Back to Journals » Orthopedic Research and Reviews » Volume 16
Morphologic Evaluation of the Patella: The Impact of Gender and Age
Authors Nguyen TT , Le HDT, Hoang NT , Le TB , Ha TH
Received 30 October 2023
Accepted for publication 8 February 2024
Published 14 February 2024 Volume 2024:16 Pages 59—66
DOI https://doi.org/10.2147/ORR.S444533
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Thanh Thao Nguyen,1 Hoang Di Thu Le,2 Ngoc Thanh Hoang,1 Trong Binh Le,1 Thi Hien Ha1
1Department of Radiology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam; 2Department of Radiology, Oncology Hospital, Da Nang, Vietnam
Correspondence: Thanh Thao Nguyen, Department of Radiology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam, Email [email protected]
Introduction: The patellofemoral joint is a complex joint that plays a crucial role in knee joint function and stability. This study aims to describe the MRI characteristics of the patellofemoral joint in Vietnamese adults.
Subjects and Methodology: A cross-sectional study was conducted on 280 patients at Hue UMP Hospital from May 2020 to May 2021. All patients underwent knee MRI using Siemens Magnetom Amira 1.5 Tesla. The evaluation parameters included the morphology of the patella and the femoral trochlea.
Results: The study found that the morphological parameters of the patellar joint varied significantly between genders and age groups. The mean largest patellar transverse diameter was 4.26 ± 0.37 cm, the average length of the lateral joint facet was 2.5 ± 0.26 cm, and the medial joint facet was 2.0 ± 0.25 cm. The patellar height was 4.07 ± 0.35 cm. The indexes of patellar morphology were higher in men than in women, except for the lateral-medial facet ratio. The most common Wiberg classification was type B (63.9%), followed by type C (25.4%), and type A was the least common (10.7%). There was a statistically significant difference in the patellar measurements between different age groups. There was a weak negative linear correlation between the dimensions of the largest transverse diameter, the length of the articular surface, the patellar articular angle, and the age of the patient. Additionally, there was a moderate inverse linear relationship between patellar height and patient age.
Conclusion: This study highlights the significant variations in patellar morphology based on gender and age. The findings emphasize the importance of careful assessment and consideration of these variations in the imaging evaluation of the patellofemoral joint.
Keywords: patellofemoral joint, anterior knee pain, patellar morphology, Vietnamese, Insall-Salvati ratio
Introduction
The patellofemoral joint is a complex joint in terms of both kinematics and balance, ensuring knee joint function and stability.1 Anterior knee pain is a common condition in clinical practice, accounting for 11–17% of all cases of knee pain.2,3 It is characterized by pain in the anterior knee, around the patella, which occurs during activities such as squatting, walking up and down stairs, or sitting with knees bent.4 This condition reduces the ability to perform daily activities and affects the quality of life.5,6 It can occur at any age, including in adolescents, middle-aged individuals, and the elderly.4,7 Women are two to three times more likely to experience this condition than men.8,9 Anatomical variations leading to joint or patellar instability have been linked to increased joint pressure, which in turn is associated with pathological changes in the surrounding soft tissues and symptoms of patellar pain.10,11
Anterior knee pain can be long-lasting and requires appropriate treatment if risk factors persist.8 Therefore, it is important for radiologists to scrutinize the morphology of the patellofemoral joint and the surrounding soft tissues when evaluating the joint. Additionally, clinicians dealing with these disorders must have a thorough understanding of the basic anatomy and biomechanics of the patellofemoral joint. Imaging techniques are frequently required to assess the patellar joint, determine the source of pain, and exclude associated pathologies.
Radiographs are typically the initial imaging method employed for patients experiencing knee pain. Magnetic resonance imaging (MRI) assists in examining the joint from various perspectives, assessing cartilage damage, and investigating soft tissue involvement. Certain research has indicated that ethnic variances may impact the morphological aspects of the patellar joint.12–14 Therefore, this study was undertaken to delineate the MRI features of the patellofemoral joint in Vietnamese adults.
Research Subjects and Methodology
A cross-sectional study involving 280 patients was conducted at the Hue University of Medicine and Pharmacy Hospital in Vietnam from May 2020 to May 2021. Patients who had undergone knee MRI were included. Patients who had undergone previous knee surgery, experienced trauma, or exhibited bone deformities in the joint area, those with tumor-like lesions in the soft tissue surrounding the joint, and individuals with severe osteoarthritis resulting in joint deformity were excluded.
All patients underwent knee MRI scans using a Siemens Magnetom Amira 1.5 Tesla, Siemens, Erlangen, Germany with a dedicated knee coil. Evaluation was performed by two radiologists, one with 20 years of experience and the other with 3 years of experience. If there is disagreement, they discuss the issue and conclude by consensus. The evaluation parameters encompassed the imaging morphology of the patella. Statistical analysis was done using IBM SPSS Statistics version 24. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the University of Medicine and Pharmacy, Hue University, Vietnam. Approval number: H2020/161. All patients gave written informed consent.
Morphologic Parameters
- Type A: the medial joint surface is concave and almost equal to the outer joint.
- Type B: the medial joint surface is concave and smaller than the outer joint.
- Type C: the medial joint is convex and much smaller than the outer joint.
Illustrations of the morphologic measurements and Wiberg classification are given in Figures 1 and 2.
Results
Demographics
The mean age of the study group was 39 ± 14.9. Individuals aged 21 to 40 years constituted the largest proportion at 46.8%. Furthermore, the mean age was significantly higher in women than in men (p < 0.05; Mann–Whitney U-test). Please refer to Table 1 for more details.
 |
Table 1 Demographic of Participants |
Patellar Morphology
The mean transverse diameter of the patella was 4.26 ± 0.37 cm. The average lateral facet was 2.5 ± 0.26 cm, while the average medial facet was 2 ± 0.25 cm. The mean patellar joint angle was 128.3 ± 8.20 degrees. The average patellar height was 4.07 ± 0.35 cm. The indices of patellar morphology in men were statistically significantly higher than in women (except for the ratio of lateral-medial facet) (p<0.05; t-test). Please refer to Table 2 for more details.
 |
Table 2 Patellar Morphologic Parameters |
According to Wiberg classification, patellar shapes in men and women were classified as follows: type A (9.3% and 12.3%), type B (62.7% and 65.4%), and type C (28% and 22.3%), respectively (Table 3). No significant difference was found in the classification between the two sexes.
 |
Table 3 Wiberg Classification of Patella |
Patellar Morphology with BMI and Age
There was no statistically significant difference when comparing patellar sizes between BMI groups (p>0.05) (Table 4). However, there was a statistically significant difference when comparing the transverse diameter, lateral and medial facet length, and patellar height between age groups. Specifically, the transverse diameter and lateral facet were greatest in the 21–40 age group and smallest in the 41–60 age group. The medial facet was greatest in the group of 21–40 years old and smallest in the group of ≤20 years old. The patellar height was greatest in the age group ≤20 years old and smallest in the 41–60 age group (p values < 0.05; ANOVA and Kruskal–Wallis tests). There was a weak negative linear correlation between the transverse diameter, the lateral facet, the patellar facet angle, and the patient’s age. There was a moderate inverse linear relationship between patellar height and patient age. Please refer to Table 5 and Table 6 for more details.
 |
Table 4 Patella and BMI |
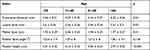 |
Table 5 Patella and Age |
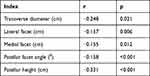 |
Table 6 Linear Correlation Between Patellar Indices and Age |
Insall-Salvati Ratio
The Insall-Salvati values of the study sample ranged from 0.52 to 1.41, with a mean of 0.96 ± 0.14. The Insall-Salvati ratio was statistically higher in women compared to men (p<0.05; t-test). 95.4% of patients had an Insall-Salvati ratio within the normal range. The percentage of patella alta was 0.4%, while the percentage of patella baja was 4.3%. Please refer to Table 7 for more details.
 |
Table 7 Insall-Salvati Ratio |
Discussion
Patellar Morphology
Our findings in the Vietnamese population align with previous studies indicating that Asians generally have thinner and smaller patella compared to Europeans.15–17 The mean value of the largest transverse diameter in our study is smaller than the results reported by Baldwin et al for the European population.18 Similarly, the mean patellar height in our study (4.3 ± 0.26 cm in men and 3.81 ± 0.26 cm in women) is smaller than the measurements in Koreans, Chinese, and Indians (Table 8).15,17,19
 |
Table 8 Comparison of the Largest Transverse Diameter and Patellar Height with the Results of Some Previous Studies |
In terms of gender differences, our study found that the sizes of the patella in men were larger than in women, except for the medial-lateral facet joint ratio. This finding is consistent with previous reports.15,16,18,20
According to the Wiberg classification, in our study type B was the most common type of patella in both men and women (62.7% and 65.4%). No significant difference was found in the classification between the two sexes. This distribution is consistent with previous studies.19,22
Our study did not find any difference in patellar sizes between BMI groups, nor did we observe a linear correlation between patellar sizes and BMI values. We observed differences in the transverse diameter, patellar height, and medial and lateral aspect length among different age groups. There is a weak negative linear correlation between patellar size and patient age, suggesting that the size of the patella slightly decreases with age, although the reason for this correlation remains unclear. This result aligns with a study by Prathum et al which found a correlation between age and morphological changes in the knee joint.23
Insall-Salvati Ratio
The position of the patella is crucial for the functioning of the patellar joint. Patella alta is associated with reduced joint contact, resulting in pain and instability of the patellar joint.24,25 Study by Leung et al demonstrated that the patella position of the Chinese population in the Northern region is approximately 15–20% higher than that of the Western population.26 This difference can be attributed to the long-term stretching of the patellar tendon resulting from common activities like squatting and kneeling in certain countries like India, China, Vietnam, and the Middle East.12,21,27,28
In our study, we observed that the Insall-Salvati ratio is higher in women compared to men, and this difference is statistically significant. The ratio for women and men in our study was 0.99 ± 0.13 and 0.93 ± 0.15, respectively. These results are consistent with other studies.21,29,30
Conclusion
This study highlights the significant variations in patellar morphology based on gender and age. The findings emphasize the importance of careful assessment and consideration of these variations in the imaging evaluation of the patellofemoral joint.
Ethical Statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the University of Medicine and Pharmacy, Hue University, Vietnam. Approval number: H2020/161. All patients gave written informed consent.
Acknowledgment
This work was supported by Hue University under the Core Research Program (Grant No. NCM.DHH.2020.09).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Loudon JK. Biomechanics and pathomechanics of the patellofemoral JOINT. Int J Sports Phys Ther. 2016;11(6):820–830.
2. Martinez-Cano JP, Ramos-Rivera JC, Gómez-García J, Casas–Barragán GA, Rosales MC, Escobar-Gonzalez SS. Anterior knee pain in runners after a half-marathon race. J Clinl Orthopaedics Trauma. 2021;23:101640. doi:10.1016/j.jcot.2021.101640
3. Phillips J, Coetsee M. Incidence of non-traumatic anterior knee pain among 11–17-years-olds. South Afr Sports Med Assoc. 2007;19. doi:10.17159/2078-516X/2007/v19i2a267
4. Sanchis-Alfonso V, Dye SF. How to deal with anterior knee pain in the active young patient. Sports Health. 2017;9(4):346–351. doi:10.1177/1941738116681269
5. Crossley KM, Callaghan MJ, van Linschoten R. Patellofemoral pain. Br J Sports Med. 2016;50(4):247–250. doi:10.1136/bjsports-2015-h3939rep
6. Collins NJ, Vicenzino B, van der Heijden RA, van Middelkoop M. Pain during prolonged sitting is a common problem in persons with patellofemoral pain. J Orthop Sports Phys Ther. 2016;46(8):658–663. doi:10.2519/jospt.2016.6470
7. Neal BS, Lack SD, Lankhorst NE, Raye A, Morrissey D, van Middelkoop M. Risk factors for patellofemoral pain: a systematic review and meta-analysis. Br J Sports Med. 2019;53(5):270–281. doi:10.1136/bjsports-2017-098890
8. Dutton RA, Khadavi MJ, Fredericson M. Patellofemoral Pain. Phys Med Rehabil Clin N Am. 2016;27(1):31–52. doi:10.1016/j.pmr.2015.08.002
9. Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725–730. doi:10.1111/j.1600-0838.2009.00996.x
10. Ali SA, Helmer R, Terk MR. Analysis of the patellofemoral region on MRI: association of abnormal trochlear morphology with severe cartilage defects. AJR Am J Roentgenol. 2010;194(3):721–727. doi:10.2214/AJR.09.3008
11. van Middelkoop M, Macri EM, Eijkenboom JF, et al. Are patellofemoral joint alignment and shape associated with structural magnetic resonance imaging abnormalities and symptoms among people with patellofemoral pain? Am J Sports Med. 2018;46(13):3217–3226. doi:10.1177/0363546518801314
12. Le Hoang Di T, Hoang Ngoc T, Ngo DHA, et al. Evaluation of the insall-salvati ratio among the Vietnamese population: application for diagnosis of patellar malalignment. Orthop Res Rev. 2021;13:57–61. doi:10.2147/ORR.S306316
13. Thomas S, Rupiper D, Stacy GS. Imaging of the patellofemoral joint. Clin Sports Med. 2014;33(3):413–436. doi:10.1016/j.csm.2014.03.007
14. Koh YG, Nam JH, Chung HS, et al. Gender-related morphological differences in sulcus angle and condylar height for the femoral trochlea using magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3560–3566. doi:10.1007/s00167-019-05423-4
15. Muhamed R, Saralaya VV, Murlimanju BV, Chettiar GK. In vivo magnetic resonance imaging morphometry of the patella bone in South Indian population. Anat Cell Biol. 2017;50(2):99–103. doi:10.5115/acb.2017.50.2.99
16. Shang P, Zhang L, Hou Z, et al. Morphometric measurement of the patella on 3D model reconstructed from CT scan images for the southern Chinese population. Chin Med J. 2014;127(1):96–101. doi:10.3760/cma.j.issn.0366-6999.20131948
17. Kim TK, Chung BJ, Kang YG, Chang CB, Seong SC. Clinical implications of anthropometric patellar dimensions for TKA in Asians. Clin Orthop Relat Res. 2009;467(4):1007–1014. doi:10.1007/s11999-008-0557-0
18. Baldwin JL, House CK. Anatomic dimensions of the patella measured during total knee arthroplasty. J Arthroplasty. 2005;20(2):250–257. doi:10.1016/j.arth.2004.09.027
19. Li Z, Liu G, Tian R, et al. The patellofemoral morphology and the normal predicted value of tibial tuberosity-trochlear groove distance in the Chinese population. BMC Musculoskelet Disord. 2021;22(1):575. doi:10.1186/s12891-021-04454-8
20. Yoo JH, Yi SR, Kim JH. The geometry of patella and patellar tendon measured on knee MRI. Surg Radiol Anat. 2007;29(8):623–628. doi:10.1007/s00276-007-0261-x
21. Upadhyay S, Raza HKT, Srivastava P. Position of the patella in adults in central India: evaluation of the Insall-Salvati ratio. J Orthop Surg. 2013;21(1):23–27. doi:10.1177/230949901302100108
22. Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):663–670. doi:10.1007/s00167-010-1329-4
23. Prathum S, Ayuthaya SS, Wangpiriyapanich K, et al. Morphological age changes in the knee joint in dry bone. Int Med J. 2018;25:181–185.
24. Ward SR, Powers CM. The influence of patella alta on patellofemoral joint stress during normal and fast walking. Clin Biomech. 2004;19(10):1040–1047. doi:10.1016/j.clinbiomech.2004.07.009
25. Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am. 2007;89(8):1749–1755. doi:10.2106/JBJS.F.00508
26. Leung YF, Wai YL, Leung YC. Patella alta in southern China. A new method of measurement. Int Orthop. 1996;20(5):305–310. doi:10.1007/s002640050083
27. Chen AF, Tetreault MW, Levicoff EA, Fedorka CJ, Rothenberg AC, Klatt BA. Increased incidence of patella baja after total knee arthroplasty revision for infection. Am J Orthop. 2014;43(12):562–566.
28. Neogi DS, Bae JH, Seok CW, Lim HC. Impact of patellar height on unicompartment knee arthroplasty: does patella baja lead to an inferior outcome? J Orthop Traumatol. 2014;15(1):47–54. doi:10.1007/s10195-013-0268-5
29. Hong HT, Koh YG, Nam JH, Kim P, Kwak YH, Kang KT. Gender differences in patellar positions among the Korean population. Appl Sci. 2020;10(24):8842. doi:10.3390/app10248842
30. Miller TT, Staron RB, Feldman F. Patellar height on sagittal MR imaging of the knee. AJR Am J Roentgenol. 1996;167(2):339–341. doi:10.2214/ajr.167.2.8686598
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


