Back to Journals » Risk Management and Healthcare Policy » Volume 16
Medical Personnel Behavior Preferences for Providing mHealth Service in China: A Discrete Choice Experiment
Authors Jiang S, Xiong M , Rao X, Liang J, Zhu X, Fu H, Chen J , Wang C
Received 8 August 2023
Accepted for publication 30 October 2023
Published 10 November 2023 Volume 2023:16 Pages 2405—2418
DOI https://doi.org/10.2147/RMHP.S430636
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gulsum Kubra Kaya
Shuai Jiang,1,2 Man Xiong,3 Xinyi Rao,3 Jieting Liang,3 Xinghan Zhu,3 Hang Fu,1,2 Jiangyun Chen,3 Chengzeng Wang1,2
1The First Affiliated Hospital of Zhengzhou University, Zhengzhou, Henan, People’s Republic of China; 2Institute for Hospital Management of Henan Province, Zhengzhou, Henan, People’s Republic of China; 3School of Health Management, Southern Medical University, Guangzhou, Guangdong, People’s Republic of China
Correspondence: Chengzeng Wang; Jiangyun Chen, Email [email protected]; [email protected]
Purpose: This study aims to investigate factors affecting medical personnel behavioral preferences for providing mHealth in China, so as to provide decision-making basis for mHealth providers and managers to encourage more doctors to participate in mHealth service delivery.
Methods: Typical case sampling techniques were applied in a hospital setting to conduct a discrete choice experimental questionnaire survey of doctors (n=216) concerning mHealth preferences between July and October 2022. A conditional logit model was used to assess medical personnel preferences for each attribute and level of mHealth services.
Results: Length of service, information security, subjects of treatment and financial compensation all have a significant effect on medical staff’s preference for providing mHealth services (p < 0.05). In terms of service duration and financial compensation, medical staff preferred mHealth services that provided shorter service duration and higher financial compensation; in terms of information security, medical staff preferred mHealth services with confidentiality of diagnostic and therapeutic information compared to information disclosure; and in terms of treatment targets, medical staff preferred the general population compared to key populations, such as pregnant women, the elderly, infants and children.
Conclusion: The preference of medical professionals to provide mHealth services is affected by a variety of factors. By enhancing the confidentiality of information in mHealth services, providing more options for service recipients, increasing their financial compensation, and shortening the duration of the service or increasing the number of service hours that can be adjusted can guide improvement of mHealth services and promoting of its adoption among medical professionals.
Keywords: doctor, mHealth, preferences, discrete choice experiment
Introduction
Background
In recent years, with the integration of the new generation of information technology in the field of health care, new forms of medical services have emerged, and mobile health care, as an innovative medical service model, is gaining more and more attention for researchers and practitioners. Mobile health (M-health), as a new medical service model, has been widely used in China and has a good development prospect in the world.1–3 The essence of mobile health care is to provide medical services with the help of mobile communication technology and mobile medical devices, regardless of time, space and geographical location.4 At present, China’s mobile medical care is promoted and applied in medical institutions, medical personnel and resident groups, and mainly smart phone applications, involving medical consultation, health management, diagnosis and treatment services, etc. Although the rapid widespread adoption of mHealth has constituted a disruption to traditional clinician-patient relationships, to a certain extent, it has compelled structural reform in the provision of health care, while effectively increasing the efficiency of medical services and improving the health status of the population.
In the background of the rapid update of mobile communication technology and equipment, the first domestic mobile medical application APP or service platform (such as Good Doctor, Chunyu Doctor) have been pushed to the medical service market, and this type of app has functions of video consultation, text communication, voice communication, provision of health consultation, treatment plans, etc.,5 and mobile medical has entered a rapid development stage. On the other hand, the pandemic undoubtedly increases the motivation for mobile healthcare deployment. The quarantine policy during the epidemic has promoted the transition from offline to online medical care, and brought new possibilities for the development of mobile medical care.6 From the perspective of service content, mobile medical services are rich, mainly including (1) mobile terminals and APP-type services for patients, providing services such as appointment registration, online diagnosis and treatment, medical and health consultation, chronic disease health management, etc.; (2) mobile diagnosis and treatment services for medical personnel, providing mobile nursing, mobile room check, remote monitoring, online learning (such as literature, medication knowledge), patient health management and question and answer services. Currently, there are no clear and unified laws and regulations on mHealth prescriptive rights, and there are disputes over the prescriptive rights stipulated in the regulations of various mHealth management practices.
Medical personnel play a leading role in the use of mHealth, clinicians are able to apply evidence-based medical practice to leverage health benefits for patients by using mHealth, and imbue trust in making such recommendations.7–9 It is evident that medical professionals generally accept the inevitable trend of introducing mHealth into the medical field, but have some doubts about the use of mHealth, which is not yet mature.10,11 For example, mobile medical APPs tend to focus on a certain type of disease diagnosis and treatment or consultation services, and cannot provide patients with multidisciplinary and holistic medical diagnosis and treatment services. Compared with traditional medical services, mobile medical services are usually in the form of text-based and voice-based communication, which makes it more difficult to realize instant video services between doctors and doctors, doctors and patients, etc. As a result, there are worries about the authenticity of each other’s identity and the authenticity of online consultation and treatment results, which reduces the possibility and motivation of medical personnel and patients to use mobile medical services.
At present, there are less relevant studies on medical personnel preferences for mHealth services in China,12 so this study used DCE to investigate the factors influencing the behavioural preferences of Chinese medical professionals in providing mHealth services, and to further explore the best strategies to improve the delivery of mHealth services by medical personnel. It is conducive to help policymakers improve incentive strategies by understanding behavioral preferences for mHealth services, to increase mHealth provider motivation and recommend mHealth services to more patients, and drive structural changes in healthcare services.
Literature Review
The Concept of mHealth
Mobile Health is closely linked to eHealth and telemedicine. Mobile health was firstly proposed by Robert Istepanian and other scholars, and it originated from “wireless electronic health” services.13 Wireless electronic health refers to the various applications of information and communication technologies in healthcare, including not only the informatization of medical processes within hospitals, but also regionalized medical information sharing and health service models. mHealth is an essential component of eHealth as it comprises the use of mobile communication devices and wearable sensors for the delivery of healthcare services, and the gathering and transmission of health data, enabling continuous monitoring of an individual’s status, rapid diagnosis of medical conditions, identification of behaviors and provision of immediate interventions to improve an individual’s health in a natural mobile environment. The biggest difference between eHealth and mHealth is that mHealth has the mobility of a mobile terminal. Telemedicine emphasizes the use of modern techniques to provide healthcare services focusing on long distances. Mobile healthcare is an aspect of telemedicine development that plays a major role in assisting telemedicine by using web-based systems to provide patients with treatment options in the form of clinic appointments and remote consultations with the help of mobile applications. The World Health Organization (WHO) defines mHealth or mobile health as medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices. It is an extension and complement to medical technology and health services, providing more efficient health services to a wider population, with the potential to not only reduce the pressure on traditional hospital services, but also to increase accessibility and meet individual patient needs.14,15
Policy and Application for mHealth
From the favorable policy, the State Council’s “Guidance on Actively Promoting” Internet+ “Action” requires the development of mobile Internet-based medical and health services in 2015;16 In 2018, the General Office of the State Council’s “Opinions on Promoting the Development of ‘Internet + Medical Health” called for the development of mobile medical demonstrations based on artificial intelligence technology and medical and health smart devices;17 In 2021, the General Office of the State Council “Opinions on Promoting the High-Quality Development of Public Hospitals” pointed out the need to promote the deep integration of new-generation information technology and medical services, and create a policy environment for the development of mobile medical care.18 For resource optimization, it was found that the number of tertiary hospitals per 1000 square kilometers in the eastern, central and western regions of China is 1.17, 0.42 and 0.11 respectively in 2019; the number of tertiary hospitals per 1000 square kilometers were 7.41, 6.25, 3.81 in Shanghai, Beijing, Tianjin municipalities, while Inner Mongolia, Gansu, Qinghai, Xinjiang were less than 0.10.19 This indicates that China’s high-quality medical resources are excessively concentrated in developed urban areas, and it is more difficult for residents in grassroots, remote and underdeveloped areas to obtain equitable medical services, while mobile medical services can provide medical services across time and space. In terms of the degree of informationization, the degree of construction of China’s communication network infrastructure and the number of Internet users have gradually increased. According to the “Statistical Report on the Development of the Internet in China” released in 2022, as of June 2022, the size of online medical users reached approximately 300 million, an increase of 1.96 million from December 2021, accounting for 28.5% of overall Internet users.20 During the outbreak of the COVID-19, mobile health care also became an important way for the public to seek medical consultation, reducing the risk of cross-infection and avoiding the crowding of medical resources while meeting patient demands for medical treatment.
mHealth for Medical Personnel
From the available studies, the majority of medical professionals have a supportive attitude towards the use of mHealth. Tanguy Leroy notes that doctors generally find mobile medical apps and devices useful in medicine, and most agree that the simplicity and ease of use of mobile medical apps greatly enhances the efficiency of healthcare professionals and brings great convenience to their work.21,22 Odendaal, Willem et al also argue that the use of mHealth has not only brought about closer collaboration between healthcare professionals, but has also improved their relationship with patients.23 However, some physicians are concerned about the security of mHealth apps and have some concerns about the privacy and security of patient data, fearing the potential risks posed by inappropriate data, which provides a significant barrier to wider adoption of mHealth by clinicians.24,25 Aline Sarradon-Eck et al noted that physicians tend to be cautious about recommending mHealth apps to their patients, even if they have a positive attitude toward mHealth procedures.26,27
Currently, studies have focused on what factors influence physicians’ willingness to use mHealth, mostly using the expectation confirmation model, technology acceptance model, dual path model, and UTAUT information system continuous use model to explore the impact of variables related to perceived usefulness and perceived ease of use on users’ continuous use.28 For example, Ju-Ling Hsiao, based on the ECM model, states that mHealth usage is mainly influenced by perceived usefulness, technology maturity, personal habits, task mobility, and user satisfaction.29 Hooi Min Lim and Boonchai Kijsanayotin et al pointed out that the more common factors that influence physicians to provide mHealth services are: performance expectations, effort expectations, social influence, convenience, etc.30–33 Gagnon et al concluded from a systematic study that the factors that promote the adoption of mHealth by healthcare professionals include perceived ease of use, perceived usefulness, interoperability, and proficiency with the technology, and that individual factors (knowledge, attitudes, and socio-demographic characteristics), and external factors (organizational environment) also contribute to some extent.34 However, these studies were often based on traditional questionnaires that allowed medical professionals to select the factors they considered important among many, an idealized selection scenario. When facing the actual situation, medical providers often chose their preferred factors among many influencing factors. Therefore, discrete choice experiments are more useful for measuring the preference of medical personnel for each important attribute of mHealth.
Theoretical Framework: Discrete Choice Experiments
Discrete choice experiments (DCE) are the most widely used quantitative method for exploring individual preferences in the field of health economics and policy research. At present, the research on discrete choice experiments in the field of health services in China mainly focuses on the field of primary health services, public health services, clinical treatment services, etc. However, most of the studies were conducted from the demand-side perspective, and there were relatively more cases using discrete choice experiments to analyze the preferences of demand and utilization of health services, lacking the supply-side perspective to explore their preferences for the choice of supply content and mode and their compensation willingness.35
Material and Methods
Sample and Data Collection
In this study, typical case sample was used and the First Affiliated Hospital of Zhengzhou University was selected as the survey site. The First Affiliated Hospital of Zhengzhou University is the only national engineering laboratory of Internet medical system and application and national telemedicine center in China, which is dedicated to key technology development and transformation, standard and specification development, industrial service support, talent training in the fields of Internet medical terminal development and testing, Internet medical software system development and testing, medical and health big data analysis and application, medical artificial intelligence and smart medical etc. The development of its telemedicine center has reached a leading level in China, forming a new telemedicine service model with inter-hospital data exchange platform as the main platform and video system as the supplement. On the other hand, not all medical staff are qualified to provide mHealth services, so we chose medical staff of medical organizations that are qualified to provide mHealth services as survey respondents. Therefore, the First Affiliated Hospital of Zhengzhou University is an ideal location to investigate the preference factors of medical staff in providing mHealth services.
The study population was selected using typical case sampling and simple random sampling, firstly, all the doctors in the sample organization who had provided mHealth services were identified through typical case sampling to form the sample frame (n=432), based on which 50% of the sample who met the inclusion criteria were selected through random number table method using simple random sampling and the questionnaire survey was conducted from July to October 2022 among the medical personnel of the sample hospital. (1) The inclusion criteria were: ①Professionals engaged in mobile medical work and service providers of medical work ②Willingness to participate in the survey with the principle of informed consent. (2) The exclusion criteria were: difficult to communicate, difficult to understand the content of the questionnaire or subjects who did not accept informed consent. (3) All participants will not receive any financial or other incentives for participating in this study.
Discrete Choice Experiment
The Discrete Choice Experiment (DCE) is one of the classic measurement methods for stated preference. DCE assumes that a good or service can be described by several characteristics, each characteristic can define different levels, combine these characteristics and levels to form a questionnaire composed of a series of choice sets, and then the research object makes choices in these selection sets, and after statistical analysis of these selection results, the influence of characteristic factors on the willingness to choose and the preference of the research object for feature factors can be analyzed.36 It can guide the research subject to consider multiple factors at the same time, reflecting the subject’s own process of weighing each characteristic.
Identification of Attributes and Levels
In this study, a total of six characteristic factors to be included in the experiment were established through literature review, namely, length of service, financial compensation, mobile device characteristics, patient evaluation, technical support, and information security; and three were established through expert opinion, namely, response time limit, treatment pattern, and treatment target. Pre investigation is a necessary step for DCE investigation. Usually, pre-testing provides an opportunity to review several elements of the design process, including the selection and definition of attributes and their levels. As with other studies of discrete choice experiments, six characteristic factors were finally screened and identified from nine characteristic factors for inclusion in the experiment through a qualitative survey method. The research team conducted a small-scale qualitative survey of medical personnel at the sample hospital, which is the First Affiliated Hospital of Zhengzhou University, using purposive sampling to investigate the views and opinions of mHealth provider of different ages, education levels, professional titles, and years of experience on these nine characteristic factors, asking them to check their most important influencing factors in providing mHealth services or to add them, as well as asking them to define the levels of some characteristics, and finally determining the characteristic factors and levels to be included in the experiment. Among them, the length of service is the number of hours per day for medical staff to provide mHealth services, the response time limit refers to whether there is a time limit for medical staff to reply when using mHealth diagnosis and treatment, information security refers to the fact that doctors do not disclose information such as diagnosis and treatment during the process of providing mobile medical services, the target of treatment is divided into the general population and the key populations, and the general population refers to populations other than the key populations of pregnant women, elderly people, infants and young children, and the mode of treatment is divided into graphic, audio and video, specific information is shown in Table 1.
 |
Table 1 Characteristics and Levels of Inclusion in Discrete Choice Experiments |
Experimental Design and Development of the Questionnaire
Participants were asked to choose among different levels of attributes and select their preferred mHealth service model. A total of three three-level factors and three two-level factors were identified in this study, which would result in a total of 33×23 = 216 options for different characteristics of mHealth services, and if these options were then combined in two-by-two groups to form a choice set, 23,220 (=216 × 215/2) choice sets could be formed. Obviously, it is not feasible to include all of these choice sets in the choice test questionnaire. Therefore, an orthogonal design was carried out in this study through the SPSS program. In the orthogonal design, the number of factors (attributes) to be included in the experimental study and the number of levels (the number of levels corresponding to the attributes) for each factor are first entered into SPSS, and 18 options are generated by running the program, one of which is used as the reference group, and the remaining 17 options are compared with it separately to form a choice set, and the combinations of the reference and comparison groups with obvious advantages and disadvantages are eliminated to form the final 15 choice sets. Considering the level of understanding of the choice test, the 15 choice sets were divided into two copies, ie, two questionnaires were formed A\B. The other parts of the two questionnaires were the same, but only the choice set of the choice test was different.
According to the rule of thumb proposed by Johnson and Orme,37,38 the minimum sample size for the DCE study can be calculated using the following formula: N > 500c/(t*a). Where 500 is a fixed value, c represents the maximum number of levels in any attribute, t denotes the number of discrete choice experimental questions per questionnaire, and a refers to the number of options included in each discrete choice experimental question. The maximum number of levels among the 6 attributes in this study is 3, so c=3; the final questionnaire contains a total of 8 discrete choice experimental sets, and each discrete choice experimental set contains a total of 2 options (choice 1, choice 2), so the minimum sample size for this study is 94 cases according to the rule of thumb.
The questionnaire is divided into two parts, the first part is the basic demographic information of the respondents, such as age, gender, education level, marital status, professional title, department, years of work, annual income, etc. The other part is the discrete choice experiment part, which asks the respondents to consider their favorite mHealth model in the task selection scenario, each respondent has 8 or 7 scenarios, each scenario has 2 alternatives, each scenario includes 6 attributes, each attribute has up to 3 levels, and the task selection example is Table 2. We distributed paper questionnaires to respondents and collected completed questionnaires on the spot, with an average completion time of 10 minutes.
 |
Table 2 Example of a Discrete Selection Task |
Data Analysis
The research data were organized according to the discrete selection experimental analysis specification by Excel, and Stata 17.0 was used to analyze the discrete selection hybrid logit model and willingness to pay, and SPSS 21.0 was used for other analyses.
Descriptive Analysis
The general demographic characteristics and work information of the study subjects were described, the mean ± standard deviation was used for continuous variables, and the frequency was used for categorical variables.
Analysis of Influencing Factors
Analysis of mHealth Service Preferences Based on Discrete Choice Experiments
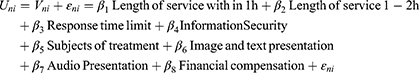
A mixed logit model was developed with the medical personnel’s preference for choice as the dependent variable and the length of service, time limit for response, information security, Subjects of treatment, treatment pattern, and financial compensation as the independent variables, in which any one level of each attribute was used as the base level, and the regression coefficients could be used to indicate the degree of preference of other levels relative to this level. The theoretical basis for the data analysis of the discrete choice experiment is random utility theory. The theory assumes that individual n will choose the one with the highest utility (U) from among J alternative policy options, that is, an individual will choose policy option i over policy option j when and only when Uni>Unj. The utility U can be expressed as:
Where Vni is the observable part of the model; and εni is the unobservable part of the model, reflecting uncertainty factors such as random error and individual variation in preferences. The probability of choosing institution i over institution j when both institution choices are presented to individual n at the same time (Pni), can be expressed as
Combining (Equation 1), then
In the analysis of discrete choice trials, assuming that the logistic distribution is obeyed, it can be deduced from probability theory that the probability of choosing institution i among all study subjects is  (3). Using the great likelihood method, the coefficients in (Equation 1) can be estimated to represent the influence of each factor on the preference for mobile health services. This step can be implemented using STATA’s clogit module.
(3). Using the great likelihood method, the coefficients in (Equation 1) can be estimated to represent the influence of each factor on the preference for mobile health services. This step can be implemented using STATA’s clogit module.
Estimation of Willingness to Pay
Willingness to pay (WTP) refers to the amount of compensation that each particular category of people is willing to pay for a given level of improvement in an attribute of the program, or for a change in an attribute that is not in line with the preferences of that category of people. In this study, “financial compensation” is treated as a continuous variable to estimate the equation, and then the willingness to pay is estimated by calculating the negative of the ratio of the regression coefficients of other characteristics to the regression coefficients of costs. “-βconfidentiality of treatment information /βfinancial compensation”, the value of which indicates how much medical professionals are willing to reduce their financial compensation in order to receive mobile health services with confidentiality of treatment information.
In addition, according to (Equation 3), the coefficient value of the corresponding feature level can be substituted, and the influence of changing the level of a certain feature factor on the selection can be calculated. For example, when the levels of other characteristic factors are all at the baseline level and the treatment target is changed from the general population to the focus population, the selection probability changes to Pgeneral population - Pfocus population. Finally, subgroup analysis was done for medical personnel of different ages, genders, education levels, income levels, professional titles, departments, and years of experience to compare the mHealth selection preferences of medical personnel with different background characteristics.
Results
Participants’ General Information
A total of 216 individuals met the inclusion criteria for this study, and 216 questionnaires were distributed and collected. Because only physicians are qualified to provide mHealth services in China, we excluded nurses and other paramedics. The results showed that the respondents were concentrated in the age group of 31–40 years (74.1%), predominantly female (53.7%), married status (83.3%), doctoral degree (59.3%); professional titles predominantly intermediate (74.1%), more specifically, professional title refers to the rank designation of professional and technical personnel’s professional and technical level, ability and achievement. The professional title here refers to the ranking of Chinese doctors based on their technical service capabilities. The departments in which the respondents work are mainly medical and surgical departments (77.7%).Medical personnel with 1–5 years of work experience accounted for 46.3%, and 6–10 years accounted for 37%; their annual income was mostly RMB 100,000–200,000 (50%). More detail can be seen in Table 3.
 |
Table 3 Descriptive Analysis |
Medical Personnel’s Preference for mHealth
The results showed that among the six attributes included in the study, length of service, information security, subjects of treatment, and financial compensation all had a significant impact on the mobile medical preference of medical personnel (P<0.05). In terms of service duration, based on more than 2h per day, the coefficient values of within 1h per day and 1–2h per day β=0.568 and 0.444, that is, medical personnel are more inclined to choose mobile medical services with shorter service hours. In terms of information security, based on the disclosure of diagnosis and treatment information, medical personnel tend to choose the confidentiality of diagnosis and treatment information (β=0.669). In terms of diagnosis and treatment target, based on priority groups, medical personnel tend to choose the general population (β=0.474). In terms of financial compensation, medical personnel tend to choose mobile medical services with higher financial compensation (β=0.005). More details are presented in Table 4.
 |
Table 4 Analysis of Discrete Selection Test Results |
Willingness to Pay
The results in Table 5 show that there is a significant difference (P < 0.05) in the willingness of medical personnel to pay for length of service, information security, and subjects of treatment. Based on the service duration of more than 2h per day, medical personnel are willing to sacrifice 123.42 yuan in compensation in exchange for service hours of less than 1 hour per day, and are willing to sacrifice 96.53 yuan in compensation in exchange for 1–2 hours of service per day; in terms of information security, medical personnel were willing to sacrifice 145.3 yuan in financial compensation for mobile medical services with confidential treatment information; in terms of treatment targets, medical personnel were willing to sacrifice 103.03 yuan to switch from the priority population to the general population.
 |
Table 5 Analysis of Willingness-to-Pay Results |
Differences in Medical Personnel’s Preferences for mHealth by Different Characteristics
To further analyse the impact of population heterogeneity on mHealth preferences, subgroup analyses of the mHealth preferences of medical personnel were further conducted, categorized by gender, marital status, professional title, and department. The results of the gender subgroup analysis showed that there was no significant difference in the preference for mHealth between males and females, and the preference was consistent with that of the overall population. The results of the marital status subgroup revealed that the preference of the unmarried and married population was consistent with that of the overall population in terms of length of service, treatment recipients, and financial compensation, and in terms of information security the married people preferred confidentiality of treatment information (β=0.716, p<0.01), while the preference of the unmarried people was not significant. The results of the professional title subgroup showed that medical personnel with intermediate and associate senior professional titles preferred shorter service hours and general population as the target group, while medical personnel with junior and intermediate professional titles preferred confidentiality and there was no significant difference between professional titles in terms of financial compensation. The results of the subgroup of departments indicated that the preferences of internal and surgical departments in terms of information security, diagnosis and treatment objects, and financial compensation were the same, in terms of service duration, surgical medical personnel tended to choose shorter service duration, internal medicine medical personnel did not have obvious preferences, and in terms of diagnosis and treatment mode, internal medicine medical personnel tended to display graphics and text (β=0.599, p<0.01) and audio display (β=0.710, p<0.01), while surgery had no obvious preference (see Supplementary Tables S1–S4 for details).
Discussion
Principal Results
This study investigated the choice preferences of medical personnel for mHealth services through a discrete choice experiment conducted in a major tertiary referral hospital in China. The results demonstrate that the length of service, information security, subjects of treatment, and financial compensation are important factors affecting the provision of mobile medical services by medical personnel. Medical providers are more likely to choose mobile medical services with shorter service duration, confidential diagnosis and treatment information, treatment for the general population, and higher financial compensation, which is consistent with other studies.
Length of Service Factor
Cesuroglu Tomris et al point out that healthcare professionals focus on the time and workload of using mHealth and they emphasize that their limited time makes it difficult to add mHealth-related work to their original workload.39 In her analysis of the current situation of internet diagnosis and treatment use by medical personnel in a tertiary hospital in Anhui Province, it was found that 48% of doctors and nurses believe that “using internet medical care will take up a lot of my life and work time and increase my work burden”.40 It’s been shown that medical professionals work an average of 49.89 hours per week, and they have heavy workloads, often work overtime and under pressure, have difficulty allocating more energy to provide mobile medical services, and tend to use mobile medical applications during breaks and off hours.41,42 In view of this, each medical institution or medical staff themselves should develop a reasonable work allocation mechanism to avoid conflicts between online and offline treatment, consider the physiological and psychological needs of medical personnel, enhance the experience and proficiency of medical staff in using the equipment through equipment support and technical training, and reduce the extra work burden.
Information Security Factor
At the same time, data privacy is challenged in the information age and information leakage happen on occasion. Doctors often have certain differences in the level and means of disease diagnosis and treatment, so who with higher medical technology usually worry that their diagnosis and treatment processes and results will be made public on the Internet, and are skeptical about the information security and confidentiality of mobile medical,24,27 preferring to keep the diagnosis and treatment information confidential. Oyungerel Byambasuren agrees that mHealth effectiveness, safety and usability issues can constrain the use of mHealth by medical professionals and reduce their confidence in providing mHealth services.27 Therefore, the management of mobile medical and Internet hospitals should strengthen the monitoring and management of medical data, actively improve network security measures, and establish a multi-dimensional network medical information security mechanism to ensure the standardized and efficient operation of mobile medical.43
Factor of Treatment Target
Medical professionals tend to offer mHealth services to the general population in order to minimise medical risks and associated medical disputes. Kerstin A Kessel’s study identifies mHealth medical liability and data privacy uncertainty as the main reasons why healthcare professionals are reluctant to use mHealth.44 Some doctors believe that the biggest disadvantage of online treatment is that they cannot ensure the quality of medical services and are worried about medical safety and medical disputes caused by online treatment.42 Medical professionals have different preferences for different treatment subjects, it may be because the symptoms of the general population are mild, clinically obvious and easy to diagnose, while priority populations, such as the elderly, infants and young children, and pregnant women, have complex and variable conditions, often with multiple complications, and the symptoms of the elderly and infants are often poorly described and result in making it difficult to diagnose and treat through mobile health.
Financial Compensation Factor
In terms of financial compensation, the price mechanism for mobile medical services is imperfect and physicians are relatively under compensated financially. In Beijing municipal hospitals, for example, the service fee for internet medical treatment is the price of general outpatient services, and the low medical service fee does not reflect the value of physicians’ labor, which greatly affects the motivation of doctors to carry out mobile internet medical treatment.45 In addition, the existing mobile medical service are mostly uniformly priced in medical institutions at different levels or doctors with different professional titles, and the lowest level of consultation fees is 25 yuan per visit, which does not truly reflect the labor value, and in particular, it will hinder the use of mHealth by doctors with the associate senior or senior professional title.42 From the patient’s perspective, patients think that their treatment results through mobile medical online services is lower than the offline face-to-face traditional service mode. As a result, they are reluctant to pay more for mobile health. The White Paper on online health services consumption in China showed that 32.2% of patients were willing to pay 11–30 yuan for an online medical consultation, while 31.5% of patients were willing to pay 31–60 yuan per visit, which clearly did not match the income expectation of doctors,46 and it could reduce physicians’ willingness to use mHealth. Therefore, on the one hand, the government should reform the price mechanism of mobile medical treatment, set reasonable price standards according to the characteristics of mobile medical treatment, and make flexible pricing for medical personnel in different service levels. On the other hand, it is necessary to make patients more aware of mHealth and willing to pay for it by strengthening the social publicity of mHealth and improving the cognitive value of patients and doctors.
Preferences of Medical Personnel with Different Characteristics
In the meantime, it also explored the differences in preferences for mHealth among medical professionals with different characteristics. The results show that married doctors prefer the information confidentiality of the diagnosis and treatment, while unmarried doctors have no significant preference for information security. The possible reason is that those married doctors have more complicated social relationships, and pay more attention to information security, which they are concerned about the impact of information leakage on individuals and even families.
From the professional title level in job, medical health providers who have the associate senior and senior professional title prefer the shorter time lengths in the mHealth compared to those junior professional title medical personnel. Most likely because those with associate senior professional title or above are responsible for more medical tasks including the diagnosis and treatment of difficult diseases, teaching, scientific research and administrative work, their work intensity and work pressure are higher than those with junior professional titles, and they have less time to provide mHealth services. Those mHealth providers who have the junior professional title has no obvious preference for treatment targets, it may be because they are in the stage of learning and growth for gathering experience in diagnosis and treatment, and they do not deliberately choose patients, while associate senior or senior doctors prefer provide mHealth for the general population. In terms of information security, medical personnel who have junior and intermediate professional titles more prefer the confidentiality of medical treatment information, while those with associate senior or senior professional title have no obvious preference, probably because those with junior professional titles are mostly young people who are more exposed to mobile internet medical and have a stronger awareness of confidentiality of information security.
Subgroup analysis of the physicians and surgeons also showed significant differences in preferences, with surgery preferring mobile medical services with shorter service lengths. It may be because surgery is generally based on surgical treatment, which takes up more time and energy with long and intensive work. As far as treatment mode, physicians prefers graphic and audio presentation in internal medicine, while surgeons have no clear preference. Probably because physicians can provide medical services in the form of remote diagnosis and consultation, and it is suitable for text description or inspection report and other graphic communication, which are highly adaptable to online medical mode, and treatment options are readily available through simple graphic and audio descriptions, which the diagnosis and treatment options includes follow-up observation, lifestyle intervention, medication, and interventional therapy.
Conclusion
In this study, based on the results of discrete choice experiments, it demonstrates the choice preference of medical personnel for mobile medical service models. Length of service, information security, subjects of treatment, and financial compensation are the four important attributes of mobile medical services, which inspire mobile medical providers to strengthen the confidentiality of system information security, introduce mobile medical services into the daily services of hospitals for complementing offline diagnosis and treatment by optimize service models and processes, improve the enthusiasm of medical personnel to provide mobile medical services through economic compensation and other material incentives, and further promote the healthy, sustainable and stable development of mHealth services.
Strengths and Limitations
In this study, the method of discrete choice experiment was used to explore the behavioral preferences of medical personnel in mobile health services, and the preferences were measured by setting scenarios and weighing choices, which could quantitatively describe the preferences of medical personnel. Different from the traditional questionnaire survey method based on actual choice behavior, the method of discrete selection experiment can avoid the constraints of real situation and quantitatively understand the preference of medical personnel for various characteristic factors. At the same time, this study takes medical personnel as the main survey object, and explores the application status and development path of mobile medical service from the perspective of mobile medical service providers, which is different from the previous patient-oriented research on patients’ willingness to use mobile medicine, which can provide a more comprehensive perspective for the development and improvement of mobile medical care.
This study also has some limitations. Firstly, the study used typical case sampling and was conducted only in the First Affiliated Hospital of Zhengzhou University, with some risk of sampling or selection bias. The sample is well represented for the sample institutions, but is limited in its representativeness for the nation’s eligible physicians. Secondly, the literature review and expert interview were used for identified the level of attributes, the hypothetical scenarios presented in the questionnaire may not exactly match real life, and this study only listed six factors that characterise mobile health services, possibly ignoring others. Thirdly, as the questionnaire for the discrete choice experiment was more complex than the general questionnaire, medical personnel may not have fully understood the purpose of the experiment and may have preferred one level of attribute over the others in their selection. In the future, we will expand our sample size and further deepen our research.
Ethics Statement
This study conformed to the principles outlined in the Declaration of Helsinki. This study was conducted with approval from the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. The ethics committee approved verbal informed consent for interview participants. Participation in the study was voluntary. Verbal informed consent was obtained from all of the participants before data collection, and the participants were explicitly informed that their responses would be anonymized and potentially published as part of the research findings.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was the Joint Co-Construction Program of Medical Science and Technology of Henan Province (LHGJ20200347), Undergraduate Research Foundation Program of School of Health Management of Southern Medical University (2022RFU016) and Key Scientific Research Project of Henan Provincial Colleges and Universities (24A630031).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Sun L, Buijsen M. Mobile health in China: Does it meet availability, accessibility, acceptability and quality standards? Health Policy and Technology, 2022; 11(3): 100660. doi:10.1016/j.hlpt.2022.100660
2. Nishimwe A, Ibisomi L, Nyssen M, Conco DN. The effect of a decision-support mHealth application on maternal and neonatal outcomes in two district hospitals in Rwanda: pre - post intervention study. BMC Pregnancy Childbirth. 2022;22(1):52. doi: 10.1186/s12884-022-04393-9
3. Wang YR, Zhang RY, He Q, et al.Analysis on Plights and Countermeasures of Mobile Health Development in China. Medicine and Society, 2017; 30(2): 19–21+44. doi:10.13723/j.yxysh.2017.02.006
4. Yin DT, Zhao WL, Yang Z. Research on teleconsultation model under the perspective of mobile healthcare. Health Economics Research, 2017; 34 (9) :59–62. doi:10.14055/j.cnki.33-1056/f.20170825.004
5. Lv Q, Jiang YT, Qi J, et al. Using Mobile Apps for Health Management: A New Health Care Mode in China. JMIR Mhealth Uhealth, 2019; 7(6):e10299. doi: 10.2196/10299
6. Asadzadeh A, Kalankesh LR. A scope of mobile health solutions in COVID-19 pandemics. Inform Med Unlocked. 2021;23:100558. doi: 10.1016/j.imu.2021.100558
7. Jezrawi R, Balakumar S, Masud R, et al. Patient and physician perspectives on the use and outcome measures of mHealth apps: Exploratory survey and focus group study. Digit Health. 2022; 8:20552076221102773. doi: 10.1177/20552076221102773
8. Hu X, Fang H, Wang P. Factors affecting doctor's recommendation for mobile health services. Digit Health. 2022; 8:20552076221125976. doi: 10.1177/20552076221125976
9. Schroeder T, Seaman K, Nguyen A, et al. Enablers and inhibitors to the adoption of mHealth apps by patients - A qualitative analysis of German doctors' perspectives. Patient Educ Couns. 2023; 114:107865. doi: 10.1016/j.pec.2023.107865
10. Maassen O, Fritsch S, Gantner J, et al. Future Mobile Device Usage, Requirements, and Expectations of Physicians in German University Hospitals: Web-Based Survey. J Med Internet Res. 2020; 22(12):e23955. doi: 10.2196/23955
11. Alazzam MB, Al-Radaideh AT, Alhamarnah RA, et al. A Survey Research on the Willingness of Gynecologists to Employ Mobile Health Applications. Comput Intell Neurosci. 2021; 2021:1220374. doi: 10.1155/2021/1220374
12. Zhang LJ, Wei Q, Sun JW. Research on the preference of doctors in public hospitals to carry out Internet diagnosis and treatment services:Based on discrete selection experiment. Chinese Journal of Health Policy, 2022; 15(11): 39–45. doi:10.3969/j.issn.1674-2982.2022.11.006
13. Laxminarayan S, Istepanian RS. UNWIRED E-MED: the next generation of wireless and internet telemedicine systems. IEEE Trans Inf Technol Biomed. 2000;4(3):189–193. doi:10.1109/TITB.2000.5956074
14. Huang C, Chen YY, Liu XY, et al. Advances in the use of mHealth in nursing. Chin J Pract Nurs. 2019;54(8):1264–1269. doi:10.3761/j.issn.0254-1769.2019.08.031
15. Hu R. Research on the application of mobile medical service based on patient perceived value.Shanghai: Shanghai Jiao Tong University; 2018.
16. The State Council of the People’s Republic of China. The State Council on actively promoting the “Internet +” action guidance; 2015. Available from: https://www.gov.cn/zhengce/zhengceku/2015-07/04/content_10002.htm.
17. The State Council of the People’s Republic of China. General office of the state council on the promotion of “Internet + medical health” development of views; 2018 Available from:, https://www.gov.cn/zhengce/content/2018-04/28/content_5286645.htm.
18. The State Council of the People’s Republic of China. Opinions of the general office of the state council on promoting the high-quality development of public hospitals; 2021. Available from: https://www.gov.cn/zhengce/zhengceku/2021-06/04/content_5615473.htm.
19. Peking union medical college press. China Health Care Statistics Yearbook. Beijing: Peking union medical college press; 2020.
20. China internet network information center, the 50th statistical report on china’s internet development, Available from: https://www.cnnic.com.cn/IDR/ReportDownloads/202212/P020230829504457839260.pdf. 2022.
21. Della VC, Leroy T, Bauquier C, et al. Willingness of French general practitioners to prescribe mHealth apps and devices: quantitative study. JMIR Mhealth and Uhealth. 2022;10(2):e28372. doi:10.2196/28372
22. Jacob C, Sanchez-Vazquez A, Ivory C. Factors impacting clinicians’ adoption of a clinical photo documentation app and its implications for clinical workflows and quality of care: qualitative case study. JMIR Mhealth and Uhealth. 2020;8(9):e20203. doi:10.2196/20203
23. Odendaal WA, Watkins JA, Leon N, et al. Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;3(3) :CD011942. doi:10.1002/14651858.CD011942.pub2
24. Byambasuren O, Beller E, Hoffmann T, et al. Barriers to and Facilitators of the Prescription of mHealth Apps in Australian General Practice: qualitative Study. JMIR Mhealth and Uhealth. 2020;8(7):e17447. doi:10.2196/17447
25. Sarradon-Eck A, Bouchez T, Auroy L, et al. Attitudes of general practitioners toward prescription of mobile health apps: qualitative study. JMIR Mhealth and Uhealth. 2021;9(3):e21795. doi:10.2196/21795
26. Zhang Y, Koch S. Mobile health apps in Sweden: what do physicians recommend? Studies in health technology and informatics. Stud Health Technol Inform. 2015;210:793–797.
27. Byambasuren O, Beller E, Glasziou P. Current knowledge and adoption of mobile health apps among Australian general practitioners: survey study. JMIR Mhealth Uhealth. 2019;7(6):e13199. doi:10.2196/13199
28. Li Y, Liu R. Influencing factors of continuance use intention of mobile health based on meta analysis. J Manag Inf Syst. 2022;31(5):893–909.
29. Hsiao JL, Chen RF. Understanding determinants of health care professionals’ perspectives on mobile health continuance and performance. MIR Med Inform. 2019;7(1):e12350. doi:10.2196/12350
30. Ma CY, Wang QZ. An empirical study on physicians' willingness to adopt online medical service platform and its influencing factors. Chin J Health Policy. 2018;11(6):68–73. doi:10.3969/j.issn.1674-2982.2018.06.011
31. Lim HM, Dunn AG, Muhammad Firdaus Ooi S, et al. mHealth adoption among primary care physicians in Malaysia and its associated factors: a cross-sectional study. Fam Pract. 2021;38(3):210–217. doi:10.1093/fampra/cmaa103
32. Wu P, Zhang R, Luan J, et al. Factors affecting physicians using mobile health applications: an empirical study. BMC Health Serv Res. 2022;22(1):24. doi:10.1186/s12913-021-07339-7
33. Kijsanayotin B, Pannarunothai S, Speedie SM. Factors influencing health information technology adoption in Thailand’s community health centers: applying the UTAUT model. Int J Med Inform. 2009;78(6):404–416. doi:10.1016/j.ijmedinf.2008.12.005
34. Gagnon M-P, Ngangue P, Payne-Gagnon J, et al. m-Health adoption by healthcare professionals: a systematic review. J Am Med Inform Assoc. 2016;23(1):212–220. doi:10.1093/jamia/ocv052
35. Zhang J, Xu L. Application and prospect of discrete choice experiment in the field of health service in China. Soft Sci Health. 2022;36(11):32–35. doi:10.3969/j.issn.1003-2800.2022.11.008
36. Lancsar E, Louviere J. Conducting discrete choice experiments to inform Healthcare decision making. Pharmacoeconomics. 2008;26(8):661–677. doi:10.2165/00019053-200826080-00004
37. Johnson R, Orme B. Sequim Sawtooth Software Research Paper Series. Sequim, WA: Sawtooth Software; 2003:6–7.
38. Orme B. Sample size issues for conjoint analysis studies Sequim: sawtooth software technical paper. Sequim, WA: Sawtooth Software; 1998:6–9.
39. Emberti Gialloreti L, Basa FB, Moramarco S. Supporting Iraqi Kurdistan health authorities in post-conflict recovery: the development of a health monitoring system. Front Public Health. 2020;8:7. doi:10.3389/fpubh.2020.00007
40. He X, Li J, Zhu Q, et al. Investigation and analysis of the status quo of internet diagnosis and treatment by medical staff in a tertiary hospital in Anhui Province. Chin Health Quality Manag. 2021;28(06):27–30. doi:10.13912/j.cnki.chqm.2021.28.6.08
41. Sun J, Luo HY, Feng QM, et al. Job stress and influencing factors of health workforce at primary health care institutions, Guangxi. Mod Prev Med. 2017;44(9):1630–1633.
42. Yao K, Yao JS, Wu LQ, et al. Qualitative analysis of barriers to the promotion of online healthcare of outpatient clinics in internet hospitals based on physicians’ perspectives of a medical group in Shenzhen. Med Soc. 2022;35(9):127–132. doi:10.13723/j.yxysh.2022.09.024
43. Xu XY, Xiang YL, Zhou X, et al. The improvement of doctor-patient relationship by mobile health care and “Internet + medicine”: the case of Nanning City. China Internet Week. 2022;18:54–59.
44. Kessel KA, Vogel MM, Schmidt-Graf F, et al. Mobile apps in oncology: a survey on health care professionals’ attitude toward telemedicine, mHealth, and oncological apps. J Med Internet Res. 2016;18(11):e312. doi:10.2196/jmir.6399
45. Zhang H. Analysis of Internet Diagnosis and Treatment in Beijing Municipal Hospitals. Beijing: Peking Union Medical College; 2022.
46. iResearch. 2022年中国在线医疗健康服务消费白皮书 [White paper on the consumption of online medical and health services in China]; 2022. Available from: https://report.iresearch.cn/report/202209/4057.shtml.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.