Back to Journals » International Journal of Women's Health » Volume 12
Knowledge, Attitude, and Practices (KAP) Survey Towards Pelvic Floor Muscle Training (PFMT) Among Pregnant Women
Authors Temtanakitpaisan T , Bunyavejchevin S, Buppasiri P, Chongsomchai C
Received 15 December 2019
Accepted for publication 30 March 2020
Published 17 April 2020 Volume 2020:12 Pages 295—299
DOI https://doi.org/10.2147/IJWH.S242432
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Teerayut Temtanakitpaisan,1 Suvit Bunyavejchevin,2 Pranom Buppasiri,1 Chompilas Chongsomchai1
1Department of Obstetrics and Gynecology, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand; 2Department of Obstetrics and Gynecology, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
Correspondence: Teerayut Temtanakitpaisan
Department of Obstetrics and Gynecology, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand
Tel +66819656423
Email [email protected]
Objective: To assess knowledge, attitude, and practices (KAP) of pelvic floor muscle training (PFMT) among Thai pregnant women.
Patients and Methods: One hundred and ten Thai pregnant women who attended the antenatal clinic of a tertiary care hospital were recruited. They were classified as “aware” if they could recognize PFMT. Questionnaires regarding the participants’ attitudes and practice toward PFMT were subsequently collected from “aware” group.
Results: The mean ±SD of age and gestational age were 30.5 ± 5.4 years and 20.8 ± 10.8 weeks, respectively. Sixty-one participants (55.5%) recognized PFMT, but only seventeen (27.9%) correctly answered all of the questions, which is classified as perceptive. There was no association between their educational level and PFMT knowledge (p = 0.63). Most of them (98.4%) understood that PFMT can be performed during pregnancy and believed that PFMT did not affect the pregnancy outcomes. However, only 10.7% of the aware women performed PFMT irregularly during pregnancy.
Conclusion: Half of the pregnant women in this study were aware of PFMT. The majority of women felt that PFMT had positive effects on their health, emotions, sex, and quality of life. Education concerning PFMT and motivation to maintain the adherence of practicing the exercises are required.
Keywords: KAP, pelvic floor muscle training, pregnant women
Introduction
Pelvic floor dysfunction (pelvic organ prolapse, urinary incontinence, and fecal incontinence) is a devastating condition following the denervation or pelvic floor muscle injury.1 Pregnancy and childbirth are considered the risk contributing to pelvic floor dysfunction.1 To prevent and treat such damage, pelvic floor muscle training (PFMT) is recommended as the first line of treatment to alleviate pelvic symptoms. The integration of PFMT during the antenatal and postnatal periods has been widely recommended so as to treat and prevent urinary incontinence.2 However, the beneficial effect of PFMT has been well established only in the case of treating pelvic floor dysfunction. A setting of prophylaxis against pelvic floor dysfunction prior to delivery has not yet been well studied.2 Moreover, a systematic review reported that the supervised PFMT is an effective means to incorporate the exercise programs into the women’s routines.3 Although PFMT is known to be an effective measure to improve and prevent pelvic floor dysfunction, a considerable number of women are reported to irregularly perform these exercises.4 Guerrero et al reported that the engagement in pelvic floor exercises increased in the immediate postnatal period and subsequently dropped off. Pregnant women are aware that PFMT should be performed daily, but only 15% put this knowledge into practice.5 A study in Taiwanese women reported that the adherence to pelvic floor muscle exercise varies according to attitudes towards the exercise, dyadic cohesion, and perceived benefits of the exercise.6 Tantisiriwat and Manchana found that a majority of women who visited at a gynecologic clinic have limited understanding and half of the women in that study were unaware of PFMT efficacy, and interestingly most of the health care professionals were reported not to know how to instruct women to perform the exercises.7 Whitford et al revealed that almost 80% of the pregnant women acquire knowledge of the PFMT primarily from books and that one-third require additional instruction. More than 50% of the women require a training during the antenatal period.4
Pelvic floor muscle training can reduce stress urinary incontinence and improve symptoms of urogenital prolapse,8 nonetheless, few women realize these advantages. One study reported that half of the women in a gynecologic clinic understand the efficacy of PFMT.7 To perform PFMT regularly, it is critical to know women’s perspective in this exercise. Due to the limited information about women’s attitude on PFMT practice in pregnant women, KAP survey in pregnant women is advocated. Currently, there is no data regarding KAP survey in Thai pregnant women. The aim of this study was therefore to assess the KAP concerning pelvic floor muscle training (PFMT) in Thai pregnant women.
Patients and Methods
A cross-sectional study was conducted at Srinagarind Hospital, Khon Kaen University, Thailand. After IRB approval, one hundred and ten voluntary pregnant women who presented at the antenatal clinic (convenient sampling) from October 2014 to April 2015 were recruited. All participants provided written informed consent, and that this study was conducted in accordance with the Declaration of Helsinki. The inclusion criteria were that participants were singleton pregnant women aged over 18 years old. Meanwhile, participants were excluded if they were found the following high-risk conditions: pre-eclampsia, premature membrane rupture, twin pregnancy, placenta previa, preterm labor, antepartum hemorrhage, history of preterm labor, history of antepartum hemorrhage, and those not understanding Thai language. The research nurses were assigned to deliver and collect self-administered anonymous questionnaires at the antenatal clinic on the day of the visit.
The questionnaires comprise three parts: knowledge, attitudes, and practices. The knowledge part dealt with four questions relating to the pelvic floor exercise (PFE) anatomy, techniques, and usefulness. Participants were classified as perceptive if they could recognize PFMT and correctly answer all questions. The attitude part dealt with 12 questions designed to investigate subjects’ attitudes towards pregnancy outcomes, the effects of pelvic floor functions and the sources influencing their decision about whether to perform PFMT. The practice section constituted a question about the frequency of PFE practice.
Development of the Questionnaire
The questionnaire was based on the conceptual framework (physical, psychosocial, and cultural aspects) derived from focus-group interviews with 10 Thai pregnant women, modified and tested in other 10 Thai pregnant women. A psychometric test was conducted in other 20 pregnant women in order to access its validity and reliability. The content validity was confirmed by two urogynecologists from King Chulalongkorn Memorial Hospital. The test-retest was conducted over a two-week period (Cronbach’s alpha was 0.83, and intraclass correlation (ICC) was 0.95). The developed questionnaire was used as shown in Supplement 1. The sample size was calculated based on a study by Tantisiriwat and Manchana,7 which found that 50% of women were unaware of PFMT. The acceptable rate of error was 10% with an additional 10% for incomplete data. Therefore, a sample size of 110 cases was required.
Statistical Analysis
Statistical analysis was performed using SPSS program version 13.0. Normality testing was conducted using Kolmogorov–Smirnov testing. Demographic data were expressed as percentage, mean (for parametric data) or median (for non-parametric data), and minimum and maximum range. Chi-square tests for correlation were used for categorical variables. Bivariate analysis was performed to evaluate the relationship between women’s responses to the questions and their opinion on PFMT. For the purposes of this analysis, Chi-square tests were used for categorical variables and t-tests were used for continuous variables.
Results
One hundred and ten pregnant participants were recruited. The mean ±SD of age was 30.5 ±5.4 years and the gestational age at the time of enrolment was 20.8 ±10.8 weeks. Participants’ baseline characteristics are shown in Table 1. There was no association between the educational level and the prior knowledge of PFMT (p = 0.63). Sixty-one of the patients (55.5%) possessed the knowledge of the pelvic floor muscle training. However, after being tested for the knowledge of PFMT, only seventeen (27.9%) knew the correct answers, who were classified as the perceptive. Of the 61 participants recognizing PFMT, fifty-seven (93.4%) realized the advantages of PFMT and forty-eight (78.7%) realized the disadvantages of PFMT. In addition, fifty-nine (96.7%) possessed the understanding that they could undergo PFMT with safety during pregnancy.
 |
Table 1 Patients' Characteristics (N= 110) |
The principal sources of information from which the subjects acquired the knowledge of PFMT were health-care providers (58.8%) and media outside hospital (35.3%) (Table 2). Interestingly, however, among health-care providers, no subjects received information directly from physicians. As for the aware participants’ understanding of PFMT towards pregnancy outcomes, 78.7% believed that PFMT could facilitate delivery. In addition, 57.4% believed that PFMT could reduce vaginal trauma during vaginal birth. None of the participants believed that PFMT caused difficult vaginal childbirth or fetal demise (Table 3).
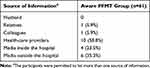 |
Table 2 The Sources of Pelvic Floor Muscle Training Information Among Aware PFMT Women (n=61) |
 |
Table 3 Attitudes Toward Pregnancy Outcomes and Pelvic Floor Functions Among Aware PFMT Women (n=61) |
The majority of women in aware group believed that PFMT could improve all aspects of pelvic floor dysfunction such as sexual dysfunction, pelvic pain, urinary incontinence, voiding dysfunction, pelvic organ prolapse symptoms, constipation, fecal incontinence, and overall quality of life (Table 3).
As for PFMT practice, only 10.7% of the aware women performed PFMT but irregularly during pregnancy.
Discussion
Pelvic floor muscle training during pregnancy plays a critical role in preventing pelvic floor dysfunction. Fundamental data from the survey of pregnant women regarding PFMT can provide information for health-care workers to realize the problem and plan of treatment.
This study revealed that half of the pregnant women recognized PFMT. However, only 27.9% were perceptive, indicating that they lack the relevant detailed information about PFMT. The most common source of information concerning PFMT was derived from health-care providers. This finding is in agreement with Whitford et al’s study, which revealed that 77.9% of pregnant women received PFMT information from health professionals.9 Only one-fourth of the aware group had correct understanding. This suggests that additional knowledge in PFMT is required in pregnant women. Therefore, health-care providers, especially physicians as well as nurses at the antenatal clinic, should realize the benefits of PFMT and advice the pregnant women to incorporate these exercises throughout pregnancy.
Most of the pregnant women in this study perceived that PFMT ensured safety to perform during pregnancy and that it improved the symptom of pelvic floor dysfunction. The findings from a study showed the similar positive attitudes toward PFMT toward pelvic floor dysfunction.10 The Cochrane review in 2017 supported the evidence of the preventive role of PFMT during antenatal period in continent pregnant women. Urinary incontinence risk was significantly lower in late pregnancy and mid-postnatal period (3–6 months’ postpartum) when compared with not doing the PFMT.11 Moreover, data from one systematic review published in 2018 regarding the pelvic floor intervention during pregnancy found that pelvic floor muscle training during pregnancy significantly reduced the duration of second stage of labor (p<0.01) and decreased the incidence of urinary incontinence (p=0.04).12
The underlying problem of PFMT practice lied in adherence to the PFMT regimen. We found that the participants rarely performed the regular exercises. According to our findings, only 10.7% of the participants practiced irregularly, which is consistent with the report from Guerrero et al.5 A previous report found that a decision of the practice of PFMT depends on patients’ awareness of the benefits of PFMT.13 In addition, we found that women’s knowledge and attitudes were the crucial factors in determining whether to perform PFMT. Thus, in order to motivate Thai pregnant women to practice PFMT regularly, we recommend to educate the benefits of PFMT and undergo follow-ups during pregnancy. The integration of PFMT into daily life activity may also enhance the compliance rate.13,14 Moreover, beliefs with regard to the efficacy of the practices are a potential factor in adherence prediction.14 So as to raise awareness of the health concern, PFMT should be integrated into the gym or fitness center classes to promote the pelvic floor exercises.
To our knowledge, this survey is the first study based on a knowledge, attitudes, and practices (KAP) survey regarding PFMT in Thai pregnant women. This study was conducted using a validated questionnaire investigating attitudes regarding effects of PFMT on pregnancy outcomes and pelvic floor function.
As this was a cross-sectional study, we asked only about compliance without evaluating PFMT techniques, which is the limitation of our study.
Conclusions
The findings suggest that only half of the subjects were aware of PFMT, but they rarely practiced regularly. Based on our data, almost all women felt that PFMT has positive effects on health, emotions, sex, and quality of life. Thus, it is recommended to provide essential education or motivation in order to raise importance of PFMT practice in pregnant Thai women.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The abstract of this paper was presented at the IUGA 2015 Conference name “KNOWLEDGE, ATTITUDE AND PRACTICE (KAP) SURVEY TOWARDS PELVIC FLOOR MUSCLE TRAINING (PFMT) AMONG THAI PREGNANT WOMEN” as a poster presentation with interim findings. The poster’s abstract was published in IUGA academy website as: Hyperlink https://academy.iuga.org/iuga/2015/40th/141950/teerayut.temtanakitpaisan.knowledge.attitude.and.practice.28kap29.survey.towards.html. The authors report no conflicts of interest in this work.
References
1. Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am. 1998;25(4):723–746. doi:10.1016/S0889-8545(05)70039-5
2. Boyle R, Hay-Smith EJC, Cody JD, Mørkved S. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2012;10:CD007471.
3. Mørkved S, Bø K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: a systematic review. Br J Sports Med. 2014;48(4):299–310. doi:10.1136/bjsports-2012-091758
4. Whitford HM, Alder B, Jones M. A longitudinal follow up of women in their practice of perinatal pelvic floor exercises and stress urinary incontinence in North-East Scotland. Midwifery. 2007;23(3):298–308. doi:10.1016/j.midw.2006.05.009
5. Guerrero K, Owen L, Hirst G, Emery S. Antenatal pelvic floor exercises: a survey of both patients’ and health professionals’ beliefs and practice. J Obstet Gynaecol. 2007;27(7):684–687.
6. Chen S-Y, Tzeng Y-L. Path analysis for adherence to pelvic floor muscle exercise among women with urinary incontinence. J Nurs Res. 2009;17(2):83–92. doi:10.1097/JNR.0b013e3181a53e7e
7. Tantisiriwat N, Manchana T. Knowledge and acceptance of Thai women toward the pelvic floor muscle training. J Med Assoc Thai. 2014;97(1):7–11.
8. Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–240. doi:10.1002/nau.20870
9. Whitford HM, Alder B, Jones M. A cross-sectional study of knowledge and practice of pelvic floor exercises during pregnancy and associated symptoms of stress urinary incontinence in North-East Scotland. Midwifery. 2007;23(2):204–217. doi:10.1016/j.midw.2006.06.006
10. Liao Y-M, Dougherty MC, Liou Y-S, Tseng I-J. Pelvic floor muscle training effect on urinary incontinence knowledge, attitudes, and severity: an experimental study. Int J Nurs Stud. 2006;43(1):29–37. doi:10.1016/j.ijnurstu.2005.01.004
11. Woodley SJ, Boyle R, Cody JD, Mørkved S, Hay-Smith EJC. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2017;12:CD007471.
12. Schreiner L, Crivelatti I, de Oliveira JM, Nygaard CC, Dos Santos TG. Systematic review of pelvic floor interventions during pregnancy. Int J Gynaecol Obstet. 2018;143(1):10–18. doi:10.1002/ijgo.12513
13. McClurg D, Frawley H, Hay-Smith J, et al. Scoping review of adherence promotion theories in pelvic floor muscle training - 2011 ICS state-of-the-science seminar research paper i of iv. Neurourol Urodyn. 2015;34(7):606–614. doi:10.1002/nau.22769
14. Hay-Smith EJC, McClurg D, Frawley H, Dean SG. Exercise adherence: integrating theory, evidence and behaviour change techniques. Physiotherapy. 2016;102(1):7–9. doi:10.1016/j.physio.2015.08.006
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
