Back to Journals » Integrated Pharmacy Research and Practice » Volume 11
Knowledge, Attitude and Practice of Community Pharmacists in Relation to Dispensing Antibiotics Without Prescription in Sudan: A Cross-sectional Study
Authors Abdelrahman Hussain M , Osman Mohamed A , Sandel Abkar A, Siddig Mohamed F, Khider Elzubair H
Received 24 April 2022
Accepted for publication 13 July 2022
Published 25 July 2022 Volume 2022:11 Pages 107—116
DOI https://doi.org/10.2147/IPRP.S363079
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Jonathan Ling
Mohamed Abdelrahman Hussain, Ahmed Osman Mohamed, Alsara Sandel Abkar, Fatima Siddig Mohamed, Hana Khider Elzubair
Department of Pharmaceutical Microbiology, Faculty of Pharmacy, International University of Africa, Khartoum, Sudan
Correspondence: Ahmed Osman Mohamed, Department of Pharmaceutical Microbiology, Faculty of Pharmacy, International University of Africa, P. O. Box 2469, Madani Street, Khartoum, Sudan, Email [email protected]
Background: Dispensing antibiotics without prescription (DAwP) is a widespread practice, especially in developing countries, contributing to antibiotic resistance. Community pharmacists play a significant role in promoting rational use of antibiotics by refraining from DAwP, and providing drug information to patients. This study aimed to evaluate community pharmacists’ knowledge, attitude and practice, and to assess the factors behind DAwP.
Methods: A cross-sectional study was conducted in 2020 among random sample of community pharmacists in Sudan. Online semi-structured questionnaire was used for data collection. The association between dependent and independent variables was assessed using Chi-square test; a P-value less than 0.05 was considered significant.
Results: Of the 1217 pharmacists who participated, the majority were female (n = 645, 53%). Most pharmacists have a B. Pharm degree (n = 1026, 84%) and less than 5 years’ experience (n = 718, 59%). Notably, the majority of community pharmacists have good knowledge (n = 735, 61.7%), which is significantly associated with years of experience (P < 0.00). More than half (n = 623, 52.2%) of the pharmacists have above average score of practice. Nearly all the pharmacists who participated have a positive attitude in relation to DAwP (n = 1204, 98.9%). More than half of the pharmacists were DAwP for tonsillitis (n = 817, 67%), wound infection (n = 766, 62.9%), and urinary tract infection (n = 664, 54%). The leading factor behind DAwP was the low socioeconomic status of the patients (n = 624, 51%). Additionally, 47% of the pharmacists (n = 572) thought that they were knowledgeable enough to DAwP.
Conclusion: Despite their positive attitude and average level of knowledge regarding DAwP, Sudanese community pharmacists frequently are DAwP for tonsillitis. Low patients’ socioeconomic status was the leading factor behind DAwP. Accordingly, extensive work from health authorities to improve the accessibility and affordability of the health system as well as the development of an antibiotic stewardship program are required to diminish DAwP.
Keywords: DAwP, Sudan, pharmacist practice, antimicrobial resistance
Introduction
Antimicrobial resistance (AMR) has been declared by the World Health Organization (WHO) as one of the top ten global public health threats facing humanity.1 Currently, AMR is causing 700,000 deaths worldwide each year and this number is expected to be approximately 10 million people by 2050. The majority of deaths are anticipated to be in low- to middle-income countries (LMICs), where devastating infectious diseases are well-established.2
It has been estimated that in the United States of America more than 2 million people are infected with antibiotic-resistant bacteria, resulting in 23,000 deaths annually.3 While in Europe, 25,000 deaths occur each year due to AMR.4 Whereas in Asia, the mortality rate as a consequence of AMR reaches 96,000 per year.5
The current situation in African countries is catastrophic and very difficult to precisely describe since very few countries give a regular national surveillance report on AMR.6 The poor hygiene along with the growth in immunocompromised patients are further exaggerating the AMR in Sub-Saharan Africa (SSA).6 It was claimed that the majority of global antibiotic consumption between 2000 and 2015 was in LMICs, especially in SSA, mainly due to their high incidence of infectious diseases. Additionally, it was reported that most of the deaths are expected to be in SSA owing to their low financial capability of the health care system.7
Several factors contribute to the development of AMR,8 however overuse and misuse of antibiotics are the most prevalent, accelerating the development of AMR; yet they are easily preventable.9,10 Despite the constraints which have been devolved to combat the misuse of antibiotics, it has been estimated that 50% of the antibiotics are prescribed without prescription worldwide.11 In Africa, recent Meta-analysis has reported that the overall proportion of non-prescription dispense of antibiotics was 69% in Sub-Saharan Africa more frequently prescribed for upper respiratory tract infection and diarrhea.7
Dispensing antibiotics without prescription (DAwP) and antibiotic self-medication are multidimensional and require public awareness and good practice on the part of both clinicians and pharmacists.12 In LMICs pharmacists are believed to be the common cause of antibiotic self-medication.13,14 The low socioeconomic status of the patients is rated as the most common cause of antibiotic self-medication in LMICs.
The regulation of the health system in Sudan is carried out at three levels: federal, state, and locality. The national health insurance was introduced in 1990; however, universal coverage has not yet been achieved and, consequently, economic status is rated as the common cause behind self-medication in addition to the easy accessibility of medication from pharmacies.15 In Sudan, a report published in 2006 indicated that out of 817 participants, antibiotics were the most common self-medication (36%).16 Also, a cross-sectional study in Khartoum state reported that 41–80% of participants use antibiotics and antimalarials as self-medication.17 Furthermore, in 2017 a simulated study was conducted in Khartoum state to determine DAwP by community pharmacists, which concluded that patients’ inability to afford consultation fees was the main factor behind DAwP.18
Recently, a national action plan was launched in 2018 against AMR to achieve a better understanding of AMR, build surveillance research on AMR, and improve antimicrobial use in humans and animals (https://www.who.int/publications/m/item/sudan-national-action-plan-on-antimicrobial-resistance). However, previous reports indicate that pharmacists are still DAwP.18,19 Thus the current study was conducted to assess the knowledge, attitude, and practice of pharmacists in relation to antibiotics and AMR as well as to understand the main factors behind DAwP. It also explores the common medical conditions for DAwP by community pharmacists.
Materials and Methods
Study Design and Setting
A cross-sectional descriptive study was conducted in all Sudan regions (a country located in Northeast Africa with a total population estimated to be 44 million people distributed in 18 states) between 25th February and 29th November 2020.
Eligibility Criteria
All registered pharmacists at the Sudan Medical Council (SMC) who were willing to participate in the study were included. Pharmacists not working in community pharmacies were excluded.
Sample Size
The total number of registered pharmacists in Sudan is 20,000 (data were obtained from Sudan Medical Council, December 2019 update). Sample size was calculated based on Solvin’s equation20 as follows: n = N/ 1+ N (e) 2, where n = sample size, N = targeted population attending a different pharmacy, e = margin of error (0.05) at 95% confidence level, resulting in a sample size of 380. However, we use all 1217 received responses to ensure generalizability.
Data Sources and Measurement
An online semi-structured questionnaire with closed-ended questions was designed based on previous studies.18,21 The questionnaire link was shared with pharmacists through WhatsApp groups of each state of Sudan where most of the pharmacists gather.
The questionnaire consisted of 28 questions divided into six sections. Section one gathered information regarding pharmacist gender, years of experience, and current qualifications. Section two assessed pharmacists’ knowledge (7 items) regarding antibiotic usage and antibiotic resistance in three scales (yes, no, or unsure). Pharmacists’ attitude was measured by asking 5 questions on a 5-point Likert scale in section three. In section four, practice of the community pharmacists was assessed (9 items) on three scales (always, sometimes, or never). Sections five and six were dedicated to investigate the factors behind DAwP and the common medical conditions for DAwP, respectively (more than one option was allowed in these sections). The complete form of the questionnaire used for data collection is provided as Supplementary Material.
Since there was no consistency in scaling knowledge, attitude, and practice in the current literature, we used the median to categorise the pharmacists into good and poor knowledge, good and poor practice, and positive and negative attitude. For each participant, the overall knowledge, attitude, and practice was calculated by dividing the summation of the correct answers over the total question numbers in each section.
The questionnaire was validated at two levels;22 content validity was assessed by a Professor of Pharmacology and an Associated Professor of Pharmaceutical Microbiology who are experts in this field. Their comments were used to improve the questionnaire content, structure, and language. Face validity was carried out by a pilot questionnaire administered to 21 community pharmacists; their comments were adopted to clarify the questions. Those pharmacists who participated in the pilot study were excluded from the final result.
Statistical Methods
Data were entered and analysed using SPSS (Statistical Package for Social Sciences) software, version 25. Descriptive statistics using frequency and proportion were used to summarize the data; chi-square test and Fisher exact test were used, where applicable, to assess the association between demographic data and knowledge, attitude, and practice; and a P-value of less than 0.05 was considered statistically significant.
Ethical Statements
The protocol of the present study was approved by the Faculty of Pharmacy, International University of Africa. Informed consent was provided to all participants in the first statement of the questionnaire. Names and personal identifiers were not used to ensure confidentiality.
Results
Socio-Demographic Characteristics
A total of 1217 pharmacists completed and returned the questionnaire from 18 states in Sudan; more than one-quarter of the respondents were from the capital state of Khartoum (n = 353, 29%). Out of 1217 pharmacists, 53% were female (n = 645), and more than half (n = 718, 59%) have less than 5 years of experience in community pharmacies. The vast majority of the participating pharmacists have a B. Pharm degree as a higher qualification (n = 1026, 84%). Socio-demographic characteristics are shown in Table 1.
 |
Table 1 Socio-demographic Characteristic of the Participating Pharmacists |
Pharmacists’ Knowledge
Out of 1217 pharmacists enrolled in the study, the total knowledge score of participants was 4.34 ± 1.36 out of the maximal attainable score of 7. In this study, more than half (n = 735, 61.7%) of the participants have a good knowledge of antibiotics and AMR. The good knowledge score was significantly associated (P = 0.008) with Pharmacists who have than more than 10 years’ experience, whereas, pharmacists’ gender and qualifications were not statistically significant.
Nearly half of the pharmacists (n = 629, 51.7%) thought that antibiotics are indicated to relieve inflammation. More than two-thirds of the pharmacists declared that resistant bacteria can be transmitted in health facilities, while more than half believed that the occurrence of resistance is a problem only in a hospital setting (n = 703, 57.8%). The vast majority (n = 1174, 96.5%) agreed with the fact that inappropriate antibiotic usage will increase the emergency of resistance; on the other hand, one-quarter of the pharmacists advised patients to stop taking antibiotics when their symptoms improved (n = 209, 23.8%). Table 2 summarizes the pharmacist’s responses to individual questions.
 |
Table 2 Community Pharmacists’ Knowledge Regarding Antibiotic Resistance |
Pharmacists’ Practice
Among the 1217 participating pharmacists, the total practice score was 5.47 ± 1.75. Nearly half (n = 623, 51.2%) of the pharmacists have good practice when DAwP; 70% always ask about medication history; and 79% explain to the patients the importance of medication adherence. Nearly two-thirds (n = 755, 62%) receive feedback when DAwP. There were no significant differences between pharmacists’ practice and gender, years of experience, and qualifications (Tables 3 and 4).
 |
Table 3 Practice of Community Pharmacists Regarding Dispensing Antibiotics Without Prescription |
 |
Table 4 Association Between Knowledge, Attitude, Practice and Characteristics of the Community Pharmacists Included in the Study |
Pharmacists’ Attitude
In the current study, the overall score of attitudes among the participating pharmacists was 4.49 ± 0.35 out of a maximum achievable score of 5. The vast majority of the participating pharmacists (n = 1204, 98.9%) have a positive attitude concerning DAwP. The majority of the pharmacists (n = 1100, 82%) strongly agreed with the fact that antibiotics are overprescribed in Sudan. More than one-third (n = 505, 41.5%) of the pharmacists agreed that forbidding the dispensing of antibiotics without medical prescription will decrease pharmacy profits. Pharmacists’ attitude was not statistically significant in relation to gender, qualifications or years of experience (Tables 4 and 5).
 |
Table 5 Community Pharmacists’ Attitude Regarding Dispensing Antibiotics Without Prescription |
Common Medical Conditions and Pharmacists’ Reasons Behind DAwP
As shown in Table 6, two-thirds of the pharmacists (n = 817, 67%) were DAwP for tonsillitis and more than half for wound infection (n = 766, 62.9%) and UTIs (n = 664, 54.6%). Low socioeconomic status of patients was the main factor behind DAwP (n = 624, 51%). On the other hand, nearly half of the pharmacists (n = 572, 47%) thought that they were knowledgeable enough to DAwP. Common pharmacists’ reasons behind DAwP are shown in Table 7.
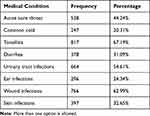 |
Table 6 Common Medical Conditions for Which Pharmacists Dispense Antibiotics Without Prescription |
 |
Table 7 Factors Behind Dispensing Antibiotics Without Prescription |
Discussion
DAwP is a key factor contributing to irrational use of antibiotics, which in turn hastens the rate of emerging resistant pathogens. To the best of our knowledge, this study is the first nationwide observational study to assess level of knowledge, attitude, and practice of community pharmacists in Sudan, as well as to determine pharmacists’ reasons for DAwP and the common medical conditions for DAwP. Out of 1217 pharmacists enrolled, more than half have good knowledge (61%) and practice (51%), and roughly all of the pharmacists have a positive attitude (98.9%).
In the present study, 61% of the pharmacists have good knowledge regarding DAwP and AMR. This finding is higher than that obtained in Egypt (51%),21 and lower than in Tanzania (77%).23 Variations in the studies are attributed to the structure of the questionnaire and questions used. They might also be due to the scoring system used in each study, since there is inconsistency in the scaling system; in the current study the median of the data was used as a cut-off. Similar to the results obtained in Tanzania,23 overall knowledge scores were significantly associated with years of experience (P = 0.008). The proportion of pharmacists with more than 10 years’ experience having a good knowledge score (70%) was greater than those having less than 10 years’ experience (60%).
Alarmingly, more than half of the pharmacists (51%) thought that antibiotics can be used to treat inflammations. This finding is much higher than that in an Egyptian study (15.1%),21 which might be due to the fact that pharmacists were confused between the terms “infection” and “inflammation”. Also, one-quarter (23.1%) of the pharmacists thought that patients should stop taking antibiotics when their symptoms improved, clearly pointing to their poor knowledge. To overcome this, the department of continuing professional development in the Ministry of Health should develop further courses on antibiotic usage and prescriptions for graduated community pharmacists. Furthermore, the SMC should focus on AMR and how antibiotics are prescribed in the professional examination for pharmacists to obtain their licence.
While more than half (52.2%) of the pharmacists have above-average scores in relation to practice, worryingly the vast majority of the pharmacists were “always” or “sometimes” DAwP (93.4%), which is higher than is reported in Egypt (77.6%) and Tanzania (77.2%).21,23 Additionally, nearly half (48%) of the pharmacists were DAwP if the patients request a particular antibiotic by name; this figure is lower than in a previous study in Nigeria (65%).24 However, such findings reflect the malpractice of the Sudanese community pharmacists, given the fact that antibiotics are stated to be “Prescription only Medicine” in Sudan.19 Health authorities should thus implement an antibiotics stewardship program, particularly as adoption of such strategies in some countries has dramatically reduced DAwP.25,26
In contrast, more than two-thirds of the pharmacists always explain to patients why they do not need antibiotics, ask patients about their medical and medication history, and educate patients about the importance of adherence and completing the full course of antibiotics.
Fortunately, nearly all participating pharmacists have a positive attitude regarding DAwP (98.9%). This figure is higher than that obtained in Egypt (42.7%).21 Additionally, most of the pharmacists (80.5%) strongly agreed that they have a responsibility to take an effective role in reducing antibiotic resistance. Given their positive attitude, the role of the pharmacists should be extended further to educate the public about the negative consequences of DAwP.
An attempt to explore the common medical conditions for which community pharmacists DAwP was included in the current study and more than half of the pharmacists DAwP to treat tonsillitis (67.1%), UTIs (54.6%), and wound infections (62.9%), which is similar to the findings in a previous study in Nigeria where 62.9% and 83% of the pharmacists were DAwP to treat wound infection and UTIs, respectively.24 On the other hand, the finding is inconsistent with that reported in the Kingdom of Saudi Arabia, in which 68.4% of the pharmacists were DAwP to treat colds and flu (20% in this study).27 The possible reason for such discrepancies might be due to variations in the epidemiology of these conditions in the three countries. However, regardless of the symptoms, DAwP should be prohibited by the community pharmacist.
The common factors behind DAwP were investigated in this study, strictly following a previous qualitative exploratory interview study in Sudan, in which patients’ inability to afford consultation fees was reported to be the main factor behind DAwP. More than half (51.3%) of the participating pharmacists indicated that low socioeconomic status of the patients was the main factor; additionally, more than one-third (37.1%) declared that patient pressure was the common factor.18 The association between self-medication, low socioeconomic status and lack of medical insurance was reported previously among the Sudanese community.28,29 These findings require urgent action to further improve the accessibility and quality of the governmental health services provided, particularly the national health insurance. Moreover, the role of the community pharmacists should be further extended to educate patients about the negative consequences of antibiotics as a self-medication.
One of the findings that must be pointed out in this study is that nearly half of pharmacists (47%) thought that they were knowledgeable enough to DAwP, a finding that is consistent with that reported in Nigeria (78%).24 This finding is paradoxical, since nearly half of community pharmacists lack basic knowledge of antibiotics (51% have good knowledge). Health authorities in Sudan should undertake comprehensive measures to further guide community pharmacists about the rational use of antibiotics.
DAwP is a malpractice accelerating the development of AMR and must be urgently prohibited; however, this is caused by low socioeconomic status, poor accessibility of medicine, and lack of insurance. Accordingly, a multidimensional approach from the regulatory authorities is required to delay the development of AMR in Sudan.
One of the limitations required to be pointed out in this study is that the findings are subject to selection bias since this is an online survey. An attempt was done to minimize this by sending the link to a known WhatsApp group for pharmacists.
Conclusion
Despite their positive attitude and average level of knowledge regarding antibiotics and antimicrobial resistance, Sudanese community pharmacists frequently DAwP to treat tonsillitis. Patient pressure and primarily low socioeconomic status are the main factors leading to this malpractice.
Acknowledgment
The authors would like to acknowledge all the pharmacists who participated in this study.
Disclosure
The authors reported no conflicts of interest in relation to this work.
References
1. Dadgostar P. Antimicrobial resistance: implications and costs. Infect Drug Resist. 2019;12:3903. doi:10.2147/IDR.S234610
2. O’Neill J. Review on antimicrobial resistance: tackling drug-resistant infections globally: final report and recommendations; 2016.
3. Control CfD, Prevention. Antibiotic resistance threats in the United States, 2013; 2013. Available from: https://www.cdc.gov/drugresistance/threat-report-2013/index.html.
4. Pourmand A, Mazer-Amirshahi M, Jasani G, May L. Emerging trends in antibiotic resistance: implications for emergency medicine. Am J Emerg Med. 2017;35(8):1172–1176. doi:10.1016/j.ajem.2017.03.010
5. Khan MU, Hassali MAA, Ahmad A, Elkalmi RM, Zaidi STR, Dhingra S. Perceptions and practices of community pharmacists towards antimicrobial stewardship in the state of Selangor, Malaysia. PLoS One. 2016;11(2):e0149623. doi:10.1371/journal.pone.0149623
6. Berhe DF, Beyene GT, Seyoum B, et al. Prevalence of antimicrobial resistance and its clinical implications in Ethiopia: a systematic review. Antimicrob Resist Infect Control. 2021;10(1):1–14. doi:10.1186/s13756-021-00965-0
7. Belachew SA, Hall L, Selvey LA. Non-prescription dispensing of antibiotic agents among community drug retail outlets in Sub-Saharan African countries: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2021;10(1):1–15. doi:10.1186/s13756-020-00880-w
8. World Health Organization Geneva. Antibiotic resistance: World Health Organization Geneva; 2018.
9. Rather IA, Kim B-C, Bajpai VK, Park Y-H. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci. 2017;24(4):808–812. doi:10.1016/j.sjbs.2017.01.004
10. Levy SB. The antibiotic paradox. How miracle drugs are destroying the miracle; 1992.
11. Cars O, Nordberg P. Antibiotic resistance–The faceless threat. Int J Risk Saf Med. 2005;17(3, 4):103–110.
12. Lescure D, Paget J, Schellevis F, Van Dijk L. Determinants of self-medication with antibiotics in European and Anglo-Saxon countries: a systematic review of the literature. Front Public Health. 2018;6:370. doi:10.3389/fpubh.2018.00370
13. Alhomoud F, Aljamea Z, Almahasnah R, Alkhalifah K, Basalelah L, Alhomoud FK. Self-medication and self-prescription with antibiotics in the Middle East—do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis. 2017;57:3–12. doi:10.1016/j.ijid.2017.01.014
14. Zawahir S, Lekamwasam S, Aslani P. A cross-sectional national survey of community pharmacy staff: knowledge and antibiotic provision. PLoS One. 2019;14(4):e0215484. doi:10.1371/journal.pone.0215484
15. Salim AMA, Hamed FHM. Exploring health insurance services in Sudan from the perspectives of insurers. SAGE Open Med. 2018;6:2050312117752298. doi:10.1177/2050312117752298
16. Awad AI, Eltayeb IB, Capps PA. Self-medication practices in Khartoum state, Sudan. Eur J Clin Pharmacol. 2006;62(4):317–324. doi:10.1007/s00228-006-0107-1
17. Awad A, Eltayeb I, Thalib L, Matowe L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Pharm Pharm Sci. 2005;8(2):326–331.
18. Salim AM, Elgizoli B. Exploring the reasons why pharmacists dispense antibiotics without prescriptions in Khartoum state, Sudan. Int J Pharm Pract. 2017;25(1):59–65. doi:10.1111/ijpp.12317
19. Mahmoud MA, Aldhaeefi M, Sheikh A, Aljadhey H. Community pharmacists perspectives about reasons behind antibiotics dispensing without prescription: a qualitative study. Biomed Res. 2018;29(21). doi:10.4066/biomedicalresearch.29-18-1112
20. Galero-Tejero E. A Simplified Approach to Thesis and Dissertation Writing. Mandaluyong City: National Book Store; 2011:43–44.
21. El-din M Z, Samy F, Mohamed A, Hamdy F, Yasser S, Ehab M. Egyptian community pharmacists’ attitudes and practices towards antibiotic dispensing and antibiotic resistance; a cross-sectional survey in Greater Cairo. Curr Med Res Opin. 2019;35(6):939–946. doi:10.1080/03007995.2018.1544119
22. Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179(3):245–252. doi:10.1503/cmaj.080372
23. Poyongo BP, Sangeda RZ. Pharmacists’ knowledge, attitude and practice regarding the dispensing of antibiotics without prescription in Tanzania: an explorative cross-sectional study. Pharmacy. 2020;8(4):238. doi:10.3390/pharmacy8040238
24. Abubakar U, Tangiisuran B. Knowledge and practices of community pharmacists towards non-prescription dispensing of antibiotics in Northern Nigeria. Int J Clin Pharm. 2020;42(2):756–764. doi:10.1007/s11096-020-01019-y
25. Santa-Ana-Tellez Y, Mantel-Teeuwisse AK, Dreser A, Leufkens HG, Wirtz VJ. Impact of over-the-counter restrictions on antibiotic consumption in Brazil and Mexico. PLoS One. 2013;8(10):e75550. doi:10.1371/journal.pone.0075550
26. Bavestrello L. trends of community consumption of antibiotics in Chile. Rev Med Chile. 2002;130(11):1265–1272.
27. Hadi MA, Karami NA, Al-Muwalid AS, et al. Community pharmacists’ knowledge, attitude, and practices towards dispensing antibiotics without prescription (DAwP): a cross-sectional survey in Makkah Province, Saudi Arabia. Int J Infect Dis. 2016;47:95–100. doi:10.1016/j.ijid.2016.06.003
28. Elhada A, Eltayeb IB, Mudawi MM. Pattern of self-medication with antibiotics in Khartoum State, Sudan. World J Pharm Res. 2014;3(5):678–692.
29. Yousif M. In-home drug storage and utilization habits: a Sudanese study. East Mediterr Health J. 2002;8(2–3):422–431. doi:10.26719/2002.8.2-3.422
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
