Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Kinesiophobia in Elderly Polish Patients After Ischemic Stroke, Including Frailty Syndrome
Authors Bąk E , Młynarska A , Marcisz C , Kadłubowska M, Marcisz-Dyla E, Sternal D, Młynarski R , Krzemińska S
Received 2 December 2021
Accepted for publication 22 February 2022
Published 31 March 2022 Volume 2022:18 Pages 707—715
DOI https://doi.org/10.2147/NDT.S352151
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Ewelina Bąk,1 Agnieszka Młynarska,2 Czesław Marcisz,2 Monika Kadłubowska,1 Ewa Marcisz-Dyla,3 Danuta Sternal,1 Rafał Młynarski,4 Sylwia Krzemińska5
1Faculty of Health Sciences, University of Bielsko-Biala, Bielsko-Biala, Poland; 2Department of Gerontology and Geriatric Nursing, School of Health Sciences, Medical University of Silesia, Katowice, Poland; 3Faculty of Management, Psychology, Katowice Business University, Katowice, Poland; 4Department of Electrocardiology and Heart Failure, School of Health Sciences, Medical University of Silesia, Katowice, Poland; 5Department of Clinical Nursing, Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland
Correspondence: Sylwia Krzemińska, Email [email protected]
Introduction: In patients after stroke, the relationship between the occurrence of kinesiophobia and the accompanying frailty syndrome, as well as the acceptance of the disease and the level of mood, has not been recognized so far. The aim of this study was to determine the prevalence of kinesiophobia in elderly Polish people after ischemic stroke, including the frailty syndrome and the associations between the prevalence of kinesiophobia and feelings of anxiety and degree of the illness acceptance.
Methods: A cross-sectional study was used to achieve the study objectives. The study involved 152 hospitalized patients aged of minimum 60 (mean age 63), qualified for post-stroke rehabilitation, including 76 women and 76 men. The patients were divided into two groups, with kinesiophobia (119 persons) and without kinesiophobia (33 persons). The Tampa Scale of Kinesiophobia (TSK), the Tilburg Frailty Indicator (TFI), the Hospital Anxiety Depression Scale (HADS) and the Acceptance of Illness Scale (AIS) were used. Study results were calculated using MedCalc Software.
Results: Kinesiophobia has been demonstrated in 78% of people after ischemic stroke. The values of TFI and HADS were higher in the patients with kinesiophobia (p< 0.001). In patients with ischemic stroke, it was shown that the level of kinesiophobia increased with higher anxiety (p< 0.001), higher total TFI score, (p< 0.05), and a lower level of illness acceptance (p< 0.001).
Conclusion: The occurrence of kinesiophobia in elderly Polish people after ischemic stroke is common and the determinants of its development are the coexistence of the frailty syndrome, anxiety and a low level of illness acceptance. In post-stroke patients, the presence of kinesiophobia should be considered, especially in the situation of comorbid frailty syndrome. The issue of kinesiophobia in patients after stroke requires further in-depth research, especially in the field of cognitive-behavioral prevention aimed at ways to reduce this phenomenon.
Keywords: kinesiophobia, elderly patients, ischemic stroke, frailty syndrome
Introduction
One of the common cardiovascular diseases is a stroke, which is a serious public health problem. In 2016, over 24 million people worldwide developed a stroke.1 Stroke patients require rehabilitation, especially in the psychomotor field. Stroke rehabilitation is a coordinated use of medical, social and educational measures in order to achieve the highest possible physical and psychological fitness and socio-professional potential, in accordance with physiological and environmental limitations.2 The importance of physical activity in the psychomotor rehabilitation of stroke patients in order to minimize symptoms with a chance for better functioning has been strongly emphasized in the literature.3 An important barrier to achieve adequate physical activity levels might be specifically a fear of movement, called kinesiophobia.4 According to Kori et al, kinesiophobia is a condition in which the person experiences an excessive, irrational and debilitating fear of movement and physical activity resulting from the feeling of being susceptible to painful injuries or their recurrence.4 Models describing the causes of kinesiophobia perceive pain as a threat and a factor influencing the development of anxiety and fear, thus leading to avoiding a situation that may cause or intensify the feeling of pain.5 Avoidance behaviors cause a person to withdraw from activities that may be a predicate of pain and uncomfortable situation. The cognitive avoidance model of movement suggests that when a painful experience is interpreted as threatening, it can lead to the belief that exercise will cause pain and the risk of re-injury. Over time, this can lead to avoidance behaviors that, in the long run, result in disability, disuse, and depression.4,6
Kinesiophobia is a commonly seen factor among patients with musculoskeletal pain, observed in approximately 50% of the responders.7 In another study, kinesiophobia was found in 56% of patients with chronic musculoskeletal pain occurring more frequently in men (72%) than in women (48%).8 The prevalence of kinesiophobia in persistent pain ranges from 50 to 70%.9 In elderly Polish patients with coronary artery disease over 76% of the examined patients had a high level of kinesiophobia.10
Kinesiophobia was found to be higher in stroke patients and was positively correlated with advanced age, disease duration and stroke severity.11 It was shown that the occurrence of kinesiophobia in stroke patients was quite common and it concerned even more than 80% of patients.12 In another study it was observed that patients with stroke had mild kinesiophobia, which was related to a fear of falling.13 The above-cited publications, the only ones in the available literature, show that the problem of the occurrence of kinesiophobia in patients after stroke has not been well recognized so far, and it must be admitted that learning about this phenomenon would facilitate planning the methods of effective post-stroke rehabilitation.
Not only were older post-stroke patients more susceptible to a frequent occurrence of kinesiophobia,11 but also were they more likely to have frailty syndrome.14 Frailty syndrome generally occurs in elderly people who have health problems and a progressive decline in physical function and resistance to stressogenic factors.15 Frailty was defined as a clinical syndrome in which three or more of the following criteria were present: unintentional weight loss (10 lbs in the past year), self-reported exhaustion, weakness, slow walking speed, and a low physical activity.16 The question arises whether the coexistence of frailty syndrome with stroke may intensify the phenomenon of kinesiophobia in elderly patients rehabilitated after ischemic stroke.
A fear of physical activity plays a major role in kinesiophobia4 and a fear of falling in stroke patients.13 The feeling of anxiety is a serious barrier to undertake physical rehabilitation.5,17 Elderly stroke patients had a low level of illness acceptance, which had an impact on the deterioration of their functional and emotional state causing mood disorders, which was a significant problem in rehabilitation of these patients.18
In patients after stroke, the relationship between the occurrence of kinesiophobia and the accompanying frailty syndrome, as well as the acceptance of the disease and the level of mood has not been recognized so far. The aim of this study was to determine the prevalence of kinesiophobia in elderly Polish people after ischemic stroke, including the frailty syndrome and the associations between the prevalence of kinesiophobia and feelings of anxiety and a degree of the illness acceptance.
Materials and Methods
A cross-sectional study was performed according to The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting the observational studies.19 A study was conducted from January to December 2019 at the community hospital in Wilkowice-Bystra, Poland. The sample consisting of 152 patients (76 women and 76 men, mean age - 63 years) was recruited from 185 elderly (age > 60 years) patients who had been suffering from ischemic stroke for at least 4 months. Patients were consecutively admitted to the neurological rehabilitation department. The recruitment process is presented in Figure 1.
 |
Figure 1 The recruitment process. |
The inclusion criteria for the study were: previous ischemic stroke, a mental state enabling verbal contact and understanding the survey questions, age over 60 years and an informed consent to participate in the study. The exclusion criteria were: psychosis, anemia, chronic kidney disease > stage 2, a decreased awareness, cognitive impairment suggesting moderate or severe dementia, and a negative attitude towards the study. All examined patients were qualified for post-stroke rehabilitation.
According to the data of the National Health Fund in Poland in 2018, about 30,000 patients over 60 were diagnosed with ischemic stroke.20 Based on the population size and maximum error of 8% at the confidence level of 95%, it was estimated that the sample should include a minimum of 149 individuals. Therefore, the size of the sample used in the study was deemed sufficient.
The study was approved by the independent Bioethics Committee of the Medical University of Silesia, Poland no. KNW/0022/KB/154/19. All patients were informed on the study protocol and provided informed consent to participate. The study protocol was developed in accordance with the Declaration of Helsinki.
The study used an original questionnaire to collect basic sociodemographic and clinical data. Body mass index (BMI), hemoglobin and blood glucose levels were determined and the glomerular filtration rate (eGFR) was calculated. Such standardized diagnostic tools as: the Tampa Scale of Kinesiophobia (TSK), the Tilburg Frailty Indicator (TFI), the Hospital Anxiety Depression Scale (HADS) and the Acceptance of Illness Scale (AIS) were also used.
The TSK was developed in 1991 as an assessment of fear of pain and injury caused by physical activity. This scale consists of 17 questions rated on a 4-point Likert scale. You can get from 17 to 68 points on the scale. Kinesiophobia is defined by obtaining more than 37 points.21–23 The value of Cronbach’s α coefficient of the Polish version of the questionnaire was 0.8.
The TFI is a simple diagnostic tool for the frailty syndrome. The questionnaire consists of two parts. Part A (determinants of frailty) includes questions about socio-demographic data (gender, age, marital status, country of origin, level of education and a monthly income), as well as lifestyle, the prevalence of chronic and traumatic diseases in the last year, and environmental conditions. Part B deals with the frailty component and includes questions about the three aspects of frailty. In the physical sphere, they relate to somatic health, unintentional weight loss, difficulties in moving, as well as disturbances in balance, hearing, vision, reduction of muscle strength and physical fatigue. The psychological sphere includes the assessment of cognitive disorders and a mood (4 questions), and in the social sphere, social relations and the occurrence of loneliness are assessed (3 questions). The total score is in the range of 0–15 points, with 5 being the cut-off point for the frailty syndrome.24,25 The Polish version of the questionnaire is similar to the original one in terms of the internal consistency (Cronbach’s α coefficient 0.72 vs 0.79).
The HADS is used to assess anxiety and depression in hospitalized patients. The questionnaire contains two independent subscales for the assessment of anxiety and depression; each subscale has seven items. The answers are given according to the 4-point Likert scale (0–3). The final score for each subscale is in the range of 0–21 points. Scores in the 0–7 point range are normal, the 8–10 point range indicates the cut-off level, and the 11–21 point range is considered abnormal.26,27 The values of Cronbach’s α coefficients of the subscales of anxiety and depression in the Polish version of the questionnaire were 0.815 and 0.892, respectively.
The AIS by Felton, Revenson and Hinrichsen in the Polish adaptation of Juczyński contains 8 statements identifying the negative consequences of diseases. For each of the statements, the respondents described their current health status on a 5-point scale (1- I strongly agree; 2- I agree; 3- I do not know; 4- I disagree; 5- I strongly disagree). A strong consent means a bad adaptation to the disease, while a strong opposition - full acceptance. The scope of the AIS scale ranges from 8–40 points (< 20 points – a low level of acceptance and adaptation to the disease, > 30 points – a high level of acceptance of the disease state; 20–30 points – a medium adaptation to the disease.28 The value of Cronbach’s α coefficient of the Polish version of the AIS was 0.85.
Statistical Analysis
The Shapiro–Wilk test was used to check the normality of the data distribution. The two groups were compared using the Student’s t test for the normal distribution of the variable, while groups without a normal distribution were analyzed using the Mann–Whitney U-test. The chi2 test and chi2 test with the Yates correction were used for the selected nonparametric data. In order to assess whether the analyzed parameters were predictors of dependent variables, a multiple regression analysis using the stepwise method was used. A receiver operating characteristic (ROC) curve analysis was used to evaluate the diagnostic occurrence of kinesiophobia. The area under the curve was calculated to compare the predictive value of kinesiophobia to select the patients with a frailty syndrome. The results were considered to be significant at p values < 0.05. All of the presented analyses were performed using MedCalc (MedCalc Software, Ostend, Belgium).
Results
The characteristics of post-stroke patients are presented in Table 1. In the group of patients with an ischemic stroke, kinesiophobia was demonstrated in 78.3% of patients. For the purpose of the analysis, the patients included in the study were divided into two groups: with and without kinesiophobia. The groups of patients with and without kinesiophobia were statistically comparable in terms of their age, BMI, hemoglobin and blood glucose levels, eGFR, comorbidities and time after stroke (p > 0.05). Patients with kinesiophobia had higher systolic blood pressure than patients without kinesiophobia (p < 0.01).
 |
Table 1 The Characteristics of the Stroke Patients |
The total value of TFI and the value of the anxiety and depression component of HADS were significantly higher in the group of patients with kinesiophobia compared to patients without kinesiophobia, respectively: p<0.001, p<0.001, p < 0.01. AIS values turned out to be statistically comparable in both groups of patients (p > 0.05). All the details are presented in Table 2.
 |
Table 2 The Occurrence of the Frailty Syndrome, The Level of Anxiety and Depression as Well as the Acceptance of Disease in Stroke Patients with and without Kinesiophobia |
In the multiple regression model using the stepwise input method, adjusted to age and gender, the predictors were: TFI values, especially physical and social components, the level of anxiety and depression in HADS and the value of AIS, and the dependent variable was the TSK value defining kinesiophobia. This model turned out to be statistically significant and explained 41% of the observed variance of the dependent variable (p < 0.001, R2 = 0.411). In patients with ischemic stroke, it was shown that the level of kinesiophobia increased with increasing anxiety (p < 0.001) and increasing total TFI score, ie the occurrence of the frailty syndrome (p < 0.05), and a lower level of disease acceptance (p < 0.001).
The ROC curves for the frailty syndrome predicting kinesiophobia in stroke patients are shown in Figure 2. The area under the curve was 0.807 (95% CI = 0.735–0.867). The cut-off value for the frailty syndrome was TFI > 6 (p < 0.01). The TFI is able to distinguish kinesiophobia in patients with stroke with a sensitivity of 73.7% and a specificity of 85.8%.
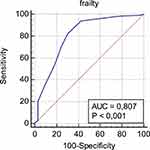 |
Figure 2 Receiver operating characteristic curves of frailty for the prediction of kinesiophobia in patients with stroke. |
Discussion
The main purpose of this study was to determine the occurrence of kinesiophobia in association with frailty syndrome in post-stroke rehabilitation elderly patients after ischemic stroke. It was shown that the occurrence of kinesiophobia in elderly people after ischemic stroke was common and was intensified in patients with accompanying frailty syndrome. As in our study, other authors have also shown a high prevalence of kinesiophobia in elderly stroke patients.11,12 According to Wasiuk-Zawada et al, the incidence of kinesiophobia varied depending on the degree of motor disability according to Rankin, including 83.3% of patients with mild disabilities and 73.1% of patients with moderate disabilities.12 In the above studies11,12 and in our study, kinesiophobia was defined on the basis of the TSK criterion, which allowed for a comparative analysis of the frequency of this phenomenon, which turned out to be high in the majority of stroke patients in studies from various centers. One of these studies included post-stroke patients in Poland.12 The problem of kinesiophobia was also assessed in other neurological diseases, such as Parkinson’s disease12,29,30 and a multiple sclerosis.12,31 In these diseases, similarly to stroke, the level of kinesiophobia increased in comparison to the results obtained in the persons from the control groups.
The literature review shows that the problem of kinesiophobia in diseases of the central nervous system, especially following a stroke, has not been recognized so far. Factors determining the development of kinesiophobia and the mechanisms of this development in post-stroke brain injury have not been elucidated. The relationship between the occurrence of kinesiophobia in post-stroke patients and the examined factors proved inconclusive. In the above-cited study12 it was shown that kinesiophobia in patients with stroke was related to age and self-assessment of fitness and not related to the intensity of pain and the duration of the disease. In another study, an increased incidence of kinesiophobia in stroke patients was positively correlated with advanced age, disease duration and stroke severity.11 Moreover, it was observed that post-stroke kinesiophobia was related to a fear of falling.13 Our observations show that the intensity of kinesiophobia in patients with stroke showed correlation with a higher level of anxiety assessed with the use of HADS, higher TFI value for the frailty syndrome, and a low level of acceptance of their disease. Based on our study and other authors’ results,11–13 it can be concluded that the factors and probably the mechanisms determining the development of kinesiophobia in patients after stroke are diverse. The elucidation of these relationships in terms of the pathomechanism of kinesiophobia in patients after stroke requires further in-depth research.
The coexistence of the frailty syndrome with stroke has been the subject of many studies. In an extensive meta-analysis, Palmer et al showed that the prevalence of pre-frailty and frailty syndrome in people with stroke was on average among 49% and 22% of patients, respectively.14 In these patients with a stroke, the frailty syndrome occurred twice as often as in the population of people without a stroke. These results may have clinical implications, as they identify the need to assess frailty in post-stroke survivors and assess how it may affect prognosis. Better quality, longitudinal research that examines the temporal relationship between stroke and frailty, as well as studies on other types of cerebrovascular diseases are needed.14 The authors’ research showed that the occurrence of the frailty syndrome among people with stroke was more common in patients with kinesiophobia than in those without kinesiophobia. The percentage of people with frailty syndrome among patients with kinesiophobia was 1.5 times higher than among patients without kinesiophobia. According to Fried et al, frailty syndrome includes such symptoms as self-reported exhaustion, weakness, slow walking speed, and a low physical activity.16 The combination of such symptoms with stroke can lead to the development of kinesiophobia. Based on the determined ROC curve for the frailty syndrome in the prognosis of kinesiophobia in patients with stroke, it can be predicted that obtaining more than 6 points on the TFI scale will result in the occurrence of kinesiophobia. In another study evaluating the association of the frailty syndrome with kinesiophobia in elderly patients after cardiac surgery treatment of coronary artery bypass surgery, the effect of this syndrome on the intensity of kinesiophobia was not observed, which was associated with a lower level of fear of physical activity.32 The fact of the presence of severe kinesiophobia in our patients with the frailty syndrome accompanying stroke requires special attention due to the recommended need for physical rehabilitation in these patients.
Our observations show that the intensity of kinesiophobia in patients with stroke showed correlation with a higher level of anxiety. In a clinical setting, anxiety has been recognized as an important aspect of patients’ disability that must be addressed, as it influences rehabilitation strategies.5,17 Based on the anxiety avoidance model,4 when pain is perceived as threatening, it can develop anxiety related to this pain, leading in turn to avoidance behaviors. Avoidance behavior is a state in which a person withdraws from many activities that are associated with high levels of pain. Then, avoidance behavior as an adaptation to pain in the long run would lead to disability and a depression.6
In the elderly, the consequences of reduced activity can be severe, increasing the risk of a wide variety of health problems, functional deterioration, and premature death.4–6 Several studies33,34 confirm the validity of the cognitive model of anxiety avoidance among the elderly.35–37
As it is believed that kinesiophobia has a negative impact on the results of rehabilitation, this phenomenon should be taken into account in every clinical situation. A psychological management strategy that may be helpful in reducing pain and kinesiophobia is a cognitive behavioral therapy.38,39 This therapy may be effective in reducing the anxiety associated with pain, thereby reducing pain and improving motor function. Cognitive behavioral therapy includes cognitive recovery, relaxation training, deep breathing exercises, active involvement in distraction activities to modify and/or reduce the impact of pain and physical and psychosocial disabilities, and overcome barriers to physical and psychosocial recovery.40
Limitations
The work covers the occurrence of kinesiophobia only in the elderly people with ischemic stroke. Introducing younger patients to the research would broaden the horizon of this phenomenon in post-stroke patients. The studies were not conducted in the whole population of patients after stroke, as the more severely ill people with disabilities were necessarily excluded. Moreover, the groups of patients with and without kinesiophobia compared in the studies differed significantly in terms of the number of patients. The study did not take into account the psychological treatment of patients qualified for post-stroke rehabilitation. From the current observation it can be concluded that such a procedure was not carried out professionally, especially targeting patients with the problem of kinesiophobia. Another limitation is not checking the post-stroke recovery status using, for example, the Brunnstrom stages.
Conclusions
1. The occurrence of kinesiophobia in elderly Polish people after ischemic stroke is common and the determinants of its development are the coexistence of the frailty syndrome, anxiety and a low level of illness acceptance. 2. In post-stroke patients, the presence of kinesiophobia should be considered, especially in the situation of comorbid frailty syndrome. 3. The issue of kinesiophobia in patients after stroke requires further in-depth research, especially in the field of cognitive-behavioral prevention aimed at ways to reduce this phenomenon.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528. doi:10.1161/CIR.0000000000000659
2. Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet. 2011;377(9778):1693–1702. doi:10.1016/S0140-6736(11)60325-5
3. Saunders DH, Greig CA, Mead GE. Physical activity and exercise after stroke: review of multiple meaningful benefits. Stroke. 2014;45:3742–3747. doi:10.1161/STROKEAHA.114.004311
4. Kori SH, Miller RP, Todd DD. Kinesophobia: a new view of chronic pain behavior. Pain Manag. 1990;3:35–43.
5. Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. doi:10.1016/s0304-3959(99)00242-0
6. Vlaeyen JW, Kole-Snijders AM, Rotteveel AM, Ruesink R, Heuts PH. The role of fear of movement (re)injury in pain disability. J Occup Rehabil. 1995;5(4):235–252. doi:10.1007/BF02109988
7. Lundberg M, Larsson M, Östlund H, Styf J. Kinesiophobia among patients with musculoskeletal pain in primary healthcare. J Rehabil Med. 2006;38:37–43. doi:10.1080/16501970510041253
8. Bränström H, Fahlström M. Kinesiophobia in patients with chronic musculoskeletal pain: differences between men and women. J Rehabil Med. 2008;40(5):375–380. doi:10.2340/16501977-0186
9. Luque-Suarez A, Martinez-Calderon J, Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J Sports Med. 2019;53:554–559. doi:10.1136/bjsports-2017-098673
10. Knapik A, Dąbek J, Brzęk A. Kinesiophobia as a problem in adherence to physical activity recommendations in elderly polish patients with coronary artery disease. Patient Prefer Adherence. 2019;13:2129–2135. doi:10.2147/PPA.S216196
11. Koca TT, Gülkesen A, Nacitarhan V, Koca Ö. Does kinesiophobia associated with poststroke neuropathic pain and stroke severity? J PMR Sci. 2019;22(2):60–65. doi:10.31609/jpmrs.2019-66862
12. Wasiuk-Zowada D, Knapik A, Szefler-Derela J, Brzęk A, Krzystanek E. Kinesiophobia in stroke patients, multiple sclerosis and Parkinson’s disesase. Diagnostics. 2021;11:796. doi:10.3390/diagnostics11050796
13. Jo S, Choi W, Jung J, Park J, Lee S. Convergence study on the relationship between kinesiophobia and fear of falling in patients with stroke. J Korea Convergence Soc. 2019;10(10):33–41. doi:10.15207/JKCS.2019.10.10.033
14. Palmer K, Vetrano DL, Padua L, et al. Frailty syndromes in persons with cerebrovascular disease: a systematic review and meta-analysis. Front Neurol. 2019;29(10):1255. doi:10.3389/fneur.2019.01255
15. Rockwood K. What would make a definition of frailty successful? Age Aging. 2005;34:432–434. doi:10.1093/ageing/afi146
16. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56(3):46–56. doi:10.1093/gerona/56.3.m146
17. Lundberg M, Grimby-Ekman A, Verbunt J, Simmonds MJ. Pain-related fear: a critical review of the related measures. Pain Res Treat. 2011;2011:494196. doi:10.1155/2011/494196.494196
18. Guzek Z, Kowalska J. Analysis of the degree of acceptance of illness among patients after a stroke: an Observational Study. Clin Interv Aging. 2020;15:2063–2072. doi:10.2147/CIA.S268095
19. Vandenbroucke JP, von Elm E, Altman DG, et al. STROBE initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–1524. doi:10.1016/j.ijsu.2014.07.014
20. National Health Fund of health. Ischemic stroke of the brain. Warsaw, [Raport] Headquarters of the National Health Fund Department of Analysis and Strategy ISBN: 978-82-944034-3-0; 2019.
21. Miller RP, Kori S, Todd D. The tampa scale: a measure of kinesiophobia. Clin J Pain. 1991;7(1):51–52. doi:10.1097/00002508-199103000-00053
22. Lundberg M, Styf J, Carlsson S. A psychometric evaluation of the Tampa Scale for Kinesiophobia – from a physiotherapeutic perspective. Physiother Theory Pract. 2004;20:121–133. doi:10.1080/09593980490453002
23. Misterska E, Jankowski R, Głowacki J, Shadi M, Walczak M, Głowacki M. Kinesiophobia in pre-operative patients with cervical discopathy and coexisting degenerative changes in relation to pain-related variables, psychological state and sports activity. Med Sci Monit. 2015;21:181–194. doi:10.12659/MSM.891045
24. Gobbens R, van Assen M, Luijkx K, Wijnen-Sponselee M, Schols J. The Tilburg frailty indicator: psychometric properties. J Am Med Dir Assoc. 2010;11:344–355. doi:10.1016/j.jamda.2009.11.003
25. Uchmanowicz I, Gobbens R, Jankowska-Polanska B, Loboz-Rudnicka M, Manulik S, Loboz-Grudzien K. Cross-cultural adaptation and reliability testing of the Tilburg Frailty Indicator for optimizing care of Polish patients with frailty syndrome. Clin Interv Aging. 2014;9:997–1001. doi:10.2147/CIA.S64853
26. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
27. Majkowicz M. Practical assessment of the effectiveness of palliative care - selected research techniques. In: De Walden-gałuszko K, Majkowicz M, editors. Assessment of the Quality of Palliative Care in Theory and Practice. Gdańsk: Akademia Medyczna Gdańsk, Zakład Medycyny Paliatywnej; 2000:21–42.
28. Felton BJ, Revenson TA. Coping with chronic illness: a study of illness controllability and the influence of coping strategies on psychological adjustment. J Consult Clin Psychol. 1984;52:343–353. doi:10.1037/0022-006X.52.3.343
29. Jiménez-Cebrián AM, Becerro-de-bengoa-vallejo R, Losa-Iglesias ME, et al. Kinesiophobia levels in patients with parkinson’s disease: a case-control investigation. Int J Environ Res Public Health. 2021;18:4791. doi:10.3390/ijerph18094791
30. Monticone M, Ferrante S, Ambrosini E, Rocca B, Secci C, Foti C. Development of the Tampa scale of kinesiophobia for Parkinson’s disease: confirmatory factor analysis, reliability, validity and sensitivity to change. Int J Rehabil Res. 2015;38:113–120. doi:10.1097/MRR.0000000000000095
31. Kahraman T, Ozdogar A, Yigi P, et al. Feasibility of a 6-month yoga program to improve the physical and psychosocial status of persons with multiple sclerosis and their family members. Explore. 2018;14:36–43. doi:10.1016/j.explore.2017.07.006
32. Kluszczyńska M, Młynarska A, Mikulakova W. Influence of frailty syndrome on kinesiophobia according to the gender of patients after coronary artery bypass surgery. Healthcare. 2021;9:730. doi:10.3390/healthcare9060730
33. Kovacs F, Noguera J, Abraira V, et al. The influence of psychological factors on low back pain-related disability in community dwelling older persons. Pain Med. 2008;9(7):871–880. doi:10.1111/j.1526-4637.2008.00518.x
34. Basler HD, Luckmann J, Wolf U, Quint S. Fear-avoidance beliefs, physical activity, and disability in elderly individuals with chronic low back pain and healthy controls. Clin J Pain. 2008;24(7):604–610. doi:10.1097/AJP.0b013e31816b54f6
35. Ledoux E, Dubois JD, Descarreaux M. Physical and psychosocial predictors of functional trunk capacity in older adults with and without low back pain. J Manipulative Physiol Ther. 2012;35(5):338–345. doi:10.1016/j.jmpt.2012.04.007
36. Raftery MN, Sarma K, Murphy AW, De la Harpe D, Normand C, McGuire BE. Chronic pain in the Republic of Ireland - community prevalence, psychosocial profile and predictors of pain-related disability: results from the Prevalence, Impact and Cost of Chronic Pain (PRIME) study, Part 1. Pain. 2011;152(5):1096–1103. doi:10.1016/j.pain.2011.01.019
37. Pereira LV, de Vasconcelos PP, Souza LAF, Pereira Gde A, Nakatani AYK, Bachion MM. Prevalence and intensity of chronic pain and self-perceived health among elderly people: a population-based study. Rev Lat Am Enfermagem. 2014;22(4):662–669. doi:10.1590/0104-1169.3591.2465
38. Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80:329–339. doi:10.1016/S0304-3959(98)00229-2
39. Verbunt JA, Westerterp KR, van der Heijden GJ, et al. Physical activity in daily life in patients with chronic low back pain. Arch Phys Med Rehabil. 2001;82:726–730. doi:10.1053/apmr.2001.23182
40. Chung OY, Bruehl SP. Complex regional pain syndrome. Curr Treat Options Neurol. 2003;5:499–511. doi:10.1007/s11940-996-0018-6
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
