Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Laboratory Test Utilization Practices in Hamad Medical Corporation; Role of Laboratory Supervisors and Clinicians in Improper Test Utilization; a Descriptive Pilot Study
Authors Alshekhabobakr HM, AlSaqatri SO , Rizk NM
Received 31 May 2021
Accepted for publication 7 January 2022
Published 3 March 2022 Volume 2022:15 Pages 413—429
DOI https://doi.org/10.2147/JMDH.S320545
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Hafsa Mohammed Alshekhabobakr,1 Salim O AlSaqatri,2 Nasser Moustafa Rizk1,3
1Biomedical Sciences Department, College of Health Sciences, QU Health, Qatar University, Doha, Qatar; 2Community College of Qatar, Doha, Qatar; 3Biomedical Research Center (BRC), Qatar University, Doha, Qatar
Correspondence: Nasser Moustafa Rizk, Biomedical Sciences Department, College of Health Sciences, QU Health, Qatar University, Doha, Qatar, Email [email protected]
Background: The use of diagnostic laboratory tests is increasing worldwide. Improper test utilization (ITU) is a common problem for all healthcare systems as it costs substantial expenses for the health systems and impacts optimal patient care.
Purpose: The present small-scale survey aims to highlight the current practice of ITU among the labs and physicians, and investigate the actions of diagnostic laboratories towards ITU, and identify the reasons affecting test ordering decisions among physicians.
Methods: A cross sectional study based on two different surveys was developed and distributed from March 2017 to April 2017 to laboratory supervisors and physicians (clinicians) at Hamad Medical Corporation (HMC), Qatar. Fourteen laboratory supervisors and eighty-nine physicians were surveyed about improper test utilization practices. The overall results are descriptive data.
Results: The overall proportion of improperly utilized tests detected by the laboratory supervisors were 50.0%, 35.7%, and 14.3% for overused, misused, and underused lab tests, respectively. Among the physicians, 91% used the electronic ordering template to select the appropriate tests. Moreover, 78.7% of the physicians used the clinical guidelines, while 73% were not employing the laboratory handbook. Furthermore, 95.5%% of the physicians preferred to get feedback about inappropriate tests, while 51.1% were not receiving any, and 40.9% were rarely receiving. Finally, 67.4% were unaware of the tests’ costs among surveyed physicians, and 63.6% showed a willingness to reduce their orders if the cost was high and unnecessary.
Conclusion: The physician’s and the laboratories’ communication were inadequate and not systematized, causing ITU practices. The improvement strategy should focus on the communication between clinical labs and physicians and enhance physician implementation to order appropriate lab tests. This could be achieved by conducting legitimate educational methodologies, continuous feedback reviews, ongoing audits, executing health information technology instruments, engaging laboratory practice guidelines, and applying demand management and testing algorithms.
Keywords: improper laboratory test utilization, laboratory supervisors, physicians (clinicians), surveys, Qatar, descriptive study
Introduction
Providing high-quality care while minimizing expenditures is essential for healthcare organizations.1 For instance, healthcare industry costs in the USA were reported to be around $2.5 trillion per year, and laboratory testing expenditures constitute 4% of these costs (around $60 billion).2 Pathology and laboratory costs were reported to increase by 20–25% each year,2 and the return on investment of these costs is lower compared to past years.1 On the contrary, a recent publication documented that the effect of diagnostic analysis on a healthcare financial statement is lesser than 2.5%, though its cost-effectiveness is over 100%, a net income margin more than 7-times greater than whatever another human business.3
For health care organizations to deliver optimum patient care, laboratory procedures should be precise and cost-effective, starting from the test selection criteria provided in the laboratory handbook. Unfortunately, physicians face an enormous pile of tests to choose from, which results in ordering too many tests and the possibility of delayed or wrong diagnosis.4
Expenses and outcomes of improper lab test utilization (ILTU) are the key indicators that show the requirement of investigating and boosting healthcare management. Precise test selection for the right patient and prevention of unnecessary sample collection and testing is essential.5 Although many tools are available to control test utilization when placing an order,6,7 there are no constraints in ordering a test repeatedly and raising the incidence of unrequired tests.7,8 As many tests invade the markets, countless tests are being overused every day, and this imposes a robust system to prevent such improper practice.1,2 The common term for such a comprehensive system is Test Utilization Management and can be defined as “an assembly to reduce costs and improve healthcare through encompassing a wide range of tools and approaches to correct the consumption of laboratory tests”.2 Furthermore, due to the impact of the COVID-19 crisis on the health care system in terms of cost, supply chain, and quality, the present study could increase the awareness of the cost of over-testing and lead to a better understanding of the factors that result in improper test utilization.
To the authors’ knowledge, no studies are reporting on Qatar’s test utilization practices, despite evidence that the problem of inappropriate practices occurs as reported elsewhere.9,10 Hamad General Hospital (HMC) was endorsed in 1982, and it has achieved an international reputation as a teaching and referral hospital. It is accredited by the American Hospital Association and offers medical and surgical sub-specialties to more than 2 million people. Therefore, laboratory supervisors and physicians at Hamad Medical Corporation (HMC) were surveyed about the test utilization practice in this study. The Department of Laboratory Medicine and Pathology (DLMP) at HMC is certified by The College of American Pathologists (CAP) accreditation. The DLMP accomplished over 20 million lab tests in 2019, offering a broad range of dedicated laboratory facilities for the people in Qatar. The present small-scale survey of this study aims to emphasize the current practice of ITU among the lab supervisors and physicians, and investigate the actions of diagnostic laboratories towards ITU, and identify the reasons affecting test ordering decisions among physicians. The study’s outcomes should help overall process improvement and establish a future background for a more specific investigation of test utilization practice, and it could be used as a pilot study for further work in such a field.
Materials and Methods
Participants
A cross sectional study based on two different surveys was developed and distributed from March 2017 to April 2017 to laboratory supervisors of DLMP and physicians at HMC, Qatar. The total number of participants was 103, composed of 14 laboratory supervisors and 89 physicians. The surveys were conducted via the internet anonymously and were conducted to ask about improper test utilization and lab utilization test practices at HMC. In addition, one interview was conducted with the HMC laboratory supervisors and the other with the physicians to execute the study properly. Ethical approval had been received for this study from Hamad Medical Corporation Research Center for Review in compliance with the deceleration of Helsinki.
Materials and Procedures
Two different anonymous surveys were sent by email to the laboratory supervisors and physicians. Each of the surveys required 10 to 15 minutes for completion. Complete voluntary participation was stated in the survey introduction as consent, and anyone taking the survey had the chance to quit at any time during the survey and accepted to publish his response as part of the current data after analysis.
Survey questions were extracted from research articles and reviews, and the editorial board approved them of HMC Research Center. The survey questions had been extracted from research articles and reviews and revised by the study team as previously published10–13 The survey for the laboratory supervisors was organized into areas of interest such as demographic, laboratory role, test utilization malpractices, and impact of improper test utilization on clinical lab performance. The survey for the physicians and specialists was categorized into specific areas as demographic, current use of software and properties, available information sources, inquiries, assessments and involvement of others, test outcomes and results, the cost of testing, and other factors involved in the ordering of the lab tests.
Both surveys were developed as online surveys using Blue Survey Software (Explorance Inc., Canada) provided by Qatar University. The link was submitted anonymously, and IP-logging was inhibited. A brief lecture was given to the laboratory supervisors to highlight the importance of the study, and the laboratory supervisors’ survey was circulated by the Department of Laboratory Medicine and Pathology at HMC. In addition, two reminders were sent to encourage doing the survey. Finally, the physicians’ survey was sent individually to the physicians through the heads of the medical departments. The surveying process started from March 2017 to April 2017 to gain the maximum response count. The following definitions were used in the study:
Overuse occurs when a service is provided even though its risk of harm exceeds its likely benefit—when it is not warranted on medical grounds. Underuse: while some services are overused, others do not get provided even though they would have been medically beneficial. Misuse: a term that includes incorrect diagnoses as well as medical errors and other sources of avoidable complications.9
The surveys questions were included in the tables in the results section and in Supplementary Figure S1.
Statistical Analysis
The data were collected, coded, and entered the computer for analysis. The comprehensive data of the present study are mainly descriptive. Data were presented as numbers and percentages of frequency. Regression analysis was used to investigate the factors that impact IUT on lab practice among LS and the ordering behavior among physicians. The impact of IUT on lab practice (dependent variable), while increased cost, inventory, turnaround time, hire more staff, are the independent factors.
Furthermore, the order behavior of physicians (dependent variable) and factors affecting it such as ease of ordering, peer pressure, fear of litigation, impatience vs a desire for certainty of diagnosis, financial incentives, patient demand, part of management, and follow-up plan as independent variables. The regression analysis and graphs were performed using GraphPad Prism 9 for Windows, GraphPad Software, San Diego, California USA, www.graphpad.com. The data entry and analysis were performed using Excel 2016 program for data presentation (Microsoft Corporation, USA) (2016).
Results
Fourteen supervisors and eighty nine physicians (clinicians) were surveyed throughout the study. The details and the results of the surveys conducted are given in the following sections.
Laboratory Supervisors
1-Demographic data of lab supervisors (Figure 1)
This data aims to elucidate the educational background and experience of the lab supervisors who participated in the present study. The data is presented in Figure 1.
2-Current practice of lab supervisors (Table 1)
 |
Table 1 Response of Lab Supervisors to Questions About Test Utilization |
The next part of the survey highlights the importance of improper test utilization in the current practice. Assessing the role of LS in evaluating the improper test utilization is presented in (Table 1). Of note, LS can recognize the test utilization areas that can be improved is (92.9%); furthermore, (78.6%) responded that it is easy of detecting incorrect lab test utilization (LTU), and (57.1%) responded that they keep track of incorrect LTU in their labs, as shown in (Table 1). However, when we asked the LS about providing feedback to physicians about their request for incorrect test utilization practices, the responses were almost equivocal (35.7%). Further investigation about the answer of “sometimes,” LS claimed that their reasons were for patient management, as the physicians were not responding most of the time and even ordering the same test for other patients and physicians know about the clinical condition of their patients. The role of the LS towards LTU demonstrated that (71.4%) of LS did not conduct audits regarding test utilization practices.
Furthermore, (42.9%) of LS indicated the presence of a system to correct improper test utilization (ITU) practices to follow. A laboratory handbook is an essential tool to communicate with physicians. The handbook contains the test specifications and explains how to order the tests. In this survey, 12 supervisors (85.7%) indicated an online handbook was available and were up to date (Table 1).
3-Test utilization malpractices (Table 2, and Supplementary Tables S1 and S2)
Following, we assessed the most common types of improper lab tests; LS responded that most laboratory services are being overused (50%), followed by misused (35.7%), then underused (14.3%) tests (Table S1). Moreover, to gain in-depth about overused, misused, and underused observed per month in the last 12 months, the supervisors who responded by yes were asked about the range of such tests, which is shown in Table 2), which indicates more than six tests per month is observed per month in the last 12 month.
Furthermore, we asked LS, who answered yes for overused, misused, and underused improper LTU, to give examples of such test orders. As shown in (Supplementary Table S2), most of the overused tests are related to virology lab tests, such as Hepatitis B, C, and Delta, Hepatitis B eAg and Hepatitis Delta, Epstein-Barr virus (EBV), HIV PCR, and Varicella-zoster virus (VZV), then followed by the immunological tests and others as shown in Supplementary Table S2. Among the misused tests are the Hepatitis B and C, and HCV, Beta, and Alpha-thalassemia genotyping and FISH Test (Fluorescence In Situ Hybridization), which map the genetic material. FISH Test is commonly done on breast cancer tissue. Of exciting note, some lab tests are observed in both overused and misused tests such as Chromosomal Microarray and HIV PCR. The underutilized reported tests were Flu, dengue, and molecular diagnostic tests. The results are given in Supplementary Table S2.
4-Actions of LS in response to lab test utilization malpractices (Table 3).
 |
Table 2 Numbers of Lab Test Utilization Malpractices Detected by a Lab. Supervisors (%) and Role of Labs Towards Malpractice |
 |
Table 3 Actions of a Lab. Supervisors in Response to Lab Test Utilization Malpractices (%) |
To assess the actions of LS in different labs towards lab test utilization malpractice by physicians, we evaluated the responses, as shown in Table 3. The question allows the responses by LS to select one answer or more. Among the 14 participants, there were 21 responses, and the top-ranking action was to call the requested physician (47.6%), while in the bottom ranking was to report that the test is not indicated (4.8%).
5-Effect of improper test utilization on lab process (Figure 2)
When the effect of the incorrect utilization practices on the lab processes was questioned, the following independent factors (cost, inventory, turnaround time, more staff are needed) were imposing the impact on lab performance. Among LS, (29.7%) reported increasing the cost. The other main effects reported were bad inventory management (24.3%), increasing the turnaround time (21.6%), and the ultimate need for more stuff (18.9%) (Figure 2). The analysis demonstrated a significant impact of improper test utilization on the lab process (dependent factor), p= 0.015.
- Physicians (clinicians)
1-Demographics data (Figure 3)
The current data was questioned to demonstrate the experience of the physicians (including GP and specialists) who participated in the survey, as shown in Figure 3.
2-Current practice
The following parts of the surveys questioned the current practice, including several aspects about software use, available sources, assistance for ordering lab tests, feedback about ITU, and factors impacted in lab test orders.
A-Current software and its properties (Table 4)
 |
Table 4 Use of Software by Physicians |
To identify the causes behind improper test utilization practices, the physicians had been asked about different aspects of the current ordering system. Since the current software Cerner is being used as the main ordering tool, the main concern is the redundant test ordering. Cerner’s electronic ordering templates are the primary tool used by physicians (90.9%) to order lab tests. Of note, (58.4%) of the participants reported not being alerted about the redundant tests being ordered. On the other hand, more than three-quarters of physicians (76.4%) like the previous test result to be shown as a warning for a redundant test.
Moreover, 41.6% of physicians express their feeling as being alert-fatigued when ordering tests electronically. Further questions about possible reasons for feeling as being alert-fatigued, the answer in ranking is alerts are irrelevant (25.8%), followed by no time to check alerts (22.5%), then alerts are not convincing (18.0%). Furthermore, 83.3% of physicians prefer to be interruptive alerts for most important cases.
Sixty-four physicians (71.9%) reported that Cerner’s display of test results could affect them. Sixty-three of the physicians (70.8%) accepted with the help of the corollary order notifications “consequent electronic orders for laboratory tests that are required because of other orders.” Moreover, 88.0% of the physicians settled on the help of the reflex testing protocols, “electronic protocols allowing additional tests to be ordered depending on the initial test results” (Table 4).
B-Available information sources (Table 5)
 |
Table 5 The Available Information and Obscure Diagnosis by Physicians |
The second part that influences test utilization practices is the available information. These questions aim to find the essential sources of information when physicians order lab tests and minimize inappropriate test utilization. The responses by physicians about the availability of clinical practice guidelines are (78.4%) who reported that they used it in their ordering, while (7.5%) of them reported that such guidelines were not helpful. Further, we investigated if there are enough resources that help to choose the appropriate tests, and half of the physicians responded positively, while 32.6% were not sure (Table 5).
To improve the result interpretations and influence future test selection, the physicians had been asked if pathologist interpretation accompanies test results are useful; 55 (61.8%) affirm the usefulness of such interpretations. In comparison, 31 of them (34.8%) reported that they were sometimes useful, and (3.4%) reported them as not useful (Table 6B). Another vital source of information is the Laboratory Handbook (Laboratory practice guidelines book). Astonishingly, 65 (73.0%) of the participating physicians indicated not using the handbook. This information highlighted that the lab handbook should be evaluated and frequently updated to be useful for physicians.
 |
Table 6 The Inquiries, Assessments, and Involvement of Others- Physicians |
Moreover, the Positive Predictive Value (PPV), the Negative Predictive Value (NPV), Clinical Utility (CU), and the overall accuracy of the test are of great importance before ordering any test in clinical-based evidence diagnosis. The results demonstrated that one-third of physicians (33%) reported that they were considering it as a source, while half of them (52.8%) reported when it was needed (Table 5). Furthermore, when the diagnosis is obscure, 27 (30.3%) of the physicians prefer to order tests in parallel, while 41 (46.6%) prefer to order in sequence, but 21 (23.9%) stated that their ordering pattern would depend on the suspected diagnosis (Table 5).
C-The inquiries, assessments, and involvement of others (Table 6)
People surrounding the physicians can affect their decisions or even take the lead in certain situations. The physicians reported that sometimes (58%) are asking colleagues about the proper test, while (11.4%) reported as often, and (30.7%) of them reported as rarely (Table 6). In addition, 85 (95.5%) of the participants welcome the idea of receiving feedback regarding improper test ordering behavior from the laboratory. However, the number of physicians favoring feedback is reduced to 65 (73.0%) when asked if they prefer the division’s chair to share the feedback (Table 6). Moreover, most participants (51.7%) surprisingly reported that they had not been contacted regarding ITU, and 40.9% reported that they were rarely contacted, while (8%) reported being contacted frequently. When it was asked who contacted the physicians, (56.2%) responded as not applicable, while (28.1%) were contacted by laboratory staff, (6.7%) by laboratory consultants, and (3.4%) by laboratory managers (Table 6). Finally, the physicians were asked if they would favor a consultant in the field to be the single individual allowed to order esoteric tests; (63.6%) agreed, while (36.4%) disagreed (Table 6).
D-Test orders, outcomes, and results (Table 6).
All physicians (100%) reported that they consider the benefit of test outcome with the treatment plans before ordering. Among physicians, (97.7%) reported that they also consider the time required to obtain results and the degree to which an abnormal test value could affect their diagnosis (Table 6).
E-Test cost (Table 7)
As shown in Table 7, (67.4%) reported that they were not aware of the financial cost per each test, while 29 of them (33%) reported that they were aware (Table 7). Furthermore, when asked about the impact of high-cost tests, (63.3%) reported that they would reduce their ordering (Table 7). On the other hand, when participants were asked about the impact of low-cost tests, (70.5%) replied that it would not affect their ordering, while (19.3%) reported increased ordering and (10.2%) reported decreased ordering (Table 7).
 |
Table 7 Effect of Cost and Other Factors That Influence Orders by Physicians |
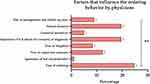
F- Other factors (Figure 4).
As shown in (Figure 4 and Table 7), among the 178 responses obtained for the factors affecting ordering behavior, (44 responses, 24.7%) highlighted the ease of ordering, (35 responses, 19.7%) for impatience vs. a desire for certainty of diagnosis, and (35 responses, 19.7%) for patient demand. On the other hand, the others reported the effect of peer or supervisor pressure (22 responses, 12.4%), fear of litigation (15 responses, 8.4%), financial incentives (9 responses, 5.1%), ignorance of test characteristics (2 responses, 1.1%), and part of management and follow up plan (16 response, 9.0%), and such factors significantly affect the ordering, p=0.003 (Figure 4).
Discussion
The present study is one of the first surveys performed in Qatar about Test Utilization Management. The results of the current context of improper lab test utilization are based on the opinions of both lab supervisors and physicians. Therefore, we utilized two surveys, one for laboratory supervisors and the other for physicians (clinicians), to explore the areas that may require enhancements, improve lab utilization practice, and decrease healthcare costs. The positive perceptions of this study demonstrated that both LS and physicians are surging to minimize the ITU and improve ordering systems for the sake of patient care outcome and cost of the health care system. Furthermore, good laboratory management practices are crucial components that significantly impact laboratory processes. Therefore, both groups of LS and physicians have a significant role in improving the lab utilization practice.14
Effective administration of laboratory test utilization necessitates the laboratory unit, including LS, making use of their competencies and acquaintance to recognize utilization subjects, to carry out a program that will accomplish more functional testing, and establish proper processes of the test phase to minimize the ITU practice.15 Laboratory supervisors were surveyed, and most of LS were aware of test utilization areas that could be improved, and many of them could easily identify incorrect test utilization (Table 1). However, as a reply to the actions taken by LS regarding the improper practices, more than half of the responses indicated to keep tracking on such improper tests, but the communication with the physicians was not adequate about ITU practice. For example, 35.7% of LS just called the requested physicians, but only 28.6% audited such incorrect utilization practices, and less than half of the supervisors (42.9%) used a systematic approach to correct test utilization improper practices. Such data reflect ineffective communication between labs and physicians and require close collaboration and cooperation between labs and physicians, as previously published.14
Studies of tests and medical situations indicate that inappropriate laboratory testing is a significant challenge throughout medicine.16 The current survey among LS showed that test utilization’s main concern was the overused tests (50.0%) as shown in Supplementary Table S1, which parallel previous studies.13,17 For instance, the present study demonstrated that the HbA1c test was being overused. Similarly, two studies by Trivelli et al18 and Lyon et al19 revealed that unnecessarily repeated measurements evidenced HbA1c test overutilization within 10 and 30 days, respectively. Another example of test overuse presented by this study was the vitamin D test,20 and as an inappropriate test,21 showing that test is more than 100% for vitamin D testing in many laboratories.
The second group is the misused tests with a percentage of 35.7%. One of the tests being misused is thalassemia genotyping. Dickerson et al, stated that genetic testing was the most expensive and misused test.22 Ultimately, the underused tests scored a percentage of 14.3 in the current study. One participant indicated that underused tests were molecular tests that fit the patient’s clinical condition. One study by Levy et al showed that BRCA1/2 tests for high-risk breast cancer patients were underused in the USA.23 Further studies are required for different types of inappropriate use since one of the participants stated that there were too many to be counted (Supplementary Data). In addition, a previous study demonstrated an increase in the possibility for diagnostic mistakes when these overused and underused tests for bleeding and thrombosis give false-positive or false-negative outcomes for these patients.24
The data obtained in the present survey shows that the core apprehension of test utilization is increasing the laboratory cost due to overused tests, similar to the case in the USA.25 Most of the supervisors stated a significant impact on their labs as the cost’s effect is substantially increased, as it required hiring more staff and resulted in dreadful inventory management and impacts the patient diagnosis, treatment, and follow-up delay due to prolonged turnaround time. In addition, previous studies demonstrated that overutilization leads to substantial costs on labs,26 and inappropriate tests increase the costs and diagnostic errors.27
In short, the survey of LS demonstrated they have the knowledge about areas of ITU which need improvement and its impact on lab performance and cost, but the central point of concern is the effective way to communicate with physicians to improve the lab test practice to be more effective.
The second part of the study aimed to identify the physicians’ behavior in ordering laboratory tests. Physicians (clinicians) represent a crucial potential switch to enhance the use of laboratory testing and reduce inappropriate utilization and its associated costs.28 The demographic data of the participated physicians reflects outstanding experience in the medical field that could impact lab test utilization practice. This is evident as the demographic data is based on their ages, specialty, and duration of clinical work. Several previous studies demonstrated the impact of the practice, skills, experience, and knowledge of the physician in test order for the sake of patient outcome,29–34 Unfortunately, the actual number of lab tests they ordered could not be obtained through the current survey. Therefore, it would be advantageous if the Information System Department at HMC tracked the physicians’ ordering patterns, numbers and ensured that they followed the clinical practice guidelines.
Alerting physicians about unnecessary tests pre-ordering, displaying previous test results, or ordering guidelines were shown to reduce the tests ordered significantly.4,35–37 Cerner is software that physicians are applying to request laboratory services in HMC. The survey among physicians demonstrated that Cerner is helpful as it displays the results correctly (72%), and the electronic template helps to choose appropriate tests (91%), but unfortunately, 59% of the physicians were not warned about Cerner’s unnecessary tests. Meanwhile, 76% preferred to get alerted with previous results before ordering a redundant test. So far, 48% of physicians were not alert-fatigued when ordering tests electronically and expressed that the reasons are irrelevant alerts and no time to check due to the workload by the physicians, and they preferred such alert to be interruptive as previously published.38,39 A previous study revealed that clinicians receive 56 alerts per day and consume 49 min per day in handling them, creating them an essential component of daily care workflows.40 Previous studies showed decreased inappropriate utilization practices when using corollary orders notification, well-designed test templates, and reflex testing protocols.41 Overall, the present survey among physicians at HMC found Cerner’s features valuable to select the proper lab test as previously reported.41–43
Most physicians obviously cannot be anticipated to stay up to date with each complicated test and diagnostic algorithm. The lack of updated information with the heavy workload of physicians in a clinical setting may lead many of them to order many tests, some of which are unneeded or fail to order the proper test leading to a delayed or incorrect diagnosis, putting patients at risk or harmful regarding medical care.44 Therefore, the information accessible to physicians can potentially influence their practices. Therefore, investigating the possible sources of information in the current study revealed important data. Half of the physicians reported that enough resources are available to choose the proper test to order. The available information sources for clinicians in the current survey highlighted that Clinical Practice Guidelines (CPG) are the primary source of information while the laboratory handbook is the least source of information that physicians could use. CPG is used to standardize physicians’ practice effectively and reduce inappropriate test orders. The present study results demonstrated that 70.0% of the physicians used CPG as the primary source to get the correct information. However, a physician requires more updates and other resources of information.
For example, pathologist interpretations provided proof for improvement in future test selection.41,45,46 The present study showed that 61.7% of the physicians consider such interpretations valuable, but on the other hand, the physicians who stated sometimes suggested that these interpretations were inconsistent and ambiguous. Furthermore, the Laboratory Handbook is an enriched laboratory source of information by which clinical laboratories must be communicating with physicians as effective search tools. However, despite the lab supervisors’ efforts to update and maintain their handbooks, the survey showed that 73% of the physicians were not using them, and 9.1% considered them useless. This data refers to ineffective communication between labs and physicians to minimize ITU practice, and this subject requires organizing a meeting regularly to declare any issue about laboratory service and organization. Other important considerations as the source of information for clinicians to order any lab test are PPV, NPV, CU, and test accuracy. Most physicians (52.8%) were calculating them in their minds when required, while 32.6% were giving attention to such parameters as previously published.13
A common approach to diagnose a new patient with vague complaints, like vertigo, is ordering tests in sequence (one after the other) or parallel (simultaneously). The survey indicated 46.6%of physicians prefer to order a test in sequence than in parallel (29.5%). However, this ordered approach may impact diagnosis correctly in time and increase costs.47
The physicians’ decisions are likewise influenced by others’ requests, assessments, and involvement, such as peer opinion, feedback from the labs, and help from the chair department. For example, if peers are not accessible, practitioners had demonstrated to order additional tests, while peer review and audits had demonstrated to reduce the test warrants.48–50 The current study showed that physicians mostly trusted to ask colleagues about the proper test to order.
Several studies22,51,52 reported the significance of feedback in reducing test utilization. Most physicians (95.5%) preferred getting feedback about their improper test orders. The feedback is crucial as it affords a good chance for the laboratory to help physicians order the proper test and guide them to use the laboratory handbook. On the other hand, the physicians’ percentage of welcoming the laboratory’s feedback is lowered by nearly a quarter once asked if they preferred the feedback from their chair of the division, even if it was unidentified. The work ecosystem should be welcoming constructive feedback, either positive or negative, and use it to benefit both the hospital and the physicians. Otherwise, destructive consequences could lead to inappropriate workplace behavior, stress, and feedback avoidance.53 For example, a previous study proposed restricting the search terms for esoteric tests in the computerized supplier order entry to reduce inappropriate test orders by the physician’s,41 which parallel the data of the current survey where many surveyed physicians (63.6%) agreed to such a recommendation.
Physicians order lab tests to diagnose, manage, or follow-up their patients as commonly known. Therefore, it is necessary to plan how the results, whether regular, abnormal, or ambiguous, obtained from the laboratory would be used.13 In this study, the clinicians considered the time and the test outcome elements a high priority when ordering a lab test. Favorably, all the physicians were considering the results before test ordering. Moreover, the time to get a result must be considered in clinical decision-making, especially when dealing with critically ill patients.13,54 Furthermore, selecting the proper test order may affect the cost. For example, a previous study employing selective test orders for trauma patients was estimated to result in significant cost savings of over $1.5 million per year.55
Several studies showed that awareness of testing costs would reduce orders,7,56,57 while one of the most extensive randomized trials carried out in this field showed no significant effect.55 The results obtained in this study discovered that a significant portion of the surveyed physicians (67%) was not concerned about the cost of testing. Appreciatively, more than half of the surveyed physicians (63.3%) said that they would cut test orderings if the cost were high; instead, 70.8% stated that the low-cost test would not affect their ordering practice.
Other factors that might drive physicians to order unnecessary tests were reported to be adherence to firm protocols, fear of uncertainty, defensive medicine, etc.58 In this study, the key four elements which significantly affect the behavior order aims to order lab tests were ease of ordering (25%), the inpatient vs desire for certainty of diagnosis (20%), patient demand (19%), and peer pressure (12%). Furthermore, they reported that even getting abnormal lab results affects the diagnosis.
The assessment of the clinician’s role in improper test utilization highlighted some issues which need more attention, such as lab results being significant in diagnosis and follow-up of the patients. Therefore, the physicians are looking for support and continuous education to enhance their lab test orders and minimize inappropriate test utilization practices.There are many practical approaches to enhance laboratory utilization practice that include education, peer review and feedback, administrative changes, rationing, financial penalties or rewards, laboratory utilization committees, laboratory test formulary, hard stops, and approval systems, gatekeeping, and demand management strategy [Cadamuro et al, 2019].1,13,59 The demand management strategy is a new tool, which means decreasing the cost of unnecessary lab tests, which could reach up to 25% (Fryer & Smellie, 2013).60 The demand management has many recommendations; for example, it focuses on an inappropriate request; that should not be administered, thus avoiding the wrong request to be performed.
Limitations
This study has several limitations. First, the number of laboratory supervisors was low since the available number of HMC supervisors was limited. Secondly, one of the nurses was taken out of the laboratory supervisors’ survey, and one laboratory technologist was taken out of the physicians’ survey. A third limitation was that it would be more accurate to know the physicians’ software’s ordering pattern. Unfortunately, this information could not be obtained due to confidentiality issues and HMC restricted rules. Finally, the two surveys were not validated before distributing to the participants, but they were only extracted from published research articles and reviews.
Conclusion
The present study revealed several factors that result in the inappropriate test utilization practice operated by the two most crucial health care players: laboratory supervisors and medical doctors. First, the physician’s and the laboratories’ communication were inadequate and not systematized, causing ITU practices. The improvement strategy should focus on the communication between clinical labs and physicians and enhance physician implementation to order appropriate lab tests. Laboratory supervisors expect proper exercise and guidance from HMC to establish a robust system to overcome improper test utilization practices. This system should include regular feedbacks and audits and develop user-friendly handbooks. On the other hand, physicians practice can be improved through customizing the software to give timely alerts and notifications, limiting search terms, better communications with frequent feedbacks, reading laboratories handbooks, better continuous education courses, constructive feedback from peers and senior physicians, increased awareness of the cost testing, and understanding and overcoming other factors that may result in improper test utilization.
Prospective
This study has provided some suggestions about protocols or systems that may help laboratories and physicians to eliminate unnecessary testing safely and effectively with the required administrative support. Test utilization inspections must be performed regularly in each laboratory to find specific solutions and improvement strategies. In addition, HMC should apply the demand management strategy. Considering Qatar’s Vision 2030, HMC should take good initiatives and specific measures to improve health care while reducing expenses.
Acknowledgments
The authors would like to thank Hamad Medical Corporation, Qatar University Department of Biomedical Sciences, and the College of Health Sciences for supporting this study. Special thanks to Dr. Nisreen H. Alshaibi for her support in the survey setup from HMC, Dr. Muna A. Al-Maslamani, Dr. Mahmoud A. Naasse, and Dr. Jalal Bhuiyan for their technical support and guidance.
The study is categorized under quality management IRB, approved by the Institutional Review Board (HMC research center) of Hamad Medical Corporation (#MRC0184/2017). Dr. Rizk (corresponding author) and Ms. Hafsa (first primary author, during her work at HMC labs) are included in the study approval by HMC. In addition, Dr. Nesrin from HMC is acknowledged for help and support in the study.
This study was extracted from the master thesis of Mr. Alshekhabobakr titled “Test Utilization Practices in Hamad Medical Corporation: laboratories and clinicians” presented in September 2017, supervised by Dr. Nasser Rizk. The thesis is presented as a text on Qspace of Qatar University website: https://qspace.qu.edu.qa/handle/10576/11345.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Snozek C, Kaleta E, Hernandez JS. Management structure: establishing a laboratory utilization program and tools for utilization management. Clin Chim Acta. 2014;427:118–122. doi:10.1016/j.cca.2013.09.026
2. Riley SB. Trends in laboratory utilization. Clin Microbiol Newsl. 2017;39(9):69–73. doi:10.1016/j.clinmicnews.2017.04.001
3. Lippi G, Plebani M. Cost, profitability and value of laboratory diagnostics: in god we trust, all others bring data. J Lab Med. 2019;43(1):1–3. doi:10.1515/labmed-2018-0321
4. Baron JM, Dighe AS. Computerized provider order entry in the clinical laboratory. J Pathol Inform. 2011;2:35. doi:10.4103/2153-3539.83740
5. Ng VL. Utilization management in the core laboratory. Clin Chim Acta. 2014;427:154–157. doi:10.1016/j.cca.2013.09.038
6. Jackson BR, Krasowski MD, Sims PJ. Laboratory diagnostic oversight committees and the profession of laboratory Medicine. Am J Clin Pathol. 2013;139(3):273–274. doi:10.1309/AJCPYK7EKWDCBTJC
7. Kim JY, Dzik WH, Dighe AS, Lewandrowski KB. Utilization management in a large urban academic medical center: a 10-year experience. Am J Clin Pathol. 2011;135(1):108–118. doi:10.1309/AJCP4GS7KSBDBACF
8. May TA, Clancy M, Critchfield J, et al. Reducing unnecessary inpatient laboratory testing in a teaching hospital. Am J Clin Pathol. 2006;126(2):200–206. doi:10.1309/WP59YM73L6CEGX2F
9. Zhi M, Ding EL, Theisen-Toupal J, Whelan J, Arnaout R. The landscape of inappropriate laboratory testing: a 15-year meta-analysis. PLoS One. 2013;8(11):e78962. doi:10.1371/journal.pone.0078962
10. Meidani Z, Farzandipour M, Farrokhian A, Haghighat M. A review on laboratory tests’ utilization: a trigger for cutting costs and quality improvement in health care settings. Med J Islam Repub Iran. 2016;30:365.
11. Bakarman MA, Kurashi NY, Hanif M. Utilization of laboratory investigations: study of knowledge, attitude and practice among primary care physicians. J Family Community Med. 1996;3(2):32–40.
12. van Walraven C, Naylor CD. Do we know what inappropriate laboratory utilization is? A systematic review of laboratory clinical audits. JAMA. 1998;280(6):550–558. doi:10.1001/jama.280.6.550
13. Yeh DD. A clinician’s perspective on laboratory utilization management. Clin Chim Acta. 2014;427:145–150. doi:10.1016/j.cca.2013.09.023
14. Ibarz M, Cadamuro J, Sumarac Z, et al. Clinicians’ and laboratory Medicine specialists’ views on laboratory demand management: a survey in nine European countries. Diagnosis. 2021;8(1):111–119. doi:10.1515/dx-2019-0081
15. Freedman DB. Towards better test utilization - strategies to improve physician ordering and their impact on patient outcomes. EJIFCC. 2015;26(1):15–30.
16. Plebani M. Exploring the iceberg of errors in laboratory Medicine. Clin Chim Acta. 2009;404(1):16–23. doi:10.1016/j.cca.2009.03.022
17. MacMillan D. Calculating cost savings in utilization management. Clin Chim Acta. 2014;427:123–126. doi:10.1016/j.cca.2013.09.024
18. Trivelli LA, Ranney HM, Lai HT. Hemoglobin components in patients with diabetes mellitus. N Engl J Med. 1971;284(7):353–357. doi:10.1056/NEJM197102182840703
19. Lyon AW, Higgins T, Wesenberg JC, Tran DV, Cembrowski GS. Variation in the frequency of hemoglobin A1c (HbA1c) testing: population studies used to assess compliance with clinical practice guidelines and use of HbA1c to screen for diabetes. J Diabetes Sci Technol. 2009;3(3):411–417. doi:10.1177/193229680900300302
20. Rollins G. Vitamin D testing—what’s the right answer? Labs grapple with confusing analytics, evidence. Clin Lab News. 2009;35:1–9.
21. Woodford HJ, Barrett S, Pattman S. Vitamin D: too much testing and treating? Clin Med. 2018;18(3):196–200. doi:10.7861/clinmedicine.18-3-196
22. Dickerson JA, Cole B, Conta JH, et al. Improving the value of costly genetic reference laboratory testing with active utilization management. Arch Pathol Lab Med. 2014;138(1):110–113. doi:10.5858/arpa.2012-0726-OA
23. Levy DE, Byfield SD, Comstock CB, et al. Underutilization of BRCA1/2 testing to guide breast cancer treatment: black and Hispanic women particularly at risk. Genet Med. 2011;13(4):349–355. doi:10.1097/GIM.0b013e3182091ba4
24. Sarkar MK, Botz CM, Laposata M. An assessment of overutilization and underutilization of laboratory tests by expert physicians in the evaluation of patients for bleeding and thrombotic disorders in clinical context and in real time. Diagnosis. 2017;4(1):21–26. doi:10.1515/dx-2016-0042
25. Grossman RM. A review of physician cost-containment strategies for laboratory testing. Med Care. 1983;21(8):783–802. doi:10.1097/00005650-198308000-00003
26. Vegting IL, van Beneden M, Kramer MH, Thijs A, Kostense PJ, Nanayakkara PW. How to save costs by reducing unnecessary testing: lean thinking in clinical practice. Eur J Intern Med. 2012;23(1):70–75. doi:10.1016/j.ejim.2011.07.003
27. Vrijsen BEL, Naaktgeboren CA, Vos LM, van Solinge WW, Kaasjager HAH, Ten Berg MJ. Inappropriate laboratory testing in internal medicine inpatients: prevalence, causes and interventions. Ann Med Surg. 2020;51:48–53. doi:10.1016/j.amsu.2020.02.002
28. Horn DM, Koplan KE, Senese MD, Orav EJ, Sequist TD. The impact of cost displays on primary care physician laboratory test ordering. J Gen Intern Med. 2014;29(5):708–714. doi:10.1007/s11606-013-2672-1
29. Schroeder SA, Kenders K, Cooper JK, Piemme TE. Use of laboratory tests and pharmaceuticals. Variation among physicians and effect of cost audit on subsequent use. JAMA. 1973;225(8):969–973. doi:10.1001/jama.1973.03220360029007
30. Kristiansen IS, Hjortdahl P. The general practitioner and laboratory utilization: why does it vary? Fam Pract. 1992;9(1):22–27. doi:10.1093/fampra/9.1.22
31. Stafford RS, Misra B. Variation in routine electrocardiogram use in academic primary care practice. Arch Intern Med. 2001;161(19):2351–2355. doi:10.1001/archinte.161.19.2351
32. McGillivray DL, Roberts-Brauer R, Kramer MS. Diagnostic test ordering in the evaluation of febrile children. Physician and environmental factors. Am J Dis Child. 1993;147(8):870–874. doi:10.1001/archpedi.1993.02160320072022
33. Franks P, Williams GC, Zwanziger J, Mooney C, Sorbero M. Why do physicians vary so widely in their referral rates? J Gen Intern Med. 2000;15(3):163–168. doi:10.1046/j.1525-1497.2000.04079.x
34. Yuan H, Chung F, Wong D, Edward R. Current preoperative testing practices in ambulatory surgery are widely disparate: a survey of CAS members. Can J Anaesth. 2005;52(7):675–679. doi:10.1007/BF03016552
35. Tierney WM, McDonald CJ, Martin DK, Rogers MP. Computerized display of past test results. Effect on outpatient testing. Ann Intern Med. 1987;107(4):569–574. doi:10.7326/0003-4819-107-4-569
36. Bates DW, Kuperman GJ, Rittenberg E, et al. A randomized trial of a computer-based intervention to reduce utilization of redundant laboratory tests. Am J Med. 1999;106(2):144–150. doi:10.1016/S0002-9343(98)00410-0
37. Chen P, Tanasijevic MJ, Schoenenberger RA, Fiskio J, Kuperman GJ, Bates DW. A computer-based intervention for improving the appropriateness of antiepileptic drug level monitoring. Am J Clin Pathol. 2003;119(3):432–438. doi:10.1309/A96XU9YKU298HB2R
38. Embi PJ, Leonard AC. Evaluating alert fatigue over time to EHR-based clinical trial alerts: findings from a randomized controlled study. J Am Med Inform Assoc. 2012;19(e1):e145–e148. doi:10.1136/amiajnl-2011-000743
39. Olakotan OO, Yusof MM. Evaluating the alert appropriateness of clinical decision support systems in supporting clinical workflow. J Biomed Inform. 2020;106:103453. doi:10.1016/j.jbi.2020.103453
40. Murphy DR, Reis B, Sittig DF, Singh H. Notifications received by primary care practitioners in electronic health records: a taxonomy and time analysis. Am J Med. 2012;125(2):
41. Baron JM, Dighe AS. The role of informatics and decision support in utilization management. Clin Chim Acta. 2014;427:196–201. doi:10.1016/j.cca.2013.09.027
42. Harrison JP, McDowell GM. The role of laboratory information systems in healthcare quality improvement. Int J Health Care Qual Assur. 2008;21(7):679–691. doi:10.1108/09526860810910159
43. Aziz HA, Alshekhabobakr HM. Health informatics tools to improve utilization of laboratory tests. Lab Med. 2017;48(2):e30–e35. doi:10.1093/labmed/lmw066
44. Konrad TR, Link CL, Shackelton RJ, et al. It’s about time: physicians’ perceptions of time constraints in primary care medical practice in three national healthcare systems. Med Care. 2010;48(2):95–100. doi:10.1097/MLR.0b013e3181c12e6a
45. Sepulveda JL, Young DS. The ideal laboratory information system. Arch Pathol Lab Med. 2013;137(8):1129–1140. doi:10.5858/arpa.2012-0362-RA
46. Thomas RE, Croal BL, Ramsay C, Eccles M, Grimshaw J. Effect of enhanced feedback and brief educational reminder messages on laboratory test requesting in primary care: a cluster randomised trial. Lancet. 2006;367(9527):1990–1996. doi:10.1016/S0140-6736(06)68888-0
47. O’Sullivan JW, Albasri A, Nicholson BD, et al. Overtesting and undertesting in primary care: a systematic review and meta-analysis. BMJ open. 2018;8(2):e018557. doi:10.1136/bmjopen-2017-018557
48. Greco PJ, Eisenberg JM. Changing physicians’ practices. N Engl J Med. 1993;329(17):1271–1273. doi:10.1056/NEJM199310213291714
49. Keating NL, Zaslavsky AM, Ayanian JZ. Physicians’ experiences and beliefs regarding informal consultation. JAMA. 1998;280(10):900–904. doi:10.1001/jama.280.10.900
50. Solomon DH, Hashimoto H, Daltroy L, Liang MH. Techniques to improve physicians’ use of diagnostic tests: a new conceptual framework. JAMA. 1998;280(23):2020–2027. doi:10.1001/jama.280.23.2020
51. Bunting PS, Van Walraven C. Effect of a controlled feedback intervention on laboratory test ordering by community physicians. Clin Chem. 2004;50(2):321–326. doi:10.1373/clinchem.2003.025098
52. Winkens RA, Pop P, Bugter-Maessen AM, et al. Randomised controlled trial of routine individual feedback to improve rationality and reduce numbers of test requests. Lancet. 1995;345(8948):498–502. doi:10.1016/S0140-6736(95)90588-X
53. Whitman MV, Halbesleben JRB, Holmes IVO. Abusive supervision and feedback avoidance: the mediating role of emotional exhaustion. J Organ Behav. 2014;35(1):38–53. doi:10.1002/job.1852
54. Watts NB. Reproducibility (precision) in alternate site testing. A clinician’s perspective. Arch Pathol Lab Med. 1995;119(10):914–917.
55. Tasse JL, Janzen ML, Ahmed NA, Chung RS. Screening laboratory and radiology panels for trauma patients have low utility and are not cost effective. J Trauma. 2008;65(5):1114–1116. doi:10.1097/TA.0b013e318184b4f2
56. Emerson JF, Emerson SS. The impact of requisition design on laboratory utilization. Am J Clin Pathol. 2001;116(6):879–884. doi:10.1309/WC83-ERLY-NEDF-471E
57. Hindmarsh JT, Lyon AW. Strategies to promote rational clinical chemistry test utilization. Clin Biochem. 1996;29(4):291–299. doi:10.1016/0009-9120(96)00042-2
58. Miyakis S, Karamanof G, Liontos M, Mountokalakis TD. Factors contributing to inappropriate ordering of tests in an academic medical Department and the effect of an educational feedback strategy. Postgrad Med J. 2006;82(974):823–829. doi:10.1136/pgmj.2006.049551
59. Eisenberg JM, Williams SV. Cost containment and changing physicians’ practice behavior. Can the fox learn to guard the chicken coop? JAMA. 1981;246(19):2195–2201. doi:10.1001/jama.1981.03320190053032
60. Fryer AA, Smellie WS. Managing demand for laboratory tests: a laboratory toolkit. J Clin Pathol. 2013;66(1):62–72. doi:10.1136/jclinpath-2011-200524
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.