shorter or longer time to death.
Materials and Methods
This investigation is one part of a larger study designed to explore the role of eating-related challenges and nutrition care practices within the context of the end-of-life experience of long-term care (LTC) residents.34
Study Sample
The sample was comprised of deceased residents from LTC homes affiliated with a single for-profit chain in southern Ontario, Canada. Participants were selected after death so there was no researcher influence on the anticipation of end-of-life decline. Of 19 homes in the chain, 9 were randomly selected for participation. Residents were eligible for inclusion if they had been admitted to one of these 9 homes for at least 6 months to ensure adequate health record history and had a death date falling between December 1, 2018 and March 11, 2020. These dates ensured availability of electronic records, which were implemented chain-wide in the year prior, and excluded deaths that occurred after the World Health Organization (WHO) declaration of the COVID-19 pandemic on March 11, 2020, given the significant impact of the emergency order on the care provided in the LTC sector. Ten residents from each home were randomly selected using a random number generator. Residents under the age of 65 years (n = 5) were removed retroactively, so the sample consisted of 85 residents who were over the age of 65 and had been admitted to their respective home for at least 6 months. Individuals who did not have a change of status indicative of end-of-life decline documented in their progress notes prior to death (n = 9) were excluded from this study. Thus, the final sample consisted of 76 participants.
Data Collection
Data for the study were collected by a single researcher (JMK) through a retrospective chart review using medical record review methodology (Supplement 1).36–39 The resident charts were documented electronically in PointClickCare© (Mississauga, ON, 2020), a cloud-based health record software, and accessed remotely using a virtual private network (VPN). Data on nutrition-related eating challenges and care interventions, focusing on the last 6 months of life, were extracted from the participants’ clinical progress notes, assessments, and care plans by a single researcher using a data extraction form with detailed definitions for each item. Extracted data were recorded electronically using REDCap Software, a secure web platform for building and managing online databases.40,41 Only the first author (JMK) had access to the resident charts for data extraction, and all data were de-identified by name and LTC home upon extraction to protect resident privacy. Deidentified datasets and associated documents were stored on an encrypted, password-protected network drive hosted by the University of Waterloo in accordance with data protection regulations. Ethics approval for the study was obtained from the Office of Research Ethics at the University of Waterloo (ORE#40789) and subjected to an additional approval process according to institutional policies within the LTC home chain.
Resident characteristics for sample description were obtained from the resident admission forms, progress notes, and the Resident Assessment Instrument Minimum Data Set 2.0 (MDS 2.0), a standardized instrument that assesses the health and functional status of residents, reported quarterly by trained staff in LTC homes across Ontario.15,42 To align with the goals of the larger study, the MDS 2.0 assessment recorded approximately 6 months prior to death was extracted. Extracted items included: diagnoses; leaving >25% of food uneaten at most meals (yes vs no); moderate/severe cognitive impairment (Cognitive Performance Scale [CPS] ≥3 vs <3);43 moderate/high health instability (CHESS ≥3 vs <3);44 extensive/total dependence on Activities of Daily Living Self Performance Hierarchy Scale (ADL ≥3 vs <3);45 probable depression (Depression Risk Scale [DRS] ≥3 vs <3);46 any responsive behaviors (Aggressive Behavior Scale [ABS] ≥1 vs 0);47 and daily vs less than daily pain.48 One item indicating existing swallowing problems was also extracted from the MDS 2.0 assessment recorded approximately six months prior to death. The residents’ progress notes from the final month of life were scanned for swallowing difficulty reported by the LTC care team.
The event of interest was the point at which the care providers reported a “change in status” that signaled suspected end-of-life decline, including a guarded prognosis, transition to comfort-focused care, or direct anticipation of death. This event was identified primarily by a keyword search, described in further detail below. Since the aim of this study was to retrospectively understand the resident nutrition and non-nutrition challenges that led the care team to suspect end-of-life decline, the search was first limited to progress notes documented in the 6 months prior to death. If a change in status event was not obvious in the last 6 months of the resident’s life, or if the care goals expressed in the progress notes within 6 months of death suggested that the change in status had already occurred (eg, comfort-focused care goals were already established), earlier progress notes (ie, prior to 6 months before death) were reviewed to identify the point at which a significant change in status was first noted, if at all. Change in status was identified by first reviewing the progress notes informally to get a sense of the resident’s trajectory towards death. This initial chart scan was followed by a keyword search of the charted progress notes. Search terms included “end-of-life”, “terminal”, “deteriorate”, “comfort”, and derivatives and synonyms of these words (eg, “end of life” and EOL were also searched), to identify the earliest mention of the change in residents’ status. A description of the steps used to identify the change of status, including the list of search terms, can be found in Supplement 2 (Table 2.1).
The date of the change in status reported by healthcare providers was noted. Contextual details around the documented change in status were extracted as a free-text description, preserving the original wording of the progress notes as much as possible. Details of interest included the role of the person who initiated the conversation (eg, nursing staff, physician, family member), the reasons for flagging the change in status, and the context around the conversation (eg, arising from a planned care conference, recent hospitalization). Progress notes in the days leading up to the change in status reporting were summarized where necessary to gain more context, for example, if the progress note referred to an event occurring on a previous day. The date of initiation of formalized palliative/end-of-life orders (ie, ordered by physician or entered into the care plan) was also noted for descriptive purposes.
Intra-rater reliability of the entire data extraction (293 items), including the date of first mention of a change in status, was done in duplicate for 15 randomly selected resident charts (~10% of the total sample for the larger study, n = 176) (Supplement 1). Agreement on the change of status date was found for 13 (87%) of the 15 charts, indicating an acceptable level of reliability. One of the disagreements referred to the same event but was one day off. In the other case of disagreement, two different dates were recorded in the variable field, but both dates with similar text descriptions were noted both times the chart was reviewed.
Dependent Variable
The outcome of interest was “time to death”, measured as the number of days from the date on which the change in status was reported in the resident’s progress notes to the date of death.
Independent Variables
The independent variables of interest were the signs and symptoms (“signals”) reported at the same time as the healthcare provider reported the change in the resident’s status. A directed content analysis, consisting of three steps, was performed to convert the free-text description of the change in status progress note into quantitative data points.49 First, authors (JMK and HK) developed preliminary codes for these signals based on a priori knowledge, existing literature, and a brief scan of the contents of the documented texts. JMK and SL then independently coded the progress note extracts using the preliminary list of signals. Once all resident extracts had been independently coded, JMK and SL compared their codes for each resident, discussed discrepancies, and refined the definition of each code until a consensus was reached between JMK and SL for all resident files. HK reviewed the final list of codes and definitions for appropriateness. The final list of codes included 7 nutrition-related and 18 non-nutrition signals (Supplementary Table 2.2).
Analysis
Chi-square, Fisher’s exact, t-tests and Mann–Whitney U-tests were used to compare the demographic (ie, age, sex, length of admission, hospital death) and functional characteristics (ie, MDS 2.0 scores, diagnoses, history of swallowing problems, swallowing difficulty reported in the final month of life) between included and excluded individuals. Descriptive statistics of the change in status event, including the frequency of each signal and other contextual details, were provided. The distribution of the time to death following the change in status in this sample was highly right-skewed, so in addition to mean time to death, survival time was described using quartile estimates (ie, the number of days at which 25%, 50%, and 75% of residents were expected to have died) and 95% confidence intervals using a log–log transformation. Formalized end-of-life orders were also described, similarly including mean number of days to death and quartile estimates of survival time.
Bivariate tests of equality (ie, Log rank test) compared the homogeneity of survival curves (ie, Kaplan–Meier estimate) for each signal.50 Cox proportional hazards regression analysis with backward elimination, removing all variables that had a p-value >0.05, identified which signals were associated with time to death. Model fit statistics (−2Log L, AIC, and SBC) were compared during model-building to identify the final model; lower values for each of these three scores indicated better model fit so were preferred.
Results
The study sample consisted of LTC decedents who had a documented change in status that suggested end-of-life decline (n = 76) while those without a documented change in status were excluded (n = 9) (Table 1). Participants had a mean age of 88 ± 7 years at the time of death, were 60% female, had been admitted to the LTC home for a median of 37 [Q1, Q3: 24, 59] months. A high proportion of participants (83%) had moderate/severe cognitive impairment. Nearly half (49%) of participants had a history of leaving food uneaten and more than one-fifth (22%) had a history of swallowing problems according to the MDS 2.0 assessment completed approximately 6 months prior to death. The sample had a high level of complex comorbidities, including cancer (20%), diabetes (25%), hypothyroid disorder (22%), cardiovascular disorders (78%), arthritis (37%), and stroke (25%). Multimorbidity was highly prevalent in this sample, with 88.2% (n = 67) of participants having three or more diagnoses. In the final month of life, 59% of residents exhibited signs of swallowing difficulty as reported by LTC care providers in the progress notes. The sample demographics were not significantly different from the excluded group, except for the proportion who died in the hospital (9% of included vs 56% of excluded; p < 0.001), proportion who exhibited responsive behaviors (58% of included vs 22% of excluded; p = 0.04), and report of swallowing difficulty in the final month of life (59% included vs 11% excluded; p=0.01).
 |
Table 1 Sample Descriptives with Comparison of Residents Who Had an End-of-Life Discussion Documented to Those Who Did Not |
The time to death following the documented change in status was highly variable, ranging from 0 days to over 2 years, and skewed with 53% of conversations documented within the last month of life (Table 2). The change in status was documented within the context of a planned care conference for nearly 20% (n = 15) of participants. These participants had a longer time to death (median = 84 days) as compared to individuals for whom the change in status was noted based on routine care (median = 21 days), though this difference was not statistically significant (p = 0.25). Nursing staff (41%) were the most common group to first document the change in status of residents. The dietitian first flagged a change in status in 7% of participants. In 15% of cases, family members initiated the end-of-life discussions by raising concerns about the resident’s health or opting out of life-prolonging treatments such as dialysis. A formalized palliative/end-of-life order was initiated for 80% of participants, the majority of which occurred in the last 2 weeks of life.
 |
Table 2 Description of the First Reporting of a Possible End-of-Life Decline, n=76 |
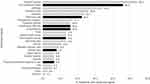
Twenty-five signals of end-of-life decline were coded from the contextual details of the documented change in status. The most common nutrition-related signal supporting the consideration of end-of-life decline was low food/fluid intake (46%) (Figure 1). Swallowing difficulty was cited as a reason for suspecting end-of-life decline for 12 individuals (13% of the sample). Of these 12 individuals, 50% had an indication of swallowing problems at least 6 months prior to death. Furthermore, these 12 individuals accounted for slightly more than one quarter (27%) of the 45 residents who had swallowing difficulty reported in their progress notes in the final month of life. The most common non-nutrition signal was general (ie, non-specific) decline in health (54%) (Figure 1). Three quarters of residents had at least one nutrition-related challenge cited, and multiple signs/symptoms were commonly cited to signal a change in status (Supplementary Table 2.3). Bivariate survival curves were significantly different for cognitive decline, cancer, and delirium, although it must be noted that only one individual was flagged with delirium as an indicator of end-of-life decline in this sample (Table 3).
 |
Table 3 Bivariate Comparison of the Homogeneity of Survival Curves When Each Sign/Symptom Was Observed versus Not Observeda, n=76 |
The final Cox proportional hazards model with removal of nonsignificant signals is provided in Table 4. Only one nutrition-related signal was retained; swallowing difficulty documented as a signal of decline was a significant predictor of time to death. Individuals for whom swallowing difficulty was cited as a reason for considering end-of-life decline were more likely to die sooner (hazard ratio [HR] = 2.99, 95% confidence interval [CI] = 1.41, 6.33) compared to those for whom it was not cited, when adjusting for other significant signals. Cognitive decline and new or existing cancer diagnosis, when cited as reasons for the change in status, were associated with a longer time to death (HR <1). Delirium was associated with shorter time to death; the model fit (−2LogL and AIC) was improved when delirium was included in the model despite only having one participant with this signal. The total number of nutrition-related signals and total signals overall were tested in the model but neither was significantly associated with time to death.
 |
Table 4 Cox Proportional Hazards Regression Analysis to Test the Associations Between Observed Signs/Symptoms and Mortality, n=76 |
Discussion
This exploratory retrospective study of deceased LTC resident charts identified both nutrition- and non-nutrition-related signs and symptoms reported by care providers to indicate potential end-of-life decline. The identified signals are consistent with other qualitative studies31,32 and make a novel contribution by quantifying the prevalence and time to death of these signals in a random sample of LTC participants from a home chain in Ontario, Canada. These findings contribute to a better understanding of the changes in residents’ health and routines that indicate to care providers in current practice that a transition in goals of care may be necessary and stimulates discussion around how these signals could serve as targets for initiating comfort-focused end-of-life conversations.
The findings of this study suggest that prognostication of LTC residents is difficult and a change in approach for managing end-of-life decline that does not rely on anticipated timelines is needed. Typical of the broader LTC population, a high proportion of the participants in this sample had significant cognitive impairment, loss of independence, and multiple diagnoses representing a highly frail population with complex health and functional needs. Given the complexity of this population, it is not surprising that a variety of signals were noted by care providers to indicate that residents were nearing death, but that very few of these signals were associated with time to death. General decline was the most often cited reason for indicating end-of-life decline, consistent with a previous study that highlighted how care providers in LTC had difficulty specifying early signs of decline but described it as residents “going into a bubble”, citing subtle changes in daily routines as non-specific indicators that residents were moving toward the end of life.31 Low food/fluid intake was also noted for nearly 50% of residents as a signal of end-of-life decline indicating that care providers acknowledge decreased intake as a sign of decline, consistent with other studies.25,31 Realistically, a number of factors including residents’ signs and symptoms and care providers’ knowledge and attitudes affect the decision to initiate end-of-life care conversations and are highly context dependent.31,51 The signs and symptoms identified in this study may be used as markers to indicate the need for goals of care conversations within the specific context of individual residents.
Regarding timing to death, though some signals were identified to be associated with shorter or longer time to death, findings indicate that these factors are also context dependent. The longer time between the initial documentation of potential end-of-life decline and death when cancer and cognitive impairment were noted is potentially explained by the known association between these chronic and life-limiting conditions and mortality,52,53 which may have increased the acceptability of earlier initiation of end-of-life care conversations. However, only 16% of the sample had accelerated cognitive decline documented as a signal of end-of-life decline, whereas 83% presented with moderate or severe cognitive impairment at 6 months prior to death indicating that changes in cognition are not consistently used as an indicator of end-of-life decline for LTC residents. Likewise, cancer was identified as a signal of end-of-life decline in 10% of cases, but 20% had a diagnosis of cancer in the sample. It is more likely that complications, concerns, or provider-specific perspectives associated with these conditions prompted earlier end-of-life conversations. Alternatively, swallowing difficulty and delirium, when noted as a signal of end-of-life decline, were associated with a shorter time to death. As highlighted previously, adversities such as dysphagia and delirium are complications of multimorbidity and resulting frailty,3,4 and are both independently associated with mortality.8,54 As such, both of these conditions may be rightly viewed as late signals of end-of-life decline in LTC residents because they are indicators of severe cognitive and physical dysregulation or impairment in an already frail and vulnerable population. However, this interpretation is limited in the current study because of a lack of context. For example, whereas 16% of residents were noted to have swallowing difficulty as a signal of end-of-life decline, nearly 60% of the total sample displayed signs of impaired swallowing in the last month of life. It could be that some residents had sudden onset of swallowing difficulty or their symptoms were more severe when noted to indicate end-of-life decline. Further context is needed to determine how care providers attribute various signals as indicators of end-of-life decline among LTC residents.
The initial conversations prompted by change of status of LTC residents most often occurred within 3 months of death with timing skewed towards the date of death. Identification of the change of status relied on multiple signs and symptoms and was context dependent, reinforcing previously noted challenges with identifying the appropriate timing of comfort-focused care initiation in response to end-of-life decline among older adults with complex needs.23,29 Regular assessments of residents' health and changing needs with the support of established prognostic tools are important for adjusting goals of care and anticipating end-of-life decline, as evidenced by the longer (albeit, statistically non-significant) time to death found when the change in status was noted in the context of a planned care conference. However, the majority (80%) of documented conversations arose from concerns based on daily observations (ie, between scheduled assessments), pointing to the importance of recognizing when resident changes may be indicative of end-of-life decline, rooted in continuity of care and a familiarity with their usual habits and routines.33
Mealtimes present multiple daily opportunities for observing residents’ habits around eating and social participation and offer an accessible focal point for introducing comfort-focused care conversations when decline is observed. Indeed, eating challenges were a common consideration in identifying significant change in status of LTC residents, several of which (eg, low food/fluid intake, refusal to eat, swallowing difficulty, weight loss) are commonly associated with mortality.25,31,54–56 However, with the exception of swallowing difficulty, none were associated with a specific point in the end-of-life trajectory from the perspective of care providers. Non-nutritional signs were also identified. Although some of these were medical considerations (eg, unstable vitals, abnormal labs, specific diagnoses), others such as general decline, lethargy, mental health issues (eg, anxiety, restlessness), and social withdrawal are readily observable through interactions in the dining room and other points of contact with residents over the course of the day. Observed changes to residents’ eating patterns and other social routines may prompt the introduction of comfort-focused care conversations, regardless of timing to death, and are recommended as novel targets for future exploration.
Most of the identified signs and symptoms were not significantly associated with timing to death. Instead, they were identified by care providers across the trajectory of decline, lending to the interpretation of dying in LTC as a process of many, and sometimes fluctuating, signs and symptoms that can span several months preceding death.29,31 This finding may allow some emphasis to shift away from “early” identification of end-of-life decline and alleviate concerns around “unclear prognoses” because variable trajectories allow for flexibility in initiating comfort-focused conversations geared towards maintaining quality of life over the course of complex and life-limiting conditions. Alternatively, the suggested goal may be to have “timely” conversations, where the timing is person-centered, opportune, context-dependent, and reflective of the holistic needs of the resident and their substitute decision makers.57 The factors identified by care providers in this study may be considered as potential triggers for timely initiation of comfort-focused end-of-life conversations, regardless of the suspected prognosis. Pursuit of such opportunities for questioning possible end-of-life decline is worthwhile because, if not addressed, it can lead to missed opportunities for having end-of-life conversations58 and for initiating comfort-focused care.33 Indeed, conversations about the end of life in nursing homes have been shown to improve comfort-focused care.59 Care providers in the LTC setting are encouraged to reflect on when and if certain triggers (eg, low food intake, weight loss, general health instability or decline) might be opportune focal points for timely discussions on comfort-focused goals of care.
Limitations
This study was strengthened by a rigorous and in-depth data collection on a randomly selected sample of deceased long-term care residents. However, accessing all the homes from one chain limited the generalizability of the findings since end-of-life care conversations are likely driven at least in part by home culture, educational resources, and specific initiatives that may have been common to all of the homes. The sample size was relatively small, so the statistical power for identifying true associations was limited. We decided not to test interacting effects between signals (eg, weight loss and cancer) given these sample size limitations and lack of clear hypotheses for specific interactions, but, by not doing so, may have missed significant and clinically meaningful findings.
The original data extraction from the resident charts was performed by a single rater. While there were intra-rater reliability checks to ensure consistency over time and detailed definitions of each item were recorded for transparency, the data collection may have been influenced by personal biases of the data extractor. Furthermore, we may have missed important contextual details that were not documented in the residents’ progress notes, such as informal conversations and personal communications between family and team members. Since this study was not the main focus of the larger study that drove the data extraction, we did not collect data on formal measures of end-of-life decline, such as the palliative performance scale (PPS) or CHESS in relation to the timing of these end-of-life conversations, so were not able to assess the role of these prognostic indicators.
Directed content analysis is useful in condensing qualitative data (eg, free-text from resident charts) into discrete units for quantitative analysis. However, coding based on existing literature introduces bias towards confirming previously identified signs and symptoms where a new contextual interpretation may be warranted.49 Also, creating operational definitions for some of the codes was challenging because of the wide variety of documented information observed in the resident charts and loss of nuance with condensing the text into discrete units, which could potentially have led to misclassification.49 In particular, our definition of swallowing difficulty broadly included any indication of impaired swallowing (eg, diagnosed dysphagia, coughing or choking at meals) and did not account for the severity of these difficulties, a formalized diagnosis, nor a change in this symptom from a previous state. Such broad definitions of our codes limit the possible interpretation.
Conclusion
Given the high rate of morbidity and mortality among LTC residents, initiating end-of-life discussions and transitioning to comfort-focused care goals are important aspects of the care experience for residents and their family caregivers. However, the study findings reveal that the timing of these conversations is variable, often late in the end-of-life trajectory, and context dependent from the perspective of care providers. Our novel study findings identify the reasons given by care providers for suspecting end-of-life decline in current practice and draw attention to these signs and symptoms as focal points for revisiting goals of care. Awareness of such signs and symptoms, supported by educational initiatives to conduct more timely end-of-life conversations, has the potential to improve the quality of life and care outcomes for both residents and care providers.33,59 The authors contend that recognition of changes in residents’ eating habits and routines highlighted in this study in particular (eg, decreased food intake, refusal to eat) that are already observed and associated with end-of-life from the care provider perspective can be transformed into opportunities for introducing timely palliative-minded goals of care regardless of prognosis. Future work should explore ways to systematically incorporate comfort care conversations in response to these changes, facilitated by resources such as conversation guides, to support and maintain quality of life in the final months of life of LTC residents and the people who care for them.
Funding
This work was funded by the Canadian Institutes of Health Research (GSD-164141 to JMK).
Disclosure
Dr Jill Morrison-Koechl reports personal fees from Schlegel-UW Research Institute for Aging, outside the submitted work. Professor Heather Keller is the endowed research chair for Schlegel-UW Research Institute For Aging, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Ontario Long Term Care Association [OLTCA]. This is long-term care 2019. Ontario Long Term Care Association; 2019. Available from: https://www.oltca.com/OLTCA/Documents/Reports/TILTC2019web.pdf.
2. Ontario Long Term Care Association [OLTCA]. The data: long-term care in Ontario. Ontario Long Term Care Association; 2023. Available from: https://www.oltca.com/about-long-term-care/the-data/.
3. Yarnall AJ, Sayer AA, Clegg A, Rockwood K, Parker S, Hindle JV. New horizons in multimorbidity in older adults. Age Ageing. 2017;46(6):882–888. doi:10.1093/ageing/afx150
4. Yang RY, Yang AY, Chen YC, Lee SD, Lee SH, Chen JW. Association between dysphagia and frailty in older adults: a systematic review and meta-analysis. Nutrients. 2022;14(9):1812. doi:10.3390/nu14091812
5. Kojima G. Prevalence of frailty in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc. 2015;16(11):940–945. doi:10.1016/j.jamda.2015.06.025
6. Milte R, Petersen J, Boylan J, et al. Prevalence and determinants of physical frailty among people living in residential aged care facilities: a large-scale retrospective audit. BMC Geriatr. 2022;22(1):424. doi:10.1186/s12877-022-03101-8
7. Namasivayam AM, Steele CM. Malnutrition and dysphagia in long-term care: a systematic review. J Nutr Gerontol Geriatr. 2015;34(1):1–21. doi:10.1080/21551197.2014.1002656
8. Komici K, Guerra G, Addona F, Fantini C. Delirium in nursing home residents: a narrative review. Healthcare (Basel). 2022;10(8):1544. doi:10.3390/healthcare10081544
9. Borkent JW, Van Hout HPJ, Feskens EJM, Naumann E, De Van Der Schueren MAE. Diseases, health-related problems, and the incidence of malnutrition in long-term care facilities. Int J Environ Res Public Health. 2023;20(4):3170. doi:10.3390/ijerph20043170
10. Keller HH, Vucea V, Slaughter SE, et al. Prevalence of malnutrition or risk in residents in long term care: comparison of four tools. J Nutr Gerontol Geriatr. 2019;38(4):329–344. doi:10.1080/21551197.2019.1640165
11. Söderström L, Rosenblad A, Thors Adolfsson E, Bergkvist L. Malnutrition is associated with increased mortality in older adults regardless of the cause of death. Br J Nutr. 2017;117(4):532–540. doi:10.1017/S0007114517000435
12. Ng R, Lane N, Tanuseputro P, et al. Increasing complexity of new nursing home residents in Ontario, Canada: a serial cross-sectional study. J Am Geriatr Soc. 2020;68(6):1293–1300. doi:10.1111/jgs.16394
13. Menec VH, Nowicki S, Blandford A, Veselyuk D. Hospitalizations at the end of life among long-term care residents. J Gerontol A Biol Sci Med Sci. 2009;64A(3):395–402. doi:10.1093/gerona/gln034
14. Tanuseputro P, Hsu A, Kuluski K, et al. Level of need, divertibility, and outcomes of newly admitted nursing home residents. J Am Med Dir Assoc. 2017;18(7):616–623. doi:10.1016/j.jamda.2017.02.008
15. Canadian Institute for Health Information [CIHI]. Continuing care metadata; 2021. Available from: https://www.cihi.ca/en/continuing-care-metadata.
16. Kaasalainen S, Kaasalainen S, Sussman T, Neves P, Papaioannou A. Strengthening a Palliative Approach in Long-Term Care (SPA-LTC): a new program to improve quality of living and dying for residents and their family members. J Am Med Dir Assoc. 2016;17(3):B21. doi:10.1016/j.jamda.2015.12.067
17. Eisenmann Y, Golla H, Schmidt H, Voltz R, Perrar KM. Palliative care in advanced dementia. Front Psychiatry. 2020;11:699. doi:10.3389/fpsyt.2020.00699
18. Cloutier D, Stajduhar KI, Roberts D, Dujela C, Roland K. ‘Bare-bones’ to ‘silver linings’: lessons on integrating a palliative approach to care in long-term care in Western Canada. BMC Health Serv Res. 2021;21(1):610. doi:10.1186/s12913-021-06606-x
19. Canadian Institute for Health Information [CIHI]. Access to palliative care in Canada. CIHI; 2018. Available from: https://www.cihi.ca/sites/default/files/document/access-to-palliative-care-in-canada-2023-report-en.pdf.
20. Xiong B, Freeman S, Banner D, Spirgiene L. Hospice use and one-year survivorship of residents in long-term care facilities in Canada: a cohort study. BMC Palliat Care. 2019;18(1):100. doi:10.1186/s12904-019-0480-z
21. Qureshi D, Tanuseputro P, Perez R, Pond GR, Seow HY. Early initiation of palliative care is associated with reduced late-life acute-hospital use: a population-based retrospective cohort study. Palliat Med. 2019;33(2):150–159. doi:10.1177/0269216318815794
22. Barclay S, Froggatt K, Crang C, et al. Living in uncertain times: trajectories to death in residential care homes. Br J Gen Pract. 2014;64(626):e576–e583. doi:10.3399/bjgp14X681397
23. Hill E, Savundranayagam MY, Zecevic A, Kloseck M. Staff perspectives of barriers to access and delivery of palliative care for persons with dementia in long-term care. Am J Alzheimers Dis Other Demen. 2018;33(5):284–291. doi:10.1177/1533317518765124
24. van der Steen JT, Radbruch L, Hertogh CM, et al. White paper defining optimal palliative care in older people with dementia: a Delphi study and recommendations from the European Association for Palliative Care. Palliat Med. 2014;28(3):197–209. doi:10.1177/0269216313493685
25. Brandt HE. Symptoms, signs, problems, and diseases of terminally ill nursing home patients: a nationwide observational study in the Netherlands. Arch Intern Med. 2005;165(3):314. doi:10.1001/archinte.165.3.314
26. The National Hospice Organization. Medical guidelines for determining prognosis in selected non-cancer diseases. Hosp J. 1996;11(2):47–63. doi:10.1080/0742-969X.1996.11882820
27. Stuart B. The NHO medical guidelines for non-cancer disease and local medical review policy: hospice access for patients with diseases other than cancer. Hosp J. 1999;14(3–4):139–154. doi:10.1080/0742-969X.1999.11882934
28. Lunney JR. Patterns of functional decline at the end of life. JAMA. 2003;289(18):2387. doi:10.1001/jama.289.18.2387
29. Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ. 2005;330(7498):1007–1011. doi:10.1136/bmj.330.7498.1007
30. Boyd M, Frey R, Balmer D, et al. End of life care for long-term care residents with dementia, chronic illness and cancer: prospective staff survey. BMC Geriatr. 2019;19(1):137. doi:10.1186/s12877-019-1159-2
31. Åvik Persson H, Sandgren A, Fürst CJ, Ahlström G, Behm L. Early and late signs that precede dying among older persons in nursing homes: the multidisciplinary team’s perspective. BMC Geriatr. 2018;18(1):134. doi:10.1186/s12877-018-0825-0
32. Bern-Klug M. Calling the question of “possible dying” among nursing home residents: triggers, barriers, and facilitators. J Soc Work End Life Palliat Care. 2006;2(3):61–85. doi:10.1300/J457v02n03_06
33. Gonella S, Basso I, Clari M, Dimonte V, Di Giulio P. A qualitative study of nurses’ perspective about the impact of end‐of‐life communication on the goal of end‐of‐life care in nursing home. Scand J Caring Sci. 2021;35(2):502–511. doi:10.1111/scs.12862
34. Koechl JM. Exploring End-of-Life Nutrition Care for Residents of Long-Term Care: a Retrospective Chart Review [Doctoral Dissertation]. http://hdl.handle.net/10012/19739: University of Waterloo; 2023.
35. Brown MA, Sampson EL, Jones L, Barron AM. Prognostic indicators of 6-month mortality in elderly people with advanced dementia: a systematic review. Palliat Med. 2013;27(5):389–400. doi:10.1177/0269216312465649
36. Allison JJ, Wall TC, Spettell CM, et al. The art and science of chart review. Jt Comm J Qual Improv. 2000;26(3):115–136. doi:10.1016/S1070-3241(00)26009-4
37. Gearing RE, Mian IA, Barber J, Ickowicz A. A methodology for conducting retrospective chart review research in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2006;15(3):126–134.
38. Banks NJ. Designing medical record abstraction forms. Int J Qual Health Care. 1998;10(2):163–167. doi:10.1093/intqhc/10.2.163
39. Worster A, Haines T. Advanced statistics: understanding medical record review (MRR) studies. Acad Emerg Med off J Soc Acad Emerg Med. 2004;11(2):187–192. doi:10.1111/j.1553-2712.2004.tb01433.x
40. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
41. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010
42. Carpenter I, Hirdes JP. “Using interRAI assessment systems to measure and maintain quality of long-term care”, in A Good Life in Old Age?: Monitoring and Improving Quality in Long-term Care (Paris: OECD Publishing); 2013. doi: 10.1787/9789264194564-7–en.
43. Morris JN, Fries BE, Mehr DR, et al. MDS cognitive performance scale. J Gerontol. 1994;49(4):174. doi:10.1093/geronj/49.4.m174
44. Hirdes JP, Frijters DH, Teare GF. The MDS-CHESS scale: a new measure to predict mortality in institutionalized older people. J Am Geriatr Soc. 2003;51(1):96–100. doi:10.1034/j.1601-5215.2002.51017.x
45. Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol Biol Sci Med Sci. 1999;54(11):546. doi:10.1093/gerona/54.11.m546
46. Burrows AB, Morris JN, Simon SE, Hirdes JP, Phillips C. Development of a minimum data set-based depression rating scale for use in nursing homes. Age Ageing. 2000;29(2):165–172. doi:10.1093/ageing/29.2.165
47. Perlman CM, Hirdes JP. The aggressive behavior scale: a new scale to measure aggression based on the minimum data set. J Am Geriatr Soc. 2008;56(12):2298–2303. doi:10.1111/j.1532-5415.2008.02048.x
48. Fries BE, Simon SE, Morris JN, Flodstrom C, Bookstein FL. Pain in U.S. nursing homes: validating a pain scale for the minimum data set. Gerontologist. 2001;41(2):173–179. doi:10.1093/geront/41.2.173
49. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi:10.1177/1049732305276687
50. Goel MK, Khanna P, Kishore J. Understanding survival analysis: Kaplan-Meier estimate. Int J Ayurveda Res. 2010;1(4):274–278. doi:10.4103/0974-7788.76794
51. Lee J, Cheng J, ming AK, et al. Improving the quality of end-of-life care in long-term care institutions. J Palliat Med. 2013;16(10):1268–1274. doi:10.1089/jpm.2013.0190
52. Sachs GA, Carter R, Holtz LR, et al. Cognitive impairment: an independent predictor of excess mortality: a cohort study. Ann Intern Med. 2011;155(5):300. doi:10.7326/0003-4819-155-5-201109060-00007
53. Jørgensen TL, Hallas J, Friis S, Herrstedt J. Comorbidity in elderly cancer patients in relation to overall and cancer-specific mortality. Br J Cancer. 2012;106(7):1353–1360. doi:10.1038/bjc.2012.46
54. Wirth R, Pourhassan M, Streicher M, et al. The impact of dysphagia on mortality of nursing home residents: results from the nutritionDay project. J Am Med Dir Assoc. 2018;19(9):775–778. doi:10.1016/j.jamda.2018.03.016
55. Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361(16):1529–1538. doi:10.1056/NEJMoa0902234
56. Fringer A, Stängle S, Büche D, Ott SCH, Schnepp W. The associations of palliative care experts regarding food refusal: a cross-sectional study with an open question evaluated by triangulation analysis. PLoS One. 2020;15(4):e0231312. doi:10.1371/journal.pone.0231312
57. Dhedhi SA, Swinglehurst D, Russell J. ‘Timely’ diagnosis of dementia: what does it mean? A narrative analysis of GPs’ accounts. BMJ Open. 2014;4(3):e004439. doi:10.1136/bmjopen-2013-004439
58. Towsley GL, Hirschman KB, Madden C. Conversations about end of life: perspectives of nursing home residents, family, and staff. J Palliat Med. 2015;18(5):421–428. doi:10.1089/jpm.2014.0316
59. Gonella S, Basso I, Dimonte V, et al. Association between end-of-life conversations in nursing homes and end-of-life care outcomes: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(3):249–261. doi:10.1016/j.jamda.2018.10.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.