Back to Journals » Nature and Science of Sleep » Volume 14
Not Only Excessive Daytime Sleepiness but Also Depression Symptoms, Chronological Age and Onset-Age Were Associated with Impulsivity in Narcolepsy Type 1 Patients
Authors Yang Y, Zhang J, Han F, Xiao F
Received 4 June 2022
Accepted for publication 11 October 2022
Published 17 October 2022 Volume 2022:14 Pages 1857—1866
DOI https://doi.org/10.2147/NSS.S377372
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Yang Yang,1 Jun Zhang,2 Fang Han,3 Fulong Xiao4
1Department of Neuropsychiatry and Behavioral Neurology and Clinical Psychology, Beijing Tiantan Hospital, Capital Medical University, Beijing, 100070, People’s Republic of China; 2Department of Neurology, Peking University People’s Hospital, Beijing, 100044, People’s Republic of China; 3Sleep Medicine Center, Department of Respiratory and Critical Care Medicine, Peking University People’s Hospital, Beijing, 100044, People’s Republic of China; 4Department of General Internal Medicine, Peking University People’s Hospital, Beijing, 100044, People’s Republic of China
Correspondence: Fang Han; Fulong Xiao, Peking University People’s Hospital, No. 11, South Avenue, Beijing, People’s Republic of China, Email [email protected]; [email protected]
Objective: To detect the factors associated with total and subscales impulsivity scores in narcolepsy and further explore the non-linear relationship between these factors and impulsivity score.
Methods: One hundred and fifty-eight narcolepsy type 1 (NT1) patients were involved in this cross-sectional study. Patients completed questionnaires evaluating impulsivity symptoms (Barratt impulse scale-11, BIS-11), depression symptoms (Center for Epidemiologic Studies Depression Scale for Children, CES-DC or Self-Rating Depression Scale, SDS) and sleepiness (Epworth Sleepiness Scale, ESS). Parameters from polysomnography and multiple sleep latency test were also collected. Linear regression analysis was performed to detect the factors associated with total and subscales impulsivity scores. Then, generalized additive models and smooth curve fitting were performed to explore the non-linear relationship between chronological age and impulsivity scores.
Results: Factors associated with higher total impulsivity score were higher ESS, older onset and adolescents. Factors associated with higher attentional impulsivity score were higher ESS, older onset and adolescents. Factors associated with higher motor impulsivity score were higher ESS, younger onset and depression symptoms. Factors associated with higher non-planning impulsivity score were adolescents, older onset and depression symptoms. A non-linear relationship between age and impulsivity scores (total impulsivity score, attentional impulsivity score and non-planning impulsivity score) was detected in NT1 patients.
Conclusion: Not only excessive daytime sleepiness but also onset-age, depression symptoms and chronological age were associated with impulsivity in NT1 patients. The non-linear relationship between age and impulsivity scores suggested brain and mental development alterations in NT1 patients.
Keywords: narcolepsy, impulsivity, excessive daytime sleepiness, depression, smooth curve fitting
Introduction
Narcolepsy type 1 (NT1) is a central sleepiness disorder due to hypocretin deficiency in the hypothalamus, which is characterized by excessive daytime sleepiness, cataplexy, hypnagogic/hypnopompic hallucination and sleep paralysis. Recent research findings suggested that disturbed nocturnal sleep (DNS) is considered a specific symptom that is independent of other symptoms in narcolepsy.1 DNS in narcolepsy is characterized by patients’ complaints of frequent awakenings, increased N1 sleep and decreased sleep efficiency.1 DNS may be primary or secondary to comorbid sleep disorders including insomnia or sleep apnea in narcolepsy.1 Approximately 20–30% of narcolepsy patients reported sleep apnea, which is associated with age, body mass index (BMI) and male sex.2,3 Limited studies have demonstrated that narcolepsy itself rather than sleep apnea may play a greater role in the pathogenesis of daytime sleepiness,2 although sleep apnea can exacerbate the DNS in narcolepsy.
Impulsivity is a feature of actions out of spontaneous impulses without thinking about consequences.4 Impulsivity is a heterogeneous personality and behavioral construct, presenting in the general population and several psychiatric disorders.4,5 It should be noted that greater impulsivity is a known risk factor for the development of addiction and substance abuse.6 Insufficient nocturnal sleep has been associated with poor impulsivity control and emotional dysfunction,7 possibly due to the interaction between sleep deprivation and the lack of inhibitory brain control.8,9 Based on this link, many studies have demonstrated that sleepiness produced by sleep deprivation or fatigue was associated with impulsivity by neuropsychological tasks.10 Another study demonstrated that both poor sleep quality and chronic insomnia were significantly associated with high self-rated impulsivity.11 Pediatric sleep apnea can increase impulsivity and risk-taking behaviors similar to sleep deprivation in children.12,13
Higher prevalence of impulsivity and impaired reward processing have been reported in previously published reports about narcolepsy.14,15 Moreover, some studies found that medication treatment (psychostimulants) might increase the risk of impulsivity even mania in narcolepsy patients.16,17 To further explore the role of daytime sleepiness, sleep apnea and DNS in narcolepsy impulsivity, this study was designed to collect data about sleepiness (questionnaire and polysomnography), sleep apnea and DNS (arousal index, sleep efficiency, sleep stage percentage)1 and other sleep-related parameters in narcolepsy. We hypothesized that daytime sleepiness and other factors, including depression symptoms, onset-age and chronological age, may independently associate with impulsivity in NT1 patients. In addition, among NT1 patients, taking into account the differences in clinical manifestation and severity of illness between adolescents and adults, there may be a nonlinear relationship between chronological age and impulsivity in NT1 patients. Therefore, we performed an analysis to explore other factors associated with impulsivity and the specific relationship between chronological age and impulsivity in NT1 patients.
Methods
Participants
In total, 158 drug-naïve NT1 patients were recruited from the Sleep Medicine Center in Peking University People’s Hospital. The inclusion/exclusion criteria of this study are as follows: 1) all narcolepsy patients were newly diagnosed according to the International Classification of Sleep Disorders −3 (ICSD-3)18: the presence of daytime sleepiness lasting at least 3 months, typical cataplexy, with mean sleep latency ≤8 minutes and 2 or more sleep-onset REM periods (SOREMPs) on the Multiple Sleep Latency Test (MSLT). Or lower levels of orexin (<110pg/mL) in cerebral spinal fluid; 2) all narcolepsy patients did not have any psychostimulants treatment before; 3) all subjects must have normal intelligence and cognitive function; 4) patients with mental disorders (including ADHD) or family history of mental illness and substances/alcohol abuse were excluded; 5) patients with other serious disease or trauma were excluded. Another 42 group-matched on age and gender healthy controls (ranging from 9 to 46 years old, with 8 adolescents and 34 adults) with no known significant healthy and sleep problems were recruited from the community by advertisement. All participants were provided written informed consent, and this study was conducted by the Declaration of Helsinki. This study was approved by the ethics committees of Peking University People’s Hospital.
Polysomnography for Narcolepsy
All NT1 patients underwent one overnight polysomnography (PSG, Respironics LE-Series Physiological Monitoring System, Alice 6 LE, FL, USA) with recording starting from 10 pm to 6 am the next morning. Following the guideline of the American Academy of Sleep Medicine (AASM), the standard electroencephalogram derivations, chin electromyogram, electrooculogram and electrocardiogram were recorded. The oral and nasal airflow, snoring, chest and abdominal breathing, oxygen saturation and body position were also recorded. The PSG recordings were visually scored according to the AASM Manual for Scoring Sleep to every 30-second epoch of the data. The apnea–hypopnea index (AHI) was calculated as the average of the total number of apnea and hypopnea events experienced per hour of sleep. The PLMS index was also recorded as the frequency of PLMS (Periodic leg movement in sleep) per hour of sleep. PLMS was defined and scored using standard criteria from the AASM manual for Scoring Sleep and Associated Events: a series of 4 consecutive leg movements lasting 0.5–5s with an amplitude ≥8μv above the resting baseline and separated by intervals of 5–90s. A leg movement was not scored if it occurred during a period from 0.5s preceding an apnea, hypopnea or respiratory event-related arousal to 0.5s following such an event.
Multiple sleep latency test (MSLT) was performed the next day after the overnight PSG. A total of five naps were scheduled at 2-h intervals. Sleep latency was defined as the time that elapsed from the start of the test to the first 30-second epoch scored as sleep. Each MSLT was ended 20 minutes after the onset of sleep or after 20 minutes of wakefulness. The average sleep latency from the 5 naps was calculated.
Impulsivity Questionnaire
The degree of impulsivity was measured using the Barratt impulse scale (BIS)-11, which is revised by Patton and the most widely used.19 The Chinese version of BIS-1120,21 has been proved to have good reliability and validity in children, adolescents and adults.22,23 The whole scale is composed of 30 items, using a 5-point Likert scale for each item, with a higher total score meaning higher impulsivity. The scale includes three independent subscales: “attentional impulsivity” measures the difficulty in focusing and paying attention on a task, such as attention deficiency, having extraneous thoughts when thinking; “motor impulsivity” measures the tendency to act rashly without any forethought, such as making a decision quickly, lack of perseverance; and “non-planning impulsivity” measures the inability to an adequate plan, such as low self-control.
Depression Symptoms
The Center for Epidemiologic Studies Depression Scale for Children (CES-DC) of Chinese version was used for measuring the depression symptoms in adolescent NT1 patients.24,25 CES-DC is a 20-item scale and there are 4-point response options (0–3 points) for each item. Total scores range from 0 to 60 and higher scores indicate increasing levels of depression symptoms, with a cut-off score ≥20 suggesting depression symptoms.26 The Self-Rating Depression Scale (SDS) was used for assessing the depression symptoms in adult NT1 patients.27 The SDS comprises 20 items. Each item is scored on a 4-point scale, and the total score for each questionnaire is multiplied by 1.25 to convert it into a standardized score, with a cut-off ≥53 suggesting depression symptoms.28
Other Variables
Other variables include demographic variables about age, gender, body mass index (BMI), narcolepsy-related information including age at narcolepsy onset (namely disease onset-age), hypnagogic/hypnopompic hallucinations and sleep paralysis. Excessive daytime sleepiness was measured by the Epworth Sleepiness Score (ESS). Parameters about PSG, including sleep efficiency, percentage of sleep stage (N1+N2, N3, REM), arousal index and mean sleep latency from MSLT, are also involved as other variables.
Statistical Analysis
The continuous variables were expressed as mean ± SD deviation or quartiles and qualitative variables were expressed as frequencies and percentages. We used Χ2 (categorical variables) or two-sample t-test (normal distribution) to test for differences between NT1 patients and healthy controls. Partial correlation analysis was used to detect the relationship between age and total impulsivity score in healthy controls after adjusting for ESS. These statistical tests were performed using SPSS Statistics version 23. The level of significance was set at P<0.05.
Factors Associated with Impulsivity in NT1 Patients
The questionnaire score for depression symptoms was transformed as a binary variable (with or without depression symptoms) according to the cut-off point. Chronological age was transformed as a binary variable (adolescents or adults) according to the cut-off point (age ≥18 as adults and age ≤17 as adolescents). Multiple linear regression with forward stepwise selection was conducted to identify factors associated with total and the subscales impulsivity score in NT1 patients. Variables with P < 0.05 were considered statistically significant. Demographic characteristics such as age, gender, BMI and disease-related information such as disease onset-age, hypnagogic/hypnopompic hallucinations, sleep paralysis, ESS and parameters in PSG were involved as independent variables. The regression statistical analysis was conducted using SPSS Statistics version 23.
Nonlinear Relationship Between Age and Impulsivity in NT1 Patients
We further explored the nonlinear relationship between age and impulsivity scores (total impulsivity score, attentional impulsivity score and non-planning impulsivity score) using generalized additive models (GAM) and smooth curve fitting (penalized splines). If the nonlinear relationship is detected, the inflection point was computed in which the relationship between age and impulsivity scores began to change and became notable using a trial method. The trial inflection point was moved along a predefined interval and detected the inflection point that gave the maximum model likelihood. Then, a piecewise linear regression model was built on both sides of the inflection point. The GAM and smooth curve fitting were performed using R (http://www.R-project.org).
Relationship Between Age and Other Variables in NT1 Patients
To get a better understanding of the nonlinear relationship between age and impulsivity scores in NT1 patients, it is necessary to illustrate how other variables, such as excessive daytime sleepiness, sleep apnea, sleep efficiency and depression, vary with age. GAM and smooth curve fitting were also used to detect the relationship between age and these variables in NT1 patients. The GAM and smooth curve fitting were performed using R (http://www.R-project.org).
Results
Subjects Characteristics
Overall, 158 narcolepsy patients (103 male and 55 female, aged from 5 to 61, with 83 adolescents and 75 adults) were recruited for this study. Among this sample, 46.2% of the patients (n = 73) reported hypnagogic/hypnopompic hallucination, 46.8% of the patients (n = 74) reported sleep paralysis, 36.1% of the patients (n = 57) had sleep apnea (snoring or other symptoms with AHI ≥ 5) comorbidity, and 52.5% of the patients (n = 83) had depression symptoms comorbidity. Moreover, 15.7% of the adolescent NT1 patients had sleep apnea comorbidity, while 58.7% of the adult NT1 patients had sleep apnea comorbidity (P < 0.001). Descriptive analysis of other variables is shown in Table 1.
 |
Table 1 Demographic, Clinical Characteristics and Polysomnography Parameters in NT1 Patients |
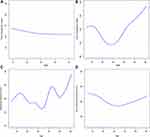
As shown in Table 2, NT1 patients reported higher impulsivity scores in total and three subscales of impulsivity compared with healthy controls. There was a non-significant relationship between age and total impulsivity score in healthy controls after adjusting for ESS (r = −0.151, P = 0.34, Figure 1A).
 |
Table 2 Demographic and Barratt Impulse Scale Score Between NT1 Patients and Healthy Controls |
Factors Associated with Impulsivity in NT1 Patients
Based on multiple linear regression analysis (Table 3), factors associated with higher impulsivity score were higher ESS (P < 0.001), older onset (P = 0.027) and adolescents (P = 0.002). For impulsivity subscales, factors associated with higher attentional impulsivity score (Table 3) were higher ESS (P = 0.016), older onset (P = 0.029) and adolescents (P = 0.001). Factors associated with higher motor impulsivity score (Table 3) were higher ESS (P < 0.001), younger onset (P = 0.014) and depression symptoms (P = 0.011). Factors associated with higher non-planning impulsivity score (Table 3) were adolescents (P = 0.007), older onset (P < 0.001) and depression symptoms (P = 0.026).
 |
Table 3 Multiple Linear Regression Investigating Factors Associated with Total and Subscales Impulsivity in NT1 Patients |
Nonlinear Relationship Between Age and Impulsivity in NT1 Patients
It is speculated that the relationship between age and impulsivity score (total impulsivity score, attentional impulsivity score and non-planning impulsivity score) in narcolepsy patients may be nonlinear, as indicated by the regression results and scatter plot of the relationship between age and impulsivity. The results of multiple linear regression showed that the binarized age variable (adolescents or adults) was statistically significant. This result indicated that there may be a nonlinear relationship between age (as a continuous variable) and impulsivity score for NT1 patients. Through the GAM and smooth curve fitting (adjusting for ESS and disease onset-age), we observed a nonlinear relationship between age and total impulsivity score in NT1 patients (Figure 1B). We also observed a nonlinear relationship between age and attentional or non-planning impulsivity score in NT1 patients (Figure 1C and D).
Relationship Between Age and Other Variables in NT1 Patients
Both ESS and AHI increase gradually with age in NT1 patients (Supplementary Figure S1A and S1B). A nonlinear relationship between age and sleep efficiency or depression was also observed in NT1 patients (Supplementary Figure S1C and S1D).
Discussion
This study evaluated factors associated with impulsivity in drug-naïve NT1 patients: We found that higher ESS, older onset-age and adolescents may have higher total impulsivity score. Comorbid depression symptoms can increase the motor impulsivity score, but decrease the non-planning impulsivity score. Older onset-age can increase both the attentional and non-planning impulsivity score, whereas younger onset-age can increase the motor impulsivity score. A non-linear relationship between age and impulsivity scores (total impulsivity score, attentional impulsivity score and non-planning impulsivity score) was detected. These results support our hypothesis that not only excessive daytime sleepiness but also onset-age, chronological age and depression symptoms exert detrimental effects on drug-naïve NT1’s impulsivity.
A cross-sectional study demonstrated that subjective sleepiness, insomnia, fatigue and modafinil or methylphenidate treatment were associated with hyperactive-impulsive symptoms by questionnaire in pediatric narcolepsy.14 One possible explanation for the connection between narcolepsy and impulsivity is DNS, and impulsivity in ADHD is associated with sleep apnea, restless leg syndrome and periodic limb movement during sleep.29,30 Various studies have indicated that inattention score in attention deficit hyperactivity disorder (ADHD) patients or total BIS score in non-treatment-seeking young adults were associated with ESS,10,31 which linked the hyperactive-impulsive symptoms with sleepiness. Other factors, such as sleep apnea, and periodic limb movement, which have been reported associated with impulsivity in previous studies,29,30 were non-significant on the condition of ESS in the regression model. Considering excessive daytime sleepiness is the main pathology for NT1 patients, which is different from ADHD, sleep apnea or other impulsivity disorders patients, our result emphasized the importance of excessive daytime sleepiness in NT1 patients’ impulsivity. Psychostimulant treatment is another significant factor in NT1 patients’ impulsivity,14 and all NT1 patients in our study were untreated, it is suggested that changes in factors affecting impulsivity before and after psychostimulant treatment are wanted in further research.
However, regression analysis showed that chronological age, rather than sleep apnea or arousal index was associated with total impulsivity score in our NT1 patients. This may be due to the age composition of the populations in this study. There are 52.5% of the adolescents in our NT1 patients, while adolescents had less percentage of sleep apnea comorbidity than adults, and adults have a higher arousal index than adolescents (Table 1). It is suggested that chronological age should be considered as a stratification factor in further studies about NT1 impulsivity. Although age has nothing to do with total impulsivity score in healthy controls, a “U”-shaped relationship between age and total impulsivity score was detected in NT1 patients using GAM and smooth curve fitting, which demonstrated a special and complicated effect of age on NT1 patients’ impulsivity. Non-linear relationship between age and attentional or non-planning impulsivity score was also detected using the same fitting method. A linear decline in self-reported impulsivity between ages 10 and 30 has been reported in healthy controls.32 The linear decline in impulsivity may be associated with brain maturation from adolescence to the 20s that subserve impulse control and self-regulation.33 Improvement in impulsive control continues from childhood to young adulthood. Compared with healthy controls, the non-linear relationship between impulsivity and age suggested brain and mental development alterations in narcolepsy patients. This should be confirmed by further research.
The 30-item BIS has three oblique factors: attentional, motor and non-planning. The attentional impulsivity measures the subject’s toleration for cognitive complexity and persistence, characterized by impatience and lack of flexibility.19 Motor impulsivity measures the subject’s tendency to act on impulse.19 The non-planning impulsivity measures the lack of sense of the future, or hopelessness, even impulsive suicide.19,34 In the subscales analysis of total BIS, linear regression results showed that depression symptoms were associated with both motor and non-planning impulsivity score. Previous reports have demonstrated that these three components of impulsivity in BIS were related differentially to affective state, mania or depression.19,34 Moreover, impulsivity may also be a component of depression.34 In bipolar disorder subjects, it has been suggested that mania contributed to motor impulsivity score, whereas depression contributed to non-planning impulsivity score.34 An epidemiological study found that impulsive suicide, like non-planning impulsivity, tends to be associated with low depression scores.35 In another study about methamphetamine users,36 the results showed that non-planning impulsivity score was a protective factor for severe depression, suggesting a negative relationship between non-planning impulsivity and depression score. This is similar to our results showing that comorbid depression symptoms can reduce the non-planning impulsivity score in NT1 patients. Maybe a questionnaire for mania should be evaluated to further illustrate the relationship between mania and non-planning impulsivity in NT1 patients.
The mechanism underlying the relationship between onset-age and impulsivity score may be attributed to disease duration and neuropsychological development. Younger onset-age can enhance the motor impulsivity score in NT1 patients, a similar result has been reported that younger onset-age can increase the risk of having impulsive-compulsive behaviors in Parkinson’s disease patients.37 It is easier to understand narcolepsy patients with a younger onset-age during development were more vulnerable to sleepiness and other neuropathology in terms of mental behavior, such as impaired motor inhibition, represented by motor impulsivity. While older onset-age was positively associated with attentional and non-planning impulsivity score. However, we could not find a non-linear relationship between onset-age and three components of BIS, and it is difficult to define the cut-off point for “younger” and “older” onset-age. The theory for this positive association is still mysterious. The density curve showed that the distribution of onset-age for NT1 patients in our study is more concentrated in the teen years (Supplementary Figure S2), which is an important period of brain development, hypocretin deficiency in NT1 may impact brain development and maturation via different neurological mechanisms in this period,38 resulting in neuropsychiatric disorders. It is suggested that a more widely distributed onset-age with large-scale and longitudinal observation is necessary for further exploring the relationship between impulsivity score and onset-age in NT1 patients.
Limitations in this study should be mentioned. First, the objective behavioral evaluation for impulsivity should be performed. Second, other factors related to impulsivity symptoms in narcolepsy, especially insomnia and fatigue in previous reports, should be considered and contributed to analyses. Finally, data about impulsivity symptoms should be collected from a larger control population and an epidemiologic survey of NT1 patients. A follow-up study after treatment, such as psychostimulants on narcolepsy and continuous positive airway pressure on sleep apnea, should be conducted to illustrate the effect of psychostimulants and positive airway pressure on impulsivity behavior in NT1 patients.
Conclusion
Not only excessive daytime sleepiness but also onset-age, depression symptoms and chronological age were associated with impulsivity in NT1 patients. Higher ESS, older onset-age and adolescents may have higher total impulsivity score. Comorbid depression symptoms can increase the motor impulsivity score but decrease the non-planning impulsivity score. Older onset-age can increase both the attentional and non-planning impulsivity score, whereas younger onset-age can increase the motor impulsivity score. A non-linear relationship between age and impulsivity score indicated brain and mental development alterations in narcolepsy patients.
Acknowledgments
We thank all the patients for their collaboration.
Funding
This work was supported by the National Natural Science Foundation of China (82070091), International Cooperation and Exchange of the National Natural Science Foundation of China (82020108001), Youth Talent Support Project from China Association for Science and Technology, Project 2020BD028 supported by PKU-Baidu Fund, Beijing Dongcheng District Outstanding Talent Funding Project (DCQYYRC-789-01-DR), Beijing Outstanding Talent Funding Project (2018000021469G235) and Youth Research Funding, Beijing Tiantan Hospital, Capital Medical University (No. 2018-YQN-18).
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Roth T, Dauvilliers Y, Mignot E, et al. Disrupted nighttime sleep in narcolepsy. J Clin Sleep Med. 2013;9:955–965. doi:10.5664/jcsm.3004
2. Rosenberg R, Hirshkowitz M, Rapoport DM, Kryger M. The role of home sleep testing for evaluation of patients with excessive daytime sleepiness: focus on obstructive sleep apnea and narcolepsy. Sleep Med. 2019;56:80–89. doi:10.1016/j.sleep.2019.01.014
3. Sansa G, Iranzo A, Santamaria J. Obstructive sleep apnea in narcolepsy. Sleep Med. 2010;11:93–95. doi:10.1016/j.sleep.2009.02.009
4. Ditrich I, Philipsen A, Matthies S. Borderline personality disorder (BPD) and attention deficit hyperactivity disorder (ADHD) revisited - a review-update on common grounds and subtle distinctions. Borderline Personal Disorder Emotion Dysregulation. 2021;8:22. doi:10.1186/s40479-021-00162-w
5. Khemiri L, Brynte C, Konstenius M, et al. Self-rated impulsivity in healthy individuals, substance use disorder and ADHD: psychometric properties of the Swedish Barratt impulsiveness scale. BMC Psychiatry. 2021;21:458. doi:10.1186/s12888-021-03462-1
6. Blevins D, Choi CJ, Pavlicova M, et al. Impulsiveness as a moderator of amphetamine treatment response for cocaine use disorder among ADHD patients. Drug Alcohol Depend. 2020;213:108082. doi:10.1016/j.drugalcdep.2020.108082
7. Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011;58:649–665. doi:10.1016/j.pcl.2011.03.002
8. Chee MW, Choo WC. Functional imaging of working memory after 24 hr of total sleep deprivation. J Neurosci. 2004;24:4560–4567. doi:10.1523/JNEUROSCI.0007-04.2004
9. Drummond SP, Brown GG, Gillin JC, Stricker JL, Wong EC, Buxton RB. Altered brain response to verbal learning following sleep deprivation. Nature. 2000;403:655–657. doi:10.1038/35001068
10. Grant JE, Chamberlain SR. Sleepiness and impulsivity: findings in non-treatment seeking young adults. J Behav Addictions. 2018;7:737–742. doi:10.1556/2006.7.2018.71
11. Van Veen MM, Karsten J, Lancel M. Poor sleep and its relation to impulsivity in patients with antisocial or borderline personality disorders. Behav Med. 2017;43:218–226. doi:10.1080/08964289.2017.1313719
12. Avis KT, Gamble KL, Schwebel DC. Obstructive sleep apnea syndrome increases pedestrian injury risk in children. J Pediatr. 2015;166:109–114. doi:10.1016/j.jpeds.2014.09.032
13. Fallone G, Acebo C, Arnedt JT, Seifer R, Carskadon MA. Effects of acute sleep restriction on behavior, sustained attention, and response inhibition in children. Percept Mot Skills. 2001;93:213–229. doi:10.2466/pms.2001.93.1.213
14. Lecendreux M, Lavault S, Lopez R, et al. Attention-Deficit/Hyperactivity Disorder (ADHD) symptoms in pediatric narcolepsy: a cross-sectional study. Sleep. 2015;38:1285–1295. doi:10.5665/sleep.4910
15. Kim J, Lee GH, Sung SM, Jung DS, Pak K. Prevalence of attention deficit hyperactivity disorder symptoms in narcolepsy: a systematic review. Sleep Med. 2020;65:84–88. doi:10.1016/j.sleep.2019.07.022
16. Tarrant N, Cavanna AE, Rickards H. Pathological gambling associated with modafinil. J Neuropsychiatry Clin Neurosci. 2010;22:123 E27–8. doi:10.1176/jnp.2010.22.1.123.e27
17. Crosby MI, Bradshaw DA, McLay RN. Severe mania complicating treatment of narcolepsy with cataplexy. J Clin Sleep Med. 2011;7:214–216. doi:10.5664/jcsm.28112
18. American Academy of Sleep Medicine. The International Classification of Sleep Disorders.
19. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–774. doi:10.1002/1097-4679(199511)51:6<768::AID-JCLP2270510607>3.0.CO;2-1
20. Lu CF, Jia CX, Xu AQ, Dai AY, Qin P. Psychometric characteristics of Chinese version of Barratt Impulsiveness Scale-11 in suicides and living controls of rural China. Omega. 2012;66:215–229. doi:10.2190/OM.66.3.b
21. Liu Y, Liu N, Shen W, Li L, Zhou W, Xu L. The abuse characteristics of amphetamine-type stimulants in patients receiving methadone maintenance treatment and buprenorphine maintenance treatment. Drug Des Devel Ther. 2021;15:2109–2116. doi:10.2147/DDDT.S305226
22. Wang Q, Wang Y, Zuo J, et al. Factors of negative affect in elderly patients with substance use disorders during COVID-19 pandemic. Front Psychiatry. 2021;12:697472. doi:10.3389/fpsyt.2021.697472
23. Yu C, Zhang J, Zuo X, Lian Q, Tu X, Lou C. Correlations of impulsivity and aggressive behaviours among adolescents in Shanghai, China using bioecological model: cross-sectional data from Global Early Adolescent Study. BMJ Open. 2021;11:e043785. doi:10.1136/bmjopen-2020-043785
24. Li HC, Chung OK, Ho KY. Center for epidemiologic studies depression scale for children: psychometric testing of the Chinese version. J Adv Nurs. 2010;66:2582–2591. doi:10.1111/j.1365-2648.2010.05440.x
25. Zhao Z, Ding N, Song S, Liu Y, Wen D. Association between depression and overweight in Chinese adolescents: a cross-sectional study. BMJ Open. 2019;9:e024177. doi:10.1136/bmjopen-2018-024177
26. Yang Y, Li C, Zhao L, Li J, Han F, Xiao F. Factors associated with depression and sub-dimension symptoms in adolescent narcolepsy. Nat Sci Sleep. 2021;13:1075–1082. doi:10.2147/NSS.S312000
27. Jokelainen J, Timonen M, Keinänen-Kiukaanniemi S, Härkönen P, Jurvelin H, Suija K. Validation of the Zung self-rating depression scale (SDS) in older adults. Scand J Prim Health Care. 2019;37:353–357. doi:10.1080/02813432.2019.1639923
28. Dunstan DA, Scott N. Clarification of the cut-off score for Zung’s self-rating depression scale. BMC Psychiatry. 2019;19. doi:10.1186/s12888-019-2161-0
29. Youssef NA, Ege M, Angly SS, Strauss JL, Marx CE. Is obstructive sleep apnea associated with ADHD? Ann Clin Psychiatry. 2011;23:213–224.
30. Picchietti DL, England SJ, Walters AS, Willis K, Verrico T. Periodic limb movement disorder and restless legs syndrome in children with attention-deficit hyperactivity disorder. J Child Neurol. 1998;13:588–594. doi:10.1177/088307389801301202
31. Oosterloo M, Lammers GJ, Overeem S, de Noord I, Kooij JJ. Possible confusion between primary hypersomnia and adult attention-deficit/hyperactivity disorder. Psychiatry Res. 2006;143:293–297. doi:10.1016/j.psychres.2006.02.009
32. Steinberg L, Albert D, Cauffman E, Banich M, Graham S, Woolard J. Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: evidence for a dual systems model. Dev Psychol. 2008;44:1764–1778. doi:10.1037/a0012955
33. Paus T. Mapping brain maturation and cognitive development during adolescence. Trends Cogn Sci. 2005;9:60–68. doi:10.1016/j.tics.2004.12.008
34. Swann AC, Steinberg JL, Lijffijt M, Moeller FG. Impulsivity: differential relationship to depression and mania in bipolar disorder. J Affect Disord. 2008;106:241–248. doi:10.1016/j.jad.2007.07.011
35. Simon OR, Swann AC, Powell KE, Potter LB, Kresnow MJ, O’Carroll PW. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2001;32:49–59. doi:10.1521/suli.32.1.5.49.24212
36. Luo D, Tan L, Shen D, et al. Characteristics of depression, anxiety, impulsivity, and aggression among various types of drug users and factors for developing severe depression: a cross-sectional study. BMC Psychiatry. 2022;22:274. doi:10.1186/s12888-022-03933-z
37. Cao L, Xu T, Zhao G, Lv D, Lu J, Zhao G. Risk factors of impulsive-compulsive behaviors in PD patients: a meta-analysis. J Neurol. 2022;269(3):1298–1315. doi:10.1007/s00415-021-10724-1
38. Stoyanova II, Rutten WLC, le Feber J. Orexin-A and Orexin-B during the postnatal development of the rat brain. Cell Mol Neurobiol. 2009;30:81–89. doi:10.1007/s10571-009-9433-z
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.