Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Levels of Peripheral Circulating IL-6 and IL-10 Decrease Over Time Despite High Depression Burden in PTSD Patients
Authors Toft H , Bramness JG, Lien L
Received 25 January 2022
Accepted for publication 24 March 2022
Published 5 April 2022 Volume 2022:18 Pages 737—747
DOI https://doi.org/10.2147/NDT.S357797
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Helge Toft,1,2 Jørgen G Bramness,1,3,4 Lars Lien1,2
1Norwegian National Advisory Unit on Concurrent Substance Abuse and Mental Health Disorders, Innlandet Hospital Trust, Brumunddal, Norway; 2Faculty of Social and Health Sciences, Inland Norway University of Applied Sciences, Elverum, Norway; 3Department of Alcohol, Tobacco and Drugs, Norwegian Institute of Public Health, Oslo, Norway; 4Department of Clinical Medicine, UiT The Arctic University of Norway, Tromsø, Norway
Correspondence: Helge Toft, Norwegian National Advisory Unit on Concurrent Substance Abuse and Mental Health Disorders, Innlandet Hospital Trust, P.O. Box 104, Brumunddal, 2381, Norway, Email [email protected]
Background: Patients with combined depression symptoms and post-traumatic stress disorder (PTSD) often exhibit high levels of circulating inflammatory biomarkers as either a cause or consequence of their disease. We aimed to investigate how cytokines and depression symptoms develop with one-year follow-up and compare them with non-PTSD patients.
Methods: The study had a longitudinal design with one-year follow-up measurements in an inpatient treatment setting at a psychiatric center in Norway. PTSD diagnoses were set using the Mini International Neuropsychiatric Interview (MINI). The first three measurements were at baseline (T0), halfway (T1) and at discharge (T2) from a 12-week main stay, followed by a final measurement one year after discharge (T3). Serum blood samples were collected on all four occasions. The Beck Depression Inventory-II (BDI-II) was administered at T0, T2 and T3.
Results: Levels of interleukin-6 (IL-6) and interleukin-10 (IL-10) in PTSD patients were higher than in patients without PTSD at T0 (p = 0.005 and 0.042). The PTSD patients had a higher average level of IL-10 across all four measurements (B = 1.62, Standard Error (SE) = 0.78, p = 0.037). The IL-10 levels in PTSD patients declined from T0 to T3 (p = 0.039). The PTSD patients were more depressed than non-PTSD patients at T3 (p = 0.019).
Conclusions: The levels of IL-10 and IL-6 in PTSD patients more closely resembled the levels in non-PTSD patients at one-year follow-up, despite level of depression being unchanged in the PTSD patients. This calls into question the close relationship between level of circulating cytokines and depressive symptoms, at least in PTSD patients. Further research is needed to investigate what appears to be a complex relationship between immune markers and depression in patients with PTSD.
Keywords: PTSD, cytokines, inflammation, depression, longitudinal
Introduction
Post-traumatic stress disorder (PTSD) may develop following exposure to exceptionally traumatic events,1 such as war, Abuse, rape, injuries, or natural disasters.2 PTSD is characterized by re-experiencing or having vivid dreams of the stressor, avoidance of circumstances associated with it, inability to recall parts of the traumatic event, and increased psychological sensitivity.3 Although PTSD has a rather low prevalence rate, ranging from 1.1 to 2.9% in Europe,4 the societal costs and disability burden of PTSD are considered to be high.5 Patients with PTSD exhibit a low-grade pro-inflammatory state with altered levels of neuroimmune markers such as cortisol, c-reactive protein (CRP)6–9 and pro- and anti-inflammatory cytokines like interleukin-6 (IL-6) and interleukin-10 (IL-10).10–12
Depressive disorder is a leading cause of disability worldwide with 4.4% of the global population affected in 2015.13 Dysregulation of inflammatory processes is known to be associated with depressive disorder,14 and it is established that inflammatory processes influence both the development and progression of the disease.15,16 These inflammatory processes include increased levels of peripheral cytokines like interleukin-1 (IL-1), IL-6 and tumor necrosis factor-α (TNF-α).14,17,18 It is unclear exactly how cytokines induce or drive depression, but one hypothesis is that cytokines stimulate synthesis of enzyme indoleamine 2,3-dioxygenase (IDO) in brain microglia, resulting in an overall decrease in serotonin and an increase in glutamatergic activity.16
Depression co-occurs in around 60% of PTSD patients. Patients with co-morbid PTSD and depression often have higher Mental and physical Healthcare utilization and a more chronic progression than patients with PTSD only.19 Hypothalamic-pituitary-adrenal (HPA) axis hyperactivity might be a shared pathway20 of PTSD21 and depression.22 The pro- and anti-inflammatory cytokine IL-623 and the anti-inflammatory cytokine IL-10 are associated with both PTSD and depressive disorder.24–27
Co-occurring PTSD and depression are two highly debilitating conditions that result in reduced life quality and poorer health than either disorder alone.19,28 To the best of our knowledge, there are no longitudinal studies assessing the development of inflammatory markers and depression symptoms in PTSD inpatients with long follow-up. The vast majority of previous studies on inflammation, PTSD and depression are cross-sectional,9,29 thus not providing sufficient insight into whether levels increase or decrease over time. We aimed to assess whether PTSD patients with depression symptoms would exhibit a more profound pro-inflammatory profile over time than patients with anxiety, eating and depression disorders, and to consider this in light of self-reported depression symptoms.
Materials and Methods
Study Participants
The patient sample consisted of a mixed-diagnosis group of inpatients in treatment at Modum Bad Psychiatric Center, a specialized treatment center in Vikersund, Norway. The center has a 12-week treatment program for individuals and groups. The staff at Modum Bad is multidisciplinary and consists of psychiatrists, nurses, psychologists, pastoral staff, art therapists and occupational therapists. The center offers treatment to patients with long-standing or treatment-resistant depression, anxiety and eating disorders, in addition to those who have been exposed to psychological trauma. The treatment involves various disorder-specific methods, such as cognitive therapy, metacognitive therapy, and traditional psychotherapy. The use of psychotropic medication is reduced to a minimum while in treatment. Some patients did use NSAIDs, anti-viral drugs and immune suppressants. The use of medication was recorded by searching each patient’s medical record. Patients who are referred to Modum Bad have tried treatment elsewhere but failed to achieve remission. The center does not offer treatment to patients who have a substance abuse disorder, are psychotic, or in an active suicidal state. Being eligible for treatment at the center was the only inclusion criterion for participation in the study. Thus, all patients admitted to treatment from March 2015 until April 2016 were invited to participate in the study. Groups of eight participants were given a 15-minute oral presentation of the study by the first author on one of the first days of their main stay. The procedures were explained, and an information brochure was handed out together with the consent form. Participants returned the signed consent form within a day or two. The patient sample consisted of those who attended both the 12-week main treatment stay and the one-week follow-up stay one year after discharge from the center. Of the 147 participants attending the main stay, 57 did not attend the follow-up stay, giving a total of 90 patients (61%) in the study. Data collection commenced in 2015 and lasted for about a year. The patients who returned for a one-week stay one year after discharge re-submitted their blood samples and filled out the BDI-II questionnaire one final time.
On average, the patients who returned for the follow-up stay were away from Modum Bad for 14.5 months. Of these patients, there were 66 females (73%, mean age 38, SD 10.3) and 24 males (27%, mean age 48, SD 8.4). Fifty-seven patients were lost to follow-up, 39 of whom were females (68%, mean age 41, SD 13.3) while 18 were males (32%, mean age 48, SD 10.9). The study was approved by the Norwegian Regional Ethics Committee (REK) prior to data collection (reference number 2014/2189).
Missing Data and Undetectable Values
Two cytokines had a somewhat high proportion of the measured values (> 52%) under the lower limit of detection (LLOD) at T0. Others have also included cytokines where up to 75% of the measurements were below the LLOD.30 The average values below the LLOD, measured across four time points, were 43% for IL-6 and 50% for IL-10. There were seven (2% of 353 submitted blood samples) missing values for IL-6, and five (1.4% of 355 submitted blood samples) missing values for IL-10 across all four time points due to patients not attending blood sampling. Further, 154 values for IL-6 and 178 values for IL-10 were under the LLOD and set to zero. In sensitivity analysis (Supplementary Table S1), the zero values were replaced with the LLOD and with 1% of the mean value of each cytokine to display how these different approaches would affect the results. These two imputation methods have been used in previous publications.31,32 The following values are the LLODs (given in pg/mL): At T0, the LLOD was 0.01 for IL-6 and 0.03 for IL-10. At T1, the LLOD was 0.03 for IL-6 and 0.03 for IL-10. At T2, the LLOD was 0.03 for IL-6 and 0.02 for IL-10. At T3, the LLOD was 0.01 for both IL-6 and IL-10. Eleven patients had one missing value in the BDI-II and one patient had two missing values. There were nine patients with a missing diagnosis.
Measures
All patients were interviewed by trained psychologists or psychiatrists using the MINI.33 The MINI assesses diagnoses from the 10th revision of the International Classification of Diseases and Related Health Problems (ICD-10). All disorders were in the areas of depression, anxiety, and eating disorders. There were 23 patients with mood disorders (F30-F39), 39 with anxiety disorders (F40-F48), and 19 with eating disorders (F50). Three patients had comorbid PTSD and a mood disorder, three patients had PTSD and an eating disorder, and 27 patients with PTSD were diagnosed with another anxiety disorder in the F40-F48 spectrum. In the non-PTSD group, there were 20 with mood disorders, 12 with anxiety disorders, and 16 with eating disorders.
The Norwegian validated version of the BDI-II questionnaire was used to assess depression symptom severity34,35 and administered by the therapists. The questionnaire is designed to assess depression severity during the two weeks prior to the interview. The 21 items in the questionnaire are scored from 0 to 3, where a higher score means worse depression. A total score is computed from the 21 items, and the scores are further classified into four categories: Minimal and mild depression (score from 0 to 13), mild depression (14–19), moderate depression (20–28), and severe depression (29–63). The BDI-II questionnaires were submitted within one week of entering treatment (T0), a few days before discharge (T2), and at the one-year follow-up (T3). Although most of the PTSD patients were not diagnosed with current depressive disorder, their mean BDI-II scores at each time point were high and in the spectrum of moderate to severe depression.
Blood Collection and Serum Preparation
The serum samples were collected at four time points. These were a few days after admission to the main stay (T0), at the halfway point (T1), upon discharge (T2), and at the one-week follow-up stay one year after discharge (T3). The samples were drawn between 8 and 9 am. Sixteen patients on the depression ward submitted their blood samples between noon and 3 pm. The serum samples were collected in 8 mL Vacuette containers. The containers were rotated 8–10 times after the blood collection procedure was completed. They were at rest for 30–60 minutes in order to let the blood clot successfully. The samples were spun in a centrifuge, at room temperature, reaching 1917 g for 10 minutes. Upon completion, the samples were stored at −80°C until assay.
The blood samples were thawed on ice, vortexed, and then spun down a tube with 250 μL serum at 14,000 g for 10 min at 4°C, before dilution (1:5) and further processing. The cytokines were measured with Bio-Plex xMAP Technology (Bio-Rad, Austin, TX, USA) using a Luminex IS 100 instrument (Bio-Rad, Hercules, CA, USA). The Luminex IS 100 was powered by the Bio-Plex Manager (version 6.0.1) software. An additional standard point was added to the manufacturer’s instructions when the assay was performed.
Individual sets of samples from patients were run in the same assay in order to achieve a more reliable result. The samples were assayed in duplicate, and a magnetic plate washer was used during set up. The StatLIA software package (version 3.2; Brendan Scientific, Carlsbad, CA, USA) incorporates a weighted, five-parameter logistic curve-fitting method and was used to calculate serum cytokine levels. For the purpose of this study we analyzed IL-6 and IL-10. These biomarkers were chosen since they have frequently been assessed in previous immunopsychiatric studies, thus allowing for comparisons with the available literature. Longitudinal controls were used to validate inter-assay variation: IL-6 (16%) and IL-10 (5.7%). The mean inter-assay percentage coefficient of variability for all blood sample plates was 10.4%. The unit of measurement was picograms per milliliter (pg/mL).
Statistics
The Mann–Whitney U-Test and Pearson’s chi-square test were used for bivariate analysis of baseline (T0) data and the Wilcoxon matched-pairs signed-rank test for bivariate analysis of BDI-II scores within groups. The Kruskal–Wallis equality of populations test for equal ranks was used for a variable comprising three groups. Multilevel models were utilized to assess the continuous longitudinal dependent cytokine variables.36 Multilevel models incorporated all four measurements from T0 to T3, using all available data. Hence, a patient with missing data at one time point will still be included and contribute to an estimation based on available data from other time points. The use of multilevel models constituted a two-level structure of blood samples at level one, nested within patients at level two. In this way, the dependency of measurements within patients was handled. Maximum likelihood was used for parameter estimation as this approach is recommended for small samples (below 100) and less than 70% missing data, thus providing a reliable solution for handling missing data.37 The covariance was set to unstructured. The longitudinal cytokine variables were skewed (skewness 6.52 for IL-6 and 8.41 for IL-10), and robust standard errors were applied to account for the non-normal distribution.38 The multilevel models were tested with random intercept variation and random slope to assess the best model fit. Likelihood ratio tests revealed that a more complex model, including both random intercept variation and random slope, provided a better fit for IL-6 and IL-10 (χ2(2) = 342.97, p = <0.001 and χ2(2) = 583.05, p = <0.001, respectively). This indicated that allowing patients´ cytokine levels to vary at T0, as well as varying across time, gave the best fit. In contrast, for BDI-II, a model with random intercept variation only provided a better fit than the more complex model with random slope (χ2(2) = 0.55, p = 0.760). Q-Q plots and scatter plots of the predicted residuals of the cytokine variables were constructed to determine whether there were any outliers which violated assumptions of normal residual distribution. Three patients were identified as violating that assumption, and the models were tested without those individuals. This exclusion did not alter any p-values to any great extent. Hence, they were kept in the analysis presented. The alpha level was set at 0.05 for statistical significance, and all tests were two-tailed, but trends (p<0.10) were also reported. All statistical analyses were conducted with Stata (StataCorp. 2019, Stata Statistical Software: Release 16, College Station, TX, USA: StataCorp LLC).
Results
Table 1 shows the proportions of detectable cytokines at T0-T3, categorized across PTSD diagnosis. The detection rate of IL-6 was higher for PTSD patients at T0 (p = 0.001), T1 (p = 0.013) and T2 (p = 0.008). In addition, the detection rate of IL-10 was higher for PTSD patients at T1 (p = 0.030) and T2 (p = 0.035). At the final observation after one year, there were no differences between PTSD patients and non-PTSD patients in cytokine detection levels.
 |
Table 1 Proportions of Detectable Cytokines at Main Treatment Stay and One-Year Follow-Up Categorized by PTSD |
Table 2 presents the mean levels of IL-6, IL-10, and BDI-II at baseline. The patients aged 30 and above had higher levels of IL-6 than those under 30 years (p = 0.040). PTSD patients had higher levels of IL-6 (p = 0.005) and IL-10 (p = 0.042). Patients with childhood trauma had higher levels of IL-10 (p = 0.006).
 |
Table 2 Cytokine Levels by Patient Characteristics at Baseline |
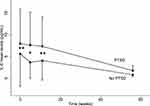
Table 3 shows results of statistical tests that are visualized in Figure 1. There was a significant main effect of PTSD on anti-inflammatory cytokine IL-10 (B = 1.62, SE = 0.78, p = 0.037), indicating that PTSD patients had higher levels of IL-10 on average across the four measurements. Furthermore, there were several trends to be observed in the data. There was a trend toward a higher level of IL-6 in the PTSD patients (B = 1.20, SE = 0.70, p = 0.086). There was also a trend effect of PTSD on BDI-II (B = 4.01, SE = 2.17, p = 0.057).
 |
Table 3 Multilevel Models with Main Effects and Interaction with Time for the Cytokines and BDI-II as Dependent Variables |
Figure 1 shows that IL-6 levels were higher in PTSD patients compared to non-PTSD patients at T0 (p = 0.005), T1 (p = 0.031) and T2 (p = 0.005), but not at T3. Figure 2 shows that the IL-10 levels were higher in PTSD patients at the same time points (p = 0.042, 0.011 and 0.004, respectively). The PTSD patients exhibited reduced IL-10 levels from T0 to T3 (Wilcoxon signed rank test; p = 0.039). Figure 3 shows that patients without PTSD had a reduced BDI score from T0 to T3 (p < 0.001). PTSD patients had more depressive symptoms than non-PTSD patients at T3 (p = 0.019).
Supplementary Tables
There were 15 patients who used anti-inflammatory drugs. Seven of these were non-PTSD patients, while eight were diagnosed with PTSD. We stratified the patients on the use of these drugs, and ran the mixed models analysis with the stratification. The stratified results are added as Supplementary Tables S2 and S3. Supplementary Table S2 shows that there were no significant main effects or interactions with time. Supplementary Table S3 shows that PTSD patients who used these drugs had a higher average level of IL-6 during the period than non-PTSD patients who did not use the drugs (B = 1.74, SE = 0.70, p = 0.014). Further, IL-10 levels in patients with PTSD declined across time (B = −0.11, SE = 0.05, p = 0.024).
Discussion
In this study, patients with PTSD had higher average levels of the anti-inflammatory cytokine IL-10. IL-10 levels in PTSD patients decreased over the one-year period. There was also a trend that the initial higher levels of IL-6 in the PTSD patients almost fell to the levels in non-PTSD patients during the observation period. At the same time, there was a trend that the PTSD patients were more depressed when all four measurements were assessed longitudinally and remained more depressed at one-year follow-up. The trajectories of IL-10, IL-6 and BDI-II did not formally interact with time in the multilevel analysis, but the figures show that the trajectories of IL-10 and IL-6 in PTSD patients meet at T3, suggesting an interaction effect with time after all.
Chronic depression is more often found in patients with PTSD.39 PTSD may act as a factor sustaining depression, reducing the prospects of remission, previously suggested to be driven by the underlying inflammatory processes with a high subjective feeling of stress.40 Furthermore, having PTSD with co-occurring depression disorder is associated with greater likelihood of current suicidal ideation and lifetime suicide attempts compared to those with PTSD alone,28 underscoring that these patients are worse off as a result of the comorbidity. This burden of co-morbidity is reflected at the inflammatory level, as seen in a study with a small sample size showing that IL-6 levels in PTSD patients both with and without depressive disorder were significantly reduced following administration of hydrocortisone, but IL-6 levels were still higher in patients with both PTSD and depressive disorder than in those with PTSD alone.1 This highlights the complexity of the psychoneuroimmunological interface in the comorbidity of PTSD and depression and might be either a contributing factor or a symptom of the high depression burden. PTSD and depressive disorder are characterized as disorders of inflammation and hypothalamic-pituitary-adrenal axis dysfunction.41 However, depressed patients both with and without PTSD are known to have high inflammatory levels.42,43 It is difficult to draw conclusions from the present data as to whether the high levels of IL-6 and IL-10 in the PTSD patients are caused by a depressive trait, or if the traumatic experiences themselves are the origin.
A review by Kim et al reported that elevated levels of IL-10 in PTSD patients have been shown in previous studies; however, other studies have reported IL-10 to be reduced in these patients.44 The authors suggested that this biomarker might not be suitable to provide insight into the pathophysiology of PTSD. However, both elevated and reduced levels of IL-10 are in line with the current study, as IL-10 was elevated at the main stay and reduced at the follow-up. We believe that this contradiction only underscores the necessity of measuring cytokines over a long period, as such biomarkers will develop differently over time depending on numerous factors.
The reduced cytokine levels at follow-up could be due to a variety of factors. Patients in inpatient settings usually experience improved sleep quality as a result of following a daily structure with fixed schedules, as well as eating regular and nutritious meals. Well-regulated sleeping and eating patterns have previously been reported to reduce inflammation in psychiatric patients.45,46 It is still uncertain whether therapy in itself reduces inflammation, as there are few robust studies on this topic to date, and our research group has previously found no associations between therapy and cytokines.47 However, one systematic review on cognitive behavioral therapy and inflammation found at least one inflammatory marker to be reduced in 14 out of 23 studies.48 Further, the review found three papers which reported that high pre-treatment inflammatory levels predicted poorer outcome from cognitive behavioral therapy. These findings may explain why cytokine levels were reduced, but with a different trajectory in individuals with PTSD.
The depressive symptoms in PTSD patients did not significantly decrease one year after admission to the main treatment stay. This might be typical of patients with comorbid PTSD and depression; they are difficult to treat and are in need of new and better treatment alternatives.
There are limitations to this study that need to be mentioned. It must be taken into consideration that we do not know if the patients received other kinds of treatment during the one-year follow-up period, or if they used any kind of medication that could have affected the inflammatory levels. Further, the blood samples at the main stay and at follow-up were analyzed in two separate batches. The use of different equipment for analysis suggests that the blood sample results could be biased and might not be directly comparable. Further, some patients had eaten breakfast before blood samples were collected, while others were fasting, which might have affected cytokine production.49 We did not record whether patients had been smoking or exercising prior to blood sampling. Smoking and exercise are known to affect cytokine levels.50,51 In addition, their body mass index was not recorded and adipose tissue is known to produce inflammatory cytokines.52 All patients who failed to submit complete measures of BDI-II were among those who did not attend the one-year follow-up. This may have represented a selection bias, as patients who did not participate in the follow-up stay might have had poorer mental health than those who were present at follow-up. This study also has strengths that should be pointed out. This study is the first to include four measurement points in a sample of depressed PTSD patients, where the final measurement point is at one-year follow-up. This approach provides a new perspective on the development of inflammatory levels and psychometric scores over a long follow-up period.
Ethical Statement
The authors state that all procedures in this study complied with the World Medical Association Declaration of Helsinki.
Acknowledgments
We wish to thank the staff and patients at Modum Bad Psychiatric Center for their cooperation. We would also like to thank Innlandet Hospital Trust, Health Region South-East, Norway, for funding the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gill J, Luckenbaugh D, Charney D, Vythilingam M. Sustained elevation of serum interleukin-6 and relative insensitivity to hydrocortisone differentiates posttraumatic stress disorder with and without depression. Biol Psychiatry. 2010;68(11):999–1006. doi:10.1016/j.biopsych.2010.07.033
2. Ralevski E, Olivera-Figueroa LA, Petrakis I. PTSD and comorbid AUD: a review of pharmacological and alternative treatment options. Subst Abuse Rehabil. 2014;5:25–36. doi:10.2147/sar.S37399
3. World Health Organization. International classification of diseases and related health problems, 10th revision. World Health Organization; 2016.
4. Bothe T, Jacob J, Kröger C, Walker J. How expensive are post-traumatic stress disorders? Estimating incremental health care and economic costs on anonymised claims data. Eur J Health Econ. 2020;21(6):917–930. doi:10.1007/s10198-020-01184-x
5. Atwoli L, Stein DJ, Koenen KC, McLaughlin KA. Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Curr Opin Psychiatry. 2015;28(4):307–311. doi:10.1097/yco.0000000000000167
6. Furtado M, Katzman MA. Neuroinflammatory pathways in anxiety, posttraumatic stress, and obsessive compulsive disorders. Psychiatry Res. 2015;229(12):37–48. doi:10.1016/j.psychres.2015.05.036
7. Wang K, Bao JP, Yang S, et al. A cohort study comparing the serum levels of pro- or anti-inflammatory cytokines in patients with lumbar radicular pain and healthy subjects. Eur Spine J. 2016;25(5):1428–1434. doi:10.1007/s00586-015-4349-4
8. Wieck A, Grassi-Oliveira R, Do Prado CH, et al. Neuroimmunoendocrine interactions in post-traumatic stress disorder: focus on long-term implications of childhood maltreatment. Neuroimmunomodulation. 2014;21(2–3):145–151. doi:10.1159/000356552
9. Passos IC, Vasconcelos-Moreno MP, Costa LG, et al. Inflammatory markers in post-traumatic stress disorder: a systematic review, meta-analysis, and meta-regression. Lancet Psychiatry. 2015;2(11):1002–1012. doi:10.1016/S2215-0366(15)00309-0
10. Gola H, Engler H, Sommershof A, et al. Posttraumatic stress disorder is associated with an enhanced spontaneous production of pro-inflammatory cytokines by peripheral blood mononuclear cells. BMC Psychiatry. 2013;13(1):1. doi:10.1186/1471-244X-13-40
11. Guo M, Liu T, Guo J-C, Jiang X-L, Chen F, Gao Y-S. Study on serum cytokine levels in posttraumatic stress disorder patients. Asian Pac J Trop Med. 2012;5(4):323–325. doi:10.1016/S1995-7645(12)60048-0
12. von Känel R, Hepp U, Kraemer B, et al. Evidence for low-grade systemic proinflammatory activity in patients with posttraumatic stress disorder. J Psychiatr Res. 2007;41(9):744–752. doi:10.1016/j.jpsychires.2006.06.009
13. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO.
14. Wohleb ES, Franklin T, Iwata M, Duman RS. Integrating neuroimmune systems in the neurobiology of depression. Nat Rev Neurosci. 2016;17(8):497–511. doi:10.1038/nrn.2016.69
15. Gilman SE, Trinh NH, Smoller JW, Fava M, Murphy JM, Breslau J. Psychosocial stressors and the prognosis of major depression: a test of axis IV. Psychol Med. 2013;43(2):303–316. doi:10.1017/s0033291712001080
16. Young JJ, Bruno D, Pomara N. A review of the relationship between proinflammatory cytokines and major depressive disorder. J Affect Disord. 2014;169:15–20. doi:10.1016/j.jad.2014.07.032
17. Liu Y, Ho RC-M, Mak A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J Affect Disord. 2012;139(3):230–239. doi:10.1016/j.jad.2011.08.003
18. Smith RS. The macrophage theory of depression. Med Hypotheses. 1991;35(4):298–306. doi:10.1016/0306-9877(91)90272-Z
19. Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J Trauma Stress. 2013;26(3):299–309. doi:10.1002/jts.21814
20. Baker DG, Nievergelt CM, O’Connor DT. Biomarkers of PTSD: neuropeptides and immune signaling. Neuropharmacology. 2012;62(2):663–673. doi:10.1016/j.neuropharm.2011.02.027
21. Yehuda R. Biology of posttraumatic stress disorder. J Clin Psychiatry. 2001;62(Suppl 17):41–46.
22. Pariante CM. Why are depressed patients inflamed? A reflection on 20 years of research on depression, glucocorticoid resistance and inflammation. Eur Neuropsychopharmacol. 2017;27(6):554–559. doi:10.1016/j.euroneuro.2017.04.001
23. Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813(5):878–888. doi:10.1016/j.bbamcr.2011.01.034
24. Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-alpha. Mol Psychiatry. 2016;21(5):642–649. doi:10.1038/mp.2015.67
25. Baune BT. Are non-steroidal anti-inflammatory drugs clinically suitable for the treatment of symptoms in depression-associated inflammation? Curr Top Behav Neurosci. 2017;31:303–319. doi:10.1007/7854_2016_19
26. Beurel E, Lowell JA. Th17 cells in depression. Brain Behav Immun. 2018;69:28–34. doi:10.1016/j.bbi.2017.08.001
27. Wang Z, Caughron B, Young MRI. Posttraumatic stress disorder: an immunological disorder? Front Psychiatry. 2017;8:222. doi:10.3389/fpsyt.2017.00222
28. Nichter B, Norman S, Haller M, Pietrzak RH. Psychological burden of PTSD, depression, and their comorbidity in the U.S. veteran population: suicidality, functioning, and service utilization. J Affect Disord. 2019;256:633–640. doi:10.1016/j.jad.2019.06.072
29. Sumner JA, Nishimi KM, Koenen KC, Roberts AL, Kubzansky LD. Posttraumatic stress disorder and inflammation: untangling issues of bidirectionality. Biol Psychiatry. 2020;87(10):885–897. doi:10.1016/j.biopsych.2019.11.005
30. Korolkova OY, Myers JN, Pellom ST, Wang L, M’Koma AE. Characterization of serum cytokine profile in predominantly colonic inflammatory bowel disease to delineate ulcerative and Crohn’s colitides. Clin Med Insights Gastroenterol. 2015;8:29–44. doi:10.4137/CGast.S20612
31. Toft H, Bramness JG, Lien L, et al. PTSD patients show increasing cytokine levels during treatment despite reduced psychological distress. Neuropsychiatr Dis Treat. 2018;14:2367–2378. doi:10.2147/NDT.S173659
32. Toft H, Lien L, Neupane SP, et al. Cytokine concentrations are related to level of mental distress in inpatients not using anti-inflammatory drugs. Acta Neuropsychiatr. 2020;32(1):23–31. doi:10.1017/neu.2019.36
33. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):
34. Beck AT, Steer RA, Brown GK. The Beck Depression Inventory (BDI-II). In: Manual.
35. Sigveland J, Kornør H. Måleegenskaper ved den norske versjonen av Beck Depression Inventory 2. utgave (BDI 2) [The psychometric properties of the Norwegian version of the Beck Depression Inventory-II (BDI-II)]. PsykTestBarn. 2011;1(5):53.
36. Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata, Volume I: Continuous Responses.
37. Jain RB, Wang RY. Limitations of maximum likelihood estimation procedures when a majority of the observations are below the limit of detection. Anal Chem. 2008;80(12):4767–4772. doi:10.1021/ac8003743
38. Chou CP, Bentler PM, Satorra A. Scaled test statistics and robust standard errors for non-normal data in covariance structure analysis: a Monte Carlo study. Br J Math Stat Psychol. 1991;44(Pt 2):347–357. doi:10.1111/j.2044-8317.1991.tb00966.x
39. Kostaras P, Bergiannaki J-D, Psarros C, Ploumbidis D, Papageorgiou C. Posttraumatic stress disorder in outpatients with depression: still a missed diagnosis. J Trauma Dissociation. 2017;18(2):233–247. doi:10.1080/15299732.2016.1237402
40. Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11(1):200. doi:10.1186/1741-7015-11-200
41. Oglodek EA, Just MJ. The association between inflammatory markers (iNOS, HO-1, IL-33, MIP-1beta) and depression with and without posttraumatic stress disorder. Pharmacol Rep. 2018;70(6):1065–1072. doi:10.1016/j.pharep.2018.06.001
42. Raedler T. Inflammatory Mechanisms in Major Depressive Disorder. Philadelphia: Lippincott Williams & Wilkins; 2011.
43. Mazza MG, De Lorenzo R, Conte C, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594–600. doi:10.1016/j.bbi.2020.07.037
44. Kim TD, Lee S, Yoon S. Inflammation in post-traumatic stress disorder (PTSD): a review of potential correlates of PTSD with a neurological perspective. Antioxidants. 2020;9(2). doi:10.3390/antiox9020107
45. Krysta K, Krzystanek M, Bratek A, Krupka-Matuszczyk I. Sleep and inflammatory markers in different psychiatric disorders. J Neural Transm. 2017;124(Suppl 1):179–186. doi:10.1007/s00702-015-1492-3
46. Guinter MA, Campbell PT, Patel AV, McCullough ML. Irregularity in breakfast consumption and daily meal timing patterns in association with body weight status and inflammation. Br J Nutr. 2019;122(10):1192–1200. doi:10.1017/s0007114519002125
47. Johnson SU, Hoffart A, Tilden T, et al. Circulating cytokine levels in the treatment of comorbid anxiety disorders. Acta Neuropsychiatr. 2020:1–7. doi:10.1017/neu.2020.38
48. Lopresti AL. Cognitive behaviour therapy and inflammation: a systematic review of its relationship and the potential implications for the treatment of depression. Aust N Z J Psychiatry. 2017;51(6):565–582. doi:10.1177/0004867417701996
49. Dixit VD, Yang H, Sayeed KS, et al. Controlled meal frequency without caloric restriction alters peripheral blood mononuclear cell cytokine production. J Inflamm. 2011;8(1):1. doi:10.1186/1476-9255-8-6
50. Belchamber K, Hall DA, Hourani SM, Benarafa C. Smoking enhances the proinflammatory effects of nucleotides on cytokine release from human lung. PLoS One. 2014;9(6):e99711. doi:10.1371/journal.pone.0099711
51. Mee-Inta O, Zhao ZW, Kuo YM. Physical exercise inhibits inflammation and microglial activation. Cells. 2019;8(7):691. doi:10.3390/cells8070691
52. Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021;320(3):C375–c391. doi:10.1152/ajpcell.00379.2020
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.