Back to Journals » Infection and Drug Resistance » Volume 17
Nirmatrelvir–Ritonavir Reduced Mortality in Hospitalized Patients with COVID-19 During the Omicron Outbreak: Real-World Evidence from Beijing
Authors Zhang Y, Wang X, Huang C, Yang H, Jiang C, Yu X, Hong J, Zhang Y, Wang Y, Zhao R, An Z, Tong Z
Received 6 November 2023
Accepted for publication 24 February 2024
Published 8 April 2024 Volume 2024:17 Pages 1367—1377
DOI https://doi.org/10.2147/IDR.S445826
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Sandip Patil
Yi Zhang,1,* Xinrui Wang,1,* Chong Huang,2 Hui Yang,1 Chunguo Jiang,3 Xiaojia Yu,1 Jun Hong,2 Yi Zhang,1 Yushu Wang,1 Rui Zhao,1 Zhuoling An,1 Zhaohui Tong3
1Department of Pharmacy, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China; 2School of Pharmaceutical Sciences, Capital Medical University, Beijing, People’s Republic of China; 3Department of Respiratory and Critical Care Medicine, Beijing Institute of Respiratory Medicine, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhuoling An, Department of Pharmacy, Beijing Chao-Yang Hospital, Capital Medical University, 8 Gongren Tiyuchang Nanlu, Chaoyang District, Beijing, 100020, People’s Republic of China, Tel +00-86-010-85231362, Email [email protected] Zhaohui Tong, Department of Respiratory and Critical Care Medicine, Beijing Institute of Respiratory Medicine, Beijing Chao-Yang Hospital, Capital Medical University, 8 Gongren Tiyuchang Nanlu, Chaoyang District, Beijing, 100020, People’s Republic of China, Tel +00-86-010-85231464, Email [email protected]
Objective: The efficacy of nirmatrelvir–ritonavir for hospitalized patients with COVID-19 has not been fully established.
Methods: We conducted a retrospective analysis of hospitalized COVID– 19 patients with high risk for disease progression at Beijing Chaoyang Hospital from October 15, 2022, to March 31, 2023. Patients ≥ 18 years old who were hospitalized with COVID-19 within 5 days of symptom onset were included. Baseline data were obtained from the routine electronic health record database of the hospital information system. Outcomes were monitored at 28 days via electronic medical record reviews or telephone interviews.
Results: We identified 1120 patients hospitalized with COVID-19 during the study period. After exclusions, 167 nirmatrelvir–ritonavir users and 132 controls were included. 28-day all-cause mortality rate was 12.0% (20/167) in the nirmatrelvir–ritonavir group, versus 22.7% (30/132) in the control group (unadjusted log-rank p = 0.010; HR = 0.49, 95% confidence interval [CI] = 0.28– 0.86, IPTW-adjusted HR = 0.58, 95% CI = 0.40– 0.86). The 28-day disease progression rates did not differ between the two groups (unadjusted HR = 0.59, 95% CI = 0.34– 1.02, IPTW-adjusted HR = 0.73, 95% CI = 0.50– 1.06). Nirmatrelvir–ritonavir significantly reduced all-cause mortality and disease progression within 28 days among patients aged ≥ 65 years without ≥ 2 vaccine doses.
Conclusion: We found significantly reduced all-cause mortality in the nirmatrelvir–ritonavir group, particularly in elderly patients who were incompletely vaccinated. Future randomized controlled studies are needed to validate our findings.
Keywords: nirmatrelvir–ritonavir, COVID-19, hospitalized
Introduction
In December 2022, China experienced a surge of infections by the SARS-CoV-2 Omicron variant, resulting in a substantial strain on the healthcare system.1,2 In response, the medical community has actively sought to identify effective treatments to mitigate the morbidity and mortality of this infection. Nirmatrelvir–ritonavir (Paxlovid), an oral antiviral drug, has displayed significant benefits in non-hospitalized patients with COVID-19.3 Emergency use authorization was granted for nirmatrelvir–ritonavir in the treatment of non-hospitalized patients with COVID-19 by the US Food and Drug Administration in December 2021.4
However, guidelines from the World Health Organization and US National Institutes of Health currently recommend nirmatrelvir–ritonavir only for non-hospitalized patients at high risk of hospitalization.5,6 The efficacy of nirmatrelvir–ritonavir for hospitalized patients with COVID-19, who might experience rapid disease progression and require more supportive care, has not been established. Previous clinical evidence indicated favorable outcomes for nirmatrelvir–ritonavir in hospitalized patients with COVID-19, including reductions in all-cause mortality, disease progression,7,8 and the need for oxygen therapy in patients without supplemental oxygen.8 However, these studies provided limited information regarding oxygen support, making it challenging to ascertain the drug’s efficacy in different disease stages.
Furthermore, the potential benefits of nirmatrelvir–ritonavir in specific populations warrant further exploration. Previous studies found that older non-hospitalized adults with COVID-19 might derive more significant benefits from nirmatrelvir–ritonavir than younger individuals,9 but the applicability of these findings to hospitalized patients remains uncertain. Additionally, the influence of vaccination on the drug’s efficacy remains unclear. Although an earlier study acknowledged that both antivirals and vaccination were independently associated with reduced risks of severe COVID-19 in outpatient settings,10 a study involving hospitalized patients with COVID-19 suggested that nirmatrelvir–ritonavir was effective regardless of vaccination status.7 Thus, additional evidence regarding patients of different ages and immunity situations is required.
To address these knowledge gaps, this retrospective cohort study evaluated the effectiveness of nirmatrelvir–ritonavir in hospitalized patients with COVID-19.
Methods
Study Design
This single-center, retrospective cohort study involved hospitalized adults with COVID-19 who visited Beijing Chaoyang Hospital between October 15, 2022 and March 31, 2023. For this retrospective study, the institutional review board of Beijing Chaoyang Hospital, Capital Medical University granted an exemption from requiring informed consent. However, for patients who were followed up during the course of the study, verbal informed consent was obtained. This procedure was approved by the ethics committee and is in compliance with the Declaration of Helsinki. The study is registered at www.clinicaltrials.gov (NCT05792865).
Data Source and Eligibility Criteria
Baseline characteristics, including demographic characteristics, the dates of hospital and intensive care unit (ICU) admission, the date of registered death, diagnoses, prescriptions, procedures, and laboratory tests, were obtained from the routine electronic health record database of the hospital information system. The vaccination status and missing data such as BMI were collected via telephone. Additional concomitant treatments initiated within 24 h of admission including respiratory support and other drug use were allowed and collected as baseline characteristics.
Patients at least 18 years old who were hospitalized with COVID-19 (defined as a diagnosis of COVID-19 upon hospital admission or a positive PT-PCR or rapid antigen test for SARS-CoV-2 infection on the date of admission) with high risk for disease progression within 5 days of symptoms onset were eligible. The index date was defined as the date of hospital admission. The exclusion criteria were as follows: 1) receipt of any antiviral drugs before the index date; 2) transfer from another hospital or any community setting; 3) death in the first 24 h of admission; and 4) diagnosis of severe liver impairment (cirrhosis, hepatocellular carcinoma) or renal impairment (estimated glomerular filtration rate < 30 mL/min/1.73 m2, dialysis); 5) without high-risk factors for disease progression.
Treatment Strategies and Follow-Up
Patients who received nirmatrelvir–ritonavir within 5 days of symptom onset were included in the treatment group. Concomitant treatments such as antibiotics and corticosteroids were recorded for covariate adjustments. Hospitalized patients who did not receive nirmatrelvir–ritonavir during the study period were included in the control group. Patients were followed up at 28 days via electronic medical record reviews or telephone interviews. In cases in which patients were unable to complete the telephone follow-up, the follow-up date was the date of discharge. The last follow-up date was April 30, 2023.
Outcomes
The primary outcome was 28-day all-cause mortality. The secondary outcomes included a composite of 28-day disease progression including invasive mechanical ventilation, ICU admission, and death, as well as their individual outcomes, cardiovascular thromboembolism events, hospital re-admission, and re-infection with SARS-CoV-2 within 28 days after the index date.
Quality Control
The accuracy and completeness of the data and clinical events in the project were ensured through the implementation of quality control strategies. All researchers involved in the study underwent comprehensive training prior to the project’s launch. This training aimed to familiarize the researchers with standardized procedures for data collection, follow-up, and outcome determination. Two researchers (YZ and XW) carefully examined the outliers in the original data to verify their accuracy and address any potential issues. Any discrepancies or inconsistencies discovered during these inspections were promptly addressed by the research team to maintain the overall quality of the data.
Statistical Analysis
Baseline demographic and clinical data are reported as the mean (standardized difference) or frequency (percentage) and compared using the chi-squared test or Student’s t-test, as appropriate. Hazard ratios (HRs) with 95% confidence intervals (CIs) for each outcome between the nirmatrelvir–ritonavir and control groups were estimated using Cox regression models. The mortality and disease progression probabilities were plotted using Kaplan–Meier curves and evaluated using the Log rank test. An inverse probability of treatment weighting (IPTW)-adjusted Cox regression model was created to adjust for potential confounding factors. Propensity scores were estimated by logistic regression according to baseline covariates. The weight of the nirmatrelvir–ritonavir group was the inverse of (1 − propensity score), and the weight of the control group was the inverse of the propensity score. Covariates used in the IPTW model were selected using all baseline characteristics. The prescription time of nirmatrelvir–ritonavir from symptom onset was modeled as a time-dependent variable. Standardized differences were used to assess the differences between the two groups before and after IPTW adjustment. A standardized difference value of <0.10 indicated good balance between the two groups.
Sensitivity analysis was conducted in three ways: 1) using the multivariate Cox regression model for all outcomes; 2) using multivariate Cox regression and IPTW-adjusted Cox regression after multiple imputations for all outcomes; and 3) including events within 24 h after admission for all outcomes.
Subgroup analyses were performed for the major outcome regarding all baseline characteristics using both the crude and IPTW-adjusted models. Additionally, we performed subgroup analyses comparing all-cause mortality and disease progression within 28 days in patients aged ≥65 years who did not receive ≥2 vaccine doses and in those aged <65 or ≥65 years who received ≥2 vaccine doses.
Statistical analysis was performed using Stata version 16.0 and GraphPad Prism version 9.5. A two-sided p-value of 0.05 was used to identify statistically significant differences.
Results
In total, 1120 hospitalized patients with COVID-19 were identified. After applying the exclusion criteria, 167 nirmatrelvir–ritonavir users and 132 controls were included in the cohort (Figure 1). The baseline characteristics of the included and excluded cohorts are presented shown in Table S1. The average duration of hospitalization was 22.97 ± 8.80 days. The mean patient age in the nirmatrelvir–ritonavir group (39.5% women) was 67.92 ± 17.32 years, versus 67.84 ± 19.60 years (31.8% women) in the control group (Table S2). Meanwhile, 96.4% and 98.5% of patients in the nirmatrelvir–ritonavir and control groups were Han Chinese, respectively. Concerning the vaccination status, the proportions of patients who received ≤1, 2, and ≥3 doses were 44.4%, 10.3%, and 46.5%, respectively, in the nirmatrelvir–ritonavir group and 48.5%, 12.8%, and 38.4%, respectively, in the control group. All patients were immunized with inactivated COVID-19 vaccines (Sinopharm or Sinovac). In total, 75.45% and 75.76% of patients in the nirmatrelvir–ritonavir and control groups received oxygen support, respectively. ICU admission and invasive mechanical ventilation within 24 h of admission were required in 16 (9.6%) and 6 (3.6%) patients, respectively, in the nirmatrelvir–ritonavir group, versus two (1.5%) and one (0.8%) patient, respectively, in the control group. Concomitant medication including dexamethasone (13.8% vs 4.6%), other systemic steroids (22.8% vs 23.5%), antibiotics (37.1% vs 41.7%), baricitinib (0.6% vs 1.5%), and tocilizumab (0.6% vs 0.0%) were used at similar rates in the two groups. After IPTW adjustment, the nirmatrelvir–ritonavir and control groups were well balanced with a standardized difference of 0.06 or smaller (Table 1).
 |
Table 1 Baseline Characteristics Before and After the Inverse Probability Weighting of Propensity Scores |
 |
Figure 1 Flowchart for selection of study population. |
The 28-day all-cause mortality rates were 12.0% (20/167) in the nirmatrelvir–ritonavir group and 22.7% (30/132) in the control group (Table 2). Nirmatrelvir users had significantly lower rates of all-cause mortality within 7 days (unadjusted HR = 0.34, 95% CI = 0.15–0.79, IPTW-adjusted HR = 0.43, 95% CI = 0.24–0.76), 14 days (unadjusted HR = 0.50, 95% CI = 0.26–0.93, IPTW-adjusted HR = 0.63, 95% CI = 0.41–0.98), and 28 days (unadjusted log-rank p = 0.010, HR = 0.49, 95% CI = 0.28–0.86, IPTW-adjusted HR = 0.58, 95% CI = 0.40–0.86; Figures 2–3). Sensitivity analysis revealed similar positive effects of nirmatrelvir–ritonavir on all-cause mortality (Tables S3–5).
 |
Table 2 Outcomes of Hospitalized COVID-19 Nirmatrelvir-Ritonavir Compared to Control Group |
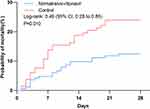 |
Figure 2 28-day cumulative incidence of outcomes all-cause mortality. |
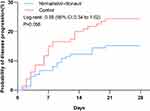 |
Figure 3 28-day cumulative incidence of the disease progression outcome consisted of all-cause mortality, initiation of invasive mechanical ventilation, intensive care unit admission. |
Meanwhile, 22 (12.0%) and 30 (22.7%) patients in the nirmatrelvir–ritonavir and control groups experienced disease progression, respectively (Table 2). The 28-day disease progression rate did not differ between the groups (unadjusted HR = 0.59, 95% CI = 0.34–1.02, IPTW-adjusted HR = 0.73, 95% CI = 0.50–1.06). Similarly, the rates of invasive mechanical ventilation (unadjusted HR = 1.56, 95% CI = 0.29–8.53, IPTW-adjusted HR = 1.58, 95% CI = 0.48–5.23) and ICU admission (unadjusted HR = 1.61, 95% CI = 0.15–17.73, IPTW-adjusted HR = 2.54, 95% CI = 0.55–11.75) were comparable between the two groups.
The rates of cardiovascular thromboembolic events, re-admission, and re-infection did not differ between the groups (Table 2).
In subgroup analyses of all-cause mortality and disease progression within 28 days, we found mostly similar results to the primary analysis (Figure 4, Tables S6–S7). Patents who received fewer vaccine doses tended to benefit from nirmatrelvir–ritonavir. Meanwhile, significant differences in outcomes were observed in the chronic liver disease and neurological disease subgroups.
 |
Figure 4 Subgroup analyses of all-cause mortality within 28 days for hospitalized COVID-19 nirmatrelvir-ritonavir versus control group. |
A significant subgroup difference in all-cause mortality was found between patients aged ≥65 years without ≥2 vaccine doses (17.3% vs 44.2%, IPTW-adjusted HR = 0.34, 95% CI = 0.20–0.59) and those aged <65 or ≥65 years with ≥2 vaccine doses (8.2% vs 8.7%, IPTW-adjusted HR = 1.34, 95% CI = 0.72–2.49, p for trend < 0.001, Table 3). Nirmatrelvir–ritonavir significantly reduced all-cause mortality and disease progression within 28 days in patients aged ≥65 years without ≥2 vaccine doses. Also, we found similar result in the subgroup analysis regarding vaccination and immunity status, showing significantly reduced all-cause mortality and disease progression rate in patients with weak immunity status (Table S8).
 |
Table 3 Hazard Ratios of Outcomes for Hospitalized COVID-19 According to Vaccination Status and Age |
Discussion
This study evaluated the real-world efficacy of nirmatrelvir–ritonavir in hospitalized patients with COVID-19 during the outbreak of the Omicron variant in Beijing, China from December 2022 to March 2023. Within this cohort of hospitalized patients, 75.6% of whom required supplemental oxygen, our analysis demonstrated that nirmatrelvir–ritonavir significantly reduced all-cause mortality rates in patients with COVID-19, but it did not significantly decrease the rate of disease progression. Furthermore, our results demonstrated the efficacy of nirmatrelvir–ritonavir in elderly patients who were incompletely vaccinated but not in completely vaccinated patients or in those younger than 65 years. These findings provide additional evidence for the use of nirmatrelvir–ritonavir in hospitalized patients with COVID-19.
Currently, there is insufficient evidence to support the efficacy of the oral antiviral nirmatrelvir–ritonavir in the treatment of hospitalized patients with COVID-19 within 5 days of symptom onset. Two large observational studies involving Hong Kong-based cohorts provided evidence for the effectiveness of nirmatrelvir–ritonavir in hospitalized patients. Wong et al8 found that nirmatrelvir–ritonavir significantly reduced the 30-day mortality rate (event rate: 3.6% in the nirmatrelvir–ritonavir group vs 10.3% in the control group, HR = 0.34, 95% CI = 0.23–0.50) among hospitalized patients infected with the Omicron variant who did not require oxygen supplementation. More recently, Wan et al7 conducted a study of hospitalized patients diagnosed with COVID-19 enrolled within 5 days of symptom onset and showed that nirmatrelvir–ritonavir reduced the 28-day mortality rate (cumulative event rate: 7.9% in the nirmatrelvir–ritonavir group vs 10.3% in the non-use group, HR = 0.77, 95% CI = 0.66–0.90). However, the latter study did not provide the proportion of patients who required oxygen supplementation, a key indicator of disease progression. Therefore, the efficacy of nirmatrelvir–ritonavir in hospitalized patients remains unclear. Nevertheless, numerous studies, including the EPIC-HR trial, previously confirmed the efficacy of nirmatrelvir–ritonavir in patients with COVID-19 who do not require oxygen supplementation.3,7,11,12 With the recent termination of the EPIC-HOS study evaluating the use of nirmatrelvir–ritonavir in hospitalized patients with severe COVID-19 because of limitations in its feasibility,13 the importance of the results of this study is heightened. This study confirmed that nirmatrelvir–ritonavir can reduce the 28-day mortality rate among this cohort of hospitalized patients with COVID-19 during the Omicron outbreak, most of whom received oxygen support within 24 h of admission. The cumulative event rate for the nirmatrelvir–ritonavir group was 11.98%, compared with 22.73% for the control group (HR = 0.58, 95% CI = 0.40–0.86). These results provide a critical supplement to the current evidence base for the use of nirmatrelvir–ritonavir in hospitalized patients with COVID-19 whose symptoms appeared within 5 days of admission.
As of March 2023, China has administered an estimated 3.5 billion doses of inactivated SARS-CoV-2 vaccines.14 Within our study cohort, 57% of patients had received at least two doses of the SARS-CoV-2 vaccine, surpassing previous investigations. Previous studies involving mRNA vaccines showed their positive and independent effect than antivirals on reducing viral shedding time in high-risk COVID-19 patients.15,16 The effect of vaccination is reportedly relevant for high-risk patients, but less for low-risk immune-competent patients affected by mild or asymptomatic diseases.17,18 Remarkably, we observed a positive correlation between the reduction in vaccine dosages and the enhanced therapeutic benefits of nirmatrelvir–ritonavir in hospitalized patients. Earlier research conducted in Hong Kong19 and Shanghai20 demonstrated that individuals who received the inactivated vaccine CoronaVac prior to infection exhibited expedited viral clearance and reduced risks of severe COVID-19. Additionally, a positive dose–response relationship was identified, highlighting the potential of the vaccine dosage to optimize clinical outcomes.21 Therefore, further research is warranted to ascertain whether nirmatrelvir–ritonavir can confer noteworthy clinical benefits to fully vaccinated hospitalized patients with COVID-19.
The impact of age on the clinical efficacy of nirmatrelvir–ritonavir has been a topic of previous studies focusing on non-hospitalized patients. Investigations conducted in Israel and Hong Kong8,9 demonstrated a notable reduction in hospitalization and COVID-19–related mortality rates among individuals aged 65 years or older who received nirmatrelvir–ritonavir compared with their counterparts who did not receive nirmatrelvir–ritonavir. Conversely, there was no statistically significant decrease in the risk of hospitalization or mortality among individuals younger than 65 years. A stratified analysis of the Israeli population9 evaluating the efficacy of nirmatrelvir–ritonavir revealed a higher hospitalization rate (8%) in the subgroup lacking prior SARS-CoV-2 immunity, particularly among elderly patients, than in the subgroup with prior immunity (1%). Based on our investigation, which included a stratified analysis considering the patient vaccination status and age, our findings demonstrated a significant reduction in mortality and composite disease progression rates among elderly individuals with suboptimal vaccine dosing who received nirmatrelvir–ritonavir compared with that in the untreated cohort. However, this effect was not statistically significant among individuals younger than 65 years or among those who had received at least two vaccine doses. Hence, vaccination should be prioritized over antivirals in high-risk patients, also from the cost-effective perspective, the risk of developing anti-viral resistance in case of widespread use of antivirals, as well as its potential effect on reduction of risk of post-COVID-19 sequelae.22,23
This study revealed some interesting findings. First, the effectiveness of nirmatrelvir–ritonavir was not ideal in patients with mild-to-moderate liver dysfunction. Prior research confirmed that liver impairment is an independent risk factor for poor prognosis in COVID-19 patients.24 Although studies have suggested that nirmatrelvir–ritonavir causes less liver damage,25 there is currently insufficient evidence regarding its benefits in patients with liver dysfunction. Additionally, whether the adverse effects caused by ritonavir through the inhibition of liver enzymes are amplified in patients with liver dysfunction also warrants investigation. Furthermore, our analysis revealed a lack of significant effects of nirmatrelvir–ritonavir among patients with neurological disease. It is noteworthy that previous studies reported a direct correlation between neurological disease and mortality in patients with COVID-19. Although the limited sample size in our study could affect the stability of conclusions drawn from stratified analyses, we recommend focusing on the effects of nirmatrelvir–ritonavir in patients with liver dysfunction or neurological disease in clinical practice while eagerly awaiting further validation of our findings through subsequent research.
Our study had several strengths. First, few patients received baricitinib or tocilizumab, and none received remdesivir, thereby naturally shielding our study from these confounding treatment effects. This unique attribute enables a more direct evaluation of the effectiveness of nirmatrelvir–ritonavir in hospitalized patients with early-stage COVID-19, a key strength lacking in prior studies.7 Additionally, to mitigate the impact of confounding factors, we carefully considered potential confounders and employed propensity score inverse probability weighting to balance confounding variables while conducting extensive sensitivity analyses.
We must acknowledge several limitations in our study. First, as a retrospective observational study, our sample size was not large, and some secondary outcomes and stratified analyses could have been susceptible to instability because of sample size limitations. Our results is also influenced by the type of vaccine used in this population (Sinovac or Sinopharm), with a different efficacy from other vaccines widely administered in other countries, especially Europe and North America. Second, the potential for higher comorbidity severity in the control group due to the numerous drug interactions of nirmatrelvir–ritonavir, which might necessitate the continuation of contraindicated medications and could lead to increased mortality. In addition, we acknowledge the critical distinction between deaths directly attributable to COVID-19 and those where COVID-19 may have been incidental. Furthermore, some of the data on the vaccination status and post-hospitalization outcomes were obtained through follow-up, which could be subject to recall bias, despite the implemented rigorous quality control procedures. Lastly, it is possible that some cases included in this study were underdiagnosed because of limited medical resources. For example, some patients might have been unable to receive ICU admission because of bed shortages or a refusal to undergo invasive mechanical ventilation. These factors could have resulted in an incomplete representation of disease progression outcomes among patients in this study. Further validation is needed to generalize our findings in randomized controlled trials.
Conclusion
In conclusion, this retrospective cohort study evaluated the effectiveness of nirmatrelvir–ritonavir in hospitalized patients with COVID-19, of which approximately three-quarters required oxygen therapy. We found significantly reduced all-cause mortality in the nirmatrelvir–ritonavir group, particularly in elderly patients who were incompletely vaccinated. There was no significant impact on the incidence of disease progression events. These findings support the potential use of nirmatrelvir–ritonavir for antiviral treatment in hospitalized patients with COVID-19 during the early stages of infection. Future randomized controlled studies are needed to validate our findings.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Informed Consent
This study was approved by the institutional review board and ethics committee of Beijing Chaoyang Hospital, Capital Medical University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from the Capital’s Funds for Health Improvement and Research (Grant No. 2022-1-1061) and the Ministry of Science and Technology of the People’s Republic of China (2021YFC0863600, 2023YFC0872500).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Xinhua. China Focus: china releases measures to optimize COVID-19 response; 2022. Available from: https://english.news.cn/20221111/d4399114a082438eaac32d08a02bf58d/c.html.
2. Xinhua. China Focus: COVID-19 response further optimized with 10 new measures; 2022. Available from: https://english.news.cn/20221207/ca014c043bf24728b8dcbc0198565fdf/c.html.
3. Hammond J, Leister-Tebbe H, Gardner A, et al. Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19. N Engl J Med. 2022;386(15):1397–1408. doi:10.1056/NEJMoa2118542
4. Administration UFaD. Fact sheet for healthcare providers: emergency use authorization for Paxlovid. Available from: https://wwwfdagov/media/155050/download.
5. World Health Organization. Update to living WHO guideline on drugs for covid-19. BMJ. 2021;374:n2219. doi:10.1136/bmj.n2219
6. Health NIo. COVID-19 Treatment Guidelines. Available from: https://www.covid19treatmentguidelines.nih.gov/therapies/antivirals-including-antibody-products/ritonavir-boosted-nirmatrelvir--paxlovid-/.
7. Wan EYF, Yan VKC, Mok AHY, et al. Effectiveness of Molnupiravir and Nirmatrelvir–Ritonavir in Hospitalized Patients With COVID-19. Ann Internal Med. 2023;176(4):505–514. doi:10.7326/M22-3057
8. Wong CKH, Ich A, Lau KTK, Lau EHY, Cowling BJ, Leung GM. Real-world effectiveness of early molnupiravir or nirmatrelvir-ritonavir in hospitalised patients with COVID-19 without supplemental oxygen requirement on admission during Hong Kong’s omicron BA.2 wave: a retrospective cohort study. Lancet Infect Dis. 2022;22(12):1681–1693. doi:10.1016/s1473-3099(22)00507-2
9. Arbel R, Wolff Sagy Y, Hoshen M, et al. Nirmatrelvir Use and Severe Covid-19 Outcomes during the Omicron Surge. N Engl J Med. 2022;387(9):790–798. doi:10.1056/NEJMoa2204919
10. Najjar-Debbiny R, Gronich N, Weber G, et al. Effectiveness of Paxlovid in Reducing Severe Coronavirus Disease 2019 and Mortality in High-Risk Patients. Clin Infect Dis. 2023;76(3):e342–e349. doi:10.1093/cid/ciac443
11. Ganatra S, Dani SS, Ahmad J, et al. Oral Nirmatrelvir and Ritonavir in Nonhospitalized Vaccinated Patients With Coronavirus Disease 2019. Clin Infect Dis. 2023;76(4):563–572. doi:10.1093/cid/ciac673
12. Zheng Q, Ma P, Wang M, et al. Efficacy and safety of Paxlovid for COVID-19: a meta-analysis. J Infect. 2023;86(1):66–117. doi:10.1016/j.jinf.2022.09.027
13. A Study to Learn About the Medicine Called Nirmatrelvir Used in Combination With Ritonavir in People With Weakened Immune Systems or at Increased Risk for Poor Outcomes Who Are Hospitalized Due to Severe COVID-19 (EPIC-HOS). Available from: https://www.clinicaltrials.gov/ct2/show/NCT05545319.
14. Chinese Center for Disease Control and Prevention. Nationwide Updates on Novel Coronavirus Infection Situation; 2023. Available from: https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_13141/202303/t20230311_264174.html.
15. Cegolon L, Pol R, Simonetti O, Larese Filon F, Luzzati R. Molnupiravir, Nirmatrelvir/Ritonavir, or Sotrovimab for High-Risk COVID-19 Patients Infected by the Omicron Variant: hospitalization, Mortality, and Time until Negative Swab Test in Real Life. Pharmaceuticals. 2023;16(5):721. doi:10.3390/ph16050721
16. De Vito A, Moi G, Saderi L, et al. Vaccination and Antiviral Treatment Reduce the Time to Negative SARS-CoV-2 Swab: a Real-Life Study. Viruses. 2023;15(11):2180. doi:10.3390/v15112180
17. Cegolon L, Mastrangelo G, Emanuelli E, Camerotto R, Spinato G, Frezza D. Early Negativization of SARS-CoV-2 Infection by Nasal Spray of Seawater plus Additives: the RENAISSANCE Open-Label Controlled Clinical Trial. Pharmaceutics. 2022;14(11):2502. doi:10.3390/pharmaceutics14112502
18. Lin JL, Zhang F, Li YB, et al. Efficacy of physiological seawater nasal irrigation for the treatment of children with SARS-CoV-2 Omicron BA.2 variant infection: a randomized controlled trial. World J Pediatr. 2023. doi:10.1007/s12519-023-00749-z
19. McMenamin ME, Nealon J, Lin Y, et al. Vaccine effectiveness of one, two, and three doses of BNT162b2 and CoronaVac against COVID-19 in Hong Kong: a population-based observational study. Lancet Infect Dis. 2022;22(10):1435–1443. doi:10.1016/s1473-3099(22)00345-0
20. Wang Y, Zhao D, Liu X, Chen X, Xiao W, Feng L. Early administration of Paxlovid reduces the viral elimination time in patients infected with SARS-CoV-2 Omicron variants. J Med Virol. 2023;95(1):e28443. doi:10.1002/jmv.28443
21. Qi T, Jin Y, Wang H, et al. Nirmatrelvir-ritonavir therapy and COVID-19 vaccination improve clinical outcomes of SARS-CoV-2 Omicron variant infection. J Med Virol. 2023;95(2):e28497. doi:10.1002/jmv.28497
22. Cegolon L, Mauro M, Sansone D, et al. A Multi-Center Study Investigating Long COVID-19 in Healthcare Workers from North-Eastern Italy: prevalence, Risk Factors and the Impact of Pre-Existing Humoral Immunity-ORCHESTRA Project. Vaccines. 2023;11(12). doi:10.3390/vaccines11121769
23. Fernández-de-las-Peñas C, Raveendran AV, Giordano R, Arendt-Nielsen L. Long COVID or Post-COVID-19 Condition: past, Present and Future Research Directions. Microorganisms. 2023;11(12):2959. doi:10.3390/microorganisms11122959
24. Yip TC, Lui GC, Wong VW, et al. Liver injury is independently associated with adverse clinical outcomes in patients with COVID-19. Gut. 2021;70(4):733–742. doi:10.1136/gutjnl-2020-321726
25. Wong GL, Hui VW, Yip TC, Lui GC, Hui DS, Wong VW. Minimal Risk of Drug-Induced Liver Injury With Molnupiravir and Ritonavir-Boosted Nirmatrelvir. Gastroenterology. 2023;164(1):151–153. doi:10.1053/j.gastro.2022.09.008
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
