Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Investigation of the Methodology of Specific Airway Resistance Measurements in COPD
Received 6 June 2023
Accepted for publication 1 October 2023
Published 13 November 2023 Volume 2023:18 Pages 2555—2563
DOI https://doi.org/10.2147/COPD.S424696
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
James Dean,1,2,* Dave Singh1,2,*
1Division of Infection, Immunity and Respiratory Medicine, School of Biological Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester University NHS Foundation Trust, Manchester, UK; 2Medicines Evaluation Unit, Manchester, UK
*These authors contributed equally to this work
Correspondence: James Dean, Medicines Evaluation Unit, Southmoor Road, Manchester, M23 9QZ, UK, Tel +44 (0)161 946 4081, Fax +44(0)161 946 1459, Email [email protected]
Introduction: Specific resistance (SRaw) measurements in Chronic Obstructive Pulmonary Disease (COPD) patients may be performed by panting or tidal breathing. The aim of this study was to compare how breathing frequency affected SRaw in COPD and compare different tangent plotting methods.
Methods: Fifteen COPD patients participated. Three protocols were performed: tidal 1 – spontaneous tidal breathing; tidal 2 – tidal breathing with a flow of ± 1 L/sec; panting – 60 breaths per min. Effective (SReff), total (SRtot), ± 0.5 L/s (SR0.5), and mid (SRmid) specific resistance were assessed.
Results: The tidal breathing protocols provided similar results. Panting resulted in higher SReff (p = 0.0002) and SRtot (p < 0.0001) versus tidal breathing, but not SR0.5 or SRmid. Breathing frequency did not affect intra-test variance. SReff and SRtot measurements were similar, and were higher than SR0.5, during tidal breathing (p = 0.0014 and p < 0.0001 respectively) and panting (p = 0.0179 and p < 0.0001 respectively). SRtot was higher than SRmid during tidal breathing (p < 0.0001) and panting (p < 0.0001). Intra-test variance of SReff and SRtot were similar and showed the lowest percent coefficient of variation during both tidal breathing and panting.
Conclusion: Panting and tidal breathing manoeuvres are not interchangeable in COPD patients. Panting widens the clubbing in the SRaw loop. SR0.5 and SRmid may underestimate abnormal physiology in COPD.
Plain Language Summary: The effort to breathe can be measured as specific airway resistance (SRaw), which is a measure of the airflow that a person can achieve. SRaw is calculated from a plotted loop, but may be affected by the way that the test is performed and calculated. SRaw can be measured during panting or tidal breathing, and can be calculated using different methods of plotting the SRaw slope. In COPD patients, we found that panting SRaw is higher than during tidal breathing, and the calculation methods that use the extremities of the SRaw loop give higher values and have the lowest variability.
Keywords: specific resistance, COPD, panting, tidal, plethysmography
Introduction
Body plethysmography is a well-established pulmonary function test, allowing measurement of specific airway resistance (SRaw). This sensitive method allows small changes in airway function to be measured. Resistance measurements have been used in clinical trials to evaluate drug effects,1 and are often used in clinical practice as part of routine pulmonary function testing in chronic obstructive pulmonary disease (COPD). Different methodologies exist for measuring SRaw in COPD.2
SRaw is calculated by plotting a tangent line through data from a breathing cycle, where airflow is plotted on the y-axis and shift volume on the x-axis, the latter being the change in volume within the plethysmograph caused by compression and rarefaction of thoracic gas.2 SRaw is the reciprocal gradient of the tangent line. This can be measured using either tidal breathing or panting, and can be affected by thermo-hygrometric artefact arising from inspiration of ambient air and exhalation of warm humid air.3 Shallow panting reduces this artefact by minimising the temperature difference between inspired and expired air,4 while also reducing upper airway resistance.5 Electronic compensation removes artefact during tidal breathing by reducing temperature effects on box volume, artificially closing the SRaw loops.3 Tidal breathing is also considered easier to perform and increases the chance of a successful test.6 In obstructive lung conditions the loop becomes more horizontal and non-uniform (opening at the expiratory part of the loop).7 Some COPD patients may find it difficult to pant during the manoeuvre, and it is important to determine whether there are differences between tidal breathing and panting in terms of SRaw loop shape.
Different SRaw calculation methods previously described are illustrated in Figure 1:3 effective SRaw (SReff) which utilises least squares regression of all the points in the loop; total SRaw (SRtot) which is plotted through the extremes of the x-axis loop values (thus defining the greatest shift volume); 0.5 L/s SRaw and mid SRaw, plotted through a flow of ± 0.5 L/s (y-axis) on the right side of the loop (SR0.5) or through the centre of the loop (SRmid). SReff and SRtot may result in lower tangent gradients (ie flatter loops) and higher SRaw values as they utilise the extremities of the loop, rather than just the portion between ±0.5 L/s.
COPD SRaw loops have a different shape compared to healthy subjects.7 It is therefore relevant to investigate whether the breathing technique used or the method of SRaw tangent plot influence the results obtained in COPD patients. The aim of this study was to investigate methodological aspects that may cause variability in SRaw measurements in COPD patients; first by comparing panting versus tidal breathing and second by comparing results obtained using different tangent plotting methods.
Methods
Sixteen COPD patients were recruited with post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio <0.7, ≥10 pack year smoking history, and no history of asthma. All patients were free from exacerbation within the preceding 6 weeks, and provided written informed consent using a protocol that complies with the Declaration of Helsinki, approved by the Greater Manchester East Research Ethics Committee (North West: 05/Q1402/41).
Patients performed plethysmography with the following breathing protocols, in a randomised order; tidal protocol 1 – spontaneous tidal breathing; tidal protocol 2 – tidal breathing with a flow of at least ±1 L/sec (augmented flow without change in breathing frequency); panting protocol – panting to approximately 60 breaths per minute (1 Hz). Tidal protocol 2 was included in case spontaneous tidal breathing (ie tidal protocol 1) did not achieve flows of 0.5 L/s, as required to accurately plot the tangents of SR0.5 and SRmid. Lung volumes were also measured (see Supplement and Figure S1). Testing was performed on the Vyntus Body system (Vyaire, Hoechberg, Germany). For tidal breathing protocols, thermo-hygrometric compensation was applied automatically by the device. SReff, SRtot, SR0.5 and SRmid were calculated automatically by the device software, using loops that were considered consistent by the operator. Spirometry (NDD, Zurich, Switzerland) was measured in accordance with ATS/ERS standards,8 and the COPD assessment test (CAT) and modified medical research council dyspnoea scale (mMRC) questionnaires were administered. All lung function measurements were performed post-bronchodilator to protect against altered airway calibre from repeated testing, maintaining consistency between tidal and panting protocols.
A sample size of 15 subjects was considered sufficient for a within-subject analysis. The median value from 5 consecutive SRaw loops was reported, using the same loops for each method of plotting the SRaw tangent. Intra-test variance of each method was calculated as percent coefficient of variation (CoV) of these 5 loops. Data was assessed for normal distribution using D’Agostino & Pearson omnibus normality test, with any data sets containing non-normally distributed data assessed using non-parametric test. Comparisons between tidal breathing and panting was assessed using the Wilcoxon matched-pairs signed rank test for SRaw values, and paired t-test for SRaw CoV. Comparisons between the methods of plotting SRaw tangents was assessed using the Friedman test with Dunn’s multiple comparison test, adjusted for multiplicity. Analysis was performed using Prism 9 (GraphPad, CA, USA). P values <0.05 were considered statistically significant.
Results
Of the 16 COPD patients recruited, one patient was unable to tolerate occlusion during plethysmography, so was excluded from the analysis. Patient characteristics are shown in Table 1. The majority of patients were male and former smokers, from across all GOLD stages (FEV1 range: 28–98% predicted), with mean CAT score 16.
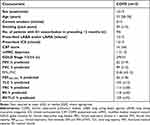 |
Table 1 Patient Characteristics |
No significant differences existed between the tidal protocol 1 and the panting protocol for lung volumes (see Supplement and Table S1). There was no difference in SRaw values between the two tidal breathing protocols (see Supplement and Table S2), so only data from spontaneous tidal breathing (tidal protocol 1) and panting (protocol 3) are presented. Figure 2 shows example SRaw loops for two COPD patients during tidal breathing and panting. Clubbing at the bottom of the loop, during expiration, was common during panting, but slightly less so during tidal breathing (Figure 2A). Visual inspection showed that 11 subjects had some evidence of clubbing during both tidal breathing and panting, and 4 subjects only during panting, although no objective definition exists for clubbing. In some but not all COPD patients, flattening at the top of the panting loop was noticed, indicating upper airway obstruction during inspiration (Figure 2B).
Comparisons between tidal breathing and panting are shown in Figure 3. Panting resulted in higher SReff and SRtot (p = 0.0002 and p < 0.0001 respectively), but not SR0.5 or SRmid (p = 0.15 and p = 0.76 respectively). Breathing frequency (ie tidal or panting) did not affect intra-test variance.
Comparisons between the methods of plotting SRaw tangents are shown in Figure 4. SReff and SRtot measurements were similar, and both produced higher values than SR0.5, during tidal breathing (p = 0.0014 and p < 0.0001 respectively) and panting (p = 0.0179 and p < 0.0001 respectively). SRtot was also higher than SRmid during tidal breathing (p < 0.0001) and panting (p < 0.0001). There were no differences between SR0.5 and SRmid.
 |
Figure 4 (A) Tidal SRaw values; (B) Tidal SRaw CoV; (C) Panting SRaw values; (D) Panting SRaw CoV. SRaw values are plotted as median (IQR) and CoV as mean (95% CI). *p<0.05; **p<0.01; ****p<0.0001. |
Comparison of the variance of the different SRaw tangents is shown in Figure 4. SReff and SRtot variance was similar and showed the lowest CoV. SR0.5 and SRmid were similar with significantly higher CoV compared to SReff and SRtot, during both tidal breathing and panting.
Discussion
A major finding was that panting in COPD patients resulted in higher SRaw values compared to tidal breathing when using SReff and SRtot. It was also observed that SReff and SRtot values were higher than SR0.5 and SRmid during both tidal breathing and panting. SR0.5 and SRmid provided the lowest median values but also displayed the highest intra-test variance. Clubbing of SRaw loops is common in COPD; this study provides new information quantifying the differences in values obtained when different tangent plotting methods are applied to COPD SRaw loops. The results highlight significant differences that can exist for SRaw values in COPD patients due to either breathing frequency or the method of tangent plotting.
Tidal breathing SRaw values are known to be higher than panting values in healthy children9 and adults,5 which is likely due to a dilation effect of panting on structures in the extrathoracic airways.10 Panting therefore has a methodological benefit in reducing upper airway resistance. However, we observed higher SRaw values during panting in COPD compared to tidal breathing, which suggests that upper airway resistance does not constitute a significant component of total resistance in COPD. Upper airway resistance has been reported to represent half of the resistance in healthy volunteers, but only approximately 20% of airway resistance in emphysema.11 Although panting is expected to reduce upper airway resistance, it appears that panting caused increased intrathoracic airway resistance in COPD, resulting in greater total airway resistance compared to tidal breathing. This can be seen by the widening of the expiratory part of the loop during panting, in addition to flattening of the whole loop (Figure 2). The mechanism by which panting increases SRaw values in COPD was not assessed here, but it is likely to result from a greater contribution of turbulent flow to airway resistance.12 Additionally, panting is likely to expose the distensible airways to increased pressure fluctuations, which combined with airway collapsibility in COPD patients can cause dynamic compression13 and increased expiratory resistance.2 Although tidal breathing may result in greater extrathoracic airway resistance compared to panting, it is unlikely to do so in all COPD patients,14 and will be outweighed by the increased airway resistance from intrathoracic airway narrowing.15 We found evidence that panting induced a degree of upper airway obstruction in some COPD patients, as shown by flattening of the top of the SRaw loop12 (Figure 2B). This is the opposite of what is expected when panting (ie dilation of upper airway structures) and may be explained by increased upper airway obstruction16 and collapsibility17 in COPD patients.
Visually, the effect of panting in COPD patients can be seen as the characteristic clubbing at the bottom of the SRaw loop (Figure 2). SReff and SRtot include the extremities of the SRaw loop, which during panting was found to create more “clubbing” and a flatter tangent gradient. SR0.5 and SRmid represent the middle portion of the loop, where the gradient may be comparable between panting and tidal breathing. It is likely that SR0.5 and SRmid are less sensitive to the changes in the loop caused by panting in COPD patients. The extremities of the loop may represent elastance in the peripheral airways, whereas the middle portion of the loop may be sensitive to resistance of central airways,18 meaning that the different SRaw plotting measurements may evaluate different parts of the airways. The various patterns of looping, and its dependency on breathing frequency, may indicate that the relative contributions of distal and proximal airway disease to the SRaw value are not always fixed.
We found that SReff and SRtot were also higher than SR0.5 and SRmid at tidal breathing frequencies, due to the extremities of the SRaw loop. This likely represents an important disease abnormality, indicating increased shift volume during expiration. Shift volume refers to the deviation during inspiration or expiration from the corresponding volume in the breath cycle if alveolar and box pressure were equal (ie volume if the patient were to hold their breath).12 Physiologically this means that as a COPD patient exhales, expiratory flow lags behind the pressure generated to create it, more so than would be expected compared to a healthy individual, indicating a greater work of breathing.
The abnormality seen in the SRaw loop of a COPD patient may result from expiratory flow limitation (EFL), which is a phenomenon where choke points form in the intrathoracic airways during tidal exhalation.1,19–21 Diminished elastic recoil and airway remodelling in these patients contribute to airway narrowing that occurs earlier during exhalation, and results in gas trapping and ventilation inhomogeneity. This can be seen as an asymmetry between the inspiratory and expiratory parts of the SRaw loop. During exhalation, EFL develops flow irregularities as the airways become narrower, which is likely to contribute to the phase shift between flow and shift volume, and the open “clubbing” seen during the expiratory part of the SRaw loop. A close relationship has been reported between clubbing of flow-alveolar pressure loops (derived from tidal SRaw loop data) and EFL in COPD patients during resting breathing.22 Panting worsened the clubbing in some of our COPD patients, and additional work is required to investigate the relationship between resistance loop clubbing and markers of EFL in COPD.
SReff and SRtot values are more dependent on breathing frequency than SR0.5 and SRmid, as shown by higher panting values in the former when compared to tidal breathing. During panting, both flow and breathing frequency increase, similar to exercise but without the increase in tidal volume. This may suggest panting simulates some of the ventilatory changes that occur during exercise, while tidal breathing reflects resting ventilatory mechanics in COPD patients, although this speculation remains to be proven. During exercise, ventilation is firstly increased by increasing tidal volume, followed by increasing breathing frequency.23 In health, increases in lung volume above functional residual capacity (FRC) lead to a reduction in airway resistance,24 suggesting volume increases are unlikely to account for our results. However, increases in breathing frequency result in greater resistance during expiration in COPD patients, which may be linked to breathlessness.25 It is likely that EFL is not present during rest in some patients, but develops when panting, causing expiratory clubbing of the SRaw loop and greater SReff and SRtot values. As it is only possible to quantify SRaw before and after exercise, we speculate that panting manoeuvres may be alternative method to identify COPD patients who are at risk of developing EFL upon increased ventilation.
The intra-test variability of each measurement was not affected by breathing frequency, but was influenced by the method of SRaw tangent plotting. SReff and SRtot had considerably lower variance than SR0.5 and SRmid, so may be more sensitive to small changes in lung function, and therefore have greater clinical utility in monitoring disease progression or therapeutic intervention. No significant difference in variability was found between SReff and SRtot. SReff uses more data points which will theoretically reduce the impact of changes in maximum shift volume between loops, caused by either artifact, changes in breathing frequency, or changes in flow. Conversely it could be argued that SRtot is more likely to be affected by clubbing of the loop than SReff, and therefore is a more physiologically representative measure of SRaw. These differences are likely to be minor in most settings.
It has been suggested that a tidal breathing manoeuvre will increase the likelihood of a successful test in children.26 We found that COPD patients were able to perform acceptable SRaw measurements, and volume of thoracic gas (VTG) measurements during occlusion, both in panting and tidal breathing manoeuvres. Although SRaw values were frequency dependent, lung volumes were not, as FRC was reported as the volume at the end of baseline tidal breathing, and not the volume during occlusion (ie VTG). Our study was limited to 15 patients, only one of which was classified as very severe (GOLD stage 4). It is possible that patients with more severe airflow obstruction would not tolerate panting manoeuvres and would prefer tidal breathing.
This study investigated the variability due to SRaw methodology in COPD patients. The sample size was too small to robustly investigate associations with other lung function characteristics, such as hyperinflation and EFL, or clinical characteristics, as such analysis require larger sample sizes to evaluate differences between individuals. The current analysis focused on within subject comparisons, enabling clear differences due to methodology to be demonstrated even with a limited sample size.
It is useful to consider the role of SRaw in the management of COPD patients, and the potential clinical implications of our results. FEV1 is used for COPD diagnosis and severity assessment (GOLD stage 1–4), and is a prognostic marker.27,28 However, FEV1 reflects the physiology of the proximal airways rather than the distal lung where significant small airway dysfunction exists in COPD.29 SRaw measurements require more complex equipment, but can provide unique information on airway mechanics which also includes the distal lung.3 Body plethysmography measurements of airway resistance and conductance are more sensitive than FEV1 for measuring the effects of pharmacological interventions in COPD patients,1,30,31 and so can have utility for longitudinal monitoring to assess inhaled treatments. Additionally, the differences identified here between tidal breathing and panting could potentially be used to identify individuals with breathing frequency dependent changes in airway mechanics. Further work is needed in a larger cohort to understand the relationship of SRaw to symptoms, exercise performance, and clinical outcomes. The contribution of airflow obstruction and hyperinflation to SRaw changes also needs to be better understood.
In conclusion, panting and tidal breathing manoeuvres are not interchangeable in COPD patients. Panting widens the “clubbing” seen in the SRaw loop, and therefore may increase the magnitude of abnormal physiology measured in COPD patients. Tidal breathing is a suitable method to assess COPD patients in a rested state, and perhaps both methods can be applied in COPD patients but require different interpretation. COPD patients with breathing frequency dependent airway resistance may be identified by comparing panting and tidal SRaw values. SReff and SRtot have higher median values and lower variability. Considering that clubbing in the SRaw loop is physiologically relevant in COPD patients, SR0.5 and SRmid may underestimate abnormal physiology in COPD.
Abbreviations
SRaw, specific airway resistance; COPD, chronic obstructive pulmonary disease; SReff, effective specific resistance; SRtot, total specific resistance; SR0.5, specific airway resistance at a flow of ±0.5 L/s; SRmid, specific airway resistance at a flow of ±0.5 L/s through the middle of the loop; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; Hz, hertz; ATS, American thoracic society; ERS, European respiratory society; CAT, COPD Assessment Test; mMRC, Modified Medical Research Council dyspnoea scale; CoV, percent coefficient of variation; GOLD, Global Initiative for Chronic Obstructive Lung Disease; EFL, expiratory flow limitation; FRC, functional residual capacity; IOS, Impulse Oscillometry; VTG, volume of thoracic gas; Vol, Volume; LABA, long acting beta2 agonist; LAMA, long acting muscarinic antagonist; ICS, Inhaled Corticosteroid; FEF25%-75%, forced expiratory flow between 25% and 75% of FVC; SD, standard deviation; IQR, Interquartile range; TLC, total lung capacity; RV, residual volume; CI, confidence interval.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Patient Consent
All patients provided written informed consent using a protocol approved by Greater Manchester East Research Ethics Committee (North West: 05/Q1402/41).
Acknowledgments
The authors would like to thank Leanne Archer and Natalie Jackson (Medicines Evaluation Unit, Manchester, UK) for their assistance during data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was funded by the Medicines Evaluation Unit.
Disclosure
JD declares no competing interests in this work. DS has received personal fees from Aerogen, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, CSL Behring, Epidendo, Genentech, GlaxoSmithKline, Glenmark, Gossamerbio, Kinaset, Menarini, Novartis, Orion, Pulmatrix, Sanofi, Synairgen, Teva, Theravance and Verona.
References
1. Dean J, Panainte C, Khan N, Singh D. The TRIFLOW study: a randomised, cross-over study evaluating the effects of extrafine beclometasone/formoterol/glycopyrronium on gas trapping in COPD. Respir Res. 2020;21:21. doi:10.1186/s12931-020-1278-5
2. Beardsmore CS. Chapter 5: plethysmography. Eur Respir Mon. 2010;47:66–86.
3. Goldman MD, Smith HJ, Ulmer WT. Chapter 2: whole-body plethysmography. Eur Respir Mon. 2005;31:15–43.
4. DuBois AB, Botelho SY, Comroe JH. A new method for measuring airway resistance in man using a body plethysmography: values in normal subjects and in patients with respiratory disease. J Clin Invest. 1956;35:327–335. doi:10.1172/JCI103282
5. Krell WS, Agrawal KP, Hyatt RE. Quiet-breathing vs. panting methods for determination of specific airway conductance. J Appl Physiol. 1984;57:1917–1922. doi:10.1152/jappl.1984.57.6.1917
6. Coutier L, Stouvenot M, Ioan I, et al. Specific airway resistance in preschool children: panting vs tidal breathing. Eur Respir J. 2014;44:1157.
7. Topalovic M, Exadaktylos V, Troosters T, Celis G, Aerts JM, Janssens W. Non-Linear parameters of specific resistance loops to characterise obstructive airways diseases. Respir Res. 2017;18(9). doi:10.1186/s12931-016-0484-7
8. Graham BL, Steenbruggen I, Miller MR, et al. Standardization of Spirometry 2019 update: an official American thoracic society and European respiratory society technical statement. Am J Respir Crit Care Med. 2019;200(8):e70–e88. doi:10.1164/rccm.201908-1590ST
9. Kirkby J, Stanojevic S, Welsh L, et al. Reference equations for specific airway resistance in children: the Asthma UK initiative. Eur Respir J. 2010;36:622–629. doi:10.1183/09031936.00135909
10. Spann RW, Hyatt RE. Factors affecting upper airways resistance in conscious man. J Appl Physiol. 1971;31:708–712. doi:10.1152/jappl.1971.31.5.708
11. Hyatt RE, Wilcox RE. Extrathoracic airway resistance in man. J Appl Physiol. 1961;16:326–330. doi:10.1152/jappl.1961.16.2.326
12. Criee CP, Sorichter S, Smith HJ, et al. Body plethysmography - Its principles and clinical use. Respir Med. 2011;105:959–971. doi:10.1016/j.rmed.2011.02.006
13. Santus P, Radovanovic D, Henchi S, et al. Assessment of acute bronchodilator effects from specific airway resistance changes in stable COPD patients. Respir Physiol Neurobiol. 2014;197:36–45. doi:10.1016/j.resp.2014.03.012
14. Higenbottam T, Payne J. Glottis narrowing in lung disease. Am Rev Respir Dis. 1982;125:746–750. doi:10.1164/arrd.1982.125.6.746
15. Sekizawa K, Sasaki H, Takishima T. Laryngeal resistance immediately after panting in control and constricted airways. J Appl Physiol. 1985;58:1164–1169. doi:10.1152/jappl.1985.58.4.1164
16. van Noord J, Wellens W, Clarysse I, Cauberghs M, Van de Woestijne KP, Demedts M. Total respiratory resistance and reactance in patients with upper airway obstruction. Chest. 1987;92:475–480. doi:10.1378/chest.92.3.475
17. Biselli P, Grossman P, Kirkness J, et al. The effect of increased lung volume in chronic obstructive pulmonary disease on upper airway obstruction during sleep. J Appl Physiol. 2015;119:266–271. doi:10.1152/japplphysiol.00455.2014
18. Mahut B, Caumont-Prim A, Plantier L, et al. Relationships between respiratory and airway resistances and activity-related dyspnea in patients with chronic obstructive pulmonary disease. Int J COPD. 2012;7:165–171.
19. Dean J, Kolsum U, Hitchen P, Gupta V, Singh D. Clinical characteristics of COPD patients with tidal expiratory flow limitation. Int J COPD. 2017;12:1503–1506. doi:10.2147/COPD.S137865
20. Beech A, Jackson N, Dean J, Singh D. Expiratory flow limitation in a cohort of highly symptomatic COPD patients. ERJ Open Res. 2022;2022:8.
21. Pedersen O, Butler J. Expiratory flow limitation. Compr Physiol. 2011;1:1861–1882.
22. Pecchiari M, Radovanovic D, Silianti C, et al. Tidal expiratory flow limitation induces expiratory looping of the alveolar pressure-flow relation in COPD patients. J Appl Physiol. 2020;129:75–83. doi:10.1152/japplphysiol.00664.2019
23. Ofir D, Laveneziana P, Webb K, Lam YM, O’Donnell DE. Mechanisms of dyspnea during cycle exercise in symptomatic patients with GOLD stage I chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2008;177:622–629. doi:10.1164/rccm.200707-1064OC
24. Briscoe WA, DuBois AB. The relationship between airway resistance, airway conductance and lung volume in subjects of different age and body size. J Clin Invest. 1958;37:1279–1285. doi:10.1172/JCI103715
25. Nakagawa M, Hattori N, Haruta Y, et al. Effect of increasing respiratory rate on airway resistance and reactance in COPD patients. Respir. 2015;28:87–94.
26. Ioan I, Demoulin-Alexikova S, Coutier L, et al. Specific airway resistance may be measured in preschool children during routine lung function. Eur Respir J. 2016;48:1804–1807. doi:10.1183/13993003.01302-2016
27. Singh D, Hurst J, Martinez F, et al. Predictive modelling of COPD exacerbation rates using baseline risk factors. Ther Adv Respir Dis. 2022;16:1–15. doi:10.1177/17534666221107314
28. Soriano J, Lamprecht B, Ramirez A, et al. Mortality prediction in chronic pulmonary disease comparing the GOLD 2007 and 2011 staging systems: a pooled analysis of patient data. Lancet Respir Med. 2015;3:443–450. doi:10.1016/S2213-2600(15)00157-5
29. Hoesterey D, Das N, Janssens W, et al. Spirometric indices of early airflow impairment in individuals at risk of developing COPD: spirometry beyond FEV1/FVC. Respir Med. 2019;156:58–68. doi:10.1016/j.rmed.2019.08.004
30. Borrill Z, Houghton C, Tal-Singer R, et al. The use of plethysmography and oscillometry to compare long-acting bronchodilators in patients with COPD. Br J Clin Pharmacol. 2007;65:244–252. doi:10.1111/j.1365-2125.2007.03013.x
31. Singh D, Brooks J, Hagan G, Cahn A, O’Connor BJ. Superiority of “triple” therapy with salmeterol/fluticasone propionate and tiotropium bromide versus individual components in moderate to severe COPD. Thorax. 2008;63:592–598. doi:10.1136/thx.2007.087213
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




