Back to Journals » Journal of Pain Research » Volume 16
Musculoskeletal Pain Management and Thermotherapy: An Exploratory Analysis of Italian Physicians’ Attitude, Beliefs, and Prescribing Habits
Authors Ventriglia G, Gervasoni F, Franco M, Magni A, Panico G, Iolascon G
Received 14 December 2022
Accepted for publication 28 March 2023
Published 11 May 2023 Volume 2023:16 Pages 1547—1557
DOI https://doi.org/10.2147/JPR.S401550
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Alaa Abd-Elsayed
Giuseppe Ventriglia,1 Fabrizio Gervasoni,2 Massimiliano Franco,1 Alberto Magni,1 Giorgio Panico,2 Giovanni Iolascon3
1SIMG (Italian College of General Practitioners and Primary Care), Florence, Italy; 2Rehabilitation Unit, Luigi Sacco University Hospital, ASST Fatebenefratelli-Sacco, Milan, Italy; 3Department of Medical and Surgical Specialties and Dentistry, University of Campania “Luigi Vanvitelli”, Naples, Italy
Correspondence: Fabrizio Gervasoni, Rehabilitation Unit, Ospedale L. Sacco, ASST Fatebenefratelli-Sacco, Via G.B. Grassi 74, Milan, 20157, Italy, Tel +39 02 39041, Email [email protected]
Purpose: In Italy, musculoskeletal (MSK) disorders are pervasive with one-third of adults seeking medical consultation for a MSK issue in the past year. MSK pain is often treated with local heat applications (LHAs) which can be integrated into MSK care by different specialists and in different settings. Compared to analgesia and physical exercise, LHAs have been less evaluated, and the quality of randomized clinical trials is generally low. The aim of the survey is to assess the knowledge, attitude, perception/practices of general practitioners (GPs), physiatrists and sports medicine doctors towards thermotherapy as delivered by superficial heat pads or wraps.
Patients and Methods: The survey was conducted between June and September 2022 in Italy. An online questionnaire with 22 multiple-choice questions was administered to explore the demographics and prescribing habits of the participants; the clinical profile of MSK patients; and physicians’ attitude and beliefs about the use of thermotherapy/superficial heat applications in MSK pain management.
Results: GPs are at the forefront of the MSK patient journey and preferentially select NSAIDs as first-line option in arthrosis, muscle stiffness, and strain while prescribing heat wraps as preferred choice in presence of muscle spasm/contracture. Similar pattern of prescribing habits was found among specialists who, in contrast to GPs, adopted more frequently ice/cold therapy to relieve pain due to muscle strain and limited paracetamol use. Generally, survey participants agreed on the benefits of thermotherapy in MSK care management, namely increased blood flow and local tissue metabolism as well as connective tissue elasticity and pain relief which all may be of help in attaining pain control and improvement of function.
Conclusion: Our findings provided the basis for further investigations aimed at optimizing the MSK patient journey while building up additional evidence supporting the benefit of using superficial heat applications to effectively manage patients with MSK disorders.
Keywords: musculoskeletal disorder, superficial heat therapy, general practitioner, heat pads, heat wraps
Introduction
Musculoskeletal (MSK) conditions are leading contributors to severe long-term pain, disability, and sick leave as well as common reasons to seek medical advice. It is presumably a dramatic increase in the disease burden of these conditions on both individuals and society in the next few years due to the aging population.1,2 To date, the latest estimates on a global level indicate there were over a billion prevalent cases and almost 140 million disability-adjusted life years (DALYs) due to MSK disorders in 2017.1 MSK conditions may differ in terms of pathophysiology despite they share similar anatomical and clinical profiles characterized by pain and functional impairments. MSK disorders significantly impair patients’ health-related quality of life (HRQoL) and contribute to high direct and indirect healthcare costs.3
The earlier MAPPING study provided the first evidence that in Italy MSK disorders were pervasive in the general adult population with at least one-fourth of individuals suffering from MSK pain4 and with one-third of the adult population seeking medical consultation for a musculoskeletal issue in the past year.5 More recent studies on chronic pain (CP) management revealed that in our country over 70% of CP is MSK within primary care settings,6 with low back pain (LBP) and osteoarthritis (OA) being the most frequent reason for patient referral by general practitioners (GPs) to second-level pain centers.7 The burden is also economic as the annual average cost of treating a patient with chronic MSK pain has been reported equal to €212.60.8 Therefore, greater efforts should be placed to improve MSK care and ensure to patients suffering from MSK disorders the access to adequate MSK treatment.
MSK pain is managed by a wide range of treatment options, most delivered in primary care by first-contact clinicians, such as GPs;9 nevertheless, MSK care is unique because patients can seek advice from physicians with various subspecialty backgrounds10 such as physiatrists, sport medicine doctors, rheumatologists. For instance, MSK patients with substantial impairments may preferentially self-refer or are referred by GPs to physiatrists.10 As GP and specialists have crucial role in the diagnosis and management of MSK pain, assessment of their knowledge, attitude, and prescribing habits toward pain management is paramount.
MSK pain is often treated with local heat applications (LHAs) and superficial heat therapy stands as a well-tolerated therapeutic option that can be integrated into the treatment of MSK pain by different specialists and in different settings (hospital, home, rehabilitation clinics) and when used correctly, it does not bear negative effects.11 However, compared to other therapeutic approaches such as analgesia and physical exercise, LHAs have been less frequently evaluated, and the quality of randomized clinical trials is generally low. Moreover, the relevant clinical and methodological heterogeneity within the trials did preclude statistical pooling of effect estimates while no evidence has been accumulated so far regarding specific patient subgroups which might benefit most from such an approach.9 Therefore, physicians should primarily rely on their clinical experience when selecting the most appropriate MSK treatment option. Of note, expert consensus recommendations may provide guidance when objective clinical data are lacking.
A recent Delphi study attempted to reach a consensus among 116 European physicians on the place in role of heat therapy in MSK care.12 Most panelists agreed on the indication of superficial heat therapy in MSK pain management, particularly in non-specific LBP,13 chronic MSK pain, mechanical pain, delayed-onset muscle soreness (DOMS), strain, and sprain during rehabilitation (or after the acute phase of rehabilitation).12
Given the burdensome prevalence of MSK pain among the general population in our country4–6 and the clinical relevance of integrating noninvasive, inexpensive, and well-tolerated options in the therapeutic armamentarium physicians refer to when managing patients with MSK disorders, it is important to investigate the Italian physicians’ knowledge, beliefs, and prescribing habits, with a focus on local heat applications. Therefore, this exploratory survey aimed to assess the knowledge, attitude, perception/practices of healthcare providers, most involved in MSK patients’ care such as GPs14 and specialists like physiatrists and sports medicine doctors, towards thermotherapy as delivered by superficial heat pads or wraps.
Materials and Methods
Survey
The present survey was conducted between June and September 2022 in Italy. The physicians were administered an online questionnaire, developed by EDRA SpA (Milan, Italy), through a Computer-Aided Web Interview (CAWI) using the free software SurveyMonkey. An invitation was sent by e-mail to 26,000 Italian physicians registered in an online, EDRA-managed, platform MediKey (https://ssl.medikey.it/about.aspx): 455 (1.3%) accepted to participate and returned a completed questionnaire. No specific exclusion/inclusion criteria were established as the scope of the survey is to provide an as-much-comprehensive-as-possible overview of the Italian scenario. Answers were collected on an anonymous basis. The questionnaire comprised 22 multiple-choice questions (Q) addressing the following items: a) participant demographics (Q1-Q3); b) clinical profile of the patients encountered by the participant physicians in their daily practice (Q4-Q11); c) therapeutic approach and prescribing habits of physicians when dealing with patients with MSK pain (Q12-Q16); d) physician attitude and beliefs about the place in therapy of thermotherapy/superficial heat applications in MSK pain management (Q17-Q22). Of note, participants were asked to rate their agreement to items regarding the use and associated benefits of superficial heat applications in MSK pain patients from 0 to 4 (0, complete disagreement; 4, complete agreement) on a 4-point Likert-type scale. A full description of the questionnaire is provided in the Supplementary Materials.
The participants were made aware that the survey was sponsored by a pharmaceutical company and received a small incentive (eg, two EDRA-edited manuals on physical medicine and rehabilitation and soccer game physician, respectively) for the participation in the study. All participants provided voluntary, informed consent to data collection and use, based upon a clear understanding of the purpose of the data collection. The questionnaire was performed, and ethical issues were addressed, following the Code of Conduct of the European Pharmaceutical Market Research Association (EphMRA) [European Pharmaceutical Market Research Association (EphMRA). Code of Conduct. 2022. https://www.ephmra.org/sites/default/files/2022-08/EPHMRA%202022%20Code%20of%20Conduct.pdf. Accessed 4 Nov 2022.]. As indicated by Article 1.3 of the EphMRA Code of Conduct, this market research study did not require Clinical Research Ethics Committee or Independent Review Board approval. No personal data were collected, and all participants remained anonymous throughout the study.
Data Analysis
All data are presented descriptively as mean ± standard deviation, median (range), or percentage of valid cases. Since results in the physiatrist and sports medicine doctor groups were not significantly different, only the aggregated results are presented.
The Pearson’s chi-squared test was performed to assess differences between GP and other specialist’s prescription habits. Statistical analyses were performed using Stata version 16.0 (Stata Corporation, College Station, TX, USA). All tests were two-sided and p-values < 0.05 were conventionally regarded to as statistically significant.
Results
Demographic characteristics and clinical practice attendance of the survey participants are described in Table 1. In total, 455 physicians completed the questionnaire with the majority (61%) being general practitioners (n=276) and more than one-third (39%) being specialists in physiatry and sports medicine (n=179) (Q1). Overall, most survey participants reported > 20 years of medical practice thus suggesting that the sample population is 45–65 years old (Q3).
 |
Table 1 Characteristics of Survey Participants (n=455). The Data are Expressed as Mean or Percentage |
In line with the high frequency of primary care consultations for a MSK pain-related problem documented in other European countries, the surveyed GPs reported that patients in their daily practice would seek advice for MSK pain often (42%) or always (56%) (Q4).
In line with the role of GPs as first-contact physicians in MSK pain care, among the patients referring to the surveyed GPs for MSK pain only 7% of them are naïve patients in terms of seeking medical help, dealing with their pain only with self-medications. On the contrary 5% of the patients had already attempted one or more trials of analgesic treatment, and 64% tried both analgesic treatments and self-medications (Q5). Of note, more than one-fourth of patients visiting specialists (27%) have been already received an analgesic prescription thus presumably seeking an improvement of their current MSK pain care.
Arthrosis and poor posture are listed among the most frequent pain causes as reported by the patients, encountered by both GPs and specialists in daily practice, with GPs also taking care of patients with demanding work while specialists are also focused on pain related or stemming from intense/prolonged physical exercise (Q9). MSK pain can be either of traumatic (eg, contusions, sprains, fractures) or non-traumatic origin (eg, spine, joint, and tendon disorders). Musculoskeletal injuries and the associated pain of traumatic origin are more frequently reported by specialists in young patients (18–40 years) while middle-aged patients (40–65 years) are more frequently visiting GPs to seek medical advice (Q10). In contrast, MSK pain of non-traumatic origin impacts primarily middle-older age patients (Q11). As MSK conditions are linked anatomically, it is relevant to identify the most frequent anatomical sites of MSK pain as reported by the patients. As shown in Figure 1, patients visiting GPs reported low back as the most frequent anatomical site of MSK pain followed by the cervical region, shoulder, and knee. Similar results were also found among patients encountered in daily practice by specialists such as physiatrists and sport medicine doctors (Q6).
The primary goals of MSK care are the control of pain and its related symptoms and the improvement of function and QoL.15 To pursue such objectives, physicians may rely on a wide range of treatment options, including pharmacological, non-pharmacological and surgical procedures.9 Nevertheless, physicians prescribing habits may differ depending on the cause of pain, the presence of comorbidities and the occurrence of injuries following work or athletic activities. Therefore, the choice of MSK pain treatment in a patient reporting muscle stiffness may differ from that in a patient suffering from a strain or muscle contracture.
Figure 2 illustrates the prescribing habits of GPs and specialists when managing patients with MSK pain. GP prescription preferences significantly differed from specialists’ habits only regarding the initial management of pain due to muscle fatigue/stiffness (Q12, p-value<0.001), muscle strain (Q13, p-value<0.001), contracture pain (Q14, p<0.001), arthrosis pain (Q16, p-value<0.001) and in the presence of trigger point (Q15, p-value<0.001).
More in details, GPs preferred different treatment options based on the cause of MSK pain. NSAIDs and rest were chosen as first-line approaches when dealing with patients reporting muscle stiffness/fatigue and muscle strain followed by paracetamol and heat wraps in the former and heat and therapeutic cooling in the latter.
Among the physiological effects of superficial heat applications, changes in elasticity of connective tissue, reduction in muscle spasms and the subsequent increase in range of motion (ROM) may be of help in managing a muscle contracture.11,16–18 In line with this, GPs selected heat wraps as the first-line choice in presence of a muscle contracture, followed by rest, NSAIDs and paracetamol. Chronic MSK disorders are often associated with the presence of discrete, focal, hyperirritable spots located in a taut band of skeletal muscle which produces pain locally thus resulting in a decreased ROM of the affected muscles. Of note, patients with trigger points may benefit from a multimodal treatment plan including dry needling and manual therapy techniques.19,20 In line with this, manual procedures were selected as first-line approach by GPs and, along with needling, stand as the most frequent therapeutic approach. Interestingly, superficial heat applications were also reported to be chosen as the first-line option thus suggesting that GPs may be aware that the local heating of trigger points holds promise in providing pain relief in MSK pain such as neck and plantar.21 Comparing the answers obtained GPs working in medical practice for more than 20 years (87% of the sample, n=237) and GPs working for less than 20 years (13%, n=36), the observed prescription attitude for pain management was similar in both groups (Figure 1S). However, the sample size is too small to hypothesize any patterns or correlations.
Rest was often chosen among the first approach by the specialists dealing with patients reporting muscle stiffness, strain, and contracture along with either NSAIDs (muscle stiffness) or ice/cold therapy (muscle strain) or heat wraps (muscle contracture). In agreement with the GPs’ prescribing habits, specialists selected heat wraps as the first choice in presence of muscle contracture and, among the first options along with manual procedures, in presence of trigger point. Interestingly, specialists did favor ice/cold therapy and rest when treating a patient with a muscle strain instead of prescribing NSAIDs as more commonly observed among GPS.
As reported in Table 1, arthrosis stands as the primary cause of pain leading patients with MSK pain to seek medical advice. NSAIDs represent the first line choice regardless of medical specialization followed by paracetamol which is prescribed more frequently by GPs than specialists (Figure 2S).
Improvement of muscle flexibility, increased blood flow and metabolism and contribution to the healing process have been recently ascribed among the benefits of heat application on muscle in a recent Delphi study.12 In line with this, both GPs and specialists indicated increased blood flow and local tissue metabolism among the benefits of thermotherapy along with pain relief and augmented connective tissue flexibility (Q20 - Figure 3A). Interestingly, most physicians, regardless of medical specialization, would mostly employ thermotherapy in combination with pharmacological and non-pharmacological treatments thus supporting the use of superficial heat therapy as part of a multimodal approach to pain (Q18 - Figure 3B).12
 |
Figure 3 Benefits of thermotherapy as perceived by GP and specialists (A) and its use as part of multimodal approach to MSK pain (B). |
Superficial heat therapy is indicated mostly in chronic MSK pain when secondary causes (including non-specific LBP) are excluded12,13 while being not indicated in acute inflammatory joint pain. To better explore which types of MSK pain could be eligible for heat treatment and assess physician perception of the timing and modalities of heat treatment physicians were also asked to rate their agreement about the rationale for use of thermotherapy in MSK pain. As shown in Figure 4A (Q21), regardless of medical specialty, most physicians much agreed on the indication of thermotherapy in MSK pain, even chronic, by its ability in promoting muscle stretching and the rest as well as in altering pain perception. As shown in Figure 4B (Q17), both GPs and specialists much agreed that during the treatment of traumatic pain. No statistically significant differences between GP and specialists were found concerning the utility of thermotherapy after having treated a trauma with the ice/cold application for 48–72h (Q17, p-value=0.161) and the use of heating bands/patches in relation to other therapies (Q18, p-value=0.106). However, differences in the frequency of suggesting the use of heating bands/patches were found (Q22, p-value=0.006).
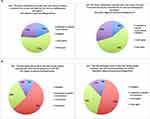 |
Figure 4 Level of agreement about the rational of use of thermotherapy (A) and its benefits following ice/cold application in traumatic pain (B). |
Discussion
Our exploratory survey in a sample population of Italian physicians provides the first preliminary evidence of the degree of knowledge, attitude and prescribing habits when managing patients seeking their advice for MSK pain and unveils some concordance between physicians’ behavior and guidelines/expert consensus recommendations about the clinical relevance of superficial heat applications in MSK care.
MSK disorders commonly prompt most patients to seek treatment and contribute significantly to the most frequent pain complaints presented to primary care.22–24 Irrespective of their etiology, MSK disorders, and the associated pain and functional impairment are major sources of suffering and require appropriate and timely care. In addition, MSK pain is often multifactorial with not all patients having the same symptoms or rate of disease progression. Therefore, MSK disorders care is challenging despite the wide availability of drugs and non-pharmacological interventions. To date, the latest edition of the International Classification of Diseases (ICD-11)25 distinguishes chronic MSK pain into chronic primary MSK pain and chronic secondary MSK pain, of which the former is mostly encountered in primary care. In Italy, general practice is the gatekeeper to the health service and GPs are uniquely placed to both provide first-level of care and to deliver coordinated management of MSK disorders through referral and collaboration with specialists frequently consulted by patients suffering from MSK pain such as physiatrists and sports medicine doctors. Therefore, gathering information about the Italian physicians’ knowledge, beliefs, and prescribing habits in MSK care may aid in optimizing existing therapeutic approaches as well as identifying barriers to adequate MSK care. In this scenario, our focus on the local heat applications relies on the observation that, despite their frequent use in clinical practice and the conditional recommendation for patients with knee, hip and/or hand OA26 or the strong recommendation in acute and subacute non-specific LBP,27 such approach has been less frequently evaluated compared to pain medications or physical therapy and is currently characterized by limited scientific evidence.
In line with previous studies,9,28 our findings confirm that GPs are at the forefront of the MSK patient journey, mostly taking care of the initial therapy prescription as less than 10% of their patients were already experiencing a trial of analgesic treatment. In line with previous reports indicating NSAIDs as the dominant prescription for MSK pain in primary care,28,29 Italian GPs preferentially select NSAIDs as first-line option in arthrosis, muscle stiffness, and strain while prescribing heat wraps as preferred choice in presence of muscle spasm/contracture. The latter choice would acknowledge GPs’ understanding of the physiological effects of superficial heat applications, particularly those relevant in case of muscle contracture such as the changes in elasticity of connective tissue and the reduction in muscle spasms.16–18 A similar pattern of prescribing habits can be found among specialists who, in contrast to GPs, adopted more frequently ice/cold therapy to relieve pain due to muscle strain and limited paracetamol use. After an acute injury, ice could be used to minimize swelling for the first two to three days. Therefore, icing rationale of use lies upon the premise that it eases pain, reduces tissue metabolism, and modifies vascular responses to decrease swelling.30 Once the swelling has subsided, heat could be used to increase blood flow and speed up the natural healing process. Knowing exactly when to use heat or ice can shorten recovery time and help with chronic aches, pains, and stiffness. To date, the greater rate of paracetamol use among GPs could be the result of the large clinical experience with this drug over the years, even in special populations like the elderly who are the most frequent age group referring to GPs for MSK pain of non-traumatic origin. Nevertheless, although paracetamol use has been long debated due to liver toxicity (albeit at doses higher than 4g/day), it is still recommended by guidelines for the treatment of multiple painful conditions.31
Our findings highlight a general agreement among survey participants regarding the benefits ascribed to thermotherapy in MSK care management with increased blood flow and local tissue metabolism as well as connective tissue elasticity and pain relief which all help address the primary goals in MSK care, namely the pain control and the improvement of function. To date, the increased blood flow and the related enhanced tissue metabolism can accelerate the healing process while changes in connective tissue were found to improve the ROM and enhance tissue extensibility.13,16,18,32
The latest ICD-11 combined the underlying mechanisms of CP with early MSK disorders to provide a more accurate epidemiological analysis of diseases characterized by MSK pain. Such changes are expected to allow for a more patient-centered management, not only pathophysiology-driven by disease, and to reinforce the need for a multimodal treatment approach to pain.33 In line with this concept, most physicians used thermotherapy in combination with pharmacological and non-pharmacological treatments thus supporting its use as a key component of a multimodal approach to MSK pain and underlying its relevance as a useful adjunct to pain medication and/or physical therapy.12
Our work has several limitations. First, we obtained a response rate of less than 2% (455 completed questionnaires/26,000 email invitations). Therefore, the sample may not be representative of all Italian physicians treating patients with MSK pain, and the findings here reported may not entirely mirror the clinical management seen in routine practice. Additionally, the majority of the responders (81%) was represented by physicians who had been practicing for >20 years; hence they could not be representative of the younger generation prescribing attitude towards pain management.
However, the low response rate may underscore an insufficient engagement, in such type of investigation, of the physicians interested in MSK patient care and in complementary non-pharmacological approaches like thermotherapy. To this end, in the future, the recruitment of participating physicians could benefit from alternative media channels beyond email invitations, like social media campaigns aimed at increasing physicians’ awareness and increasing the engagement of a younger population about the therapeutic potential of thermotherapy in MSK patient care alongside analgesic medications and physical therapy.
Second, the questionnaire was designed to cover specific aspects of interest, which limits the comparability with studies using standardized questionnaires. Furthermore, the questionnaire has not been validated; hence comparisons with other studies are difficult. Nevertheless, our preliminary findings provide the basis for a more structured investigation while encouraging a change in physicians’ engagement in such research through the enrollment among the members of the corresponding scientific societies or specific awareness campaigns mostly targeting young generations of physicians who are almost absent within our sample population. Finally, this is a convenient national sample of GPs and specialists and may not be generalizable to other countries where patterns of care and treatment options are different.
Conclusion
Our survey gathered information on the perceived impact of thermotherapy on MSK pain management from first-contact physicians, namely GPs, to those specialists who more frequently encounter MSK pain patients in their daily practice routine. Assessing the attitude and the prescribing habits from the perspective of the physicians mostly engaged in MSK care has provided important, albeit preliminary, insights into the challenges experienced and the beliefs that may hinder MSK care. Collectively, our findings provided the basis for further investigations aimed at optimizing the MSK patient journey while building up additional evidence supporting the benefit of using superficial heat applications to effectively manage patients with MSK disorders.
Acknowledgments
Writing and editing assistance, including preparation of a draft manuscript under the direction and guidance of the authors, incorporation of author feedback, and manuscript submission, was provided by EDRA, with the helpful support of Chiara Degirolamo, PhD, and supported by an unconditioned grant from Angelini Pharma.
Disclosure
Dr Fabrizio Gervasoni reports personal fees from Edra S.p.A., during the conduct of the study; personal fees, non-financial support from Edi Ermes, personal fees from Angelini Holding S.p.A., personal fees, non-financial support from Springer Healthcare Italia S.r.l., personal fees from Sanofi, personal fees from Bookia s.r.l., personal fees from Agence Compact, personal fees, non-financial support from Affidabile Formazione Continua S.r.l., personal fees from Edra S.p.A., personal fees from Dynamicom Education s.r.l., personal fees from Ibsa, personal fees from AlfaSigma, personal fees from Carocci Editore S.p.A., personal fees from Aretré S.r.l., personal fees from GlaxoSmithKline Consumer Healthcare S.r.l. Unipersonale, personal fees from SUMMEET S.r.l., personal fees from DOCEO ECM Educazione continua in Medicina S.r.l., personal fees from H-FARM S.p.A., personal fees from Mast&r S.r.l., personal fees from Ma.CRO Lifescience S.r.l., personal fees from SIMFER - Società Italiana di Medicina Fisica e Riabilitativa, personal fees from Italfarmaco, personal fees, non-financial support from I-TECH Medical Division (I.A.C.E.R.), personal fees, non-financial support from Podartis, grants from Società Aziende Chimiche Riunite Angelini Francesco A.C.R.A.F. S.p.A., outside the submitted work; Dr Massimiliano Franco reports grants from edra, outside the submitted work. Dr Alberto Magni reports grants from Pfizer, grants from Grunenthal, grants from MSD, grants from Mundipharma, grants from Angelini, outside the submitted work. This work was carried out thanks to an unconditioned grant from Angelini Pharma. The authors report no other conflicts of interest in this work.
References
1. Safiri S, Kolahi AA, Cross M, et al. Prevalence, deaths, and disability-adjusted life years due to musculoskeletal disorders for 195 countries and territories 1990–2017. Arthritis Rheumatol. 2021;73(4):702–714. doi:10.1002/art.41571
2. Moradi-Lakeh M, Forouzanfar MH, Vollset SE, et al. Burden of musculoskeletal disorders in the eastern mediterranean region, 1990–2013: findings from the global burden of disease study 2013. Ann Rheum Dis. 2017;76(8):1365–1373. doi:10.1136/annrheumdis-2016-210146
3. Beaudart C, Biver E, Bruyère O, et al. Quality of life assessment in musculo-skeletal health. Aging Clin Exp Res. 2018;30(5):413–418. doi:10.1007/s40520-017-0794-8
4. Salaffi F, De Angelis R, Grassi W. MArche Pain Prevalence; INvestigation Group (MAPPING) study. Prevalence of musculoskeletal conditions in an Italian population sample: results of a regional community-based study. I. The MAPPING study. Clin Exp Rheumatol. 2005;23(6):819–828.
5. Salaffi F, De Angelis R, Stancati A, et al. MArche Pain; Prevalence INvestigation Group (MAPPING) study. Health-related quality of life in multiple musculoskeletal conditions: a cross-sectional population based epidemiological study. II. The MAPPING study. Clin Exp Rheumatol. 2005;23(6):829–839.
6. Camilloni A, Nati G, Maggiolini P, et al. Chronic non-cancer pain in primary care: an Italian cross-sectional study. Signa Vitae. 2021;17(2):54–62.
7. Vittori A, Petrucci E, Cascella M, et al. Pursuing the recovery of severe chronic musculoskeletal pain in Italy: clinical and organizational perspectives from a SIAARTI survey. J Pain Res. 2021;14:3401–3410. doi:10.2147/JPR.S328434
8. Garattini L, Koleva D, Motterlini N, et al. Medical costs of chronic musculoskeletal pain in Italy. Clin Drug Investig. 2007;27(2):139–148. doi:10.2165/00044011-200727020-00007
9. Babatunde OO, Jordan JL, Van der Windt DA, et al. Effective treatment options for musculoskeletal pain in primary care: a systematic overview of current evidence. PLoS One. 2017;12:e0178621. doi:10.1371/journal.pone.0178621
10. Cheng AL, Calfee R, Colditz G, et al. PROMIS physical and emotional health scores are worse in musculoskeletal patients presenting to physiatrists than to other orthopedic specialists. PM R. 2019;11(6):604–612. doi:10.1002/pmrj.12068
11. Clijsen R, Stoop R, Hohenauer E, et al. Local heat applications as a treatment of physical and functional parameters in acute and chronic musculoskeletal disorders or pain. Arch Phys Med Rehabil. 2022;103(3):505–522. doi:10.1016/j.apmr.2021.06.015
12. Lubrano E, Mazas PF, Freiwald J, et al. An international multidisciplinary delphi-based consensus on heat therapy in musculoskeletal pain. Pain Ther. 2022;12:93–110. doi:10.1007/s40122-022-00419-4
13. Freiwald J, Magni A, Fanlo-Mazas P, et al. A role for superficial heat therapy in the management of non-specific, mild-to-moderate low back pain in current clinical practice: a narrative review. Life. 2021;11:780. doi:10.3390/life11080780
14. Margham T. Musculoskeletal disorders: time for joint action in primary care. Br J Gen Pract. 2011;61(592):657–658. doi:10.3399/bjgp11X601541
15. El-Tallawy SN, Nalamasu R, Salem GI, et al. Management of musculoskeletal pain: an update with emphasis on chronic musculoskeletal pain. Pain Ther. 2021;10(1):181–209. doi:10.1007/s40122-021-00235-2
16. Malanga GA, Yan N, Stark J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad Med. 2015;127(1):57–65. doi:10.1080/00325481.2015.992719
17. Petrofsky JS, Laymon M, Lee H. Effect of heat and cold on tendon flexibility and force to flex the human knee. Med Sci Monit. 2013;19:661–667. doi:10.12659/MSM.889145
18. Nadler SF, Weingand K, Kruse RJ. The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain Physician. 2004;7(3):395–399. doi:10.36076/ppj.2004/7/395
19. Barbero M, Schneebeli A, Koetsier E, et al. Myofascial pain syndrome and trigger points: evaluation and treatment in patients with musculoskeletal pain. Curr Opin Support Palliat Care. 2019;13(3):270–276. PMID: 31313700. doi:10.1097/SPC.0000000000000445
20. Fernández-de-Las-Peñas C, Simons D, Cuadrado ML, et al. The role of myofascial trigger points in musculoskeletal pain syndromes of the head and neck. Curr Pain Headache Rep. 2007;11(5):365–372. PMID: 17894927. doi:10.1007/s11916-007-0219-z
21. Petrofsky J, Laymon M, Lee H. Local heating of trigger points reduces neck and plantar fascia pain. J Back Musculoskelet Rehabil. 2020;33(1):21–28. doi:10.3233/BMR-181222
22. Jordan KP, Jöud A, Bergknut C, et al. International comparisons of the consultation prevalence of musculoskeletal conditions using population-based healthcare data from England and Sweden. Ann Rheum Dis. 2014;73(1):212–218. doi:10.1136/annrheumdis-2012-202634
23. Gureje O, Von Korff M, Simon GE, et al. Persistent pain and well-being: a world health organization study in primary care. JAMA. 1998;280(2):147–151. doi:10.1001/jama.280.2.147
24. Mäntyselkä P, Kumpusalo E, Ahonen R, et al. Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain. 2001;89(2–3):175–180. doi:10.1016/S0304-3959(00)00361-4
25. Perrot S, Cohen M, Barke A, et al. The IASP task force for the classification of chronic pain. The IASP classification of chronic pain for ICD-11: chronic secondary musculoskeletal pain. Pain. 2019;160(1):77–82. doi:10.1097/j.pain.0000000000001389
26. Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American college of rheumatology/arthritis foundation guideline for the management of osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020;72(2):220–233. doi:10.1002/art.41142
27. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2017;166(7):514–530. doi:10.7326/M16-2367
28. Wiitavaara B, Fahlström M, Djupsjöbacka M. Prevalence, diagnostics and management of musculoskeletal disorders in primary health care in Sweden: an investigation of 2000 randomly selected patient records. J Eval Clin Pract. 2017;23(2):325–332. doi:10.1111/jep.12614
29. Brattwall M, Turan I, Jakobsson J. Musculoskeletal pain: prescription of NSAID and weak opioid by primary health care physicians in Sweden 2004–2008—a retrospective patient record review. J Pain Res. 2010;3:131–135. doi:10.2147/jpr.s12052
30. Singh DP, Barani Lonbani Z, Woodruff MA, et al. Effects of topical icing on inflammation, angiogenesis, revascularization, and myofiber regeneration in skeletal muscle following contusion injury. Front Physiol. 2017;8:93. doi:10.3389/fphys.2017.00093
31. Freo U, Ruocco C, Valerio A, et al. Paracetamol: a Review of Guideline Recommendations. J Clin Med. 2021;10:3420. doi:10.3390/jcm10153420
32. Freiwald J, Hoppe MW, Beermann W, et al. Effects of supplemental heat therapy in multimodal treated chronic low back pain patients on strength and flexibility. Clin Biomech. 2018;57:107–113. doi:10.1016/j.clinbiomech.2018.06.008
33. Zuang J, Mei H, Fang F, et al. What is new in classification, diagnosis and management of chronic musculoskeletal pain: a narrative review. Front Pain Res. 2022;3:937004. doi:10.3389/fpain.2022.937004
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


