Back to Journals » Infection and Drug Resistance » Volume 16
Molecular Profiling of a Multi-Strain Hypervirulent Klebsiella pneumoniae Infection Within a Single Patient
Authors Cao H, Liang S, Zhang C, Liu B, Fei Y
Received 24 January 2023
Accepted for publication 3 March 2023
Published 11 March 2023 Volume 2023:16 Pages 1367—1380
DOI https://doi.org/10.2147/IDR.S404202
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Huijun Cao,1,* Shiwei Liang,1,2,* Chenchen Zhang,2 Bao Liu,1 Ying Fei1
1Centre for Clinical Laboratories, the Affiliated Hospital of Guizhou Medical University, Guiyang, 550004, People’s Republic of China; 2School of Clinical Laboratory Science, Guizhou Medical University, Guiyang, 550004, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ying Fei, Email [email protected]
Background: The rising prevalence of infections caused by carbapenem-resistant and hypervirulent Klebsiella pneumoniae (CR-hvKP) has outpaced our understanding of their evolutionary diversity. By straining the antimicrobial options and constant horizontal gene transfer of various pathogenic elements, CR-hvKP poses a global health threat.
Methods: Six KP isolates (KP1~KP6) from urine, sputum and groin infection secretion of a single patient were characterized phenotypically and genotypically. The antimicrobial susceptibility, carbapenemase production, hypermucoviscosity, serum resistance, virulence factors, MLST and serotypes were profiled. Genomic variations were identified by whole-genome sequencing and the phylogenetic differentiation was analyzed by Enterobacterial repetitive intergenic consensus (ERIC)-PCR.
Results: All KP strains were multi-drug resistant. Four of them (KP1, KP3, KP5 and KP6) belonged to ST11-K64, with high genetic closeness (relatedness coefficient above 0.96), sharing most resistance and virulence genes. Compared with KP1, the later isolates KP3, KP5 and KP6 acquired blaKPC-1 and lost blaSHV-182 genes. KP2 and KP4 had the same clonal origin of ST35-K16 (relatedness coefficient 0.98), containing almost identical genes for resistance and virulence. They were non-mucoid and carried blaNDM-5 gene.
Conclusion: A co-infection with two types of CR-hvKP affiliated with different clades within a single patient amplified the treatment difficulties. In addition to source control and epidemiological surveillance, investigation of the in-host interactions between CR-hvKP variants may provide valuable treatment solutions.
Keywords: Klebsiella pneumoniae, carbapenem-resistance, virulence, ST11-K64, ST35-K16, MLST, whole-genome sequencing
Introduction
Klebsiella pneumoniae (KP) is a common gram-negative bacillus ubiquitously present in natural environment and different hosts. KP also constitutes the normal flora of human mucosal surfaces such as intestine, skin and nasopharynx.1 Community-acquired or nosocomial KP has emerged as one of the principal pathogens of infectious diseases including pneumonia, urinary tract infections, sepsis, liver abscesses, purulent pericarditis, and wound site infections.2–4
Decades of extensive use of antimicrobials has facilitated the rapid evolvement and dissemination of KP that produces extended-spectrum ß-lactamases (ESBLs) and carbapenemases (KPCs). These are enzymes that break down the entire last line of weapons against infectious diseases, by hydrolysing ß-lactams, fluoroquinolones and aminoglycosides, as well as penicillins, cephalosporins and monobactams, etc.5,6 Primary mechanisms adopted by carbapenem-resistant KP (CR-KP) to deactivate carbapenems are classified into the Ambler classes A (KPC), B (the metalloenzymes NDM, VIM and IMP) and D (oxacillin enzyme, OXA).4
The morbidity and mortality of KP infection are also dictated by its virulence. An arsenal of virulence factors such as capsule, lipopolysaccharide (LPS), siderophore, urease and fimbriae, manifest as phenotypic traits of adherence, immune evasion, hypermucoviscosity and nutrients scavenge. High virulence equates to greater ability of bacterial invasion, survival and proliferation.7 The distinct antigenic capsular polysaccharide of different strains has been utilized for serotype classification. From the normally opportunistic classical KP strains (cKP), the versatile evolution of KP has prompted the differentiation of hypervirulent KP (hvKP). Although the distinction between them is less definitive and tends to become blurred, they often differ in demographic and clinical distribution propensity. While the elderly people and hosts with comorbidities such as immunosuppression, diabetes mellitus and chronic renal insufficiency are at a greater risk for severe, sometimes even fatal infection of cKP, hvKP infection significantly affects younger and otherwise healthy population.3 Infections with hvKP are more often emanated from community exposure, bearing a high geographical variation (higher in Taiwan and China than in western countries and Europe).8 Besides, hvKP more likely possesses elevated iron acquisition systems and causes more metastatic phenotypes including multiple-site infection and debilitating syndromes.9–11 Although the terms hypermucoviscous KP (hmKP) and hvKP are often interchangeably used, researchers have found that mucoviscosity cannot be sufficiently used to infer hypervirulence.9 Instead, genotypic delineation of virulent factors such as iucA, iroB, peg-344, prmpA and prmpA2, and their combination patterns, are more accurate.12,13
In recent years, carbapenem-resistant hypervirulent KP (CR-hvKP) emerges and thrives on the convergence of both the drug resistance- and hypervirulence-encoding elements through plasmid fusion or conjugation.14 CR-hvKP has been relentlessly impoverishing our last resort of antimicrobials and is showing an alarming trend to disseminate from Asian pacific rim to the whole globe to cause intractable infections in individuals of all ages.3,10 While an accurate prevalence of CR-hvKP as an infectious agent is hard to measure, due to the lack of standardised diagnostic markers, devastating regional outbreaks of CR-hvKP in healthcare facilities have been reported around the world.15–20 In particular, CR-hvKP is a major cause for ventilator-associated pneumonia, with a very high mortality rate. ICU, where tracheostomy and other indwelling medical devices are regularly applied, represents a unique niche in favour of biomaterial-associated infections. Opportunistic bacteria in this environment, predominantly KP strains, can aggregate and embed themselves in a thick layer of self-produced extracellular biofilm matrix. The adherence of the biofilms to biotic or abiotic surfaces protects the bacteria from host defence and bactericidal reagents.2,21 In addition, the mobility and diversity of large plasmid/transposon burden of KP enable it to be dangerously active in inter-species transfer of the resistance elements via bacterial conjugations between different Gram-negative bacteria such as Acinetobacter baumannii and Pseudomonas aeruginosa.22
The pathogenic colonization of KP in some cases and some period of infection can be occult and asymptomatic, which heavily compounds the tracking of its inter- or intra-patient evolution and spread.3,19 Using whole-genome sequencing, researchers were able to chart a putative transmission map of multidrug-resistant KPs within a hospital environment and pin down the index patient who was discharged three weeks prior to the stealthily developed outbreak.19 However, how various KP strains interact and adapt to survive along the course of the infection within a single host is not much understood.
In this study, we identified two distinct colonies of CR-hvKPs with sequence types ST11-K64 and ST35-K16, from six KP isolates obtained successively from the urine, sputum and secretion samples of a single patient with acute respiratory failure. Molecular characterization of the drug resistance, virulence and genome sequencing were performed to discern the mechanisms conferring bacterial survival, at the cost of the host’s survival.
Materials and Methods
Bacterial Isolates and the Case History
The patient was admitted to the ICU at the local hospital in July 2021 due to recessive severe cough and long-term ventilator-dependency. A total of six strains of Klebsiella pneumoniae (KP) were recovered from isolates successively collected from the urine, sputum and groin infection secretion (Figure 1), and were labelled as KP1, KP2, KP3, KP4, KP5 and KP6 in chronological order. Considering the high risk of lower respiratory tract and multi-site infection due to tracheotomy the patient underwent, anti-infection treatment of piperacillin/tazobactam was delivered at the initial stage of hospitalization, but without significant improvement. KP1 was isolated from urine samples when urinary tract infection was diagnosed at day 7. By immediate implementation of piperacillin/tazobactam treatment, the infection was controlled by day 19. On day 23, patches of bilateral groin erythema occurred, where KP2 was collected from the purulent secretion, which was considered to be a colonization and no specific treatment was applied. On day 35, the pulmonary infection deteriorated into acute respiratory failure. Despite prompt anti-infection treatment with cefoperazone/sulbactam + tigecycline, the infection was not controlled effectively. KP3 (urine) and KP4 (sputum) were detected during this period. The patient’s condition continued to advance into septic shock on day 52. The infection was largely controlled after an additional 22 days of treatment with cefoperazone/sulbactam + tigecycline but then relapsed 3 days afterwards. Meanwhile, KP5 and KP6 were identified from urine and sputum, respectively. Extended treatment with cefoperazone/sulbactam + tigecycline regimen for another 12 days did not stop the progress of the patient’s pulmonary and urinary tract infections, nor did the alternative treatment with colistin + levofloxacin. The patient ultimately succumbed to severe infections and multiple organ failure.
KP Identification and Antimicrobial Susceptibility Test
KP identification and antimicrobial susceptibility were performed using Micro MIC method on the VITEK 2 automated microbial identification and antibiotic susceptibility system (bioMérieux, France), according to the manufacturer’s instructions. Escherichia coli ATCC25922 and Klebsiella pneumoniae ATCC700603 (Microbiologics, America) served as quality control strains. Antimicrobials included in the panel were as follows: amikacin, ampicillin/sulbactam, ampicillin, cefazolin, cefepime, cefoperazone/sulbactam, cefotaxime, cefoxitin, ceftazidime, ceftazidime/clavulanate sodium, ceftriaxone, cefuroxime, ciprofloxacin, ertapenem, gentamicin, imipenem, meropenem, levofloxacin, nitrofurantoin, piperacillin/tazobactam, polymyxin E (colistin), tigecycline, tobramycin, and trimethoprim/tazobactam. The data were interpreted in accordance with the guidelines recommended by CLSI (Clinical and laboratory Standards Institute, 2020 version).
Detection of Carbapenemase and Its Encoding Genes
The NG-Test CARBA-5 immunochromatographic assay (Changsha Zhongsheng Zhongjie Biotechnology Co., Ltd) was performed to detect the five most prevalent carbapenemase families, ie Klebsiella pneumoniae carbapenemase (KPC), oxacillin-hydrolyzing β-lactamase (OXA-48), verona integron-encodes metallo-β-lactamase (VIM), imipenem-resistant phenotype (IMP), and New Delhi metallo-β-lactamase (NDM), as described previously.23 Colony samples from bacteria grown on blood agar culture were taken with a 1-μL loop and seeded into 150 μL extraction buffer and mixed by vortexing. Next, 100 μL of the mixture suspension was transferred into NG-Test Carba 5 sample well marked with ‘S’ in the test cassette. After 15 min of incubation at room temperature, the presence or absence of the control and test lines was visualized within 20 min. Positive controls for each target were provided in the test kit.
The carbapenem resistance genes (blakpc, blaOXA-48, blavim, blaIMP, blaNDM) encoding these five carbapenemases were examined by PCR, as described in the literature.24 The bacterial DNA template was extracted by boiling procedure. PCRs were carried out in 20 μL volumes containing 1μL extracted DNA, 9.5 μL Premix Taq DNA polymerase (Dalian Bao Biological Engineering Co., Ltd) and 1μL of each primer. Reaction conditions were 94°C for 5 minutes, followed by 35 cycles of 94°C for 30 seconds, 55–58°C for 60 seconds, 72°C for 30 seconds, and a final extension at 72°C for 5 minutes. The PCR products were separated through 2% agarose gel, stained in GoldViewTM nucleic acid dye and photographed under UV by GenoSensl500 transilluminator (Shanghai Qinxiang Scientific Instrument Co., Ltd). The detail of the PCR primers and the corresponding annealing temperature are listed in Table S1 (Supplemental Material).
Detection of Virulence Factors
The presence of six hypervirulence genes including rmpA (regulator of mucoid phenotype A), mrkD (mannose-specific adhesin subunit of type 3 fimbriae), entB (enterobactin biosynthesis), ybtS (yersiniabactin biosynthesis), wcaG (endotoxin-related gene) and KfuBC (iron acquisition system-related gene) was determined by PCR. The primer information is listed in Table S1. The PCR was conducted as described in Detection of Carbapenemase and Its Encoding Genes.
String Test
String test was conducted to assess the mucoviscosity of the KP strains, as established elsewhere.13 The formation of a >5 mm viscous filament of the KP colonies on a blood agar plate, stretched upwards by an inoculation loop, was classified as hypermucoviscous phenotype.
Multi-Locus Sequence Typing (MLST)
The nucleotide sequence-based serotyping MLST was performed to determine the sequence types (ST) of the KP strains. The primers used for PCR amplification of seven housekeeping gene fragments (gapA, rpoB, mdh, pgi, phoE, infB and tonB) were designed according to the Institute Pasteur Klebsiella MLST scheme (https://bigsdb.pasteur.fr/klebsiella/primers-used/). The PCR products were sequenced and aligned with online MLST database (https://bigsdb.pasteur.fr/).
Capsular Serotyping
The capsular serotypes of the KP isolates were determined using the PCR-based capsular antigen as previously described.25 The primers used are shown in Table S1. These assays differentiate KP isolates into seven major serotypes: K1, K2, K5, K20, K54, K57 and K64. The serotype of KP2 and KP4 was not determined by this panel and was identified by genome sequencing (Whole-Genome Sequencing (WGS)).
Molecular Genotyping by ERIC-PCR
To evaluate the genetic relatedness among the KP strains, ERIC (enterobacterial repetitive intergenic consensus) analysis was performed as described previously.26,27 Genomic DNA extracted from the bacteria was amplified using the primers ERIC1: 5’-ATGTAAGCTCCTGGGGATTCA-3’and ERIC2: 5’-AAGTAAGTGACTGGGGTGAGCG-3’. PCR was performed in total volumes of 25μL, containing 1μL DNA template, 12.5 μL Premix Taq DNA polymerase (Dalian Bao Biological Engineering Co., Ltd) and 1μL of each primer. Reaction conditions were 94°C for 5 minutes, followed by 35 cycles of 94°C for 45 seconds, 52°C for 50 seconds, 72°C for 2 minutes, and a final extension at 72°C for 10 minutes. The PCR products were subject to agarose gel electrophoresis and analysis system. The bacterial community fingerprint bands of the strains were inspected using Quantity One software. The unweighted pair-group method with arithmetic mean (UPGMA) was adopted to determine the similarity clustering among the obtained KP types. An inter-strain relatedness with genetic similarity coefficient >0.90 was considered highly homogeneous.
Serum Survival Assay
The survival of the bacteria in pooled serum from healthy individuals was investigated using a standard assay.28,29 Each experiment was performed with duplicates. Briefly, bacterial growing in exponential-phase were suspended at 1×106 CFU/mL into healthy human serum (1:3 volume ratio). The response of bacteria to serum killing was determined by viable colony counts obtained at 0, 1, 2, and 3 h upon the co-incubation at 37°C with shaking. The sensitivity levels were scored into six grades and classified into three levels, ie serum-sensitive (grade 1 or 2), intermediately sensitive (grade 3 or 4), or serum-resistant (grade 5 or 6). The grade criteria were as follows. Grade 1: viable counts <10% of the inoculum at 1, 2 h and <0.1% at 3 h; grade 2: viable counts 10-100% of the inoculum at 1, 2 h and <10% at 3 h; grade 3: viable counts >100% of inoculum at 1 h and <100% at 2, 3 h; grade 4: viable counts >100% of inoculum at 1, 2 h and <100% at 3 h; grade 5: viable counts >100% of the inoculum at 1, 2, and 3 h, but decrease afterwards; and grade 6: viable counts >100% of the inoculum at 1, 2, and 3 h, and keep increasing. A graph was drawn using Graphpad prism software, where the original data of experiment duplicates (number of colonies on the plate x dilution factor) were calculated, logarithmically transformed, and expressed in the form of mean ± error.
Whole-Genome Sequencing (WGS)
Genomic DNA of all strains was extracted with a TIANamp Bacteria DNA Kit (Beijing TIANGEN Biotech Co., Ltd) following the manufacturer’s instructions. The extracted gDNA was interrupted using Covaris LE220-PLUS (Covaris, Woburn, MA, United States) and the 300–500 bp fragments were selected as templates for library construction by VAHTS DNA Clean Beads. The double-stranded DNA was repaired and dA was added to the 3 ‘end. VAHTS DNA Clean Beads were used for purification. After purification, the WGS library was prepared using the VAHTS® Universal DNA Library Prep Kit for Illumina V3 (Vazyme Biotech Co., Ltd, United States). The sequencing library was sequenced using the MGI DNBSEQ-T7 (Shenzhen MGI Co., Ltd) with PE150 model.
Results
All KP Strains, Except for KP1, are Resistant to Carbapenems
As revealed by the antimicrobial susceptibility test, all the KP strains were ESBLs-producing and resistant to ampicillin, ampicillin/sulbactam, ceftriaxone, ceftazidime, cefotaxime, cefepime, cefazolin, cefoperazone/sulbactam, cefuroxime, ciprofloxacin, levofloxacin, nitrofurantoin, gentamicin, piperacillin/tazobactam, and trimethoprim/sulfa. Two antibiotics, tigecycline and colistin, were inhibitory to all six strains. KP1 was sensitive to cefoxitin and carbapenems including ertapenem, imipenem and meropenem, whereas all the other five strains were resistant. KP2 and KP4 had intermediate sensitivity to tobramycin. In opposition to KP2 and KP4, which were sensitive to aztreonam and resistant ceftazidime/avibactam, other strains had inverted responses to these antibiotics. In addition, the strains displayed various responses to amikacin, with only KP2, KP4 and KP5 showing sensitivity. Details of MIC (minimum inhibitory concentration) and sensitivity interpretation are listed in Table 1.
 |
Table 1 Antimicrobial Susceptibility Test of Six Klebsiella pneumoniae Isolates |
In agreement, KP1 did not contain any of the five carbapenemase enzymes examined by the NG- CARBA 5 assay. KP3, KP5 and KP6 were positive for KPC (Figure 2A), while NDM was detected in KP2 and KP4. The broad substrate spectrum of KPC enzyme covers all beta-lactam classes, including nitrocefin, cefotaxime, cephalothin, cephaloridine, benzylpenicillin, ampicillin and piperacillin.5 NDM is known to inactivate all β-lactams except aztreonam,30 which explained why KP2 and KP4 were sensitive to aztreonam in the antimicrobial test.
PCR data further confirmed the carriage of blaNDM gene in KP2 and KP4, and blaKPC gene in KP3, KP5 and KP6 (Figure 2B).
All Six KP Strains Harbour Virulence Factors, but KP2 and KP4 are Non-Mucoid
The presence of six virulence genes that are among the most recognised factors contributing to hypervirulence of KP31–33 were characterized by PCR amplification. We found that all strains carried mrkD, entB, kfuBC and ybtS genes, which are responsible for production of pathogenic molecules of adhesin subunit, enterobactin, iron transporter and siderophore-dependent yersiniabacin, respectively. However, rmpA was present only in KP1, KP3, KP5 and KP6, while the fucose-synthesizing gene wcaG was detected only in KP2 and KP4 (Table 2).
 |
Table 2 Summary of the Genetic and Phenotypic Profiles of the Klebsiella pneumoniae Isolates |
Hypermucoviscosity is a phenotypic manifestation of virulence that is significantly associated with rmpA plasmid and can be measured by string test. Among all strains, visible strings longer than 5mm were stretched from the colonies of KP1, KP3, KP5 and KP6, but not KP2 and KP4 (Figure 3), which matched the status of rmpA gene.
 |
Figure 3 Images of hypermucoviscous phenotype assessed by string test. |
The KP Strains Develop Resistance to Serum Killing Along the Course of Infection
The resistance of the bacteria to the healthy defence mechanism of human serum, typically the serum compliment killing, is an important aspect to ensure their survival in the host. As demonstrated by the logarithmic number of viable colonies counted at different timepoints (Figure 4), KP1, KP2 and KP4 were sensitive (both at grade 2) to serum killing and were almost completely eradicated after three hours of co-incubation. KP6 had an intermediate grade 4 sensitivity. KP3 and KP5 displayed strong resistance to serum killing, scored grade 5 and 6, respectively. According to the percentage of surviving KP colonies at the end of three hours in comparison to the initial time point, the order of serum susceptibility was KP2>KP1>KP4>KP6>KP3>KP5 (Table 3). KP1 and KP2 were killed by two thirds and one third, respectively, after 1 hour and mostly wiped out after 3 hours of co-incubation (3.82% and 3.48% left, respectively), while other strains demonstrated various resilience to the serum killing machinery. The survival of KP5 colonies was not inhibited but even encouraged throughout the co-incubation (viable counts > 100%). Comparing KP2 and KP4, which shared all phenotypic and genotypic attributions, KP4 had slightly higher survivability than KP2 at each time point. The results suggested a gradual accretion of serum resistance from KP1 to KP5, and from KP2 to KP4.
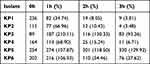 |
Table 3 Viable Counts (CFU/mL) and Percentage of Living Colonies in Serum Killing Assay |
Genomic and WGS Analyses Reveal Two Distinct Types of the KP Clones with Various Pathogenic Mechanisms
By MLST classification, KP1, KP3, KP5 and KP6 isolates were identified as ST11, whereas KP2 and KP4 were ST35. Subsequent capsular serotyping by PCR indicated that KP1, KP3, KP5 and KP6 belonged to K64. The serotype of KP2 and KP4 was not detected by the panel of common capsular serotypes covered in the PCR test but was determined separately by whole-genome sequencing (WGS). By aligning the sequence data with the MLST online database, both KP2 and KP4 were identified as K16 (Figure 5). WGS further revealed the subtypes of carbapenemase-coding genes in KP3, KP5 and KP6 as blaKPC-1, while that in KP2 and KP4 was blaNDM-5. Like common KP strains that contain blaKPC-1, KP6 was heavily resistant to imipenem, with MIC≥16 µg/mL. Noticing that the MIC of KP3 and KP5 to imipenem was 4 µg/mL, potential point mutations in the genes were suspected. But no base difference was found, the discordance of their imipenem susceptibility remained unexplained.
To identify the mechanisms responsible for the drug resistance and virulence of the KP strains, the WGS data were annotated against the Comprehensive Antibiotic Resistance Database (CARD) and the Virulence Factor Database (VFDB). Two distribution patterns of genetic features regarding resistance and virulence were distinguished between the ST11-K64 type (KP1, KP3, KP5 and KP6) and ST35-K16 type (KP2 and KP4) (Table 2).
Overall, three main resistance mechanisms were revealed as follows. 1) Antibiotic inactivation (enzyme inactivation). Firstly, all strains (KP1~KP6) carried various genes encoding broad-spectrum β-lactamase (CTX- M, TEM, and SHV). The NDM-5-producing strains KP2 and KP4 carried blaCTX-M-14 and blaSHV-33. KP1 carried blaCTX-M-65, blaTEM-1 and blaSHV-182, while the KPC-1-producing strains (KP3, KP5 and KP6) carried blaCTX-M-65 and blaTEM-1. Secondly, KP2 and KP4 carried aminoglycoside resistance factors AAC(3)-IId and APH(3”)-Ib, which encode aminoglycoside acetyltransferase and phosphotransferase, respectively, to act on the specific amino groups of aminoglycoside antibiotics or hydroxyl groups. The KPC-1-producing strains did not have these genes. However, KP1, KP3, KP5 and KP6 harboured cat II gene, encoding chloramphenicol acetyltransferase to act against chloramphenicol. 2) Antibiotic export systems, especially genes belonging to the Resistance-nodulation-division (RND) pumps (AcrA/B) and the Major Facilitator Superfamily (MFS) efflux pumps (tetracycline resistance proteins TetA and emrR) were present in all strains. Moreover, KP2 and KP4 carried Tet(D) gene and oqxA/B genes encoding RND-family transporters to facilitate resistance to fluoroquinolones. 3) Mutations via target site modification or reduced permeability, with two sequence type-specific genetic polymorphisms. All isolates contained several genes that enable the annihilation of antimicrobial inhibition by means of mutation. For instance, rmtB gene that encodes 16S rRNA methylase to disable the binding of aminoglycoside on 16S rRNA, sul1/2 gene that encodes a mutated dihydrofolate synthase (DHPS) to confer the resistance to sulfa drugs, and point mutations in chloramphenicol acetyltransferase gene cat II. In addition, all strains had OmpK37 gene, encoding a product of an outer membrane porin that reduces the permeability to limit antibiotics uptake.
The strains carried numerous virulence factors, including bacteriocins involved in iron uptake systems (yersinicins, ybtU/Q/E/X/A/S, irp1/2 etc.), enterobactins (entA/B, fepA/B/C, etc.), as well as genes encoding type 1 pilus (fimA/H) and structural subunits of pilus (yagZ/ecpA, etc.). Aerobactins (iucA/B/C/D and iutA) were present in all strains except for the NDM-5-producing KP2 and KP4.
The genetic and phenotypic profiling of carbapenem resistance, virulence, MLST and serotyping are summarised in Table 2.
Differentiated ERIC-PCR Fingerprint Patterns Infer a Heterogenous KP Infection in the Patient
Two distinct ERIC-PCR banding patterns of the six KP strains were shown (Figure 6A), one was shared among KP1, KP3, KP5 and KP6, and the other between KP2 and KP4. As indicated by the phylogenetic tree, the rates of genetic relatedness between KP1, KP3, KP5 and KP6 was over 0.96, while that of KP2 and KP4 was 0.98 (Figure 6B). In conjunction with the conspicuous pattern discerned above from the phenotypic and genomic profiles, it was evident that the resultant antimicrobial responses and disease development of the single patient were a collected manifestation of an infection of multi-strain KPs with intraspecific genetic diversity.
Discussion
Infections caused by simultaneously carbapenemase-producing and hypervirulent Klebsiella pneumoniae (CR-hvKP) are often lethal, as evidenced by our previous clinical experience3 and the present study. The mortality rate is as high as 50% around the world.6,8,34 A massive challenge arises from the genetic plasticity of the bacteria and the extremely limited choice of antibiotics. In the absence of systematic or evaluated treatment guidelines, an empiric treatment regimen needs to be tailored rapidly.
Based on the phenotypic and genotypic characteristics of the six KP isolates from the patient, we were able to reconstruct the infection route in perspective of the bacterial evolvement. KP1 was first detected from urine and belonged to ST11-K64. Although it was ESBL-producing, mucoid and contained several other virulence genes, it was highly sensitive to carbapenem and serum killing. Two more ST11-K64 strains from urine, KP3 and KP5, were respectively detected 32 days later during the episode of respiratory failure and 54 days later following the onset of septic shock. Compared with KP1, both had gained a CR factor blaKPC-1, retained ESBL-coding gene blaTEM-1 and blaCTX-M-65, but lost the blaSHV182 gene. A strain from the same clade, KP6, was identified from sputum at the same time of the detection of KP5. Notwithstanding the same genomic fingerprints shared with KP3, the resistance to serum killing and imipenem had advanced and peaked at KP5 and KP6, respectively. Parallelly, a genotypically distinct strain KP2, an NDM5-producing ST35-K16 CR-hvKP strain, was isolated from the groin purulent secretion 16 days after KP1 identification. This isolate was non-mucoid and susceptible to serum killing. KP4, bearing the same genotypic identity with KP2, was detected from sputum 17 days later, with enhanced serum resistance. As KP2 and KP4 had different isolation sites, there should be bacterial dissemination from the groin to the respiratory tract or vice versa. However, this clone of KP disappeared in the later samples of sputum, which might suggest a growth inhibition by the antibiotics or out-competition by the other KP type.
Although all isolates were sensitive to tigecycline, which has been suggested to be effective to treat various strains of CR-KP,6 a combination of tigecycline with cefoperazone-sulbactam did not achieve adequate efficacy to control the infection. The antibiogram indicated that the NDM-type KP2 and KP4 strains were sensitive to aztreonam and levofloxacin. Studies using in vitro model have shown that combining avibactam can reduce the susceptible breakpoint concentration of aztreonam, thereby enhancing its killing activity against KPs producing metallo- β-lactamases (MBLs) such as NDM and IMP.35 Successful treatment of infection with NDM-positive KP with a combination of aztreonam-ceftazidime-avibactam was also reported in a clinical case.36 However, due to the concurrent infection of the KPC-bearing CR-hvKP strain, they could not be used successfully to control the infection progress of the present patient. Although NDM-carrying KP may be susceptible to colistin and tigecycline, the former has noxious nephrotoxicity and the latter displays inconsistent efficacy among various subgroups of pneumonia patients.37 The last attempt with a reserve regime of colistin + levofloxacin did not curb the infection, although the synergistic killing of CR-KPs by colistin-based combination therapy with high efficacy was documented.38,39 The pan-drug resistance and the sum of diverse virulence of the two different clones of KP, compounded by the adverse side effects of antibiotics, contributed to the treatment failure.
ST11 is the predominant CR-KP strain in Asia and the serotype K64 constitutes its major sub-lineage.40–42 ST11-K64 infection is identified from different sources, such as sputum and liver abscess samples. Persistent colonization of ST11-K64 KP in gastrointestinal tract can aggravate gut dysbiosis, as shown in a mouse model.43 ST11-K64 is also the most common CR-hvKP clonal group causing nosocomial infections in China.44 With acquisition of blaKPC-1, rmpA/rmpA2, and siderophore gene clusters, ST11-K64 CR-hvKP possesses strengthened virulence and multi-drug resistance, which has earned its qualification for highly pathogenic “superbug” to challenge clinicians.45,46 In contrast, ST35 KP represents the major KP type in poultry species47 and is among the most prevalent KP types composing the gastrointestinal microbiome in humans.48 However, increased gut colonization of CR-KP can provide a major reservoir for healthcare-associated infectious diseases including pneumonia and bloodstream infection.49 Infections with multi-drug resistant ST35 KP were reported in different countries such as France,50 Yemen51 and China,52 but the pathogenicity of this strain was less understood. A ST35-K108 strain RJY9645, containing rmpA and blaNDM-5, was identified from the sample of a patient with bloodstream infection who was successfully treated with imipenem and levofloxacin.52 Meanwhile, K16 hvKP is less associated with MLST types53 and its implication in invasive infections is reported sporadically.54–56 Despite the initial assumption, we could not determine whether or not the ST35-K16 strains (KP2 and KP4) were derived from the patient’s gut colonization.
Infections involving multiple microbial species or different clones of the same species can exhibit magnified drug resistance and exacerbated disease progression, compared to single-strain infections. Both KP clones detected from the patient were equipped with a full range of antimicrobial resistance mechanisms, ie decrease of drug intake, modification of drug target, drug inactivation, drug extrusion, and shift in metabolic pathways.57 However, they might have unequal survivability. All the main biosynthetic genes for siderophores including yersiniabactin, enterobactin and aerobactin, which enable them to extract iron from the host, were present in the ST11-K64 strains. Notably, as aerobactin was proposed to be the most important determinator for the fitness and virulence of KP,58 its presence in ST11-K64 strains and absence in ST35-K16 strains, may partially explain why KP2 and KP4 had relatively weaker resistance to serum killing and were eliminated in sputum at later stage of the infection.
Only a few multi-strain infections of KP have been documented,19,59,60 and our understanding of the dynamic in-host interaction between the clones is meagre. The co-existing bacterial strains could compete to survive and proliferate. The combined modulation in the overall virulence and microbial resistance may favour the prosperity, dissemination, and pathogenesis of certain strains. Although exchange of genetic elements between the two types of KP strains was not suggested by the WGS results, crosstalk between them cannot be excluded. A mixed infection was reported in a case of necrotizing fasciitis (NF) caused by four Aeromonas Hydrophila strains originated from two distinct paraphyletic lineages NF1 and NF2.61 Further in vitro and mouse model investigations demonstrated that the functional type 6 secretion system (T6SS), possessed by NF1, not only was associated with multi-drug resistance but also mediated the elimination of NF2 by NF1. Conversely, NF2 assisted the rapid metastatic dissemination of NF1 by destruction of the local tissue barrier, through the exotoxin A (ExoA) virulence factor carried by NF2.62,63 In another study, mutations via insertion of IS (Insertion Sequences) elements at cps (capsular polysaccharide synthesis) locus were detected within a single host, which was suggested to be responsible for the survival competition between the mucoid form of KP and the non-mucoid KP strains.60
The unresolved but interesting questions are: 1) What are the infection sources of the KP strains? 2) Where did KP3 acquire blaKPC-1 gene from and how? 3) What are the mechanisms and clinical consequences of the loss blaSHV182? 4) Can the survival competition between co-existing KP strains turn to our advantage in treatment solutions? They can only be answered by pursuing tight clinical surveillance and quantitative assessment of the pathogenic traits.
Conclusion
Two distinct Klebsiella pneumoniae clones, KPC-1-producing CR-hvKP ST11-K64 and NDM-5-producing ST35-K16, were identified in a single patient. Both clones had rich possession of resistance and virulence factors, which aggregated to the treatment failure. Along the course of infection development, the strains demonstrated a propensity for expanded drug resistance spectrum and strengthened serum survival. The large repertoire of pathogenic gene factors detected in the strains raises an alarm for the lurking circulation of dangerous KPs.
Abbreviations
KP, Klebsiella pneumoniae; ESBLs, extended-spectrum ß-lactamases; hvKP, hypervirulent KP; hmKP, hypermucoviscous KP; cKP, classical KP; CR-hvKP, carbapenem resistant hyper-virulent KP; KPC, Klebsiella pneumoniae carbapenemase; OXA-48, oxacillin-hydrolyzing β-lactamase; VIM, verona integron-encodes metallo-β-lactamase; IMP, imipenem-resistant phenotype; NDM, New Delhi metallo-β-lactamase; MLST, multi-locus sequence typing; ST, sequence type; ERIC (enterobacterial repetitive intergenic consensus); PCR, polymerase chain reaction; CFU, colony-forming units; WGS, whole-genome sequencing.
Ethics Approval and Patient Consent
The study was approved by the Ethics Committee of the Affiliated Hospital of Guizhou Medical University. Since the patient is deceased, written informed consent for publication of his clinical details and clinical images was obtained from the next of kin. We confirm that informed consent obtained from all study participants prior to study commencement, and Guidelines outlined in the Declaration of Helsinki were followed.
Acknowledgment
The authors would like to thank Mr Dou-Dou Liu, a native English speaker, for helping us proofread the article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. HC and SL have contributed equally to the work, and are co-first authors. YF and HC conceived and designed the study. HC, SL and CZ collected the clinical specimen and performed the laboratory analyses. SL took part in drafting, and critically reviewing the article. HC and BL substantially reviewed the data analyses and revised the manuscript. All authors gave final approval of the version to be published. All authors have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
The study was financially supported by the National Natural Science Foundation of China No.81460334, and Foundation for the project of Natural Science Research Innovation Group of General Undergraduate College in Guizhou Province (Qianjiaohe KY character[2021]016).
Disclosure
The authors declare no potential conflict of interest.
References
1. Ashurst JV, Dawson A. Klebsiella Pneumonia. Treasure Island (FL): StatPearls; 2022.
2. Wang G, Zhao G, Chao X, Xie L, Wang H. The Characteristic of Virulence, Biofilm and Antibiotic Resistance of Klebsiella pneumoniae. Int J Environ Res Public Health. 2020;17:17.
3. Liang S, Cao H, Ying F, Zhang C. Report of a Fatal Purulent Pericarditis Case Caused by ST11-K64 Carbapenem-Resistant Hypervirulent Klebsiella pneumoniae. Infect Drug Resist. 2022;15:4749–4757.
4. Chang SL, Dela Cruz CS, Zhang D. Clinical Epidemiology, Risk Factors, and Control Strategies of Klebsiella pneumoniae Infection. Front Microbiol. 2021;12:750662.
5. Queenan AM, Bush K. Carbapenemases: the versatile beta-lactamases. Clin Microbiol Rev. 2007;20(3):440–458.
6. Lee GC, Burgess DS. Treatment of Klebsiella pneumoniae carbapenemase (KPC) infections: a review of published case series and case reports. Ann Clin Microbiol Antimicrob. 2012;11:32.
7. Clegg S, Murphy CN. Epidemiology and Virulence of Klebsiella pneumoniae. Microbiol Spectr. 2016;4(1):548.
8. Hirai J, Sakanashi D, Kinjo T, Haranaga S, Fujita J. The First Case of Community-Acquired Pneumonia Due to Capsular Genotype K2-ST86 Hypervirulent Klebsiella pneumoniae in Okinawa, Japan: a Case Report and Literature Review. Infect Drug Resist. 2020;13:2237–2243.
9. Shon AS, Bajwa RP, Russo TA. Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: a new and dangerous breed. Virulence. 2013;4(2):107–118.
10. Russo TA, Marr CM. Hypervirulent Klebsiella pneumoniae. Clin Microbiol Rev. 2019;32(3). doi:10.1128/CMR.00001-19
11. Choby JE, Howard‐Anderson J, Weiss DS. Hypervirulent Klebsiella pneumoniae – clinical and molecular perspectives. J Intern Med. 2020;287(3):283–300. doi:10.1111/joim.13007
12. Russo TA, MacDonald U, Hassan S, et al. An Assessment of Siderophore Production, Mucoviscosity, and Mouse Infection Models for Defining the Virulence Spectrum of Hypervirulent Klebsiella pneumoniae. mSphere. 2021;6(2). doi:10.1128/mSphere.00045-21.
13. Russo TA, Olson R, Fang CT, et al. Identification of Biomarkers for Differentiation of Hypervirulent Klebsiella pneumoniae from Classical K. pneumoniae. J Clin Microbiol. 2018;56(9):98.
14. Yang X, Dong N, Chan EW, Zhang R, Chen S. Carbapenem Resistance-Encoding and Virulence-Encoding Conjugative Plasmids in Klebsiella pneumoniae. Trends Microbiol. 2021;29(1):65–83.
15. Heiden SE, Hubner NO, Bohnert JA, et al. A Klebsiella pneumoniae ST307 outbreak clone from Germany demonstrates features of extensive drug resistance, hypermucoviscosity, and enhanced iron acquisition. Genome Med. 2020;12(1):113.
16. Martin MJ, Corey BW, Sannio F, et al. Anatomy of an extensively drug-resistant Klebsiella pneumoniae outbreak in Tuscany, Italy. Proc Natl Acad Sci U S A. 2021;118(48):54.
17. Lee CM, Liao CH, Lee WS, et al. Outbreak of Klebsiella pneumoniae carbapenemase-2-producing K. pneumoniae sequence type 11 in Taiwan in 2011. Antimicrob Agents Chemother. 2012;56(10):5016–5022.
18. Chen C, Zhang Y, Yu SL, et al. Tracking Carbapenem-Producing Klebsiella pneumoniae Outbreak in an Intensive Care Unit by Whole Genome Sequencing. Front Cell Infect Microbiol. 2019;9:281.
19. Snitkin ES, Zelazny AM, Thomas PJ, et al. Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci Transl Med. 2012;4(148):148ra116.
20. Cortes-Ortiz IA, Juarez-Gomez JC, Cu-Quijano C, et al. Klebsiella pneumoniae blaNDM-1 carrying a class 1 integron causing a hospital outbreak in a Mexican attention center. J Infect Dev Ctries. 2021;15(5):657–664.
21. Ochonska D, Scibik L, Brzychczy-Wloch M. Biofilm Formation of Clinical Klebsiella pneumoniae Strains Isolated from Tracheostomy Tubes and Their Association with Antimicrobial Resistance, Virulence and Genetic Diversity. Pathogens. 2021;10(10):87.
22. Wyres KL, Holt KE. Klebsiella pneumoniae as a key trafficker of drug resistance genes from environmental to clinically important bacteria. Curr Opin Microbiol. 2018;45:131–139.
23. Jenkins S, Ledeboer NA, Westblade LF, et al. Evaluation of NG-Test Carba 5 for Rapid Phenotypic Detection and Differentiation of Five Common Carbapenemase Families: results of a Multicenter Clinical Evaluation. J Clin Microbiol. 2020;58(7):87.
24. Indrajith S, Mukhopadhyay AK, Chowdhury G, et al. Molecular insights of Carbapenem resistance Klebsiella pneumoniae isolates with focus on multidrug resistance from clinical samples. J Infect Public Health. 2021;14(1):131–138.
25. Yu F, Lv J, Niu S, et al. Multiplex PCR Analysis for Rapid Detection of Klebsiella pneumoniae Carbapenem-Resistant (Sequence Type 258 [ST258] and ST11) and Hypervirulent (ST23, ST65, ST86, and ST375) Strains. J Clin Microbiol. 2018;56(9):9.
26. Duan H, Chai T, Liu J, et al. Source identification of airborne Escherichia coli of swine house surroundings using ERIC-PCR and REP-PCR. Environ Res. 2009;109(5):511–517.
27. Zhang S, Yang G, Ye Q, Wu Q, Zhang J, Huang Y. Phenotypic and Genotypic Characterization of Klebsiella pneumoniae Isolated From Retail Foods in China. Front Microbiol. 2018;9:289.
28. Liu Y, Liu PP, Wang LH, Wei DD, Wan LG, Zhang W. Capsular Polysaccharide Types and Virulence-Related Traits of Epidemic KPC-Producing Klebsiella pneumoniae Isolates in a Chinese University Hospital. Microb Drug Resist. 2017;23(7):901–907.
29. Du Q, Pan F, Wang C, et al. Nosocomial dissemination of hypervirulent Klebsiella pneumoniae with high-risk clones among children in Shanghai. Front Cell Infect Microbiol. 2022;12:984180.
30. Shakil S, Azhar EI, Tabrez S, et al. New Delhi metallo-beta-lactamase (NDM-1): an update. J Chemother. 2011;23(5):263–265.
31. Zhang S, Zhang X, Wu Q, et al. Clinical, microbiological, and molecular epidemiological characteristics of Klebsiella pneumoniae-induced pyogenic liver abscess in southeastern China. Antimicrob Resist Infect Control. 2019;8:166.
32. Fu L, Huang M, Zhang X, et al. Frequency of virulence factors in high biofilm formation blaKPC-2 producing Klebsiella pneumoniae strains from hospitals. Microb Pathog. 2018;116:168–172.
33. Zhan L, Wang S, Guo Y, et al. Outbreak by Hypermucoviscous Klebsiella pneumoniae ST11 Isolates with Carbapenem Resistance in a Tertiary Hospital in China. Front Cell Infect Microbiol. 2017;7:182.
34. Gasink LB, Edelstein PH, Lautenbach E, Synnestvedt M, Fishman NO. Risk factors and clinical impact of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae. Infect Control Hosp Epidemiol. 2009;30(12):1180–1185.
35. Karlowsky JA, Kazmierczak KM, de Jonge BLM, Hackel MA, Sahm DF, Bradford PA. In Vitro Activity of Aztreonam-Avibactam against Enterobacteriaceae and Pseudomonas aeruginosa Isolated by Clinical Laboratories in 40 Countries from 2012 to 2015. Antimicrob Agents Chemother. 2017;61(9):9.
36. Bocanegra-Ibarias P, Camacho-Ortiz A, Garza-Gonzalez E, Flores-Trevino S, Kim H, Perez-Alba E. Aztreonam plus ceftazidime-avibactam as treatment of NDM-1-producing Klebsiella pneumoniae bacteraemia in a neutropenic patient: last resort therapy? J Glob Antimicrob Resist. 2020;23:417–419.
37. Freire AT, Melnyk V, Kim MJ, et al. Comparison of tigecycline with imipenem/cilastatin for the treatment of hospital-acquired pneumonia. Diagn Microbiol Infect Dis. 2010;68(2):140–151.
38. Ontong JC, Ozioma NF, Voravuthikunchai SP, Chusri S. Synergistic antibacterial effects of colistin in combination with aminoglycoside, carbapenems, cephalosporins, fluoroquinolones, tetracyclines, fosfomycin, and piperacillin on multidrug resistant Klebsiella pneumoniae isolates. PLoS One. 2021;16(1):e0244673.
39. Gurjar M. Colistin for lung infection: an update. J Intensive Care. 2015;3(1):3.
40. Hu L, Liu Y, Deng L, et al. Outbreak by Ventilator-Associated ST11 K. pneumoniae with Co-production of CTX-M-24 and KPC-2 in a SICU of a Tertiary Teaching Hospital in Central China. Front Microbiol. 2016;7:1190.
41. Sanikhani R, Moeinirad M, Shahcheraghi F, et al. Molecular epidemiology of hypervirulent Klebsiella pneumoniae: a systematic review and meta-analysis. Iran J Microbiol. 2021;13(3):257–265.
42. Qi Y, Wei Z, Ji S, Du X, Shen P, Yu Y. ST11, the dominant clone of KPC-producing Klebsiella pneumoniae in China. J Antimicrob Chemother. 2011;66(2):307–312.
43. Chiang MK, Hsiao PY, Liu YY, et al. Two ST11 Klebsiella pneumoniae strains exacerbate colorectal tumorigenesis in a colitis-associated mouse model. Gut Microbes. 2021;13(1):1980348.
44. Xiong L, Su L, Tan H, et al. Molecular Epidemiological Analysis of ST11-K64 Extensively Drug-Resistant Klebsiella pneumoniae Infections Outbreak in Intensive Care and Neurosurgery Units Based on Whole-Genome Sequencing. Front Microbiol. 2021;12:709356.
45. Yang Q, Jia X, Zhou M, et al. Emergence of ST11-K47 and ST11-K64 hypervirulent carbapenem-resistant Klebsiella pneumoniae in bacterial liver abscesses from China: a molecular, biological, and epidemiological study. Emerg Microbes Infect. 2020;9(1):320–331.
46. Wei T, Zou C, Qin J, et al. Emergence of Hypervirulent ST11-K64 Klebsiella pneumoniae Poses a Serious Clinical Threat in Older Patients. Front Public Health. 2022;10:765624.
47. Franklin-Alming FV, Kaspersen H, Hetland MAK, et al. Exploring Klebsiella pneumoniae in Healthy Poultry Reveals High Genetic Diversity, Good Biofilm-Forming Abilities and Higher Prevalence in Turkeys Than Broilers. Front Microbiol. 2021;12:725414.
48. Raffelsberger N, Hetland MAK, Svendsen K, et al. Gastrointestinal carriage of Klebsiella pneumoniae in a general adult population: a cross-sectional study of risk factors and bacterial genomic diversity. Gut Microbes. 2021;13(1):1939599.
49. Shimasaki T, Seekatz A, Bassis C, et al. Increased Relative Abundance of Klebsiella pneumoniae Carbapenemase-producing Klebsiella pneumoniae Within the Gut Microbiota Is Associated With Risk of Bloodstream Infection in Long-term Acute Care Hospital Patients. Clin Infect Dis. 2019;68(12):2053–2059.
50. Marcade G, Brisse S, Bialek S, et al. The emergence of multidrug-resistant Klebsiella pneumoniae of international clones ST13, ST16, ST35, ST48 and ST101 in a teaching hospital in the Paris region. Epidemiol Infect. 2013;141(8):1705–1712.
51. Alsharapy SA, Gharout-Sait A, Muggeo A, et al. Characterization of Carbapenem-Resistant Enterobacteriaceae Clinical Isolates in Al Thawra University Hospital, Sana’a, Yemen. Microb Drug Resist. 2020;26(3):211–217.
52. Shen Z, Gao Q, Qin J, Liu Y, Li M. Emergence of an NDM-5-Producing Hypervirulent Klebsiella pneumoniae Sequence Type 35 Strain with Chromosomal Integration of an Integrative and Conjugative Element, ICEKp1. Antimicrob Agents Chemother. 2019;64(1):1–54.
53. Zhu J, Wang T, Chen L, Du H. Virulence Factors in Hypervirulent Klebsiella pneumoniae. Front Microbiol. 2021;12:642484.
54. Dong N, Yang X, Chan EW, Zhang R, Chen S. Klebsiella species: taxonomy, hypervirulence and multidrug resistance. EBioMedicine. 2022;79:103998.
55. Lee IR, Molton JS, Wyres KL, et al. Differential host susceptibility and bacterial virulence factors driving Klebsiella liver abscess in an ethnically diverse population. Sci Rep. 2016;6:29316.
56. Cheng NC, Yu YC, Tai HC, et al. Recent trend of necrotizing fasciitis in Taiwan: focus on monomicrobial Klebsiella pneumoniae necrotizing fasciitis. Clin Infect Dis. 2012;55(7):930–939.
57. Munita JM, Arias CA. Mechanisms of Antibiotic Resistance. Microbiol Spectr. 2016;4(2):98.
58. Russo TA, Olson R, MacDonald U, Beanan J, Davidson BA. Aerobactin, but not yersiniabactin, salmochelin, or enterobactin, enables the growth/survival of hypervirulent (hypermucoviscous) Klebsiella pneumoniae ex vivo and in vivo. Infect Immun. 2015;83(8):3325–3333.
59. Carrasco-Anabalon S, Conceicao Neto CO, D’Alincourt Carvalho-Assef AP, et al. Introduction of NDM-1 and OXA-370 from Brazil into Chile in strains of Klebsiella pneumoniae isolated from a single patient. Int J Infect Dis. 2019;81:28–30.
60. Lee H, Shin J, Chung YJ, et al. Evolution of Klebsiella pneumoniae with mucoid and non-mucoid type colonies within a single patient. Int J Med Microbiol. 2019;309(3–4):194–198.
61. Ponnusamy D, Kozlova EV, Sha J, et al. Cross-talk among flesh-eating Aeromonas hydrophila strains in mixed infection leading to necrotizing fasciitis. Proc Natl Acad Sci U S A. 2016;113(3):722–727.
62. Fernandez-Bravo A, Kilgore PB, Andersson JA, et al. T6SS and ExoA of flesh-eating Aeromonas hydrophila in peritonitis and necrotizing fasciitis during mono- and polymicrobial infections. Proc Natl Acad Sci U S A. 2019;116(48):24084–24092.
63. Grim CJ, Kozlova EV, Ponnusamy D, et al. Functional genomic characterization of virulence factors from necrotizing fasciitis-causing strains of Aeromonas hydrophila. Appl Environ Microbiol. 2014;80(14):4162–4183.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





