Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
Novel Preoperative Type IV Collagen to Predict the Risk of Hepatocellular Carcinoma in Patients with Hepatitis B Virus-Related Cirrhotic Portal Hypertension After Laparoscopic Splenectomy and Azygoportal Disconnection
Authors Gao TM , Jin SJ , Fang F , Qian JJ , Zhang C, Zhou BH , Bai DS , Jiang GQ
Received 4 July 2023
Accepted for publication 15 August 2023
Published 12 January 2024 Volume 2023:10 Pages 2411—2420
DOI https://doi.org/10.2147/JHC.S425814
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Mohamed Shaker
Tian-Ming Gao,1,* Sheng-Jie Jin,1,* Fang Fang,2,* Jian-Jun Qian,1 Chi Zhang,1 Bao-Huan Zhou,1 Dou-Sheng Bai,1 Guo-Qing Jiang1
1Department of Hepatobiliary Surgery, Clinical Medical College, Yangzhou University, Yangzhou, 225001, People’s Republic of China; 2Department of Gastrointestinal Surgery, Clinical Medical College, Yangzhou University, Yangzhou, 225001, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Guo-Qing Jiang; Dou-Sheng Bai, Department of Hepatobiliary Surgery, Clinical Medical College, Yangzhou University, 98 West Nantong Road, Yangzhou, 225000, People’s Republic of China, Email [email protected]; [email protected]
Purpose: Although laparoscopic splenectomy and azygoportal disconnection (LSD) can significantly decrease portal vein pressure and even the incidence of hepatocellular carcinoma (HCC) in patients with cirrhotic portal hypertension (CPH), postoperative HCC inevitably occurs in certain patients. The purpose of this study was to seek a novel preoperative non-invasive predictive indicator to predict the occurrence of postoperative HCC.
Patients and Methods: From April 2012 to April 2022, we collected clinical data of 178 hepatitis B virus (HBV)-related CPH patients. Based on inverse treatment probability weighting, candidate variables for predicting postoperative HCC were determined by means analysis. Then, a novel preoperative non-invasive prediction indicator (ie, type IV collagen-alpha fetoprotein-fibrosis-4 score [IVAF-FIB-4]) was established based on candidate variables, and its predictive ability was explored.
Results: Postoperative HCC occurred in 9 (5.1%) patients. Correlation analyses showed that the IVAF-FIB-4 had a significant positive correlation with HCC (r = 0.835, P < 0.001). IVAF-FIB-4 showed a high accuracy (the area under the receiver operating characteristic curve: 0.939, 95% confidence interval [CI]: 0.818– 1.000; sensitivity: 88.9%; specificity: 93.5%). At the end of follow-up, the incidence density of HCC in patients with IVAF-FIB-4 (1) was significant higher than that in patients with IVAF-FIB-4 (0) (138.1/1000 vs 1.1/1000 person-years; rate ratio: 130.475, 95% CI: 16.318– 1043.227). In logistic regression, IVAF-FIB-4 was an independent risk factor for HCC (odds ratio: 668.000, 95% CI: 53.895– 8279.541; P < 0.001).
Conclusion: IVAF-FIB-4 is a novel preoperative noninvasive predictive indicator for predicting postoperative HCC in HBV-related CPH patients after LSD, with satisfactory predictive ability.
Keywords: liver fibrotic markers, splenectomy, azygoportal disconnection, hepatocellular carcinoma, risk
Introduction
Liver cancer is one of the most common malignant tumors worldwide, and the most common histological type is hepatocellular carcinoma (HCC).1,2 One of the most important causes of HCC is liver cirrhosis, which can be caused by a variety of factors. Virus-related cirrhosis is most prevalent in Asia, especially hepatitis B virus (HBV). The annual incidence of HCC in patients with HBV-related cirrhosis is 3%–6%, which is the main cause of HCC in China.3,4 At present, there are about 350 million HBV-infected people in the world, and every year, over 500,000 people die from diseases associated with HBV, including liver cirrhosis and liver cancer.5
In clinical practice, the decompensated period of cirrhosis is accompanied by clinical manifestations such as low liver function, portal hypertension, splenomegaly, and hypersplenism.6,7 Due to its advantages of less trauma, faster recovery, and less inflammatory interference, laparoscopic splenectomy and azygoportal disconnection (LSD) has gradually become the ideal surgical modality for the treatment of these decompensated patients with cirrhotic portal hypertension (CPH) in Asia. Unfortunately, although LSD can improve the liver function, and portal vein pressure, and even decrease the incidence of HCC,8–10 some patients inevitably develop HCC due to the background of liver fibrosis and cirrhosis.
Implementing HCC surveillance is important because it is the only way to identify HCC at an early stage, thereby reducing disease-related morbidity and mortality.11 However, identifying which patients may or may not require close HCC surveillance is an important but unresolved issue in our clinical practice. Therefore, it is necessary to find a simple and effective method to assess and predict the risk of HCC for CPH patients. If high-risk HCC groups can be identified in advance, and then receive regular checkups, potential HCC can be detected as early as possible and treated in time.
Currently, as advanced non-invasive fibrotic indicators, laminin (LN), type IV collagen (C-IV), hyaluronidase (HA), procollagen type III (PC-III), and fibrosis-4 score (FIB-4) have aroused extensive clinical attention. These indicators have been found to be significantly associated with the progression of liver fibrosis in patients with chronic liver disease.12–14 It is well known that severe liver fibrosis is closely related to the occurrence and development of HCC.15–17 Then, whether these indicators are also related to the occurrence and development of HCC, relevant research is rare. In addition, as an important indicator for the diagnosis and efficacy monitoring of liver cancer, it is unclear whether serum alpha fetoprotein (AFP) is related to the occurrence of HCC after LSD. Therefore, the aim of this study was to seek a novel preoperative non-invasive predictive indicator to predict the occurrence of postoperative HCC after LSD and explore its predictive ability.
Materials and Methods
Study Population
From April 2012 to April 2022, We collected clinical data of 468 CPH patients with gastroesophageal variceal bleeding and secondary hypersplenism in our hepatobiliary pancreatic center. The exclusion criteria: age <18 years; any cancer before treatment; Child–Pugh class C; cirrhosis not caused by HBV; treatment with transjugular intrahepatic portosystemic shunt or liver transplantation; the first variceal bleeding treatment was not LSD; perioperative death; simple splenectomy or azygoportal disconnection; pregnancy; human immunodeficiency virus infection; uncontrolled diabetes or hypertension; and computed tomography image was not consistent with the manifestations of liver cirrhosis. In addition, we also excluded the patients with HBV DNA viral load ≥100 IU/mL at postoperative months (POM) 3 to ensure the comparability of postoperative HBV management in each patient. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards, and the Medical Ethics Committee of Clinical Medical College of Yangzhou University approved the study. This retrospective study was based on the existing data in the hospital database and did not involve intervention on patients; therefore, an exemption for informed consent of patients was obtained from the ethics committee.
Data Extraction
Considering the influence of different etiologies on the occurrence of liver cancer, in order to allow better homogeneity in etiology between the groups, this study only included HBV-related CPH patients. All patients were successfully treated with LSD in our previous study, we had reported the specific implementation methods for LSD and intraoperative autologous cell retrieval.18 The general population data of patients collected included age, gender, body mass index (BMI), and year of treatment. The clinical characteristics data of all patients included preoperative Child-Pugh classification, FIB-4, portal vein thrombus, diabetes, hypertension, spleen diameter, portal vein diameter, splenic vein diameter, white blood cell count (WBC), platelet count (PLT), hemoglobin (HGB), alanine aminotransferase (ALT), plasma albumin (ALB), total bilirubin (TBIL), creatinine (Cr), blood urea nitrogen (BUN), international normalized ratio (INR), AFP, LN, C-IV, HA, and PC-III. Considering the continuous enrollment of new patients, as well as the uncertainty of patient loss to follow-up and death, we use the incidence density to describe the occurrence of HCC. Our retrospective follow-up period was 11 years, and the follow-up endpoint of patients was HCC or death.
Preoperative Non-Invasive Predictive Indicator
Candidate variables for predicting postoperative HCC were determined by means analysis before and after weighting, and the cutoff value of candidate indicators was determined by calculating Youden’s index (sensitivity+specificity-1).19 In this study, AFP, FIB-4, and C-IV were candidate indicators, and the cutoff values were 2.08, 6.92, and 73.95, respectively. Then, a novel non-invasive predictive indicator, type IV collagen-alpha fetoprotein-fibrosis-4 score (IVAF-FIB-4) was obtained by combining these three indicators. When C-IV level ≥73.95 µg/L, AFP level ≥2.08 ng/mL, and FIB-4 ≥6.917 were met at the same time, the novel indicator was assigned a value of 1, and the other cases were assigned a value of 0. Then, the patients were divided into IVAF-FIB-4 (0) and IVAF-FIB-4 (1) groups.
Statistical Analysis
When using observational clinical data to infer causality, if the effect of covariates between groups is not considered, the causal relationship between treatment factors and effects will be distorted, and causal inference will be biased. In order to better understand the correlation between liver fibrotic markers and the occurrence of HCC, we used inverse treatment probability weighting (IPTW) to reduce the confounding bias between groups and make the covariates between groups reach relatively balanced.20
Means between groups were compared using independent samples t-test, Mann–Whitney U-test or chi-square test, combined with IPTW. Continuous variables are reported as mean (standard deviation) or median (interquartile range), and categorical variables were reported as frequencies and percentages. Receiver operating characteristic (ROC) curves, the area under the ROC curve (AUC), and correlation analysis were used to evaluate the predictive ability of these indicators. When the AUC value is 0.5 to 0.7, it means low accuracy, 0.7 to 0.9 means certain accuracy, and greater than 0.9 means high accuracy. P < 0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS 25.0 software (IBM Corp., Armonk, NY, USA) and R software (version 4.2.2).
Results
The enrollment process is shown in Figure 1. A total of 178 HBV-related CPH patients with gastroesophageal variceal bleeding and secondary hypersplenism were enrolled in the study. The mean follow-up time was 67.6 months. At the end of the follow-up, 9 patients developed postoperative HCC, and the time ranged from 4 to 72 months, with an average time of 31.5 months and a median time of 14 months. Additionally, according to whether HCC occurred after LSD, the patients were divided into HCC group (n = 9) and non-HCC group (n = 169).
 |
Figure 1 CONSORT diagram. Notes: CONSORT figure adapted from Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010;7(3): e1000251.21 Copyright: © 2010 Schulz et al. Creative Commons Attribution License. |
Comparison of HCC and Non-HCC Groups in Terms of Demographics and Clinical Characteristics
As shown in Supplementary Table 1, there were no significant differences in HBsAg, HBsAb, HBeAg, HBeAb, and HBcAb between the non-HCC group and the HCC group (all P > 0.05). Additionally, LN, HA, PC-III, and FIB-4 had no significant differences between HCC and non-HCC groups before IPTW (all P > 0.05; Table 1). After weighting for gender, age, year of treatment, BMI, cirrhotic etiology, hypertension, diabetes, Child-Pugh classification, portal vein thrombosis, longitudinal diameter of the spleen, portal vein diameter, splenic vein diameter, WBC, PLT, HGB, TBIL, ALB, ALT, INR, Cr, and BUN, the differences in LN, HA, PC-III between HCC and non-HCC groups were still not statistically significant (all P > 0.05), but the difference in FIB-4 became statistically significant (P = 0.021). Nevertheless, whether the relevant covariates were weighted or not, the C-IV and AFP were significantly different between the two groups (all P < 0.05).
 |
Table 1 Demographic and Preoperative Clinical Characteristics Between Non-HCC and HCC Groups in Unadjusted and IPTW Adjusted Population |
The ROC and Correlation Analysis of Candidate Variables and Non-Invasive Predictive Indicator
As shown in Table 2, we performed a correlation analysis of HCC with candidate variables and IVAF-FIB-4. The results showed that IVAF-FIB-4 had the highest positive correlation with the occurrence of HCC (r = 0.835, P < 0.001), followed by C-IV (r = 0.585, P < 0.001), FIB-4 (r = 0.277, P < 0.001), and AFP (r = 0.192, P = 0.010).
 |
Table 2 Correlation Analysis of HCC with C-IV, AFP, FIB-4, and IVAFP-FIB-4 |
We performed an ROC analysis of AFP, FIB-4, C-IV, and IVAF-FIB-4 to determine their clinical value for predicting postoperative HCC (Figure 2). In contrast, IVAF-FIB-4 (AUC: 0.930, 95% confidence interval [CI]: 0.812–1.000; P < 0.001) showed the highest accuracy in predicting postoperative HCC, with an associated sensitivity of 88.9% and specificity of 97.0%. Followed by C-IV (AUC: 0.912, 95% CI: 0.791–1.000; P < 0.001), FIB-4 (AUC: 0.811, 95% CI: 0.725–0.896; P = 0.002) and AFP (AUC: 0.716, 95% CI: 0.597–0.835; P = 0.029). In addition, the performance of ROC curve was compared by DeLong’s test, IVAF-FIB-4 had statistical significance compared with C-IV, FIB-4, and AFP, respectively (all P < 0.05; Figure 2).
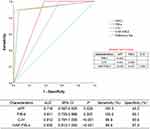 |
Figure 2 Receiver operating characteristic curve analysis to assess the accuracy of candidate variables and the non-invasive predictive indicator in discriminating patients with and without HCC. |
Incidence of HCC at the End of Follow-Up
All patients were divided into IVAF-FIB-4 (0) and IVAF-FIB-4 (1) groups according to the preoperative non-invasive predictive indicator, their mean follow-up times were 67.5 months and 69.5 months, respectively. As shown in Figure 3, at the end of the follow-up, among the all patients, 5.1% (9/178) developed postoperative HCC, while 0.6% (1/168) in patients with IVAF-FIB-4 (0) and 80.0% (8/10) in patients with IVAF-FIB-4 (1). In addition, the incidence densities of HCC among HBV-related CPH patients during the follow-up period are shown in Figure 4. At the end of follow-up, the incidence density of HCC in patients with IVAF-FIB-4 (1) was significant higher than that in patients with IVAF-FIB-4 (0) (138.1/1000 vs 1.1/1000 person-years; rate ratio: 130.475, 95% CI: 16.318–1043.227).
Independent Risk Predictors of HCC Incidence
Before IPTW, the results of logistic regression analysis showed that compared with IVAF-FIB-4 (0), IVAF-FIB-4 (1) was an independent risk factor for postoperative HCC (odds ratio: 668.000, 95% CI: 53.895–8279.541; P < 0.001; Table 3). After weighting for gender, age, year of treatment, BMI, cirrhotic etiology, hypertension, diabetes, Child-Pugh classification, portal vein thrombosis, longitudinal diameter of the spleen, portal vein diameter, splenic vein diameter, WBC, PLT, HGB, TBIL, ALB, ALT, INR, Cr, and BUN, the results of logistic regression analysis still showed that IVAF-FIB-4 (1) was an independent risk factor for postoperative HCC (odds ratio: 3244.565, 95% CI: 316.198–33293.081; P < 0.001; Table 3).
 |
Table 3 Logistic Regression Analysis of Occurrence of HCC in Unadjusted and IPTW Adjusted Population |
Discussion
It is well known that liver fibrosis is a major risk for HCC, and the more serious the degree of liver fibrosis, the higher the risk of HCC.15–17 The most serious degree of liver fibrosis is cirrhosis, and about 85–95% of HCC patients suffer from cirrhosis.22 Much of the literature has reported that C-IV is positively correlated with the progression of liver fibrosis.12–14 C-IV is an important component of the normal extracellular matrix (ECM), which is also the main component of the liver interstitial basement membrane. C-IV will occur in the serum when the basement membrane is formed or destroyed.23,24
MMP-2 and MMP-9 are the members of the matrix metalloproteinase (MMPs) family. Many studies have shown that MMPs, as important enzymes currently known to degrade ECM, play an important role in promoting tumor angiogenesis, metastasis, and invasion.25–27 MMP-2 and MMP-9 are considered as potential biomarkers in the process of tumorigenesis, as well as key effectors of ECM remodeling and important potential targets for anti-tumor therapy.28,29 The ECM degradation caused by MMPs will lead to an increased C-IV level in serum.30 Therefore, logically, C-IV level in serum may be positively correlated with the risk of tumor.
In this study, the increase in C-IV level in serum reflects the progression of liver fibrosis, on the one hand, and, on the other hand, it may also be due to the early activation of MMPs in patients, which makes basement membrane catabolism active, resulting in an increase in serum C-IV level. The expression of MMP-2/9 is reported to be associated with the progression of liver cancer.31 So, the increased C-IV level in serum may suggest important information for the early HCC development in liver cirrhosis patients, which needs to be further explored in future studies.
In addition, FIB-4 has been confirmed by many studies to have the ability to assess the degree of liver fibrosis in patients with chronic liver disease.32,33 Some scholars have indicated that in a cohort of non-cirrhotic patients with chronic HBV infection, a higher FIB-4 was associated with an increased risk of HCC.34,35 For a long time, AFP has been considered as a biomarker for the clinical diagnosis and prognosis of HCC. Moreover, some scholars have confirmed the cancer-promoting role of AFP in the development of HCC using AFP deficient mouse models. Based on these findings, the combination of C-IV, AFP, and FIB-4 may be a good potential predictor for the occurrence of HCC.
In Asia, the benefits of LSD in the treatment of patients with CPH have been increasingly recognized. LSD can not only improve liver reserve function but also reduce portal vein pressure and the risk of gastroesophageal variceal bleeding.8,9 In addition, LSD even reduced the incidence of postoperative HCC.10 However, some CPH patients after LSD still inevitably progress to HCC. Therefore, in order to seek certain markers that can better predict postoperative HCC after LSD, we explored the relationship between non-invasive predictive indicator and postoperative HCC.
In this study, we found that C-IV, AFP, and FIB-4 were potential markers to predict postoperative HCC after LSD. A novel non-invasive predictive indicator (ie, IVAF-FIB-4) resulting from combining these three indicators was an independent risk factor for postoperative HCC with satisfactory diagnostic accuracy and reasonable predictive performance. Its AUC value was 0.939, with associated sensitivity of 88.9% and specificity of 98.8%. The logistic regression analysis showed that the likelihood of postoperative HCC in patients with IVAF-FIB-4 (1) was 668 times than that in patients with IVAF-FIB-4 (0). After weighting by IPTW, the risk was increased to 3244.565 times. In addition, at the end of follow-up, the 11-year HCC incidence density in patients with IVAF-FIB-4 (1) was significantly higher than that in patients with IVAF-FIB-4 (0) (138.1/1000 vs 1.1/1000 person-years). These phenomena indicate that when the patients have C-IV ≥73.95 µg/L, AFP ≥2.08 ng/mL, or FIB-4 ≥6.917 conditions, we should pay appropriate attention. And when the patient has IVAF-FIB-4 (1) condition, we should pay more attention, in order to detect problems as early as possible and intervene in a timely manner.
The present study has several limitations. First, the sample size of this research is not big enough, mainly because liver fibrotic markers in the early stage were not tested in our department. Second, this is a retrospective study. Prospective and multi-center studies are needed to verify the findings of this study in the future. Thirdly, the patients were regularly followed up every three months within 1 year after LSD. Then, after one year, the follow-up interval is usually half a year, some patients may have developed HCC without noticing during the follow-up interval. Fourth, this study focuses on HBV-related CPH patients after LSD, and whether its finding is fit for all cirrhosis patients needs to be further investigated. Finally, the detection of HBsAg, HBeAb, HBcAb, and other indicators in our hospital were only qualitative measurements, and the concentration value cannot be obtained. We hope to increase the quantitative detection of these indicators in future prospective studies.
Conclusion
To the best of our knowledge, this is the first report on the exploration of a non-invasive predictive indicator for postoperative HCC in HBV-related CPH patients after LSD. This study found that C-IV ≥73.95 µg/L, AFP ≥2.08 ng/mL, and FIB-4 ≥6.917 were all potential indicators to predict postoperative HCC after LSD. It is worth noting that the non-invasive predictive indicator based (ie, IVAF-FIB-4) on these three indicators showed a very satisfactory predictive ability for occurrence of postoperative HCC in HBV-related CPH patients after LSD. Therefore, in clinical practice, we can identify HBV-related CPH patients with a high risk of postoperative HCC in advance, and then strengthen the regular checkups for these patients, so as to facilitate early detection of HCC and timely treatment, thereby bringing better survival benefits to these patients.
Abbreviations
LSD, laparoscopic splenectomy and azygoportal disconnection; HCC, hepatocellular carcinoma; CPH, cirrhotic portal hypertension; HBV, hepatitis B virus; LT, Liver transplantation; TIPS, transjugular intrahepatic portosystemic shunt; C-IV, type IV collagen; IPTW, inverse treatment probability weighting; LN, laminin; HA, hyaluronidase; PC-III, procollagen type III; AFP, alpha fetoprotein; FIB-4, fibrosis-4 score; IVAF-FIB-4, type IV collagen-alpha fetoprotein-fibrosis-4 score; POM, postoperative months; BMI, body mass index; WBC, white blood cells; HGB, hemoglobin; PLT, platelets; ALT, alanine aminotransferase; INR, international normalized ratio; BUN, blood urea nitrogen; Cr, creatinine; ROC, Receiver operating characteristic; AUC, area under the receiver operating characteristic curve; ECM, extracellular matrix; MMPs, matrix metalloproteinase; OR, odds ratio.
Acknowledgments
This study is a joint effort of many investigators and staff members, and their contribution is gratefully acknowledged. We especially thank all patients who participated in this study.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 82173353).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi:10.3322/caac.21660
2. Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics 2023. CA. Cancer J Clin. 2023;73:17–48. doi:10.3322/caac.21763
3. Chinese Society of Infectious Diseases, Chinese Medical Association; Chinese Society of Hepatology, Chinese Medical Association. 慢性乙型肝炎防治指南(2019)年版 [The guidelines of prevention and treatment for chronic hepatitis B (2019 version)]. Zhonghua Gan Zang Bing Za Zhi. 2019;27:938–961. Chinese. doi:10.3760/cma.j.issn.1007-3418.2019.12.007
4. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China 2015. CA. Cancer J Clin. 2016;66:115–132. doi:10.3322/caac.21338
5. Cholongitas E, Papatheodoridis GV, Goulis J, et al. The impact of newer nucleos (t) ide analogues on patients with hepatitis B decompensated cirrhosis. Ann Gastroenterol. 2015;28:109.
6. Zhang L, Zhang ZG, Long X, et al. Severe complications after splenic artery embolization for portal hypertension due to hepatic cirrhosis. Risk Manag Healthc Policy. 2020;13:135–140. doi:10.2147/RMHP.S234628
7. Singal AG, Zhang E, Narasimman M, et al. HCC surveillance improves early detection, curative treatment receipt, and survival in patients with cirrhosis: a meta-analysis. J Hepatol. 2022;77(1):128–139. doi:10.1016/j.jhep.2022.01.023
8. Bai DS, Chen P, Jin SJ, Qian JJ, Jiang GQ. Vagus nerve-preserving versus conventional laparoscopic splenectomy and azygoportal disconnection. Surg Endosc. 2018;32:2696–2703. doi:10.1007/s00464-017-5965-3
9. Bai DS, Qian JJ, Chen P, et al. Laparoscopic azygoportal disconnection with and without splenectomy for portal hypertension. Int J Surg. 2016;34:116–121. doi:10.1016/j.ijsu.2016.08.519
10. Gao TM, Zhou J, Xiang XX, et al. Splenectomy and azygoportal disconnection decreases the risk of hepatocellular carcinoma for cirrhosis patients with portal hypertension bleeding: a 10-year retrospective follow-up study based on the inverse probability of treatment weighting method. J Gastroenterol. 2023;58:503–512. doi:10.1007/s00535-023-01982-z
11. Yang JD, Heimbach JK. New advances in the diagnosis and management of hepatocellular carcinoma. BMJ. 2020;371:m3544. doi:10.1136/bmj.m3544
12. Harris R, Harman DJ, Card TR, Aithal GP, Guha IN. Prevalence of clinically significant liver disease within the general population, as defined by non-invasive markers of liver fibrosis: a systematic review. Lancet Gastroenterol Hepatol. 2017;2(4):288–297. doi:10.1016/S2468-1253(16)30205-9
13. Mei L, Ma Y, Zhao LL, et al. Correlation between serum liver fibrosis markers and early gastroesophageal varices among patients with compensated liver cirrhosis: a cross-sectional analysis. BMC Gastroenterol. 2022;22(1):515. doi:10.1186/s12876-022-02546-w
14. El-Mezayen HA, Habib S, Marzok HF, Saad MH. Diagnostic performance of collagen IV and laminin for the prediction of fibrosis and cirrhosis in chronic hepatitis C patients: a multicenter study. Eur J Gastroenterol Hepatol. 2015;27:378–385. doi:10.1097/MEG.0000000000000298
15. Cholankeril G, Kramer JR, Chu J, et al. Longitudinal changes in fibrosis markers are associated with risk of cirrhosis and hepatocellular carcinoma in non-alcoholic fatty liver disease. J Hepatol. 2023;78:493–500. doi:10.1016/j.jhep.2022.10.035
16. Affo S, Yu LX, Schwabe RF. The role of cancer-associated fibroblasts and fibrosis in liver cancer. Annu Rev Pathol. 2017;12:153–186. doi:10.1146/annurev-pathol-052016-100322
17. Dhar D, Baglieri J, Kisseleva T, Brenner DA. Mechanisms of liver fibrosis and its role in liver cancer. Exp Biol Med. 2020;245:96–108. doi:10.1177/1535370219898141
18. Jiang GQ, Bai DS, Chen P, et al. Modified laparoscopic splenectomy and azygoportal disconnection combined with cell salvage is feasible and might reduce the need for blood transfusion. World J Gastroenterol. 2014;20:18420–18426. doi:10.3748/wjg.v20.i48.18420
19. Bantis LE, Tsimikas JV, Chambers GR, Capello M, Hanash S, Feng Z. The length of the receiver operating characteristic curve and the two cutoff Youden index within a robust framework for discovery, evaluation, and cutoff estimation in biomarker studies involving improper receiver operating characteristic curves. Stat Med. 2021;40(7):1767–1789. doi:10.1002/sim.8869
20. Williamson EJ, Forbes A, White IR. Variance reduction in randomised trials by inverse probability weighting using the propensity score. Stat Med. 2014;33:721–737. doi:10.1002/sim.5991
21. Schulz KF, Altman DG, Moher D. CONSORT statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7(3):e1000251.
22. Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301–1314. doi:10.1016/S0140-6736(18)30010-2
23. Daulagala AC, Kourtidis A. ECM substrates impact RNAi localization at adherens junctions of colon epithelial cells. Cells. 2022;11(23):3740. doi:10.3390/cells11233740
24. Karsdal MA, Daniels SJ, Holm Nielsen S, et al. Collagen biology and non-invasive biomarkers of liver fibrosis. Liver Int. 2020;40(4):736–750. doi:10.1111/liv.14390
25. Nyormoi O, Mills L, Bar-Eli M. An MMP-2/MMP-9 inhibitor, 5a, enhances apoptosis induced by ligands of the TNF receptor superfamily in cancer cells. Cell Death Differ. 2003;10:558–569. doi:10.1038/sj.cdd.4401209
26. Eissa S, Ali-Labib R, Swellam M, Bassiony M, Tash F, El-Zayat TM. Noninvasive diagnosis of bladder cancer by detection of matrix metalloproteinases (MMP-2 and MMP-9) and their inhibitor (TIMP-2) in urine. Eur Urol. 2007;52:1388–1396. doi:10.1016/j.eururo.2007.04.006
27. Sang QX. Complex role of matrix metalloproteinases in angiogenesis. Cell Res. 1998;8:171–177. doi:10.1038/cr.1998.17
28. Kowalczyk A, Nisiewicz MK, Bamburowicz-Klimkowska M, et al. Effective voltammetric tool for simultaneous detection of MMP-1, MMP-2, and MMP-9; important non-small cell lung cancer biomarkers. Biosens Bioelectron. 2023;229:115212. doi:10.1016/j.bios.2023.115212
29. Cavdar Z, Canda AE, Terzi C, Sarioglu S, Fuzun M, Oktay G. Role of gelatinases (matrix metalloproteinases 2 and 9), vascular endothelial growth factor and endostatin on clinicopathological behaviour of rectal cancer. Colorectal Dis. 2011;13:154–160. doi:10.1111/j.1463-1318.2009.02105.x
30. Niu A, Qi TG. Diagnostic significance of serum type IV collagen (IVC) combined with aspartate aminotransferase (AST)/alanine aminotransferase (ALT) ratio in liver fibrosis. Ann Transl Med. 2022;10:1310. doi:10.21037/atm-22-5010
31. Ordoñez R, Carbajo-Pescador S, Prieto-Dominguez N, García-Palomo A, González-Gallego J, Mauriz JL. Inhibition of matrix metalloproteinase-9 and nuclear factor kappa B contribute to melatonin prevention of motility and invasiveness in HepG2 liver cancer cells. J Pineal Res. 2014;56:20–30. doi:10.1111/jpi.12092
32. Seong G, Sinn DH, Kang W, et al. Age and fibrosis index for the prediction of hepatocellular carcinoma risk in patients with high hepatitis B virus DNA but normal alanine aminotransferase. Eur J Gastroenterol Hepatol;2022. 69–75. doi:10.1097/MEG.0000000000001915
33. Nishikawa H, Nishijima N, Enomoto H, et al. Comparison of FIB-4 index and aspartate aminotransferase to platelet ratio index on carcinogenesis in chronic hepatitis B treated with entecavir. J Cancer;2017. 152–161. doi:10.7150/jca.16523
34. Tseng TC, Liu C, Su TH, et al. Fibrosis-4 index helps identify HBV carriers with the lowest risk of hepatocellular carcinoma. Am J Gastroenterol. 2017;112:1564–1574. doi:10.1038/ajg.2017.254
35. Chen TJ, Dai XW, Dai JJ, et al. AFP promotes HCC progression by suppressing the HuR-mediated Fas/FADD apoptotic pathway. Cell Death Dis. 2020;11:822. doi:10.1038/s41419-020-03030-7
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.