Back to Journals » Infection and Drug Resistance » Volume 15
Nomogram Prediction Model of Serum Chloride and Sodium Ions on the Risk of Acute Kidney Injury in Critically Ill Patients
Authors Lu J , Qi Z , Liu J, Liu P , Li T, Duan M , Li A
Received 1 June 2022
Accepted for publication 17 August 2022
Published 24 August 2022 Volume 2022:15 Pages 4785—4798
DOI https://doi.org/10.2147/IDR.S376168
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Jiaqi Lu,1 Zhili Qi,2 Jingyuan Liu,1 Pei Liu,2 Tian Li,2 Meili Duan,2 Ang Li3
1Department of Critical Care Medicine, Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Critical Care Medicine, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China; 3Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Meili Duan, Department of Critical Care Medicine, Beijing Friendship Hospital, Capital Medical University, No. 95 Yong’an Road, Xicheng District, Beijing, 10005, People’s Republic of China, Email [email protected] Ang Li, Beijing Ditan Hospital, Capital Medical University, #8 Jing Shun East St, Chaoyang, Beijing, 100015, People’s Republic of China, Email [email protected]
Purpose: This study aims to investigate the effect of serum chloride and sodium ions on AKI occurrence in ICU patients, and further constructs a prediction model containing these factors to explore the predictive value of these ions in AKI.
Methods: The clinical information of patients admitted to ICU of Beijing Friendship Hospital Affiliated to Capital Medical University was collected for retrospective analysis. Logistic regression analysis was used to analyzing the influencing factors. A nomogram for predicting AKI risk was constructed with R software and validated by repeated sampling. Afterwards, the effectiveness and accuracy of the model were tested and evaluated.
Results: A total of 446 cases met the requirements of this study, of which 178 developed AKI during their stay in ICU, with an incidence rate of 39.9%. Hypernatremia, heart failure, sepsis, APACHE II score, and initial creatinine value and BE value at ICU admission before the diagnosis of AKI were identified as independent risk factors for developing AKI during ICU stay. These predictors were incorporated into the nomogram of AKI risk in critically ill patients, which was constructed by using R software. Receiver operating characteristic curve analysis was further used and showed that the area under the curve of the model was 0.7934 (95% CI 0.742– 0.8447), indicating that the model had an ideal value. Finally, further evaluated its clinical effectiveness. The clinical effect curve and decision curve showed that most areas of the decision curve of this model were greater than 0, indicating that this model owned a certain clinical effectiveness.
Conclusion: The nomogram based on hypernatremia, heart failure, sepsis, APACHE II score, and initial creatinine and BE value in ICU can predict the individualized risk of AKI with satisfactory distinguishability and accuracy.
Keywords: intensive care unit, acute kidney injury, hypernatremia, hyperchloremia
Introduction
Acute kidney injury (AKI) is a common complication in hospitalized patients, especially in the intensive care unit (ICU).1 The number of the patients who developed AKI accounts for 37% among all the ICU patients.2 More than 13 million patients suffer from AKI worldwide every year, and 1.7 million die from it.3,4 AKI is associated with prolonged hospital stay, increased hospitalization costs, high morbidity and mortality.5 Especially for patients with AKI at stage 2–3, the in-hospital mortality rate is 47%, the 1-year survival rate is only 77%, and there is no improvement within 7 days.6 Although advances have been made in modern diagnostic approaches, the limitations in specificity and sensitivity have slowed down the progress in research and clinical applications. Therefore, the clinical outcome of patients can be remarkably improved by identifying high-risk factors for AKI to prevent the prevalence, diagnosing AKI at an early stage and appropriate clinical intervention.7
Electrolyte disturbance is common in hospitalized patients8 and more common in ICU patients.9 Serum sodium ion (Na +) imbalance often occurs in hospitalized patients.10 Abnormal sodium metabolism (including hyponatremia [sodium <135 mmol/L] and hypernatremia [sodium >145 mmol/L] was reported to be found in approximately 30–40% of all hospitalized patients.11 Hypernatremia (Na+>145 mmol/L)) is one of a dominant type of electrolyte disturbance in critically ill patients.12,13 In clinical practice, hypernatremia is a common and potentially life-threatening disease. It was found that 9% of ICU patients could develop hypernatremia.14 Hypernatremia can also be observed in patients with COVID-1915 and is considered as an important indicator for COVID-19.16 Hypernatremia may result in peripheral insulin resistance, hepatic gluconeogenesis disorders, neuropsychiatric disorders, cardiac systolic dysfunction, etc. If not treated in time, hypernatremia will bring multiple problems to patients and even increase mortality.17 Recently, accumulating evidence attached the importance to the relationship between sodium balance and renal function,18–20 some studies believed that abnormal sodium metabolism is a predictor for AKI.21,22 However, only a limited number of studies have focused on hypernatremia. Therefore, we assessed the predictive effect of hypernatremia on AKI in critically ill patients.
As an electrolyte easily neglected, chloride ion is often regarded as a passive partner for sodium ion.23 However, chloride itself is a potent bioactive electrolyte and the main anion in extracellular fluid, playing an important role in regulating acid-base balance, osmotic pressure and water distribution.24 Some studies found that serum chloride ions participate in the function of regulatory T cells, which in turn influences the immune system.25 In ICU, the main source of chloride ions is intravenous fluid infusion, and the main excretion route is urine via kidneys. Fluid resuscitation is a common therapeutic approach used in ICU patients; however, there is no fluid completely same as physiologic fluid. The amount of chloride ions in many commonly used fluids is more than that of the physiologic fluid. For example, 0.9% NaCl solution is often used as the first choice for rehydration therapy and the concentration of chloride ion in it is 154 mmol/L. However, the concentration of chloride ion in normal plasma is 99–110 mmol/L, in other words, the concentration of chloride ion in normal saline is nearly 50% higher than that in plasma. In recent years, increasing studies have demonstrated that rapid infusion of large amounts of crystalloid solution rich in chloride as resuscitation fluid for critically ill patients could contribute to hyperchloremic metabolic acidosis. Hyperchloremia is associated with poor clinical outcomes, especially nephrotoxic effect.26–28 Studies have shown that in critically ill patients, limiting the infusion of fluids rich in chloride could decrease AKI incidence, and a majority of patients infused with normal saline had higher peak level of serum chloride, elevated blood chloride level, and increased incidence of metabolic syndrome.29 Other research demonstrated that after ICU admission, higher average concentration of chloride ion and the maximum concentration were associated with the occurrence of AKI, suggesting that the load of chloride ion during ICU treatment might increase the risk of AKI. At the same time, it was also observed that after ICU admission, higher minimum concentration of chloride ion had a protective effect on AKI.30 Therefore, there might be a significant biological correlation between hyperchloremia and AKI.
Because substantial human resources are required to assess and treat AKI, the current capacity for detailed assessment and monitoring of AKI development is limited.31 Recent studies have reported several AKI risk prediction models in different clinical settings. Representative are risk prediction models for acute kidney injury in the intensive care setting,32 after surgery33 and induced by contrast media.34 To get an accurate prediction model, it is often necessary to select appropriate predictors. Predictors from most previous models including baseline information, baseline renal function or other biomarkers, history of comorbidities, and medication use predicted the likelihood of a patient developing AKI.35 Acute kidney injury is associated with metabolic acidosis, volume overload, electrolyte imbalance, and other complications. But we found fewer electrolyte factors to be incorporated in most prediction models, with the highest focus on sodium ions;36–45 Some studies have reported potassium ions,40–42,45 but few have investigated the role of chloride ions in the model, only individual studies have explored the case of chloride ions,44 but the results are still controversial. Therefore, the efficacy of sodium and chloride ions in the serum for predicting the risk of AKI occurrence in the ICU is uncertain. The main purpose of this study is to explore the value of serum chloride and sodium ions in predicting the risk of ICU AKI and to further refine the predictors that can be used for early AKI diagnosis in adult ICUs, helping to identify those at high risk of AKI in the ICU by investigating the high-risk factors for AKI and perform early interventions for high-risk patients to improve quality of life.
Patients and Methods
Patient Information
This retrospective study included all the patients (n = 2087) admitted to the Department of Critical Care Medicine of Beijing Friendship Hospital from January 1, 2017 to December 31, 2018. If the patient was admitted to ICU for multiple times during the study period, only the first admission into ICU was included. Inclusion criteria: ① age of the patient on the admission into ICU > 18 years old; ② ICU stay >48 hours. Exclusion criteria: ①post kidney transplantation; ②patients had regular dialysis for a long term; ③pregnant women; ④chronic renal insufficiency; ⑤lack of clinical data during ICU. This study was conducted in accordance with the Declaration of Helsinki. This study was approved by the Bioethics Professional Committee of Beijing Friendship Hospital of Capital Medical University (No. 2022-P2-082-01). As this study was a study utilizing medical record information obtained from previous clinical encounters, we applied for waiver of informed consent and ethics committee consent was obtained. Throughout the study, we respected patient privacy and ensured that data information was kept confidential.
Definition and Diagnostic Criteria
The diagnostic criteria and systemic classification defined in the Kidney Disease: Improving Global Outcomes (KDIGO) was used for diagnosing AKI46,47 and the specific criteria were as follows: the increase of serum creatinine ≥0.3 mg/dl (>26.5 µmol/l) within 48 hours; or the increase of serum creatinine ≥1.5 times the baseline value, which was known or presumed to occur within 7 days; or urine output <0.5mL/kg/h for 6 hours. Basal creatinine value is defined as the lowest creatinine value before admission. If there was a lack of relevant data before admission, creatinine value could be estimated by the standard creatinine formula. Sepsis is a kind of life-threatening dysfunction in organs caused by dysregulated responses to infection and the diagnostic criteria are as follows: patients with infection or suspected infection; SOFA score ≥2 points or the change of SOFA score ≥2 points.48 The diagnostic criteria for ICU readmission are as follows: if the patient is admitted to the ICU more than once during the study period, only the condition at the first admission to ICU is taken into account. Hypernatremia is defined as serum sodium concentration greater than 145 mmol/L, hyponatremia is defined as sodium ion concentration less than 135 mmol/L, and normal serum sodium concentration is 135–145 mmol/L. Hyperchloremia is defined as serum chloride concentration higher than 110 mmol/L, and normal serum chloride concentration is 99–110 mmol/L. Hyperlactatemia was defined as serum lactate value >2mmol/L. These definitions were based on the standard values of serum sodium and chloride ions provided by the Biochemical Laboratory of Friendship Hospital.
Data Collection
This study was approved by the Ethics Committee of Beijing Friendship Hospital Affiliated to Capital Medical University. We reviewed and collected the demographics, clinical characteristics and laboratory results of critically ill patients admitted to ICU in Beijing Friendship Hospital Affiliated to Capital Medical University from January 1, 2017 to December 31, 2018. According to the inclusion and exclusion criteria and the purposes of our study, a CRF (Case Report Forum) was created. We logged in the medical electronic information system to collect the following information of the research subjects who have met the inclusion criteria according to CRF-related content: patient basic information (age, gender), department (emergency, internal medicine, or surgery department), underlying diseases (hypertension, diabetes, coronary heart disease, heart failure, liver disease, tumor, blood system disease, etc.), surgery history, complete blood count and biochemical indicators, serum chloride ion and sodium ion-related indicators (maximum chloride and sodium ion level in patients before the diagnosis of AKI), APACHE II score, initial creatinine and BE values on admission to ICU, blood lactate value, etc. The outcome index was confirmed diagnosis of AKI during ICU stay. Missing data for variables in this study were all <5%. Missing data were handled with a simple imputation method that replaced missing data with the median of the cohort patients. There were no missing data in the diagnostic and procedural information.
Construction, Validation and Evaluation of the Prediction Models
The data is divided into training set and validation set at the ratio of 7:3. The training set was used for establishing the model. Continuous variables with normal distribution were expressed as mean ± standard deviation, and those with skewed distribution were expressed as median and interquartile range. If the two independent samples conformed to a normal distribution and the hypothesis in homogeneity of variance test was satisfied, the differences were compared using independent sample t-test. The chi-square test or Fisher’s exact test was used to determine whether there was a difference in overall rates and the constituent ratios between the two groups.
In order to establish a well-calibrated nomogram to predict outcomes, univariate and multivariate logistic regression analyses were conducted to screen predictors. The variables with P < 0.1 in univariate analysis were subjected to multivariate stepwise logistic regression.49 A nomogram prediction model based on independent risk factors was established by using R. The model is then validated and evaluated. First, the area under the receiver operating characteristic (ROC) curve (AUC) was used to assess the accuracy of the model. Second, repeated sampling verification was carried out for 1000 times, the calibration curve was plotted, and the correlation between the calibration curve and the standard curve was verified and evaluated.50 Finally, the clinical validity of the model was evaluated by clinical impact curve and decision curve analysis. Difference with P < 0.05 was considered as statistically significant.
IBM SPSS Statistics 24.0 (IBM Corporation, Armonk, New York, USA) and R version 3.3.3 (The R Foundation for Statistical Computing, Austria, and Vienna) were used as the analysis software in this study.
Results
Patient Characteristics
In this study, we reviewed the data from 2087 critically ill patients in ICU, and 895 patients met the inclusion criteria who were older than 18 years and stayed in ICU for more than 48 hours. According to the exclusion criteria, 449 patients did not meet the inclusion criteria and thus were excluded. Among them, 46 patients were excluded because of a kidney transplantation history before they were admitted to ICU; 272 patients were excluded because of a confirmed history of chronic renal insufficiency before admission to ICU; 104 patients were excluded because they received regular renal replacement therapy before admission to ICU; 24 patients were excluded because of pregnancy on the admission to ICU; 3 patients were excluded because of a lack of clinical data during ICU stay. Finally, 446 cases were included in this study. The research flow chart is shown in Figure 1, includes a training cohort (n = 312) and a validation cohort (n = 134). Of these patients, 178 (39.9%) developed AKI during their stay in the ICU. AKI prevalence accounted for 39.1% and 41.8% in the training and validation cohorts, respectively. Afterwards, we summarized the demographic and clinical characteristics of the training cohort (Table 1 and Figure 1).
 |
Table 1 Patients and Disease Characteristics |
 |
Figure 1 Study design. A total of 446 ICU patients with complete relevant data were enrolled in this study. |
A total of 22 clinical variables were analyzed (Table 1). The analysis of 312 patients in the training cohort revealed that 179 cases (57.4%) were male. The age of the patients was 60.9±16.9 years. Although the average age of the patients in the AKI group was higher than that in the non-AKI group (62.1±17.2 vs 60.1±16.7 years), the difference was not statistically significant (p = 0.314). The highest level of sodium ion in the AKI group was higher than that in the non-AKI group from the time of admission to the diagnosis of AKI (140.5±6.6 VS 139.6±4.6 mmol/L, p = 0.193). Through analyzing hypernatremia in the patients, it was shown that the incidence of hypernatremia in the AKI group was significantly higher than that in the non-AKI group (13.1 VS 6.3%) from the time of admission to the diagnosis of AKI, with a statistically significant difference (p = 0.04). However, there was no significant difference in chloride ion and hyperchloremia between the two groups (p > 0.05). Other results can be found in Table 1.
Predictors of AKI in Critically Ill Patients
The results of univariate and multivariate logistic regression analysis in the training cohort are shown in Table 2. Statistically significant variables were selected to conduct univariate binary logistic regression analysis. Statistically significant variables were further subjected to multivariate logistic regression analysis, and ultimately the variables were introduced into the prediction model. Through univariate analysis, 9 variables were found: hypernatremia before diagnosis of AKI, patients transferred from internal medicine department to ICU, diabetes mellitus, heart failure, sepsis, APACHE II score, initial creatinine value on admission to ICU, initial BE value on admission to ICU, hyperlactatemia on admission to ICU. There were significant differences in these values between AKI and non-AKI group (Table 1). In univariate analysis, there was no linear relationship among the 9 variables. These 9 variables were further subjected to multivariate logistic regression analysis using forward LR method. Hypernatremia, heart failure, sepsis, APACHE II score, initial creatinine value on admission to ICU, and initial BE value on admission to ICU were independent risk factors (Table 2). The results showed that patients with hypernatremia were more likely to develop AKI than those without hypernatremia (P = 0.011; OR 3.033, 95% CI 1.286–7.154). Patients with heart failure were more likely to develop AKI than those without heart failure (P = 0.042; OR 3.454, 95% CI 1.044–11.422). Similarly, patients with sepsis were more likely to have AKI than those without sepsis (P < 0.001; OR 3.008, 95% CI 1.703–5.312). As known to us, patients with high APACHE II scores were more likely to develop AKI than those with low scores (P = 0.001; OR 1.088, 95% CI 1.038–1.141). Patients with high initial creatinine value on admission to ICU were more likely to have AKI than those with low value (P = 0.053; OR 1.014, 95% CI 1.000–1.028), which was also included in the prediction model. Furthermore, the lower the initial BE value on admission to ICU was, the more likely the patients might have AKI (P < 0.001; OR 0.879, 95% CI 0.825–0.935).
 |
Table 2 Univariate and Multivariate Analyses of Predictors for AKI |
Before constructing the model, we included hyperchloremia in the model and performed net reclassification index and clinical discriminant index analysis (Figure 2). The result showed that p = 0.248 in the comprehensive discriminant index, indicating that there was no significance in including hyperchloremia in the model. Therefore, hyperchloremia was not included in the model. The analysis on the factors mentioned above further confirmed that hypernatremia, heart failure, sepsis, APACHE II score, initial creatinine value on the admission to ICU, and initial BE value on the admission to ICU could be used as independent risk predictors for AKI in critically ill patients. Except for hypernatremia, theses predictors were included in the nomogram which was plotted by R software (Figure 3).
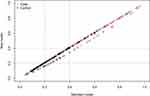 |
Figure 2 Net reclassification index. |
 |
Figure 3 Nomogram to predict the outcomes of AKI. Abbreviations: CHF, congestive heart failure; APACHE, Acute Physiology and Chronic Health Evaluation; BE, base excess. |
Determination of the Critical Value for Predicting AKI
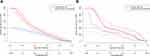
After constructing the model, we used the area under the ROC curve (AUC) to analyze the accuracy of the model. The internal and external validation of the nomogram by ROC analysis was conducted by using the training cohort (Figure 4A) and validation cohort (Figure 4B), respectively. In the internal validation, the AUC value of ROC curve was 0.7934 (95% CI 0.742–0.8447). In the external validation, the AUC value of ROC curve was 0.7649 (95% CI 0.6793–0.8505), indicating that the model showed an ideal value. To further verify the validity of the model, a calibration curve was established using R (Figure 5). The calibration of the nomogram was performed internally by using the training cohort (Figure 5A) and externally by using the validation cohort (Figure 5B). An acceptable goodness of fit was demonstrated in the calibration curve of the model relative to the standard ideal curve. This was an ideal situation in which the probability of occurrence predicted by the corresponding model was exactly the same as the actual probability of occurrence. The calibration plot (n = 1000) was plotted by using repeated sampling method to verify and evaluate the correlation between the calibration curve and the standard curve, which further presented that the model had satisfactory fitting validity and predictive value. Finally, to further assess its clinical validity, the clinical impact curve (Figure 6) and decision curve (Figure 7) were plotted by using R. Most parts of the decision curve were greater than 0, indicating that there was clinical validity. These results suggested that all models had certain predictive value.
 |
Figure 5 Calibration of the nomogram to predict the AKI in the training dataset (A) and validation dataset (B). |
Discussion
Acute kidney injury is a complicated clinical syndrome characterized by a sudden decline in renal function. AKI is defined as an increase in creatinine level (absolute or relative) or a decrease in urine output.51 It is one of the relatively critical conditions in hospitalization, which is associated with poor prognosis and increased burden to patient.52,53 The mortality rate of patients with AKI is as high as 60–70%, especially within 1 year after ICU admission.54 In addition, survivors of acute kidney injury have an increased risk of decreased renal function and end-stage renal disease.55,56 Water and electrolyte disorders often occur in hospitalized patients.57 Particularly, hyperchloremia and hypernatremia were frequently observed in hospitalized patients. The relationship between AKI and serum chloride and sodium ions currently attracts much attention and may be associated with kidney injury.18–21,58–61 The mechanism may be that hypernatremia and hyperchloremia contribute to renal vasoconstriction, resulting in decreased glomerular filtration rate and decreased renal function.62,63 Early detection and diagnosis of AKI is a great challenge for physicians in critical care department.64 Therefore, identifying clinical predictors for the risk of AKI may improve the prognosis. This study focused on predicting the risk of developing AKI and also included the analysis of clinical indicators. However, considering the heterogeneity of AKI, the accuracy of using univariate prediction is limited. Thus, we tried to use a multivariate model to predict the risk of AKI. A nomogram was constructed to predict AKI and was validated by applying an external cohort.
Hypernatremia is a common condition in clinical practice. There were numerous studies on the negative effects of hypernatremia on patients in internal medicine or surgical departments.65–67 The effects of hypernatremia on patients in the intensive care unit gained increasing attention.60,68–70 Studies of sodium disturbances in ICU mainly focused on hypernatremia, since hypernatremia in critically ill patients usually occurred after admission rather than on the admission to the hospital.65,66 Hypernatremia is primarily resulted from lack of water, which is caused by reduced intake or excessive loss.14 Generally, hypernatremia tends to occur in weak patients at an advanced age due to a reduced sensation of thirst and impaired ability to drink. Besides, the function of kidneys in urinary concentration is deteriorated as age increases.57 Hypernatremia is commonly found in ICU. As reported in a study, hypernatremia occurred in 9% of the adults admitted to ICU.66 Some studies believed that hypernatremia is an iatrogenic disease as it often occurs in hospitalized patients.13,71 Via intravascular dehydration and vasoconstriction mechanisms, hypernatremia can induce renal dysfunction in a direct way or through glomerular feedback mechanisms.72 In-vivo studies have shown that when the sodium level in renal arteries rapidly elevated, the renal blood flow and glomerular filtration rate decreased, and renin secretion was inhibited.62 These findings can be explained by the fact that, unlike other organs, high level of sodium induces vasoconstriction in the kidneys. Severe hypernatremia is associated with reduced cardiac function, insulin resistance, impaired lactate clearance in liver, neuromuscular impairment, and cognitive impairment.17,73 In previous studies by our research group, it was also confirmed that hypernatremia in sepsis patients was independently associated with an increased risk of AKI and could be used to predict AKI.69 Studies have shown that there was a strong and independent association between the risk of AKI and hypernatremia and elevated level of serum sodium.74 This study presented that 1450 (2.5%) patients among 1541 patients had AKI during the annual follow-up, of which 588 (40.4%) had pre-existing hypernatremia (on admission or during hospitalization). From this perspective, since serum creatinine shows a poor sensitivity to renal damage, higher fluctuation in sodium concentration may indicate that renal function is worsening.
Hyperchloremia is a commonly occurred electrolyte disturbance. The incidence of hyperchloremia during hospitalization has been reported to vary in a wide range, from nearly 20–90%.75–77 In the latest and largest retrospective observational study of critically ill patients, 57% of the study subjects developed hyperchloremia within 48 hours of ICU admission.76 The results of this study indicated that hyperchloremia was not associated with the occurrence of AKI, which was similar to the results of previous studies. As demonstrated by a retrospective study, there was no significant association between elevated serum chloride concentration and the occurrence of AKI after assessing the data of the patients with ST-segment elevation myocardial infarction on their admission to the hospital.78 Recently, a large randomized trial compared the effect of chloride-limited lactated Ringer’s solution and 0.9% normal saline on AKI or mortality in ICU patients and no significant difference was found.79 Yessayan et al conducted a retrospective study analyzing 1045 patients with septic shock. They found that there was no association between hyperchloremia and AKI within the first 72 hours of ICU admission.80 On the other hand, this result was contrary to that in some previous studies. Previous studies have presented that hyperchloremia was associated with AKI in patients with non-cardiac surgery,75 subarachnoid hemorrhage,81 sepsis or septic shock,29 and abdominal surgery.82 The study by McCluskey et al75 found that hyperchloremia was a risk factor for acute kidney injury in critically ill patients after non-cardiac surgery. However, McCluskey et al used the stratified diagnostic criteria of RIFLE in diagnosing AKI, while we used KDIGO diagnostic criteria in diagnosing AKI.
Extensive data can be collected from the ICU. Typically, massive data can be obtained from critically ill patients through continuous monitoring of vital signs, treatment equipment, radiological imaging, and a range of laboratory measurements. AKI risk prediction models facilitate medical decision-making when critically ill patients are admitted to the ICU and facilitate early identification or implementation of preventive measures to improve the prognosis of AKI. Multiple studies have also previously reported prediction models for AKI in different clinical settings. The study by Malhotra et al83 ultimately identified 10 clinical variables for externally validated AKI risk prediction models in the ICU, but this study did not investigate electrolyte-related metrics among the initial variables. Flechet et al84 developed an online risk calculator for AKI in ICU patients (http://akipredictor.com/), but information on patients’ electrolytes was not considered in these metrics. In a study of patients undergoing cardiac surgery, a prediction model for AKI based on perioperative basic metabolic laboratory values showed that the indicators ultimately included in the model were perioperative blood creatinine and postoperative changes in blood urea nitrogen, serum sodium, potassium, bicarbonate, and albumin.36 This study confirmed the predictive power of electrolyte imbalance for AKI, but this study did not specify the effect of hypernatremia on AKI and did not address chloride-related parameters. In the predictive model for the development of AKI after orthotopic liver transplantation, the analysis showed that the MELD Na score had potential predictive value for patients who developed AKI postoperatively.38 The model for end-stage liver disease (MELD), with multiple scoring systems derived from it, is currently a widely used liver failure evaluation system in the clinic, and studies have shown that the addition of serum sodium to meld can significantly improve the accuracy of predicting survival, so the MELD Na scoring model was proposed.85 Furthermore, a study of postoperative AKI prediction in noncardiac surgery showed that gender, EGFR, anemia, hypoalbuminemia, and proteinuria were significantly associated with AKI, but age, diabetes mellitus, expected operation time, emergency surgery, RAAS blocker use, and hyponatremia were not associated with postoperative AKI.37 Only hyponatremia was focused on in this study, and the effects of hypernatremia, as well as chloride ions, were not elucidated. A prediction model for sepsis-associated AKI that also accounted for electrolyte derangement included sodium, chloride, and potassium, but these last indicators were incorporated into the model.44
There were also some Significance of this study: This is a study with internal validation. In our study, the logistic model was chosen because clinicians were more familiar with its method and interpretation. In addition, the data collection was in a comprehensive type of critical care medicine department and was not limited to surgery or which kind of critically ill patient was specific. In addition, the choice of variables in the model, both routine as well as easily accessible indicators in clinical practice, was not incorporated into novel assays. During the construction of the model, we took into account the effect of electrolyte disturbance on AKI and conducted further studies. Meanwhile, we focused our analysis on the effect of chloride ion on AKI, because, in a clinic, chloride ion is usually our nearly forgotten electrolyte. Finally, when describing the electrolytes, we have also specifically refined the contribution of sodium as well as chloride disturbances of varying severity to AKI, eg, hypernatremia and hyperchloremia. limitations in our study. First, this study was a retrospective study, which tended to generate selection bias. The evidence level was relatively weaker compared with RCT studies. Second, the study was a single-center study. It was more likely to make misleading results compared with multi-center study, which limited the universality of the results. Finally, the number of studies included in this study was relatively small (n = 446). Although the biases and confounding factors were controlled at the most extent by using multivariate models, there still might be other known or unknown influencing factors. Thus, further experiments are required to verify the current findings.
Conclusion
The nomogram we constructed confirmed that patients with hypernatremia, heart failure, sepsis, high initial APACHE II score and creatinine value on ICU admission, and low initial BE value on ICU admission were more likely to develop AKI during their stay in the ICU compared with other patients. Therefore, by constructing an individualized prediction model, intervention could be provided for the patients with hypernatremia in advance. Once the patients with high risk are screened out, and the risk level of developing AKI is reached, intervention can be provided in advance.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article or are available from the corresponding author on reasonable request.
Ethics Approval
This study was approved by the Professional Committee on bioethics of Beijing Friendship Hospital (No. 2022-P2-082-01). Individual consent was waived for this retrospective analysis.
Acknowledgments
The authors would like to thank the database search support provided by Beijing Friendship Hospital affiliated with Capital Medical University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study did not receive any specific funding from funding agencies in the public, commercial or non-profit sectors.
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Thalji SZ, Kothari AN, Kuo PC, Mosier MJ. Acute kidney injury in burn patients: clinically significant over the initial hospitalization and 1 year after injury: an original retrospective cohort study. Ann Surg. 2017;266(2):376–382. doi:10.1097/SLA.0000000000001979
2. Calderon-Margalit R, Golan E, Twig G, et al. History of childhood kidney disease and risk of adult end-stage renal disease. N Engl J Med. 2018;378(5):428–438. doi:10.1056/NEJMoa1700993
3. Lameire NH, Bagga A, Cruz D, et al. Acute kidney injury: an increasing global concern. Lancet. 2013;382(9887):170–179. doi:10.1016/S0140-6736(13)60647-9
4. Lewington AJ, Cerdá J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 2013;84(3):457–467. doi:10.1038/ki.2013.153
5. Abd ElHafeez S, Tripepi G, Quinn R, et al. Risk, predictors, and outcomes of acute kidney injury in patients admitted to intensive care units in Egypt. Sci Rep. 2017;7(1):17163. doi:10.1038/s41598-017-17264-7
6. Peerapornratana S, Manrique-Caballero CL, Gómez H, Kellum JA. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney Int. 2019;96(5):1083–1099. doi:10.1016/j.kint.2019.05.026
7. Farrar A. Acute Kidney Injury. Nurs Clin North Am. 2018;53(4):499–510. doi:10.1016/j.cnur.2018.07.001
8. Funk GC, Lindner G, Druml W, et al. Incidence and prognosis of dysnatremias present on ICU admission. Intensive Care Med. 2010;36(2):304–311. doi:10.1007/s00134-009-1692-0
9. Yessayan LT, Szamosfalvi B, Rosner MH. Management of dysnatremias with continuous renal replacement therapy. Semin Dial. 2021;34(6):472–479. doi:10.1111/sdi.12983
10. Spasovski G, Vanholder R, Allolio B, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014;170(3):G1–47. doi:10.1530/EJE-13-1020
11. Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006;119(7 Suppl 1):S30–35. doi:10.1016/j.amjmed.2006.05.005
12. Collins NM, Carrick JB, Russell CM, Axon JE. Hypernatraemia in 39 hospitalised foals: clinical findings, primary diagnosis and outcome. Aust Vet J. 2018;96(10):385–389. doi:10.1111/avj.12749
13. Hoorn EJ, Betjes MG, Weigel J, Zietse R. Hypernatraemia in critically ill patients: too little water and too much salt. Nephrol Dial Transplant. 2008;23(5):1562–1568. doi:10.1093/ndt/gfm831
14. Sam R, Hart P, Haghighat R, Ing TS. Hypervolemic hypernatremia in patients recovering from acute kidney injury in the intensive care unit. Clin Exp Nephrol. 2012;16(1):136–146. doi:10.1007/s10157-011-0537-7
15. Pourfridoni M, Abbasnia SM, Shafaei F, Razaviyan J, Heidari-Soureshjani R. Fluid and electrolyte disturbances in COVID-19 and their complications. Biomed Res Int. 2021;2021:1–5. doi:10.1155/2021/6667047
16. Zimmer MA, Zink AK, Weißer CW, et al. Hypernatremia - a manifestation of COVID-19: a case series. A a Pract. 2020;14:e01295. doi:10.1213/XAA.0000000000001295
17. Lindner G, Funk GC. Hypernatremia in critically ill patients. J Crit Care. 2013;28:
18. Aronson D, Darawsha W, Promyslovsky M, et al. Hyponatraemia predicts the acute (type 1) cardio-renal syndrome. Eur J Heart Fail. 2014;16:49–55. doi:10.1093/eurjhf/hft123
19. Lameire N, Van Biesen W, Vanholder R. Electrolyte disturbances and acute kidney injury in patients with cancer. Semin Nephrol. 2010;30:534–547. doi:10.1016/j.semnephrol.2010.09.002
20. Hackworth WA, Heuman DM, Sanyal AJ, et al. Effect of hyponatraemia on outcomes following orthotopic liver transplantation. Liver Int. 2009;29:1071–1077. doi:10.1111/j.1478-3231.2009.01982.x
21. Adams D, de Jonge R, van der Cammen T, Zietse R, Hoorn EJ. Acute kidney injury in patients presenting with hyponatremia. J Nephrol. 2011;24:749–755. doi:10.5301/JN.2011.6410
22. Lee SW, Baek SH, Ahn SY, et al. The effects of pre-existing hyponatremia and subsequent-developing acute kidney injury on in-hospital mortality: a retrospective cohort study. PLoS One. 2016;11:e0162990. doi:10.1371/journal.pone.0162990
23. Bateman RM, Sharpe MD, Jagger JE, et al. 36th international symposium on intensive care and emergency medicine: Brussels, Belgium. 15–18 March 2016. Crit Care. 2016;20:94.
24. Berend K, van Hulsteijn LH, Gans RO. Chloride: the queen of electrolytes? Eur J Intern Med. 2012;23:203–211. doi:10.1016/j.ejim.2011.11.013
25. Barrett KE, Keely SJ. Chloride secretion by the intestinal epithelium: molecular basis and regulatory aspects. Annu Rev Physiol. 2000;62:535–572. doi:10.1146/annurev.physiol.62.1.535
26. Mojumdar EH, Sparr E. The effect of pH and salt on the molecular structure and dynamics of the skin. Colloids Surf B Biointerfaces. 2021;198. doi:10.1016/j.colsurfb.2020.111476
27. George AK, Shih A, Regan TJ. Effect of acute ketoacidosis on the myocardium in diabetes. Am J Med Sci. 1996;311:61–64. doi:10.1097/00000441-199602000-00001
28. Gunnerson KJ, Saul M, He S, Kellum JA. Lactate versus non-lactate metabolic acidosis: a retrospective outcome evaluation of critically ill patients. Crit Care. 2006;10:R22. doi:10.1186/cc3987
29. Suetrong B, Pisitsak C, Boyd JH, Russell JA, Walley KR. Hyperchloremia and moderate increase in serum chloride are associated with acute kidney injury in severe sepsis and septic shock patients. Crit Care. 2016;20:315. doi:10.1186/s13054-016-1499-7
30. Burdett E, Dushianthan A, Bennett-Guerrero E, et al. Perioperative buffered versus non-buffered fluid administration for surgery in adults. Cochrane Database Syst Rev. 2012;12:1.
31. Horton R, Berman P. Eliminating acute kidney injury by 2025: an achievable goal. Lancet. 2015;385:2551–2552. doi:10.1016/S0140-6736(15)60269-0
32. Kashani K, Al-Khafaji A, Ardiles T, et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care. 2013;17:R25. doi:10.1186/cc12503
33. Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP. A clinical score to predict acute renal failure after cardiac surgery. JASN. 2005;16:162–168. doi:10.1681/ASN.2004040331
34. Tziakas D, Chalikias G, Stakos D, et al. Development of an easily applicable risk score model for contrast-induced nephropathy prediction after percutaneous coronary intervention: a novel approach tailored to current practice. Int J Cardiol. 2013;163:46–55. doi:10.1016/j.ijcard.2011.05.079
35. Labarère J, Renaud B, Fine MJ. How to derive and validate clinical prediction models for use in intensive care medicine. Intensive Care Med. 2014;40:513–527. doi:10.1007/s00134-014-3227-6
36. Demirjian S, Bashour CA, Shaw A, et al. Predictive accuracy of a perioperative laboratory test-based prediction model for moderate to severe acute kidney injury after cardiac surgery. JAMA. 2022;327:956–964.
37. Nishimoto M, Murashima M, Kokubu M, et al. External validation of a prediction model for acute kidney injury following noncardiac surgery. JAMA Netw Open. 2021;4:e2127362. doi:10.1001/jamanetworkopen.2021.27362
38. Bao B, Wang W, Wang Y, Chen Q. A prediction score model and survival analysis of acute kidney injury following orthotopic liver transplantation in adults. Ann Palliat Med. 2021;10:6168–6179. doi:10.21037/apm-21-842
39. Martin-Cleary C, Molinero-Casares LM, Ortiz A, Arce-Obieta JM. Development and internal validation of a prediction model for hospital-acquired acute kidney injury. Clin Kidney J. 2021;14(1):309–316. doi:10.1093/ckj/sfz139
40. Liu L, Liu J, Lei L, et al. A prediction model of contrast-associated acute kidney injury in patients with hypoalbuminemia undergoing coronary angiography. BMC Cardiovasc Disord. 2020;20:399. doi:10.1186/s12872-020-01689-6
41. Liu J, Wu J, Liu S, et al. Predicting mortality of patients with acute kidney injury in the ICU using XGBoost model. PLoS One. 2021;16:e0246306. doi:10.1371/journal.pone.0246306
42. Zhu K, Song H, Zhang Z, et al. Acute kidney injury in solitary kidney patients after partial nephrectomy: incidence, risk factors and prediction. Transl Androl Urol. 2020;9:1232–1243. doi:10.21037/tau.2020.03.45
43. Patidar KR, Xu C, Shamseddeen H, et al. Development and validation of a model to predict acute kidney injury in hospitalized patients with cirrhosis. Clin Transl Gastroenterol. 2019;10:e00075. doi:10.14309/ctg.0000000000000075
44. Luo XQ, Yan P, Zhang NY, et al. Machine learning for early discrimination between transient and persistent acute kidney injury in critically ill patients with sepsis. Sci Rep. 2021;11:20269. doi:10.1038/s41598-021-99840-6
45. Luo M, Yang Y, Xu J, et al. A new scoring model for the prediction of mortality in patients with acute kidney injury. Sci Rep. 2017;7:7862. doi:10.1038/s41598-017-08440-w
46. Matuszkiewicz-Rowińska J, Małyszko J. Acute kidney injury, its definition, and treatment in adults: guidelines and reality. Pol Arch Intern Med. 2020;130:1074–1080. doi:10.20452/pamw.15373
47. Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825–830. doi:10.7326/0003-4819-158-11-201306040-00007
48. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–810. doi:10.1001/jama.2016.0287
49. Rouzier R, Pusztai L, Delaloge S, et al. Nomograms to predict pathologic complete response and metastasis-free survival after preoperative chemotherapy for breast cancer. J Clin Oncol. 2005;23:8331–8339. doi:10.1200/JCO.2005.01.2898
50. Harrell FE
51. Levey AS, James MT. Acute kidney injury. Ann Intern Med. 2017;167:Itc66–itc80. doi:10.7326/AITC201711070
52. Medve L, Antek C, Paloczi B, et al. Epidemiology of acute kidney injury in Hungarian intensive care units: a multicenter, prospective, observational study. BMC Nephrol. 2011;12. doi:10.1186/1471-2369-12-43
53. Hoste EA, Clermont G, Kersten A, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006;10:R73. doi:10.1186/cc4915
54. Goldberg A, Hammerman H, Petcherski S, et al. Inhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. Am Heart J. 2005;150:330–337. doi:10.1016/j.ahj.2004.09.055
55. Chew ST, Ng RR, Liu W, Chow KY, Ti LK. Acute kidney injury increases the risk of end-stage renal disease after cardiac surgery in an Asian population: a prospective cohort study. BMC Nephrol. 2017;18:60. doi:10.1186/s12882-017-0476-y
56. Lo LJ, Go AS, Chertow GM, et al. Dialysis-requiring acute renal failure increases the risk of progressive chronic kidney disease. Kidney Int. 2009;76:893–899. doi:10.1038/ki.2009.289
57. Adrogué HJ, Madias NE. Hypernatremia. N Engl J Med. 2000;342:1493–1499. doi:10.1056/NEJM200005183422006
58. Kalikkot Thekkeveedu R, Ramarao S, Dankhara N, Alur P. Hypochloremia secondary to diuretics in preterm infants: should clinicians pay close attention? Glob Pediatr Health. 2021;8. doi:10.1177/2333794X21991014
59. Libório AB, Silva GB
60. Aiyagari V, Deibert E, Diringer MN. Hypernatremia in the neurologic intensive care unit: how high is too high? J Crit Care. 2006;21:163–172. doi:10.1016/j.jcrc.2005.10.002
61. Li M, Hu YH, Chen G. Hypernatremia severity and the risk of death after traumatic brain injury. Injury. 2013;44:1213–1218. doi:10.1016/j.injury.2012.05.021
62. Gerber JG, Branch RA, Nies AS, Hollifield JW, Gerkens JF. Influence of hypertonic saline on canine renal blood flow and renin release. Am J Physiol. 1979;237:F441–446. doi:10.1152/ajprenal.1979.237.6.F441
63. Wilcox CS. Regulation of renal blood flow by plasma chloride. J Clin Invest. 1983;71:726–735. doi:10.1172/JCI110820
64. Lee JW. Fluid and electrolyte disturbances in critically ill patients. Electrolyte Blood Press. 2010;8:72–81. doi:10.5049/EBP.2010.8.2.72
65. Darmon M, Timsit JF, Francais A, et al. Association between hypernatraemia acquired in the ICU and mortality: a cohort study. Nephrol Dial Transplant. 2010;25:2510–2515. doi:10.1093/ndt/gfq067
66. Lindner G, Funk GC, Schwarz C, et al. Hypernatremia in the critically ill is an independent risk factor for mortality. Am J Kidney Dis. 2007;50:952–957. doi:10.1053/j.ajkd.2007.08.016
67. O’Donoghue SD, Dulhunty JM, Bandeshe HK, Senthuran S, Gowardman JR. Acquired hypernatraemia is an independent predictor of mortality in critically ill patients. Anaesthesia. 2009;64:514–520. doi:10.1111/j.1365-2044.2008.05857.x
68. Qureshi AI, Suri MF, Sung GY, et al. Prognostic significance of hypernatremia and hyponatremia among patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2002;50(4):749–755. doi:10.1097/00006123-200204000-00012
69. Zhi D, Lin J, Dong L, et al. Risk predictive role of hypernatremia for occurrence of sepsis-induced acute kidney injury. Ann Palliat Med. 2021;10:4705–4715. doi:10.21037/apm-21-792
70. Zou Z, Chen S, Li Y, et al. Risk factors for renal failure and short-term prognosis in patients with spontaneous intracerebral haemorrhage complicated by acute kidney injury. BMC Nephrol. 2020;21:311. doi:10.1186/s12882-020-01949-9
71. Milionis HJ, Liamis G, Elisaf MS. Hypernatremia in hospitalized patients: a sequel of inadvertent fluid administration. Arch Intern Med. 2000;160:1541–1542. doi:10.1001/archinte.160.10.1541
72. Froelich M, Ni Q, Wess C, Ougorets I, Härtl R. Continuous hypertonic saline therapy and the occurrence of complications in neurocritically ill patients. Crit Care Med. 2009;37:1433–1441. doi:10.1097/CCM.0b013e31819c1933
73. Darmon M, Diconne E, Souweine B, et al. Prognostic consequences of borderline dysnatremia: pay attention to minimal serum sodium change. Crit Care. 2013;17:R12. doi:10.1186/cc11937
74. Lombardi G, Ferraro PM, Naticchia A, Gambaro G. Serum sodium variability and acute kidney injury: a retrospective observational cohort study on a hospitalized population. Intern Emerg Med. 2021;16:617–624. doi:10.1007/s11739-020-02462-5
75. McCluskey SA, Karkouti K, Wijeysundera D, et al. Hyperchloremia after noncardiac surgery is independently associated with increased morbidity and mortality: a propensity-matched cohort study. Anesth Analg. 2013;117:412–421. doi:10.1213/ANE.0b013e318293d81e
76. de Vasconcellos K, Skinner DL. Hyperchloraemia is associated with acute kidney injury and mortality in the critically ill: a retrospective observational study in a multidisciplinary intensive care unit. J Crit Care. 2018;45:45–51. doi:10.1016/j.jcrc.2018.01.019
77. Marttinen M, Wilkman E, Petäjä L, et al. Association of plasma chloride values with acute kidney injury in the critically ill - a prospective observational study. Acta Anaesthesiol Scand. 2016;60:790–799. doi:10.1111/aas.12694
78. Patel N, Baker SM, Walters RW, et al. Serum hyperchloremia as a risk factor for acute kidney injury in patients with ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention. Proc. 2016;29:7–11.
79. Young P, Bailey M, Beasley R, et al. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: the SPLIT randomized clinical trial. JAMA. 2015;314:1701–1710. doi:10.1001/jama.2015.12334
80. Yessayan L, Neyra JA, Canepa-Escaro F, et al. Effect of hyperchloremia on acute kidney injury in critically ill septic patients: a retrospective cohort study. BMC Nephrol. 2017;18:346. doi:10.1186/s12882-017-0750-z
81. Sadan O, Singbartl K, Kandiah PA, Martin KS, Samuels OB. Hyperchloremia is associated with acute kidney injury in patients with subarachnoid hemorrhage. Crit Care Med. 2017;45:1382–1388. doi:10.1097/CCM.0000000000002497
82. Toyonaga Y, Kikura M. Hyperchloremic acidosis is associated with acute kidney injury after abdominal surgery. Nephrology. 2017;22:720–727. doi:10.1111/nep.12840
83. Malhotra R, Kashani KB, Macedo E, et al. A risk prediction score for acute kidney injury in the intensive care unit. Nephrol Dial Transplant. 2017;32:814–822. doi:10.1093/ndt/gfx026
84. Flechet M, Güiza F, Schetz M, et al. AKIpredictor, an online prognostic calculator for acute kidney injury in adult critically ill patients: development, validation and comparison to serum neutrophil gelatinase-associated lipocalin. Intensive Care Med. 2017;43:764–773. doi:10.1007/s00134-017-4678-3
85. Biggins SW, Kim WR, Terrault NA, et al. Evidence-based incorporation of serum sodium concentration into MELD. Gastroenterology. 2006;130:1652–1660. doi:10.1053/j.gastro.2006.02.010
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.