Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
ModAsian FINDRISC as a Screening Tool for People with Undiagnosed Type 2 Diabetes Mellitus in Vietnam: A Community-Based Cross-Sectional Study
Authors Doan L , Nguyen HT , Nguyen TTP , Phan TTL , Huy LD , Nguyen TTH , Doan TP
Received 24 November 2022
Accepted for publication 2 February 2023
Published 17 February 2023 Volume 2023:16 Pages 439—449
DOI https://doi.org/10.2147/JMDH.S398455
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Long Doan,1 Huong T Nguyen,2 Thao TP Nguyen,3 Thi Thuy Linh Phan,4 Le Duc Huy,4 Thi Thuy Hang Nguyen,4 Thuoc Phuoc Doan2
1Internal Medicine Department, University of Medicine and Pharmacy, Hue University, Hue, Thua Thien Hue, Vietnam; 2Faculty of Public Health, University of Medicine and Pharmacy, Hue University, Hue, Thua Thien Hue, Vietnam; 3Institute for Community Health Research, University of Medicine and Pharmacy, Hue University, Hue, Thua Thien Hue, Vietnam; 4Health Personnel Training Institute, University of Medicine and Pharmacy, Hue University, Hue, Thua Thien Hue, Vietnam
Correspondence: Thuoc Phuoc Doan, Faculty of Public Health, University of Medicine and Pharmacy, Hue University, Hue, Thua Thien Hue, 53000, Vietnam, Tel +84 914932577, Email [email protected]
Purpose: Our study aims to evaluate the risk of developing type 2 diabetes mellitus in the next 10 years using ModAsian FINDRISC and additionally explore associated factors among the Vietnam population.
Participants and Methods: A cross-sectional study was conducted on 2258 participants aged 25 years old or above in Thua Thien Hue Province, Vietnam. The sample size is calculated based on the estimated sensitivity, and participants were randomly selected from different geographical and socio-economic areas. All participants were thoroughly medically examined, taking blood lipid profile and fasting blood glucose, taking blood pressure, anthropometric indexes, 12-lead electrocardiogram, and behavioral factors were investigated using the Vietnamese version of the WHO STEPS toolkit. The risk of developing T2DM was made based on the ModAsian FINDRISC.
Results: The incidence of developing type 2 diabetes mellitus among the study population was 4.21%. The group with a high or very high risk of developing type 2 diabetes mellitus in the next 10 years accounted for 2.52%. Body mass index (AUC = 0.840, 95% CI: 0.792– 0.888), waist circumference (AUC = 0.824, 95% CI: 0.777– 0.871), family history of diabetes mellitus (AUC = 0.751, 95% CI = 0.668– 0.833), and history of antihypertensive medication use regularly (AUC = 0.708, 95% CI: 0.632– 0.784) are the most associated factors of the ModAsian FINDRISC. Residential location (OR = 5.62, 95% CI: 1.91– 16.54) and occupational status (OR = 0.35, 95% CI: 0.20– 0.62) were significant factors associated with a high and very high risk of developing type 2 diabetes mellitus in the next 10 year.
Conclusion: Screening for the risk of type 2 diabetes mellitus and implementing intervention programs focusing on controlling weight, waist circumference, and blood pressure are essential for reducing type 2 diabetes mellitus incidence and burden in Vietnam.
Keywords: type 2 diabetes mellitus, Vietnam, noncommunicable diseases, ModAsian FINDRISC
Introduction
Type 2 diabetes mellitus (T2DM) is a common chronic disease, with approximately 7–30% of diabetes cases remaining undiagnosed.1,2 It suffices to state that the prevalence of diabetes, diabetes-related deaths, and global healthcare expenditures on T2DM continue to rise globally,3 thus making diabetes a primary global health concern, especially in the developing and underdeveloped nations of the world.4 Besides, standard diagnostic tests, such as the glycated hemoglobin (HbA1c) and the Oral Glucose Tolerance Test (OGTT), are expensive and difficult to scale up in a large population,5 especially in resource-limited countries such as Vietnam. Moreover, timely screening for identifying individuals with undiagnosed T2DM is the key to diagnosing diabetes at the early stages and preventing T2DM complications.6 Thus, the validated diabetes risk scoring models, which are defined as “an objective assessment of the probability of the presence or future development of an adverse health condition”,7 are recommended by several international organizations2,8 that can be easily applied to identify people at high risk of having or developing T2DM.
Several tools have been developed to estimate the risk of incident diabetes and screen for individuals with undiagnosed diabetes, such as the Danish Diabetes Risk Score,9 the Finnish Diabetes Risk Score (FINDRISC),10 the New Chinese Diabetes Risk Score,11 and the QDiabetes-2018.12 Of these, the FINDRISC was found to be an outstanding and effective tool in identifying subjects at a high risk of developing T2DM in 10 years13 as it is affordable and easy to use.14–16 With its advantages, FINDRISC has been recommended as a screening tool by the International Diabetes Federation (IDF) and European guidelines.17,18
The Modified Asian FINDRISC (ModAsian FINDRISC), which applied cut-off points for waist circumference (WC) and Body Mass Index (BMI) based on Asian standards, has been proposed as a useful tool for T2DM screening in several Asian countries, such as Indonesia,19 Malaysia,20 and Vietnam.21–24 However, these study populations were primarily small sample sizes or lack of representation.20,23 To fill the research gap, we carried out the study to evaluate the performance of ModAsian FINDRISC in a large sample size distributed in different ecoregions (City, delta, mountainous and coastal). Additionally, we integrated the WHO STEPS questionnaire into our study protocol to examine the association between various behavioral risk factors and the risk of incident diabetes. To our knowledge, no published study assesses the FINDRISC scale on a large representative sample from different ecological areas in Asia.
Therefore, our study aimed to evaluate the risk of developing T2DM in the next 10 years using ModAsian FINDRISC and identify associated factors among the Vietnamese population located in different ecoregions.
Materials and Methods
Study Design and Study Population
A community-based cross-sectional study was conducted from May 1st, 2020 to January 31st, 2021 at eight community health stations which presented four different ecoregions in the Thua Thien Hue province, Vietnam.
The sample size for this study was estimated using a method for studies with a binary test outcome25 with a sensitivity of 80%, estimated precision of 6.5%, and 9.5% for the incidence of diabetes. With the approach of multistage stratified random sampling, the sample size was multiplied by the design effect of 1.5. An additional 10% of the sample was included to account for respondents who refused to complete questionnaires or returned them incomplete. In all, 2500 participants were included in the research population.
A representative sample of the adult population from Thua Thien Hue province’s diverse ecology was obtained using a multistage stratified random sampling approach. Following the eco-features, the districts of Thua Thien Hue province were divided into four distinct groups: delta, mountain, city, and coastal. In each area, a district or city was selected at random. Then, we selected two communes in each district, and the sample selected in each commune varies based on the commune’s population (Figure 1).
 |
Figure 1 The distributions of participants in the study settings. |
Our inclusion criteria included being aged 25 or above, having good communication in the Vietnamese language, without a history of diabetes, and not being in an emergency condition or having any mental health problems. The conditions for exclusion of a participant from the study are as follows: (1) a prior diagnosis of diabetes, (2) a fasting blood glucose of ≥126 mg/dL, (3) an HbA1c ≥200 mg/dL, (4) use of prescribed drugs or diets for diabetes control and management, or (5) a decline of consent. After excluding 242 participants, 2258 respondents were included in the final analysis.
Data Collection Procedure
We collaborated with community leaders to compile a list of participants randomly drawn from resident lists in certain areas. The selected participants were informed of the research information three days before the review date. All participants meeting the inclusion criteria and providing informed permission who presented themselves at the community health station on the day of the review were registered and included in the research. We also remind them to do not to have anything to eat or drink before (except water) for 8 to 12 hours. In the morning, all subjects were taken fasting blood samples for lipid profile tests and fasting blood glucose by well-trained nurses and technicians. After that, all blood samples after collection were refrigerated and transported to Hue University Hospital of Medicine and Pharmacy and then stored at −70°C before performing laboratory tests. Before completing the rest parts of the survey, participants received milk and sweeties. Following, participants were thoroughly medically examined by Internal Medicine specialists and well-trained nurses from Hue University of Medicine and Pharmacy, taking brachial blood pressure (mmHg), height (cm), weight (kg), and WC (cm). At last, all participants were interviewed using the Vietnamese version WHO STEPS toolkit.
Markedly, the collection data period took place in the context of an epidemic of acute respiratory infections due to an intense outbreak of coronavirus disease (COVID-19) nationally and globally.26 As of Jan 31th 2021, Viet Nam has reported a total of 1819 laboratory-confirmed cases of COVID-19, with 35 deaths; among these, no confirmed cases and no death were reported in Thua Thien Hue province. The infection prevention and control measures were applied in the procedure of data collection according to the guidelines of the Vietnam Ministry of Health27 and World Health Organization,28 including using masks, washing hands, and physical distancing.
Research Instruments and Assessments
According to the Vietnamese version of the STEPS questionnaire initiated by the World Health Organization (WHO),29 we developed a questionnaire to collect socio-demographic information on age, gender, ethnicity (Kinh majority group and non-Kinh minority groups) (eg Co Tu), educational level, monthly household income per adult household member, and key behavior risk factors (tobacco smoking, alcohol consumption, vegetable/ fruit diets, and physical activity).
All anthropometric measurements (weight, height, WC) and biological indexes (fasting blood glucose, fasting total cholesterol, systolic blood pressure (SBP), and diastolic blood pressure (DBP) were collected.
The Modified Asian FINDRISC (ModAsian-FINDRISC)
The ModAsian-FINDRISC questionnaire comprises eight variables as the FINDRISC (Supplementary 1). The WC cut-off values were adjusted for Asian by adding 4 points for subjects with abdominal obesity (WC ≥ 90 cm for men and ≥80 cm for women), 3 points with and no points for those with normal WC values.30 The BMI cut-off values were adjusted for Asian30 by adding 3 points if BMI ≥ 25 kg/m2, one point if BMI ranged from 23 to <25 kg/m2, and no points for those with BMI values lesser than 23. The total ModAsian-FINDRISC score ranged from 0 to 26 points.
Ethical Considerations
The protocol, informed consent, and questionnaires were approved by the Institutional Ethical Review Committee of Hue University of Medicine and Pharmacy, Hue University, Vietnam (IRB No. H2020/380). This work has been carried out following the Declaration of Helsinki.
The study was approved by the local government after clearly explaining its purposes with the consent of the participants voluntarily and without any coercion (according to the consent form of each participant). All information related to the participants is kept confidential and only disclosed in the form of data. During the study, no interventions affected the health of the study participants. After taking fasting venous blood samples for laboratory tests, all participants were given snacks/breakfast free. Participants found to be at high risk will be consulted for treatment.
Data Analysis
First, the distributions of studied variables were explored using the χ2 test, Linear-by-Linear Association, and one-way ANOVA test appropriately. Second, independent variables relating to predicting the risk of T2DM in the next 10 years through univariate tests were selected into the multivariable logistic regression model. The method of Enter was used to analyze the relationship between selected independent variables and predict the risk of T2DM in the next 10 years. Data were imported by Epidata 3.1 software; were analyzed using the IBM SPSS version 20.0 (IBM, Armonk, NY, USA). The significance level was set at p < 0.05.
Results
Finally, the sample of 2258 participants was analyzed with the distribution of participants in the study settings represented in Figure 1, including 732 from Hue city, 563 from Quang Dien District, 530 from Phu Vang District, and 433 from Nam Dong District.
Participants’ Characteristics
Table 1 presents the general characteristics of study subjects, stratified by the level of diabetes risk. The majority of participants are female (65.9%), married (83.9%), living in the city areas (32.4%), and attaining at least primary and secondary school level (80.0%).
 |
Table 1 Characteristics of the Study Population and Diabetes Risk Levels |
The percentage of smokers and alcohol consumers was 20.7% and 29.9%, respectively. Over 23.2% of participants spend less than 30 minutes daily doing physical activities. There were 30.5% of participants without daily consumption of vegetables, fruits, or berries. The prevalence of health risk behaviors was statistically different among low and slightly risk, moderate, and higher/very high-risk groups (p < 0.05).
In terms of physical measurements, the percentage of participants with BMI >25 kg/m2 and the prevalence of those with waist circumference >90 cm (male) or >80 cm (female) was 13.1% and 21.6%, respectively. Regarding the biomedical indicators, statistical differences in the average figure for Total cholesterol, Triglyceride, LDL-C, and HDL-C were found among participants with low/slight, moderate, and high risk of diabetes. In addition, the prevalence of people with dyslipidemia was 85.9%, while those treated with antihypertensive medication regularly accounted for 19.1%.
Risk of Developing Type 2 Diabetes Mellitus in the Vietnamese General Population
In Table 2, the percentage of people in the very low, slightly elevated, moderate, high, and very high-risk groups, according to the ModAsian FINDRISC, is 48.14%, 42.21%, 7.13%, 2.48%, and 0.04%, respectively. The number of people predicted to develop T2DM in the next 10 years is approximately 95 over 2258, equivalent to 4.21% of the population.
 |
Table 2 The Risk of Development of Type 2 Diabetes Mellitus in the Next 10-Year by ModAsian FINDRISC |
In Table 3, among 8 risk factors in the ModAsian FINDRISC, BMI, waist circumference, family history of DM, and history of regularly taking antihypertensive medication are the most associated factors with the AUC are 0.840, 0.824, 0.751, 0.708, respectively (Figure 2).
 |
Table 3 Area Under Curve of the Factors of the ModAsian FINDRISC |
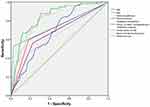 |
Figure 2 The ROC of risk factors in the ModAsian FINRISC. Abbreviations: BMI, Body mass index; DM, Diabetes mellitus. |
Associated Factors in the Risk of Developing Type 2 Diabetes Mellitus in the Next 10 Years
Table 1 shows associated risk factors by risk stratification according to ModAsian FINDRISC, 2.5% of patients are in the high and very high-risk group, of which the age group 55 and older accounts for the highest proportion. Females have a proportion of a high and very high risk of 10 years of developing T2DM was 3.0%, significantly higher than males with a proportion of 1.7% (p < 0.01). The percentage of high and very high risk of T2DM in the next 10 years was 2.6% in the overweight group and 12.5% in the obese group; the normal and underweight groups had a significantly lower percentage (p < 0.01).
Multivariate Regression Model of Related Factors to Predict High and Very High 10-Year Risk of Developing Type 2 Diabetes Mellitus
In Table 4, the associated factors with the prediction of high and very high 10-year risk of developing type 2 diabetes mellitus are presented. The multivariable logistic regression model found that the high and very high 10-year risk of developing type 2 diabetes mellitus were significantly associated with participants living in the Delta area (OR = 5.62, 95% CI: 1.91–16.54) and people who retired or infirmity (OR = 0.35, 95% CI: 0.20–0.62).
 |
Table 4 Multivariate Regression Model of Factors Related to Predicting High and Very High 10-Year Risk of Developing Type 2 Diabetes Mellitus (n = 2258) |
Discussion
The study was conducted on 2258 subjects who are aged 18 years old or above in Thua Thien Hue province. ModAsian FINDRISC calculation estimated that 4.21% of the study population in Thua Thien Hue province (approximately equivalent to 95 people) will develop T2DM by 2030. Our result is higher than the previous finding of Anne Jolle et al (4.0%),31 and Luu Minh Chau and Dau Xuan Canh (3.27%).21 The possible explanation for these differences is that our study selected people ≥25 years old, but Anne Jolle et al researched subjects ≥20 years old, and Luu Minh Chau and Dau Xuan Canh selected people ≥18 years old.21,31 In the FINDRISC and ModAsian FINDRISC, age is an important risk factor for T2DM; the older the age, the greater the risk. This can be used to explain the difference between our study and the results of Do Ich Thanh et al, with 6.0% when the study was conducted on subjects ≥45 years of age.32
Our study shows that in the population ≥25 years old, 2.52% are at high or very high risk of developing T2DM in the next 10 years, and 9.65% are at moderate to very high risk (Table 1). Compared with the study of Do Ich Thanh et al, the study conducted in Da Nang city in 1000 people ≥45 years old,32 our results are much lower than the results of 16.7% of people at moderate to very high risk of developing T2DM in the next 10 years. The difference in the age selection criteria could be the main reason for these results; as per our findings, age is a significant factor in the prognosis of the 10-year risk of developing T2DM. Age is a strong risk factor for many CVD diseases, as the SCORE233 and SCORE2-OP34 were recently demonstrated. Our results once again show that people with old age should be at least screened for diabetes and other atherosclerotic cardiovascular diseases for early prevention and treatment. But our study has findings that among the risk factors in the ModAsian FINDRISC, BMI, waist circumference, family history of DM, and history of regular taking the antihypertensive medication are the most associated factors with good to very good quality prognosis. In contrast, age, a non-modifiable risk factor, is a satisfactory risk factor with AUC = 0.685. The FINDRISC collects both traditional and modern cardiovascular risk factors but focuses on modifiable risk factors, and this helps people at risk of developing T2DM in the next 10 years to recognize their risk factors early and change their lifestyle to reduce their risk.
Interestingly, as our multivariate regression analysis results in Table 4, residential location and occupational status are strongly associated with a high and very high risk of developing T2DM. With these results, campaigns to screen for T2DM, as well as annual cardiovascular risk counseling and education programs, should especially focus on this group of people.
Our findings indicated that the ModAsian FINDRISC would be a valuable tool for healthcare workers to plan more cost-effective interventions focusing on the group with a high and very high risk of T2DM. However, adherence to intervention programs related to behavioral risk factors remains low since most programs lack supervision, and social support and employ an ineffective mode of delivery.35,36 Recently, the application of digital health (mobile apps, health chatbots, virtual health consultancy) offered novel management of modification risk factors with lower cost, more accessibility, and personalization.37,38 Thus, further study on the effectiveness of digital health intervention (mobile apps, health chatbot, virtual health consultancy) on FINDRISC score is essential to control the risk of diabetes development.
Conclusion
In conclusion, 4.21% of Vietnamese people 25 years old or above are predicted to develop type 2 diabetes mellitus in the next 10 years. The screening campaign for diabetes and lifestyle intervention focusing on reducing weight, waist circumference, and blood pressure control is needed for better prevention in the Vietnamese population.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available upon reasonable request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Ethical Review Committee of Hue University of Medicine and Pharmacy, Hue University, Vietnam (IRB No. H2020/380). The patients/participants provided their written informed consent to participate in this study.
Acknowledgments
We would like to thank all experts, doctors, nurses, medical students, and research assistants who helped with data collection. We also appreciate and acknowledge the participation of residents from the Thua Thien Hue province.
Funding
The study was fully funded by Hue University (number: DHH2020-04-121).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Bramlage P, Rey A, Thoenes M. Diabetes prevalence and metabolic risk profile in an unselected population visiting pharmacies in Switzerland. Vasc Health Risk Manag. 2012;541. doi:10.2147/VHRM.S35896
2. Liu M, Pan C, Jin M; Chinese Diabetes A. Risk score for screening of undiagnosed diabetes and abnormal glucose tolerance. Diabetes Technol Ther. 2011;13(5):501–507. doi:10.1089/dia.2010.0106
3. Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi:10.1016/j.diabres.2017.03.024
4. Nnamudi AC, Orhue NEJ, Ijeh II. Assessment of the FINDRISC tool in predicting the risk of developing type 2 diabetes mellitus in a young adult Nigerian population. Bull Natl Res Cent. 2020;44(1):186. doi:10.1186/s42269-020-00440-7
5. Levitt NS. Diabetes in Africa: epidemiology, management, and healthcare challenges. Heart. 2008;94(11):1376–1382. doi:10.1136/hrt.2008.147306
6. Selph S, Dana T, Blazina I, Bougatsos C, Patel H, Chou R. Screening for type 2 diabetes mellitus: a systematic review for the U.S. Preventive services task force. Ann Intern Med. 2015;162(11):765–776. doi:10.7326/M14-2221
7. Brown N, Critchley J, Bogowicz P, Mayige M, Unwin N. Risk scores based on self-reported or available clinical data to detect undiagnosed Type 2 Diabetes: a systematic review. Diabetes Res Clin Pract. 2012;98(3):369–385. doi:10.1016/j.diabres.2012.09.005
8. Paulweber B, Valensi P, Lindström J, et al. A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res. 2010;42(S 01):S3–S36. doi:10.1055/s-0029-1240928
9. Glümer C, Carstensen B, Sandbæk A, et al. Risk Score for Targeted Screening. Diabetes Care. 2004;27(3):727–733. doi:10.2337/diacare.27.3.727
10. Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26(3):725–731. doi:10.2337/diacare.26.3.725
11. Zhou X, Qiao Q, Ji L, et al. Nonlaboratory-based risk assessment algorithm for undiagnosed type 2 diabetes developed on a nation-wide diabetes survey. Diabetes Care. 2013;36(12):3944–3952. doi:10.2337/dc13-0593
12. Hippisley-Cox J, Coupland C. Development and validation of QDiabetes-2018 risk prediction algorithm to estimate future risk of type 2 diabetes: cohort study. BMJ. 2017;j5019. doi:10.1136/bmj.j5019
13. Lindström J, Louheranta A, Mannelin M, et al. The Finnish Diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care. 2003;26(12):3230–3236. doi:10.2337/diacare.26.12.3230
14. Janghorbani M, Adineh H, Amini M. Evaluation of the Finnish Diabetes Risk Score (FINDRISC) as a screening tool for the metabolic syndrome. Rev Diabet Stud RDS. 2013;10(4):283–292. doi:10.1900/RDS.2013.10.283
15. Rodríguez MG, Saldaña MR, Leyva JMA, Rojas RM, Molina-Recio G. The FINDRISC questionnaire capacity to predict diabetes mellitus II, arterial hypertension and comorbidity in women from low-and-middle-income countries. Health Care Women Int. 2020;41(2):205–226. doi:10.1080/07399332.2019.1680678
16. Muñoz-González MC, Lima-Martínez MM, Nava A, et al. FINDRISC modified for Latin America as a screening tool for persons with impaired glucose metabolism in Ciudad Bolívar, Venezuela. Med Princ Pract. 2019;28(4):324–332. doi:10.1159/000499468
17. Alberti KGMM, Zimmet P, Shaw J. International Diabetes Federation: a consensus on Type 2 diabetes prevention. Diabet Med J Br Diabet Assoc. 2007;24(5):451–463. doi:10.1111/j.1464-5491.2007.02157.x
18. Roglic G. WHO Global report on diabetes: a summary. Int J Noncommunicable Dis. 2016;1(1):3. doi:10.4103/2468-8827.184853
19. Rokhman MR, Arifin B, Zulkarnain Z, et al. Translation and performance of the Finnish Diabetes Risk Score for detecting undiagnosed diabetes and dysglycaemia in the Indonesian population. PLoS One. 2022;17(7):e0269853. doi:10.1371/journal.pone.0269853
20. Lim HM, Chia YC, Koay ZL. Performance of the Finnish Diabetes Risk Score (FINDRISC) and Modified Asian FINDRISC (ModAsian FINDRISC) for screening of undiagnosed type 2 diabetes mellitus and dysglycaemia in primary care. Prim Care Diabetes. 2020;14(5):494–500. doi:10.1016/j.pcd.2020.02.008
21. Châu LM, Cảnh ĐX. The prediction of type 2 diabetes for next years in 3 districts in Hung Yen province using the FINDRISC tool (Dự báo bệnh đái tháo đường typ 2 tại 3 huyện tỉnh Hưng Yên 10 năm theo thang điểm FINDRISC). Vietnam J Prev Med. 2019;29(2):52–59.
22. Mai VQ, Đạt NV, Thiệu LH, et al. Prediction of undiagnosed diabetes and prediabetes by Findrisc scale in subjects over 45 years old in Khanh Hoa province (Dự báo tiền đái tháo đường và đái tháo đường không được chẩn đoán ở đối tượng trên 45 tuổi tại tỉnh Khánh Hòa theo thang điểm FINDRISC). Vietnam J Prev Med. 2017;28(8):95–102.
23. Trần HD, Nguyễn ĐK. Study on the risk of diabetes by FINDRISC scale in hypertension patients (Nghiên cứu nguy cơ đái tháo đường theo thang điểm FINDRISC trên bệnh nhân tăng huyết áp). Vietnam J Diabetes Endocrinol. 2020;39:23–27. doi:10.47122/vjde.2020.39.3
24. Vinh NT. Using FINDRISC in screening for type 2 diabetes (Sử dụng thang điểm FINDRISC trong sàng lọc đái tháo đường tuýp 2). Vietnam J Health Policy. 2020;30:69–75.
25. Hajian-Tilaki K. Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014;48:193–204. doi:10.1016/j.jbi.2014.02.013
26. The Lancet Infectious Diseases. COVID-19: endgames. Lancet Infect Dis. 2020;20(5):511. doi:10.1016/S1473-3099(20)30298-X
27. Vietnamese Ministry of Health. Coronavirus disease (COVID-19) outbreak in Vietnam; 2020. Available from: https://ncov.moh.gov.vn/.
28. World Health Organization. Novel coronavirus (2019-nCoV) technical guidance; 2021. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technicalguidance.
29. Bui TV, Blizzard CL, Luong KN, et al. National survey of risk factors for non-communicable disease in Vietnam: prevalence estimates and an assessment of their validity. BMC Public Health. 2016;16:498. doi:10.1186/s12889-016-3160-4
30. World Health Organization, Regional Office for the Western Pacific, International Association for the Study of Obesity, International Obesity TaskForce. The Asia-Pacific Perspective: redefining Obesity and Its Treatment; 2002.
31. Jølle A, Midthjell K, Holmen J, et al. Validity of the FINDRISC as a prediction tool for diabetes in a contemporary Norwegian population: a 10-year follow-up of the HUNT study. BMJ Open Diabetes Res Care. 2019;7(1):e000769. doi:10.1136/bmjdrc-2019-000769
32. Do IT, Tran HD, Ton TT, et al. Risk prediction model for type 2 diabetes mellitus using Finnish diabetes risk score (FINDRISC) among adult population in Da Nang city. Vietnam J Prev Med. 2017;2:137–141.
33. Hageman S, Pennells L, Ojeda F; SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439–2454. doi:10.1093/eurheartj/ehab309
34. de Vries TI, Cooney MT, Selmer RM; SCORE2-OP working group and ESC Cardiovascular risk collaboration. SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur Heart J. 2021;42(25):2455–2467. doi:10.1093/eurheartj/ehab312
35. Chen D, Zhang H, Cui N, et al. Development of a behavior change intervention to improve physical activity adherence in individuals with metabolic syndrome using the behavior change wheel. BMC Public Health. 2022;22(1):1740. doi:10.1186/s12889-022-14129-1
36. Lemstra M, Bird Y, Nwankwo C, Rogers M, Moraros J. Weight-loss intervention adherence and factors promoting adherence: a meta-analysis. Patient Prefer Adherence. 2016;10:1547–1559. doi:10.2147/PPA.S103649
37. Akinosun AS, Polson R, Diaz-Skeete Y, et al. Digital technology interventions for risk factor modification in patients with cardiovascular disease: systematic review and meta-analysis. JMIR MHealth UHealth. 2021;9(3):e21061. doi:10.2196/21061
38. Hinchliffe N, Capehorn MS, Bewick M, Feenie J. The potential role of digital health in obesity care. Adv Ther. 2022;39(10):4397–4412. doi:10.1007/s12325-022-02265-4
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
