Back to Journals » Nature and Science of Sleep » Volume 15
Medical Cannabis Use Patterns for Sleep Disorders in Australia: Results of the Cross-Sectional CAMS-20 Survey
Authors Suraev A , Mills L, Abelev SV, Arkell TR , Lintzeris N, McGregor IS
Received 3 October 2022
Accepted for publication 20 February 2023
Published 17 April 2023 Volume 2023:15 Pages 245—255
DOI https://doi.org/10.2147/NSS.S390583
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Anastasia Suraev,1– 3 Llewellyn Mills,4,5 Sarah V Abelev,1 Thomas R Arkell,6 Nicholas Lintzeris,4,5,* Iain S McGregor1– 3,*
1The University of Sydney, Lambert Initiative for Cannabinoid Therapeutics, Sydney, NSW, Australia; 2The University of Sydney, Faculty of Science, School of Psychology, Sydney, NSW, Australia; 3The University of Sydney, Brain and Mind Centre, Sydney, NSW, Australia; 4Drug and Alcohol Services, South East Sydney Local Health District, Sydney, NSW, Australia; 5Department of Addiction Medicine, Faculty Medicine and Health, University of Sydney, Sydney, NSW, Australia; 6Centre for Human Psychopharmacology, Swinburne University of Technology, Hawthorn, VIC, Australia
*These authors contributed equally to this work
Correspondence: Iain S McGregor, The University of Sydney, Lambert Initiative for Cannabinoid Therapeutics, Level 6, Building M02F, 94 Mallett Street Camperdown, Sydney, NSW, 2050, Australia, Tel +612 9351 0883, Email [email protected]
Introduction: Sleep disorders are the third most common indication for the prescription of medical cannabis products in Australia, after pain and anxiety. While the use of cannabis for medical purposes is growing in Australia, underlying consumer behaviours and patterns of use, particularly around sleep disorders, are poorly understood.
Methods: We conducted a subanalysis of the cross-sectional “Cannabis as Medicine Survey” 2020– 2021 (CAMS-20) (N = 1600), to explore the characteristics of a sample of Australians who were using prescribed and/or illicit medical cannabis to treat a self-reported sleep disorder.
Results: When asked to specify up to seven different conditions they were treating with medical cannabis, a total of 1030 (64%) respondents [mean (SD) 44.9 (13.6) years] selected a sleep disorder, with “insomnia disorder” (85.5%), ‘sleep-related movement disorders’ (26%) and ‘sleep-related breathing disorders’ (11.1%) the most common subtypes. Only 165 (16.8%) respondents selected a self-reported sleep disorder as the main health condition being treated. Relative to other health conditions, use of medical cannabis for a self-reported sleep disorder was associated with younger age, increased likelihood of using both prescribed and illicit forms of medical cannabis, inhaled routes of administration, and THC-dominant products. Most respondents reported a reduction in the use of benzodiazepines and alcohol since starting medical cannabis. Binary logistic regression showed that respondents who predominantly used inhaled routes of administration, and concomitant use of medical cannabis for pain, mental health and/or substance use disorder, or a gastrointestinal disorder, were significantly more likely to also use medical cannabis to treat a self-reported sleep disorder.
Conclusion: Overall, these results suggest that self-reported sleep disorders are often being treated with medical cannabis alongside other health conditions (often pain or a mental health disorder) and that use of inhaled methods, THC-dominant products, and illicit sources of medical cannabis are common among people with self-reported sleep disorders in Australia.
Keywords: medical cannabis, THC, CBD, cannabinoid, insomnia, sleep disorders, survey
Introduction
Sleep is a biological necessity that enables restorative functions that are essential for normal daytime function.1 Approximately 30% of the general population report poor sleep, which may be attributed to lifestyle choices, environmental factors, and/or the presence of an untreated sleep disorder or other medical complaints such as pain.2 Treatment typically involves both pharmacological and behavioural approaches for optimal management. While behavioural interventions such as cognitive behavioural therapy for insomnia (CBT-I) are the mainstay of treatment,3 patients often seek short-term strategies to maintain normal daytime functionwhich often includes adjunctive use of pharmaceutical sleep aids such as benzodiazepines and Z-drugs. However, such drugs are often associated with undesirable side effects and should not be used long term,4 leading to an upsurge of interest into alternative treatments.
Medical cannabis is becoming an increasingly popular alternative to common sleep aids.5,6 In Australia, consumer surveys in 2016,7 20188 and 20209 showed that sleep disorders were the third most common indication treated with medical cannabis (either illicit or prescribed), after pain and mental health disorders. With prescribed medical cannabis, data from the Australian federal regulator, the Therapeutic Goods Administration (TGA), confirm that sleep disorders are the third most common indication being treated after pain and anxiety.10 In the US, a recent survey showed that 74% of people accessing cannabis through adult-use markets in Colorado reported effective treatment for sleep, with a concomitant reduction in the use of prescription sleep aids.5 In Canada, 92.6% of patients using prescribed medical cannabis reported a significant improvement in their sleep after six weeks of treatment as assessed using the Pittsburgh Sleep Quality Index, a validated subjective measure of global sleep quality.11
Despite the increasing worldwide interest in and uptake of medical cannabis as a sleep-promoting drug, clinical evidence supporting the use of cannabis and its constituents in the treatment of sleep disorders is limited.12 A recent systematic review and meta-analysis of 39 studies exploring the effectiveness of medical cannabis for insomnia reported moderate certainty evidence that medical cannabis results in improvements, albeit small, in sleep quality when compared to placebo.13 Most relevant studies involved individuals with insomnia secondary to chronic pain. Therefore, it remains unclear whether this is due to an improvement in sleep per se or an improvement in the associated underlying condition (ie, pain). Only one clinical study to-date has explored the efficacy and safety of cannabinoids in the treatment of insomnia disorder.14 In this randomised, placebo-controlled trial, 2-week treatment with an oral formulation containing 10 mg Δ9-tetrahydrocannabinol (THC), 1 mg cannabinol (CBN), and 0.5 mg cannabidiol (CBD) significantly improved symptoms in patients with chronic insomnia as assessed using the Insomnia Severity Index, a validated self-report questionnaire assessing the nature, severity, and impact of insomnia. Five pre-registered randomised, placebo-controlled trials are currently underway exploring the effects of CBD alone,15–17 CBD-terpene combinations18 and combined CBD and THC19 in insomnia disorder; all oral formulations. Preclinical evidence in obstructive sleep apnea (OSA) suggests that dronabinol (a synthetic form of THC) may reduce serotonin-induced reflex apneas and increase upper airway dilating muscle activity via peripherally-mediated suppression of vagal nerve activity by the endocannabinoid system.20–23 Limited clinical studies in humans with moderate-to-severe OSA have demonstrated significant reductions in apnea-hypopnea index (AHI) with dronabinol use,24,25 however further investigation is required to confirm these findings. One randomised, placebo-controlled, crossover study is currently underway examining a combination of dronabinol and acetazolamide, a carbonic anhydrase inhibitor, in OSA.26 No randomised controlled trials to-date have examined the utility of cannabinoids for restless legs syndrome (RLS). In two case series combining 18 patients with treatment-resistant RLS, smoked cannabis (ie, THC-dominant products) was self-rated as more efficacious in improving RLS symptoms than sublingual CBD.27,28 The evidence base for the use of cannabinoids in the treatment of other sleep disorders has been further reviewed elsewhere.29
Since the introduction of legal (prescribed) medical cannabis in Australia in 2016,10 consumer behaviours and patterns of use of prescribed and/or illicit medical cannabis for sleep disorders remain unclear. Prior surveys suggest that some consumers continue to rely on illicit cannabis products despite legal availability of prescribed medical cannabis and the emergence of guidance for both doctors and patients regarding the prescription and use of medical cannabis.7–9 To further understand consumer behaviors, we conducted a subanalysis of a recent nationwide, cross-sectional survey (“Cannabis as Medicine Survey” 2020–2021 or “CAMS-20”) to characterise patterns of use and perceived efficacy of medical cannabis for the treatment of subjective sleep symptoms among a sample of Australians who report using medical cannabis to treat a self-reported sleep disorder.
The term “medical cannabis” used in this paper refers to any prescribed (legal) or illicit cannabis product (including plant matter) used to treat or alleviate the symptoms of a self-identified health condition. This term does not imply that the cannabis product was indicated or prescribed by a health professional. In the Australian context, prescribed medical cannabis products are strictly regulated, federally approved, quality-assured, and only available on prescription via a medical doctor. All other medical cannabis products are unregulated (ie, of unknown composition) and hereafter referred to as illicit medical cannabis products.
Methods
Study Design
The current investigation was conducted using data collected within the “Cannabis as Medicine Survey” 2020–2021 (CAMS-20); a web-based, cross-sectional survey of Australians who self-reported using cannabis for medical reasons conducted every two years since 2016 (see CAMS-16,7 CAMS-188 and CAMS-20 surveys9). The full methodology and main findings of the CAMS-20 survey are published elsewhere.9 The study was approved by the University of Sydney Human Research Ethics Committee (2018/544) and conducted in accordance with the guidelines of the International Council for Harmonisation and principles of the Declaration of Helsinki.
Recruitment and Eligibility
Respondents were eligible to participate if they: (a) provided informed consent, (b) were aged ≥18 years, (c) resided in Australia, and (d) self-identified as a consumer of prescribed and/or illicit cannabis product(s) for a medical purpose within the previous 12 months. The CAMS-20 survey was available online over a 5-month period between September 2020 and January 2021 and advertised via social media and consumer group pages, at consumer and professional forums, and through several private medical cannabis clinics.
Survey Design
The original survey was developed by the investigators and updated with new questions to reflect the evolving regulatory changes in Australia.30 Data were collected and managed using Research Electronic Data Capture (REDcap), a secure web-based platform.31 Individuals were asked about their (a) demographic characteristics and general health; (b) current and lifetime patterns of medical cannabis use including how they accessed their medical cannabis products (ie, “Prescribed Only”, “Illicit Only” or “Prescribed and Illicit”) and specific questions relating to those products such as route of administration and perceived cannabinoid composition; (c) self-identified health conditions for which they were using medical cannabis; (d) perceived change in their subjective sleep symptom since starting medical cannabis as assessed using the Patient Global Impression of Change Scale (PGIC)32 which uses a 7-point Likert scale ranging from “very much worse” to “very much better”; and (e) change in benzodiazepine and alcohol use since starting medical cannabis (the full survey is available in the Supplementary Materials).
Respondents were asked to nominate up to seven “general conditions” they were treating with medical cannabis from a structured list of different health conditions including “sleep”, “pain”, “cancer”, “mental health and/or substance use”, “neurological”, “gastrointestinal”, and “other”. If “sleep” was selected, participants were then asked to select up to a maximum of three different sleep disorders which they were treating with medical cannabis. These included “circadian rhythm sleep disorder”, “insomnia disorder”, “narcolepsy or other hypersomnia”, “parasomnias”, “sleep apnea or other sleep-related breathing disorder”, “sleep-related movement disorder” (eg, restless legs syndrome), or “other sleep disorder”. Participants were also asked to nominate one “main condition” (eg, “insomnia disorder”) that they were treating with medical cannabis.
Respondents fell into three different groups according to how they sourced their medical cannabis: a “Prescribed Only” group who only used prescribed (regulated) medical cannabis; an “Illicit Only” group who only used illicit (unregulated) medical cannabis obtained via the grey or black market; and a “Prescribed and Illicit” group who were using both prescribed and illicit medical cannabis products.
Data Analysis
Data were analysed using SPSS version 26 (IMB Corp., Armonk, NY) and figures were created using GraphPad Prism version 9 (GraphPad Inc., San Diego, CA). Only valid responses were reported. Responses relating to perceived cannabinoid composition were collapsed into: ‘THC-dominant, ‘CBD-dominant, ‘THC/CBD-equivalent, and ‘Unknown’. Similarly, responses relating to route of administration were collapsed into: ‘Oral Only’, ‘Oral & Inhaled’, ‘Inhaled Only’ and ‘Other’ (e.g., topical, suppository). Independent t-tests were used to compare normally distributed data (i.e., Shapiro–Wilk test) between those who were using medical cannabis to treat a self-reported sleep disorder versus all other health conditions. Non-normally distributed data were analysed using the Mann–Whitney U-test. Categorical variables were compared using Fisher’s exact test or Chi-square test. Chi-square post-hoc analysis using adjusted standardised residuals with Bonferroni correction was conducted for variables with more than two categories.33 A binary logistic regression model was used to explore the influence of demographics (age and gender), cannabis use characteristics (cannabis user type, route of administration, cannabinoid composition), other health conditions treated with medical cannabis (“pain”, “mental health and/or substance abuse”, “gastrointestinal”, “cancer”, “neurological”, or “other”), alcohol use, and benzodiazepine use on the odds of using medical cannabis to treat a self-reported sleep disorder versus all other health conditions. Only statistically significant odds ratios (OR) are reported in-text (p<0.05).
 |
Table 1 Demographic and Other Characteristics of the CAMS-20 Survey Respondents Who Were Using Medical Cannabis to Treat a Self-Reported Sleep Disorder vs All Other Health Conditions |
Results
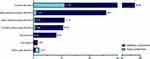
In total, 1600 respondents completed and provided valid responses to the larger CAMS-20 survey. Of these, 1030/1600 (64.4%) self-reported using medical cannabis to treat a sleep disorder when asked to specify up to seven different self-identified health conditions they were treating with medical cannabis. Figure 1 shows the types of self-reported sleep disorders being treated with medical cannabis. “Insomnia disorder” (881/1030, 85.5%) was the most common self-reported sleep disorder followed by “sleep-related movement disorders” (268/1030, 26%), “sleep-related breathing disorders” (114/1030, 11.1%), “circadian rhythm sleep disorders” (109/1030, 10.6%), “parasomnias” (84/1030, 8.2%), “narcolepsy” (15/1030, 1.5%), and “other sleep disorder” (7/1030, 0.7%). Only 165/982 (16.8%) reported using medical cannabis to treat a self-reported sleep disorder as their main health condition. The other main health conditions selected by those with a self-reported sleep disorder were as follows: “pain” (412/982, 42%), “mental health and/or substance use disorder” (319/982, 32.5%), “neurological disorder” (68/982, 6.9%), “cancer” (23/982, 2.3%), “gastrointestinal condition” (22/982, 2.2%), and “other” (55/982, 5.6%) (Supplementary Table S1). Post-traumatic stress disorder (PTSD) was the second most common mental health disorder treated with medical cannabis (54/982, 5.5%).
As Table 1 indicates, the majority of respondents treating a self-reported sleep disorder were male with a mean (SD) age of 44.9 (13.6) years. Most of these respondents (62.8%) accessed their medical cannabis via illicit sources (“Illicit Only”; 647/1030) while 10.7% were using medical cannabis products prescribed by a medical doctor (“Prescribed Only”; 110/1030), and 26.5% had used both illicit and prescribed products in the preceding 12 months (“Prescribed and Illicit”; 273/1030). Those using medical cannabis for a self-reported sleep disorder were younger compared to those using medical cannabis for all other health conditions ([mean (SD), 44.9 [13.6] vs 49.2 [15.2]], p<0.001). Respondents using medical cannabis for a self-reported sleep disorder were also younger when they first started using cannabis (for any reason and for a medical reason) compared to those using medical cannabis for all other health conditions [mean (SD), 21.4 (13.1) vs 25.5 (17.6) and 37.0 (14.9) vs 42.0 (15.9), respectively; both p=0.001]. Compared to respondents using medical cannabis for all other health conditions, those using medical cannabis for a self-reported sleep disorder were more likely to be using both prescribed and illicit forms of medical cannabis (26.5% versus 20.2%, p=0.005), inhaled routes of administration (52.4% vs 40.3%, p<0.001), and THC-dominant medical cannabis (32.1% vs 24.7%, p=0.002).
 |
Table 2 Associations Between Respondent Characteristics and Use of Medical Cannabis to Treat a Self-Reported Sleep Disorder |
Figure 2 shows the route of administration and cannabinoid composition for illicit and prescribed medical cannabis products. Prescribed medical cannabis products were consumed predominantly via oral routes (246/361, 68.1%) whereas illicit products were mostly consumed via inhaled routes (585/863, 67.9%; ie, smoking or vaporising). Cannabinoid composition of prescribed medical cannabis products was predominantly “THC/CBD equivalent” (145/364, 39.8%) or “THC-dominant” (109/364, 29.9%) while illicit medical cannabis products were self-reported as largely “THC-dominant” (300/866, 34.6%) or “Unknown” (293/866, 33.8%).
Figure 3 shows that the majority of participants reported an improvement in their subjective sleep symptoms since commencing medical cannabis. A large proportion of respondents also reduced their use of benzodiazepines (391/414, 94.5%) while alcohol intake decreased in 62.5% (321/514), remained unchanged in 37.2% (191/514), and increased in 0.3% (2/514) of respondents (Supplemental Figure S1).
Table 2 shows the results of a binary logistic regression model that assessed the relationship between respondent characteristics and the odds of using medical cannabis to treat a self-reported sleep disorder. Those using illicit medical cannabis products were twice as likely to use medical cannabis to treat a self-reported sleep disorder (OR = 2.04, 95% CI: 1.06–3.92, p=0.032). Concomitant use of medical cannabis for pain (OR = 2.15, 95% CI: 1.49–3.09, p<0.001), mental health and/or substance use disorder (OR = 2.51, 95% CI: 1.78–3.55, p<0.001), and gastrointestinal disorder (OR = 2.30, 95% CI: 1.38–3.85, p=0.001) also significantly increased the odds of also using medical cannabis to treat a self-reported sleep disorder.
Discussion
The present study examined the characteristics and cannabis use patterns among a sample of Australians who were using medical cannabis to treat a self-reported sleep disorder, recruited as part of our larger CAMS-20 survey.9 Results showed just under 65% of respondents who completed the survey were using medical cannabis to treat a self-reported sleep disorder, with insomnia disorder being the most common. Our survey data showed that Australians using medical cannabis for a self-reported sleep disorder were more likely to use a mix of both illicit and prescribed forms of medical cannabis, inhaled forms of administration (ie, smoking or vaping), and THC-dominant products compared to those using medical cannabis for all other health conditions.
These results agree with a recent analysis of medical cannabis prescriptions in Australia where patients with sleep disorders were typically prescribed flower products (ie, consumed via inhalation) and THC-containing products (ie, >2% THC).10 THC is known to increase subjective ratings of feeling “drowsy” or “sleepy/tired” after oral and smoked/vaporised consumption.34,35 Inhalation produces much faster onset and shorter duration of subjective effects with greater bioavailability (2–56%) and higher peak concentrations of THC in blood, all within minutes of exposure.36 This allows individuals to self-titrate to the desired effect with multiple smaller doses that have a rapid effect which may be of benefit to individuals with sleep-onset insomnia. In contrast, oral ingestion produces slower and less predictable onset and longer duration of subjective effects (peak concentration occurring at 2–4 hours),37 compared to inhaled methods. Low bioavailability (4–19%) and inter- and intra-individual variability in absorption of orally ingested cannabis products make dose titration difficult.38 Nonetheless, all recently published and currently ongoing clinical trials exploring the use of cannabinoid treatments for insomnia disorder utilise oral formulations. This is likely due to the ease and discreteness of using orally administered cannabis products,39 and lack of respiratory side effects compared with inhaled methods.40
Our survey found that only 16.8% of respondents selected a self-reported sleep disorder as their main condition suggesting that sleep disorders were commonly being treated secondary to, or in addition to, another health condition such as chronic pain or a mental health disorder. Sleep is often negatively affected in individuals with chronic pain,41,42 and is associated with daytime consequences such as fatigue, poor concentration, and mood disturbance.43,44 In turn, poor sleep is hypothesised to promote pain amplification via its impact on various neurobiological systems influencing nociceptive processing41 and increase the risk of developing depression.45 This may explain the high rate of medical cannabis prescription for sleep disorders in Australia;10 aimed to improve sleep in those with other co-morbid health conditions such as pain or anxiety. Nabiximols (Sativex), a registered oromucosal spray delivering equal parts THC and CBD, has been shown to improve subjective sleep outcomes in individuals with chronic pain disorders (eg, neuropathic pain, spasticity in multiple sclerosis, rheumatoid arthritis).46 THC has been shown to possess sedative,34,35 anti-spasmodic,47 and anti-emetic properties,48 and is characterised by a range of transient behavioural effects including mild euphoria, relaxation, and a sense of detachment which some describe as the ability to “unplug”.49 CBD, on the other hand, has been shown to possess anti-anxiety effects50 which may in turn promote sleep, particularly in those individuals with insomnia disorder who are prone to hypervigilance and/or excessive rumination at sleep onset.51 It is therefore possible that improvements in subjective sleep following cannabis use may be due to improvements in the associated condition (ie, pain). Indeed, prior work suggests that cannabis may be effective in improving overall quality of life by way of its diverse effects on a number of conditions and symptoms such as pain, mood, and sleep.52
Of note, abrupt discontinuation of regular cannabis use may lead to abstinence-induced insomnia53 and sleep disturbance is a commonly reported symptom of cannabis withdrawal among individuals who frequently use cannabis (ie, at least 25 days per month).54–56 Sleep disturbance is also a known risk factor for relapse following a quit attempt in people who are cannabis dependent.57 It is therefore possible that a proportion of respondents were using medical cannabis to treat a self-reported sleep disorder arising from cannabis dependence and withdrawal. An analysis of prevalence and correlates of cannabis use disorder (CUD) in our 2018 survey showed that one-third of people using cannabis for medical purposes met Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5) criteria consistent with CUD.56 Nearly all (98%) had accessed illicit, unregulated sources of medical cannabis. The odds of meeting criteria for CUD increased with inhaled routes (eg, via a joint, bong, pipe, or vaporiser) and use of medical cannabis to treat a mental health disorder. The continued reliance on illicit sources of medical cannabis in the present study does raise some safety concerns. Illicit (unregulated) cannabis products are often of unknown strength, composition and quality posing unpredictable risks to the consumer.58 The CAMS-20 survey findings highlighted some advantages in prescribed over illicit cannabis use including safer routes of administration, access to quality-assured products of known composition, and better communication with, and safety monitoring from, health-care providers.9 Future studies should examine whether the probability of meeting criteria for CUD differs depending on how the medical cannabis product was accessed (ie, prescribed vs illicit), the reasons for use (ie, medical purposes, non-medical purposes, or both) and the presence of comorbid psychopathology.
There were several limitations to this subanalysis. First, CAMS-20 was a cross-sectional survey, which does not permit a reliable inference of causality to be drawn from the data such as whether medical cannabis is a safe or effective treatment for sleep disorders. Second, the use of anonymous, self-report data may be associated with inaccurate information such as incorrect diagnosis and/or misinterpretation of efficacy and side effects which may not be generalisable to those with a clinical diagnosis. Third, convenience sampling in a survey may produce selection bias whereby those who are more likely to report favourable experiences with medical cannabis complete the survey. This may limit the extent to which our results are representative of the broader population of people with sleep disorders. Finally, the CAMS-20 survey was not primarily designed to examine the various determinants of sleep health, and some questions of known contributing factors to sleep health from previous studies (eg, race/ethnicity, seasonal temperature variation) were not included in the questionnaire.
Conclusion
The present study provides a snapshot of medical cannabis use for self-reported sleep disorders among a sample of individuals in Australia at a timepoint four years after the regulatory changes that permitted patient access to legal medical cannabis. These results suggest that self-reported sleep disorders, in particular insomnia disorder, are often being treated secondary to, or in addition to, a comorbid health condition such as a chronic pain, or a mental health disorder. The use of inhaled routes of administration, THC-dominant products, and illicit sources of medical cannabis are common among people with self-reported sleep disorders. As prescribing rates for medical cannabis continue to rise dramatically each year in Australia, it is imperative that randomised, placebo-controlled trials using quality-assured products are conducted to better understand the safety and efficacy of cannabinoid treatment in patients with clinician-diagnosed sleep disorders.
Acknowledgments
This work was supported by the Division of Addiction Medicine, University of Sydney, and the Lambert Initiative for Cannabinoid Therapeutics, a philanthropically funded center at the University of Sydney, Australia. We would like to acknowledge the important contribution of the late Associate Professor David Allsop in the creation of the original CAMS-16 questionnaire, upon which the CAMS-20 questionnaire was based. The authors gratefully acknowledge the contributions of Professor Jonathon Arnold, Dr Melissa Benson, Dr Dilara Bahceci and Rhys Cohen in this work, and the services and forums that distributed information regarding the survey. We would also like to thank the participants who gave their time in completing the survey.
Disclosure
NL has received research funding from Camurus and Indivior for unrelated research. ISM is Academic Director of the Lambert Initiative for Cannabinoid Therapeutics, a philanthropically funded research program at the University of Sydney. He has served as an expert witness in various medicolegal cases involving cannabis and has received consulting fees from Medical Cannabis Industry Australia (MCIA) and Janssen. He currently acts as an advisor/consultant to Kinoxis Therapeutics, Psylo and Emyria. He reports research grants and salary support from the Australian National Health and Medical Research Council (NHMRC) and from Lambert Initiative for Cannabinoid Therapeutics. He is an inventor on patents WO2018107216A1 and WO2017004674A1, licensed to Kinoxis Therapeutics involving use of novel small molecules (non-cannabinoid) to treat addictions and social deficits. ISM also has patents WO2020102857A1 and WO2021042178A1 related to use of small molecules (non-cannabinoid) for treating weight gain and opioid withdrawal, as well as patents WO2019227167 and WO2019071302 issued, which relate to cannabinoid therapeutics. AS and ISM has received consulting fees from the Medical Cannabis Industry Australia (MCIA). TRA has received grants from Swinburne University of Technology and the Victorian Department of Health for projects unrelated to the submitted work. All other authors have no competing financial or non-financial interests to declare.
References
1. Ramar K, Malhotra RK, Carden KA, et al. Sleep is essential to health: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2021;17(10):2115–2119.
2. Liu Y, Wheaton AG, Chapman DP, et al. Prevalence of healthy sleep duration among adults—United States, 2014. Morb Mortal Wkly Rep. 2016;65((6)):137–141.
3. Baglioni C, Altena E, Bjorvatn B, et al. The European Academy for Cognitive Behavioural Therapy for Insomnia: an initiative of the European Insomnia Network to promote implementation and dissemination of treatment. J Sleep Res. 2020;29((2)):e12967.
4. De Crescenzo F, D’Alò GL, Ostinelli EG, et al. Comparative effects of pharmacological interventions for the acute and long-term management of insomnia disorder in adults: a systematic review and network meta-analysis. Lancet. 2022;400(10347):170–184.
5. Bachhuber M, Arnsten JH, Wurm G. Use of cannabis to relieve pain and promote sleep by customers at an adult use dispensary. J Psychoactive Drugs. 2019;51((5)):400–404.
6. Piper BJ, DeKeuster RM, Beals ML, et al. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol. 2017;31((5)):569–575.
7. Lintzeris NDJ, Elias N, Arnold JC, McGregor IS, Allsop DJ. Findings from the Cannabis as Medicine Survey (CAMS-16): an online survey of medical cannabis use in Australia. Med J Aust. 2018;209:211–216.
8. Lintzeris N, Mills L, Suraev A, et al. Medical cannabis use in the Australian community following introduction of legal access: the 2018–2019 online Cross-Sectional Cannabis as Medicine Survey (CAMS-18). Harm Reduct J. 2020;2020:1–12.
9. Lintzeris N, Mills L, Abelev SV, et al. Medical cannabis use in Australia: consumer experiences from the online cannabis as medicine survey 2020 (CAMS-20). Harm Reduct J. 2022;19((1)):1–10.
10. MacPhail S, Bedoya-Perez MA, Cohen R, et al. Medicinal cannabis prescribing in Australia: an analysis of trends over the first five years. Front Pharmacol. 2022;13:1368.
11. Cahill SP, Lunn SE, Diaz P, et al. Evaluation of patient reported safety and efficacy of cannabis from a survey of medical cannabis patients in Canada. Front Public Health. 2021;9:1.
12. Suraev AS, Marshall NS, Vandrey R, et al. Cannabinoid therapies in the management of sleep disorders: a systematic review of preclinical and clinical studies. Sleep Med Rev. 2020;53:101339.
13. AminiLari M, Wang L, Neumark S, et al. Medical cannabis and cannabinoids for impaired sleep: a systematic review and meta-analysis of randomized clinical trials. Sleep. 2022;45(2):zsab234.
14. Walsh JH, Maddison KJ, Rankin T, et al. Treating insomnia symptoms with medicinal cannabis: a randomized, crossover trial of the efficacy of a cannabinoid medicine compared with placebo. Sleep. 2021;44(11):zsab149.
15. Australian New Zealand Clinical Trials Registry. A phase IIb double-blind, randomised placebo-controlled clinical trial to evaluate the efficacy and safety of a botanical cannabidiol (CBD) for sleep disturbances in a healthy population. ACTRN12621000632897. Sydney (NSW): NHMRC Clinical Trials Centre, University of Sydney (Australia). Available from: https://www.australianclinicaltrials.gov.au/anzctr/trial/ACTRN12621000632897.
16. National Institutes of Health Clinical Center. The Cannabidiol use for relief of short term insomnia (CANREST). NCT05253417. National Institutes of Health; 2022. Available from: ClinicalTrials.gov.
17. Australian New Zealand Clinical Trials Registry. Cannabidiol (CBD) treatment for insomnia. ACTRN12620000070932. Sydney (NSW): NHMRC Clinical Trials Centre, University of Sydney (Australia). Available from: https://www.australianclinicaltrials.gov.au/anzctr/trial/ACTRN12620000070932.
18. National Institutes of Health Clinical Center. Evaluation of an oral cannabidiol (CBD)-terpene formulation on sleep physiology in participants with insomnia. NCT05233761. National Institutes of Health; 2022. Available from: ClinicalTrials.gov.
19. Australian New Zealand Clinical Trials Registry. A single-dose, double-blind, placebocontrolled, randomised, crossover study of an oral cannabis-based medicine (ETC120) on sleep, cognition, and next-day function in adults with chronic insomnia disorder. ACTRN12619000714189. Sydney (NSW): NHMRC Clinical Trials Centre, University of Sydney; 2020.
20. Calik MW, Carley DW. Intracerebroventricular injections of dronabinol, a cannabinoid receptor agonist, does not attenuate serotonin-induced apnea in Sprague-Dawley rats. J Negat Res Biomed. 2016;15:1–7.
21. Calik MW, Carley DW. Cannabinoid type 1 and type 2 receptor antagonists prevent attenuation of serotonin-induced reflex apneas by dronabinol in Sprague-Dawley rats. PLoS One. 2014;9(10):e111412.
22. Calik MW, Carley DW. Effects of cannabinoid agonists and antagonists on sleep and breathing in Sprague-Dawley rats. Sleep. 2017;40:9.
23. Carley DW, Pavlovic S, Janelidze M, et al. Functional role for cannabinoids in respiratory stability during sleep. Sleep. 2002;25(4):388–395.
24. Carley DW, Prasad B, Reid KJ, et al. Pharmacotherapy of apnea by cannabimimetic enhancement, the PACE clinical trial: effects of dronabinol in obstructive sleep apnea. Sleep. 2018;41:1.
25. Prasad B, Radulovacki MG, Carley DW. Proof of concept trial of dronabinol in obstructive sleep apnea. Front Psychiatry. 2013;4:1.
26. Australian New Zealand Clinical Trials Registry. Proof of concept study on the combined effect of dronabinol and Acetazolamide on apnoea hypopnoea index (AHI) in adults with obstructive sleep apnoea. ACTRN12620000916943. Sydney (NSW): NHMRC Clinical Trials Centre, University of Sydney (Australia). Available from: https://www.australianclinicaltrials.gov.au/anzctr/trial/ACTRN12620000916943.
27. Megelin R, Ghorayeb I. Cannabis for restless legs syndrome: a report of six patients. Sleep Med. 2017;36:182e83.
28. Ghorayeb I. More evidence of cannabis efficacy in restless legs syndrome. Sleep Breath. 2020;24(1):277–279.
29. Lavender I, McGregor IS, Suraev A, et al. Cannabinoids, insomnia, and other sleep disorders. CHEST. 2022;162(2):452–465.
30. Arnold JC, Nation T, McGregor IS. Prescribing medicinal cannabis. Aust Prescr. 2020;43(5):152.
31. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
32. Hurst H, Bolton J. Assessing the clinical significance of change scores recorded on subjective outcome measures. J Manipulative Physiol Ther. 2004;27((1)):26–35.
33. Beasley TM, Schumacker RE. Multiple regression approach to analyzing contingency tables: post hoc and planned comparison procedures. J Exp Educ. 1995;64(1):79–93.
34. Spindle TR, Martin EL, Grabenauer M, et al. Assessment of cognitive and psychomotor impairment, subjective effects, and blood THC concentrations following acute administration of oral and vaporized cannabis. J Psychopharmacol. 2021;35(7):786–803.
35. Spindle TR, Cone EJ, Schlienz NJ, et al. Acute effects of smoked and vaporized cannabis in healthy adults who infrequently use cannabis: a crossover trial. JAMA Netw Open. 2018;1(7):e184841–e41.
36. Huestis MA. Human cannabinoid pharmacokinetics. Chem Biodivers. 2007;4(8):1770.
37. Schlienz NJ, Spindle TR, Cone EJ, et al. Pharmacodynamic dose effects of oral cannabis ingestion in healthy adults who infrequently use cannabis. Drug Alcohol Depend. 2020;211:107969.
38. Perucca E, Bialer M. Critical aspects affecting cannabidiol oral bioavailability and metabolic elimination, and related clinical implications. CNS Drugs. 2020;34(8):795–800.
39. MacCallum CA, Russo EB. Practical considerations in medical cannabis administration and dosing. Eur J Intern Med. 2018;49:12–19.
40. Ghasemiesfe M, Ravi D, Vali M, et al. Marijuana use, respiratory symptoms, and pulmonary function: a systematic review and meta-analysis. Ann Intern Med. 2018;169(2):106–115.
41. Haack M, Simpson N, Sethna N, et al. Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology. 2020;45(1):205–216.
42. Freeman D, Sheaves B, Waite F, et al. Sleep disturbance and psychiatric disorders. Lancet Psychiat. 2020;7(7):628–637.
43. Bjorvatn B, Jernelöv S, Pallesen S. Insomnia–a heterogenic disorder often comorbid with psychological and somatic disorders and diseases: a narrative review with focus on diagnostic and treatment challenges. Front Psychol. 2021;289:1.
44. Husak AJ, Bair MJ. Chronic pain and sleep disturbances: a pragmatic review of their relationships, comorbidities, and treatments. Pain Med. 2020;21(6):1142–1152.
45. Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2022;10(4):473–481.
46. Russo EB, Guy GW, Robson PJ. Cannabis, pain, and sleep: lessons from therapeutic clinical trials of Sativex®, a cannabis‐based medicine. Chem Biodivers. 2007;4(8):1729–1743.
47. Meyer T, Funke A, Münch C, et al. Real world experience of patients with amyotrophic lateral sclerosis (ALS) in the treatment of spasticity using tetrahydrocannabinol: cannabidiol (THC: CBD). BMC Neurol. 2019;19:1–13.
48. Grimison P, Mersiades A, Kirby A, et al. Oral THC: CBD cannabis extract for refractory chemotherapy-induced nausea and vomiting: a randomised, placebo-controlled, Phase II crossover trial. Ann Oncol. 2020;31(11):1553–1560.
49. Osborne GB, Fogel C. Understanding the motivations for recreational marijuana use among adult Canadians. Subst Use Misuse. 2008;43(3–4):539–572.
50. Blessing EM, Steenkamp MM, Manzanares J, et al. Cannabidiol as a potential treatment for anxiety disorders. Neurotherapeutics. 2015;12(4):825–836.
51. Carney CE, Harris AL, Falco A, et al. The relation between insomnia symptoms, mood, and rumination about insomnia symptoms. J Clin Sleep Med. 2013;9(6):567–575.
52. Lucas P, Boyd S, Milloy M-J, et al. Cannabis significantly reduces the use of prescription opioids and improves quality of life in authorized patients: results of a large prospective study. Pain Med. 2021;22(3):727–739.
53. Gates PJ, Albertella L, Copeland J. The effects of cannabinoid administration on sleep: a systematic review of human studies. Sleep Med Rev. 2014;18(6):477–487.
54. Allsop D, Norberg MM, Copeland J, et al. The cannabis withdrawal scale development: patterns and predictors of cannabis withdrawal and distress. Drug Alcohol Depend. 2011;119:123–129.
55. Vandrey R, Smith MT, McCann UD, et al. Sleep disturbance and the effects of extended-release zolpidem during cannabis withdrawal. Drug Alcohol Depend. 2011;117(1):38–44.
56. Mills L, Lintzeris N, O’Malley M, et al. Prevalence and correlates of cannabis use disorder among Australians using cannabis products to treat a medical condition. Drug Alcohol Rev. 2022;41(5):1095–1108.
57. Babson KA, Boden MT, Harris AH, et al. Poor sleep quality as a risk factor for lapse following a cannabis quit attempt. J Subst Abuse Treat. 2013;44(4):438–443.
58. Suraev A, Benson MJ, Martin L, et al. Determination of contaminants in artisanal cannabis products used for childhood epilepsy in the Australian community: a sub-analysis of the ‘PELICAN’ study. Epilepsy Behav. 2022;127:108496.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.