Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Integrative Korean Medicine Treatment for Obesity and Overweight in Children and Adolescents: A Multicenter Retrospective Chart Review Study
Authors Seo HS, Lee SH , Yim MH, Jeong YK , Chang GT , Ahn YJ, Lee JD, Chung WS, Ahn SY, Ahn YM, Lee BC, Noh JW , Lee B
Received 12 July 2023
Accepted for publication 26 August 2023
Published 15 September 2023 Volume 2023:16 Pages 2821—2832
DOI https://doi.org/10.2147/DMSO.S426848
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Hae Sun Seo,1,* Sun Haeng Lee,1,* Mi Hong Yim,2 Yoon Kyoung Jeong,3 Gyu Tae Chang,3 Ye-Ji Ahn,4 Jae Dong Lee,5 Won Seok Chung,6 Se Young Ahn,7 Young Min Ahn,7 Byung Cheol Lee,7 Ji-Won Noh,7 Boram Lee8
1Department of Korean Pediatrics, College of Korean Medicine, Kyung Hee University, Kyung Hee University Medical Center, Seoul, South Korea; 2Digital Health Research Division, Korea Institute of Oriental Medicine, Daejeon, South Korea; 3Department of Korean Pediatrics, College of Korean Medicine, Kyung Hee University, Kyung Hee University Hospital at Gangdong, Seoul, South Korea; 4Haeundae Hamsoa Korean Medicine Clinic, Busan, South Korea; 5Department of Acupuncture & Moxibustion Medicine, College of Korean Medicine, Kyung Hee University, Kyung Hee University Medical Center, Seoul, South Korea; 6Department of Korean Rehabilitation Medicine, College of Korean Medicine, Kyung Hee University, Kyung Hee University Medical Center, Seoul, South Korea; 7Department of Internal Medicine, College of Korean Medicine, Kyung Hee University, Kyung Hee University Medical Center, Seoul, South Korea; 8KM Science Research Division, Korea Institute of Oriental Medicine, Daejeon, South Korea
*These authors contributed equally to this work
Correspondence: Boram Lee, KM Science Research Division, Korea Institute of Oriental Medicine, 1672 Yuseong-daero, Yuseong-gu, Daejeon, 34054, South Korea, Tel +82-42-868-9622, Fax +82-42-868-9395, Email [email protected]
Introduction: Integrative Korean medicine treatment (IKM), including herbal medicine (HM) and acupuncture, has been widely used for obesity and overweight in children and adolescents in South Korea. We investigated the real-world usage status and the potential effect of the IKM for obesity and overweight in children and adolescents.
Methods: Multicenter medical charts were retrospectively reviewed of obese and overweight children and adolescents who visited Korean medicine institutions with the goal of weight control for the first time and received IKM, to analyze the usage status and effect of IKM. We defined IKM responders as those with an improved obesity grade on the body mass index (BMI) percentile and analyzed their characteristics.
Results: Medical charts of 209 patients (183 obese and 26 overweight) with a mean age of 11.45 years were examined. Patients visited the institution a mean of 5.95 times, and HM alone and HM plus acupuncture were frequently used IKM. HM was prescribed to 205 patients, 167 of whom received an HM prescription containing Ephedrae Herba. An HM of the decoction type was prescribed to 189 patients, and the average treatment duration was 76.54 days. After IKM, the percentile and z-score of BMI and weight significantly declined and height percentile and z-score were significantly enhanced, without serious adverse events. In the IKM responders, age, and the proportion of girls and overweight were significantly higher, and the percentile and z-score of height, weight, and BMI were significantly lower.
Conclusion: This is the first study to examine the real-world usage of IKM for obesity and overweight in children and adolescents. A significant improvement in obesity-related outcome measures after IKM, illustrated the potential effect of IKM.
Keywords: pediatric obesity, childhood overweight, traditional Korean medicine, herbal medicine, acupuncture
Introduction
Pediatric obesity is defined as having a body mass index (BMI) ≥ 95th percentile according to age and sex for children and adolescents aged ≥ 2 years. Pediatric overweight is defined as having a BMI ≥ 85th percentile and < 95th percentile according to age and sex.1 In recent decades, obesity has been escalating sharply, and in particular, over the past 40 years, obesity in children has increased by about eight times worldwide.2 Childhood obesity is highly likely to lead to adult obesity, and can accompany or cause various diseases such as cardiovascular diseases in adulthood, resulting in serious socioeconomic burden.3–5
According to recent clinical guidelines for the diagnosis and treatment of childhood and adolescent obesity,1 a staged approach is recommended for treatment. First, lifestyle modification is required, and if there are obesity-related comorbidities, such as diabetes and hyperlipidemia, they should be treated.1 If there is no improvement, additional treatment such as medication or surgical therapy is considered.1 However, lifestyle modification has low compliance in pediatric obese patients, and information on the efficacy and safety of medications is limited.6,7 Accordingly, the demand for safe and effective treatment for childhood and adolescent obesity is growing.
Integrative Korean medicine treatment (IKM), including herbal medicine (HM), acupuncture, moxibustion, cupping therapy, and chuna manual therapy, has been widely used for the treatment of children and adolescents with obesity and overweight in South Korea. HM involves the use of medicine collected from animals, plants, or minerals, including dried, cut, or refined in its original form. Acupuncture and moxibustion are therapeutic procedures involving the insertion of needles for remedial purposes and involving the use of ignited material to apply heat to certain points or areas of the body surface, for curing disease by regulating the function of meridians/channels and visceral organs, respectively.8 Cupping therapy is a therapeutic method involving the application of suction using a vacuumized cup or jar on the affected body surface.8 Chuna manual therapy is a manual therapy used to treat structural or functional problems by Korean medicine doctors (KMDs), who stimulate a patient’s body structures using hands, body parts, or tools such as a Chuna table.9 Although the effect of a specific HM, Slim-diet, with lifestyle modification on 13 obese children has been reported retrospectively,10 no clinical studies have investigated the use of various IKM and their effects in pediatric obesity and overweight. Therefore, to explore the current situation before examining the effect with a prospective study design, we investigated the real-world usage status and the potential effect of the IKM currently being used for children and adolescents with obesity and overweight through a multicenter chart review for the first time.
Methods
Study Design
This study was a retrospective chart review of children and adolescents with obesity and overweight treated by IKM at three Korean medicine institutions in South Korea, including two hospitals (Kyung Hee University Korean Medicine Hospital and Kyung Hee University Korean Medicine Hospital at Gangdong; both located in Seoul) and one clinic (Haeundae Hamsoa Korean Medicine Clinic located in Busan).
Study Population
Inclusion Criteria
- Children and adolescents (aged 2–19 years) who first visited the three Korean medicine institutions in South Korea from January 2012 to February 2023 with weight loss as their chief complaint. Children and adolescents in this age range were selected considering that those aged 2 years or older are classified as overweight or obese based on the BMI percentile according to age and sex,1 and Korean medicine institutions classify and treat patients under the age of 19 as children and adolescents.
- Obese and overweight patients whose BMI percentile at the time of the first visit was ≥ the 85th percentile compared to those of the same sex and age on the 2017 Korean National Growth Charts for children and adolescents, published by the Korea Centers for Disease Control and Prevention.1,11
- Those without other organic diseases that might cause obesity and overweight.
- Those patients who received IKM including HM, acupuncture, and moxibustion.
- Those participants with recorded changes in weight before and after IKM.
Exclusion Criteria
- Those judged to have other organic diseases causing obesity and overweight.
- Those subjects with insufficient medical records, such as the contents of IKM were not recorded.
- Those patients who visited after 12 months from the previous visit, judged to be ambiguous regarding outcomes as the effect of IKM.
Data Collected
Sociodemographic Characteristics
The following items were collected as sociodemographic information for patients if they could be identified in the chart: age, sex, type of visit (inpatient or outpatient), height, weight, BMI, birth weight, mid-parental height (MPH), family history, medical history including history of obesity treatment, menarche in the case of girls, and current comorbidities.
Details of Integrative Korean Medicine
The type and combination of IKM used for each patient in all institutions was determined according to the clinical KMDs’ judgment and patients’ opinion. To investigate the real-world usage of IKM in a clinical setting, details of IKM including treatment contents, treatment period, and number of treatments and visits were collected. For herbal decoction, the frequency of individual prescriptions was investigated.
Obesity-Related Outcome Measures
To explore the magnitude of the potential effect of IKM, the following obesity-related outcome measures were investigated.
- BMI percentile and z-score
- Weight percentile and z-score
- Body composition parameters including body fat mass and body fat percentage (measured by bioelectric impedance analysis)
- Height percentile and z-score
The percentile and z-score of BMI, weight, and height were calculated based on the 2017 Korean National Growth Charts for children and adolescents, published by the Korea Centers for Disease Control and Prevention.11
Investigation of Adverse Events
To explore the safety of IKM, all adverse events that occurred during the treatment period and whether they were cured were investigated.
Characteristics of Responders
The patients were classified into “responders” and “non-responders”, and responders were defined as patients with an improvement in obesity grade on the BMI percentile chart after IKM, including patients who were obese by BMI percentile at the first visit but adjusted to overweight or normal after the last treatment or patients who were overweight at the first visit but transformed to normal after the last treatment. The differences in characteristics between the two groups were compared.
Data Analysis
General characteristics of the patients were summarized as mean ± standard deviation (SD) and frequency (column proportion) for continuous and categorical variables, respectively. Differences in general characteristics between boys and girls were compared using independent two-sample t-test for continuous variables and Chi-squared test for categorical variables. Changes in obesity-related outcome measures before and after IKM were analyzed using the paired t-test or Wilcoxon signed-rank test depending on the sample size and the normality test results of the Shapiro–Wilk test. The effects sizes were calculated using Cohen’s d.12 Subgroup analysis was conducted by dividing all patients according to (1) sex, (2) BMI category (obese or overweight), and (3) whether the prescribed HM contained Ephedrae Herba. In IKM, obesity is considered as a non-physiological fluid retention state caused by abnormal fluid metabolism due to qi deficiency, decreased activity, stress, and excessive nutrition.13 Ephedrae Herba is one of the most commonly used herbs for the treatment of obesity in IKM because it can alleviate abnormalities in fluid metabolism through improvements in the functions of the spleen, lungs, and kidneys by promoting sweating to dispel pathogenic factors from the exterior portion of the body, diffusing the lungs to resolve phlegm, and opening interstices.14,15 Differences in characteristics of patients between the responder and non-responder groups were compared using Wilcoxon rank-sum tests because of the small sample size and the normality test results for continuous variables. For categorical variables, the Chi-squared test and Fisher’s exact test were used depending on whether one of the cells in the contingency table had five or fewer than five observations. All statistical analyses were performed using R version 4.2.1 (R Core Team [2022], Vienna, Austria), and a significance level of 0.05 were defined. The different sample sizes were utilized according to individual analysis due to missing values for each variable.
Ethical Considerations
This study was approved by the Institutional Review Boards (IRBs) of Kyung Hee University Korean Medicine Hospital (KOMCIRB 2022-05-001-001), Kyung Hee University Korean Medicine Hospital at Gangdong (KHNMCOH 2022-06-008), and Korea Institute of Oriental Medicine (I-2207/007-001) to analyze the data that did not include the participants’ personal identification information. Informed consent was waived by IRBs because it was practically impossible to obtain consent from participants, and it did not include personally identifiable information. Our research was conducted in compliance with the Declaration of Helsinki.
Results
Patient Characteristics
There were a total of 644 pediatric patients who first visited the three institutions for the purpose of weight loss. As a result of review according to the eligibility criteria, a total of 209 patients were included in the analysis (Figure 1). The patients consisted of 111 boys (53.11%) and 98 girls (46.89%), and the mean ± SD age was 11.45 ± 3.98 years. There were 50 girls (51.02%) who started menarche, 25 girls (25.51%) who did not, and 23 girls (23.47%) who had no relevant records. The average height, weight, and BMI for the combined sexes were 147.39 ± 17.24 cm, 59.89 ± 21.82 kg, and 26.54 ± 4.47. There were 183 obese (87.56%) and 26 overweight (12.44%) children and adolescents (Table 1). Two patients (0.96%) treated for obesity in the past had been treated with appetite suppressants, including liraglutide injection for two weeks and phentermine/topiramate for one month, respectively. All patients were not receiving any other obesity treatment at the time of their first visit and during the treatment period. Three patients (1.44%) received both hospitalization and outpatient treatment, and the rest received only outpatient treatment. Allergic rhinitis was the most common comorbidity in 39 patients (18.66%), followed by short stature (27 patients, 12.92%) and edema (14 patients, 6.70%) (Supplementary Table 1).
 |
Table 1 Characteristics of the Patients |
 |
Figure 1 A flowchart of inclusion of patients. Abbreviations: BMI, body mass index; IKM, integrative Korean medicine treatment. |
Details of Integrative Korean Medicine
Patients visited the hospitals and clinic an average of 5.95 ± 7.80 times, and the mean total period of visits, which is the period between the first and last visits was 176.8 ± 299.79 days. HM alone was used most frequently in 114 patients (54.55%), and HM plus acupuncture was also often used in 40 patients (19.14%), followed by HM, moxibustion, acupuncture, and chuna manual therapy (19 patients, 9.09%) and HM, moxibustion, and acupuncture (12 patients, 5.74%) (Table 2). When examining individual IKM, HM was administered to 205 patients (98.09%), among these patients, 189 patients received decoctions, and 109 patients received granules as the dosage form. Of the patients who were prescribed HM, 167 had Ephedrae Herba in their prescription and 38 did not. In the case of herbal decoction, an average of 1.40 ± 0.93 types were administered, and the average administration period was 76.54 ± 87.45 days. When all the herbal decoctions administered to the patients were counted, modified Wolbigachul-tang was used most often in 29 patients (14.95%), followed by modified Pyeongjin-tang in 18 patients (9.28%), and modified Taeeumjowi-tang in 17 patients (8.76%) (Supplementary Table 2).
 |
Table 2 Contents of Integrative Korean Medicine Treatment |
Moxibustion was implemented an average of 9.73 ± 11.11 times during the treatment period in 48 patients (22.97%), among them indirect moxibustion was conducted in 46 patients and direct moxibustion in two patients. Acupuncture was performed an average of 10.20 ± 17.15 times for 87 patients (41.63%), including manual acupuncture at points located on the auricle (ear acupuncture) for 38 patients, manual acupuncture at points located on the trunk and limbs for 44 patients, and electroacupuncture (electric stimulation of the needle following insertion) for 35 patients. Cupping therapy, pharmacopuncture, and chuna manual therapy were conducted in five (2.39%), seven (3.35%), and 27 (12.92%) patients, with an average of 4 ± 3, 7 ± 6.95, and 13.44 ± 10.83 times, respectively, during the treatment period. Each IKM was safely performed by licensed KMDs after completing a formal education course in the Department of Korean Medicine at universities for more than 6 years.
Changes in Obesity-Related Outcome Measures
The BMI percentile decreased significantly from an average of 97.93 ± 3.13 before treatment to an average of 96.4 ± 6.04 after treatment (p<0.001) (Figure 2), and the effect size was small to medium at 0.36. The BMI z-score also diminished statistically significantly from an average of 2.62 ± 0.97 before treatment to an average of 2.36 ± 0.94 after treatment (p<0.001) (Figure 2), and the effect size was medium to large at 0.63. The weight percentile and z-score declined significantly from 95.91 ± 6.19 and 2.31 ± 0.95 before treatment to 94.27 ± 8.12 and 2.11 ± 0.95 after treatment (all p<0.001), respectively (Table 3 and Supplementary Figure 1). These meaningful results in percentile and z-score of BMI and weight were consistent regardless of subgroup analysis according to sex (Supplementary Table 3a) and BMI category (Supplementary Table 3b). However, only patients taking HM including Ephedrae Herba showed a significant difference (Supplementary Table 3c).
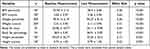 |
Table 3 Change in Obesity-Related Outcome Measures |
 |
Figure 2 Changes of BMI percentile and z-score. Abbreviation: BMI, body mass index. |
Body fat mass and body fat percentage decreased statistically significantly from 25.96 ± 10.77 and 38.9 ± 5.92 before treatment to 24.11 ± 9.98 and 36.91 ± 5.87 after treatment (all p<0.001), respectively (Table 3 and Supplementary Figure 1). However, in both outcomes, only obese patients and patients taking HM including Ephedrae Herba displayed a marked difference, and body fat mass showed a noteworthy change only in girls (Supplementary Table 3a–c).
The height percentile and z-score increased significantly from 69.29 ± 26.77 and 0.74 ± 1.03 before treatment to 70.24 ± 26.6 and 0.79 ± 1.05 after treatment (p=0.021 and 0.002) (Table 3 and Supplementary Figure 1). These significant differences were consistent only in girls and obese patients (Supplementary Table 3a and b). Height z-score presented a significant difference only in patients taking HM including Ephedrae Herba (Supplementary Table 3c).
Adverse Events
A total of 48 adverse events occurred in 16 patients during the treatment period. Among them, diarrhea was the most common with 20 cases (41.67%), followed by nausea in eight cases (16.67%), dizziness in four cases (8.33%), and vomiting in three cases (6.25%) (Table 4). The diarrhea in 19 cases out of 20 and the vomiting in three cases were all induced after taking Euphorbia kansui Liou ex Wang, a typical purgative herb used in therapies that induce vomiting and diarrhea. All adverse events disappeared spontaneously without special action or were treated with appropriate methods according to the judgment of KMDs. These adverse events did not affect the treatment contents of patients, and treatment was resumed after recovery if necessary according to the KMDs’ judgement.
 |
Table 4 Adverse Events |
Characteristics of Responders
Twenty-four patients (11.48%) responded to IKM. When the characteristics of the responder and non-responder groups were compared retrospectively, the proportion of girls and overweight in the BMI category was significantly higher in the responders, as was age. In addition, the percentile and z-score of height, weight, and BMI were significantly lower in responders. There were no significant differences between the two groups in other parameters such as birth weight, number of visits, and administration period of herbal decoction treatment (Table 5).
 |
Table 5 Characteristics of Patients According to the Treatment Response |
Discussion
Childhood and adolescent obesity is one of the most serious global public health problems of the 21st century. According to the data released by the World Health Organization in 2019,16 the number of school-age children with obesity has increased more than 10 times over the past 40 years. More than 38 million children under the age of five were also stated to be obese or overweight; therefore, all countries around the world agreed on a global goal to stop the increase in obesity and overweight.16 Although estimates of the cost of childhood obesity worldwide have yet to be described, reducing the average BMI percentile of children by 5 percentile points could save 1.1 billion euros in lifetime costs. Hence, prevention and treatment of childhood obesity may be of economic value.16 However, due to limitations such as low compliance with current lifestyle interventions and the side effects and high cost of conventional medication for childhood and adolescent obesity,6,7 there is an increasing demand for complementary and integrative medicine that can be combined with lifestyle interventions for children and adolescents who are obese and overweight.17,18 In particular, in South Korea, IKM (including HM and acupuncture) has been actively used for the treatment of children and adolescents who are overweight and obese. However, studies on its actual use, effectiveness, and safety have not been conducted thus far. Considering that an effective treatment strategy is needed due to the increase in childhood and adolescent obesity worldwide, this study attempted to present a global treatment option by examining the current status and effects of IKM.
A total of 209 patients with a mean age of 11.45 years were included in the analysis. The average number of patient visits was 5.95, and various combinations of IKM were used, but HM alone was the most common, followed by HM plus acupuncture. Herbal decoction was administered for an average of 76.54 days. Obesity-related outcome measures including the percentile and z-score of BMI and weight, body fat mass, and body fat percentile all significantly declined after treatment, and the effect size was generally small to moderate. In addition, the height percentile and z-score also showed a tendency to increase significantly after treatment.
In the subgroup analysis, the percentile and z-score of BMI and weight, body fat mass, and body fat percentage significantly improved only in patients taking HM including Ephedrae Herba. The anti-obesity effect of Ephedrae Herba is achieved by stimulating the sympathetic nerve by directly activating β1- and β2-adrenoreceptors with ephedrine, the main ingredient.19 It is also associated with accelerated body fat breakdown through decreased appetite, inhibition of cholesterol absorption in the small intestine and increased energy expenditure in adipose tissue.20 Therefore, Ephedrae Herba has been one of the most often used herbs for the treatment of obesity in IKM,15 and the significant weight loss effect of HM including Ephedrae Herba can be caused by these comprehensive actions.
There were 48 adverse events during the treatment period, and they disappeared spontaneously without special action or were treated with appropriate methods according to the judgment of KMDs. The frequently reported adverse events were diarrhea, nausea, dizziness, and vomiting. In particular, most of the patients who complained of diarrhea and vomiting occurred after taking Euphorbia kansui Liou ex Wang, a representative offensive purgative medicinal agent. Euphorbia kansui Liou ex Wang is used to remove moisture from the lower part of the human body, treat chronic indigestion, and has anti-obesity and glycemic control effects.21 Considering that Euphorbia kansui Liou ex Wang is a representative purgative medicine and is used in therapies that induce vomiting and diarrhea, these symptoms after taking it may not be considered as adverse events. In addition, dehydration symptoms, which are considered the most cautious adverse events after taking Euphorbia kansui Liou ex Wang,22 were not reported by any participant in the present study. Especially, Ephedrae Herba is associated with symptoms such as tachycardia, arrhythmia, tremor, insomnia, and lack of appetite, and adverse events related to the cardiovascular and nervous systems have been described. Hence, in South Korea, clinical safety guidelines for the use of Ephedrae Herba in obesity treatment have been published.23,24 In our study, adverse events such as palpitation and insomnia, which may be related to Ephedrae Herba, were informed in a small number of patients but disappeared spontaneously or were cured. One study25 stated that no significant changes were observed in electrocardiogram, Doppler ultrasound, blood tests, and urinalysis when healthy people were prescribed adequate amounts of Ephedrae Herba and ephedrine in the short and long term. According to the results of our study, IKM performed under the judgment of professional KMDs can make it possible for children and adolescents with obesity and overweight to achieve weight loss without serious adverse reactions.
Modified Wolbigachul-tang, Pyeongjin-tang, and Taeeumjowi-tang were the frequently used herbal decoctions in patients. Wolbichul-tang was used for edema in the Synopsis of Prescriptions of the Golden Chamber, and the its effect on obese patients has been described.26 Pyeongjin-tang is a combination of Pyeongwi-san (Pingwei-san in Chinese) and Yijin-tang (Erchen-tang in Chinese). Pyeongwi-san regulates gastrointestinal activity and water-electrolyte metabolism,27 and the effect of Yijin-tang on obesity has also been stated.28 Taeeumjowi-tang is one of the most frequently utilized and studied HMs for obesity treatment, and its weight loss effect has also been conveyed.29,30
We compared the characteristics of IKM responders and non-responders. In the responders, the proportion of girls and overweight was significantly higher, along with age. The percentile and z-score of height, weight, and BMI were significantly lower in responders. To the best of our knowledge, this is the first analysis of the characteristics of responders after IKM in obese and overweight children and adolescent and may help clinicians understand treatment outcomes and prognosis for patients. However, this was a retrospective comparison of the characteristics of two groups after operationally defining the responders of IKM following a discussion among the researchers. Consequently, there is no data to compare these with the responder ratio and characteristics of responders of other obesity-related therapies. Therefore, it cannot be concluded that the indicators reported to have significant differences between the two groups are the only indicators that directly influence IKM effects.
The limitation of this study is that the patient’s lifestyle and compliance with IKM were not sufficiently controlled due to the retrospective nature of this study. Because children and adolescent’s physical activity and eating habits are significantly related to obesity and overweight,31,32 they act as confounding variables in the results of this study. However, information on these factors was not sufficiently described in medical records, and its influence cannot be ignored. In addition, because children and adolescents are growing, sexual maturity has an important effect on the outcome of growth and development. However, because sexual maturity was recorded in only five patients, the effect on obesity-related outcomes could not be confirmed. Finally, according to the judgment of clinical KMDs, the dose and components of HMs and acupuncture tools were selected depending on the patient’s age, accompanying symptom, and pattern identification. However, due to the nature of the retrospective chart review, it was not possible to obtain complete information on all treatments. Therefore, it was not possible to determine which treatment among the IKMs was more effective.
Nevertheless, this study is the first study to examine the real-world use, preliminary effects, and safety of IKM, which is actively being conducted in clinical settings in South Korea, in obese and overweight pediatric patients through the analysis of various variables. We tried to minimize regional bias in South Korea by analyzing three multi-center chart reviews. In addition, various combinations of IKM were used against the patient’s accompanying symptoms and pattern identification, and the clinical judgement of KMDs. As a result, the preliminary effect and safety of them were examined in a practical way. Furthermore, the effect size of the change was also calculated. In the future, based on the results confirmed in this study, the effect of IKM should be investigated prospectively in comparison with an appropriate control group such as lifestyle intervention. In particular, because childhood and adolescent obesity can lead to adult obesity in many cases and cause various complications, research on the effect of IKM received in childhood on BMI and weight in adulthood through long-term registry studies with a large sample size should be conducted. In addition, if related studies are conducted in China and Japan, where HM and acupuncture are also actively performed in children and adolescents with obesity and overweight, it will help to generalize the study results. Furthermore, considering the worldwide socioeconomic impact of childhood and adolescent obesity and the need for cost-effective therapeutic methods, future economic evaluation research investigating the effects and costs of IKM will be helpful for the decision-making process of policymakers as well as clinicians, researchers, and patients.
Conclusions
Given the worldwide increase in childhood and adolescent obesity and the growing demand for safe and effective treatments, we examined the real-world use, effects, and safety of IKM for children and adolescents who are overweight and obese through a multicenter chart review for the first time, which is actively used for treatment in clinical settings in South Korea. The real-world usage of IKM indicated that HM alone was the most frequently used, and herbal decoction was administered for an average of 76.54 days. A significant reduction in BMI and weight percentile and z-score, and a significant improvement in height percentile and z-score in them after IKM, without serious adverse events revealed the potential effect and safety of IKM.
Data Sharing Statement
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
Funding
This work was supported by a grant from the Korea Health Technology R&D Project, through the Korea Health Industry Development Institute (KHIDI), and funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HF22C0035).
Disclosure
Hae Sun Seo and Sun Haeng Lee are co-first authors for this study. The authors declare that they have no conflicts of interest in this work.
References
1. Yi DY, Kim SC, Lee JH, et al. Clinical practice guideline for the diagnosis and treatment of pediatric obesity: recommendations from the committee on pediatric obesity of the Korean Society of pediatric gastroenterology hepatology and nutrition. Pediatr Gastroenterol Hepatol Nutr. 2019;22(1):1–27. doi:10.5223/pghn.2019.22.1.1
2. Abarca-Gómez L, Abdeen ZA, Hamid ZA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642.
3. Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360(9331):473–482. doi:10.1016/s0140-6736(02)09678-2
4. Ayer J, Charakida M, Deanfield JE, Celermajer DS. Lifetime risk: childhood obesity and cardiovascular risk. Eur Heart J. 2015;36(22):1371–1376. doi:10.1093/eurheartj/ehv089
5. Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488. doi:10.1111/j.1467-789X.2008.00475.x
6. Sabin MA, Kiess W. Childhood obesity: current and novel approaches. Best Pract Res Clin Endocrinol Metab. 2015;29(3):327–338. doi:10.1016/j.beem.2015.04.003
7. Coles N, Birken C, Hamilton J. Emerging treatments for severe obesity in children and adolescents. BMJ. 2016;354:i4116. doi:10.1136/bmj.i4116
8. WHO Western Pacific Region. WHO international standard terminologies on traditional medicine in the Western Pacific region. World Health Organization; 2007.
9. Hwang B-K, Park KS, S-H K, et al. Efficacy and safety of Korean herbal medicine for patients with post-accident syndrome, persistent after acute phase: a pragmatic randomized controlled trial. MDPI. 2023;11(4):534.
10. Kim KW, Kim SJ, Kim H, Shin SU, Song J, Chung WS. Clinical effects of slim-diet, with lifestyle modification for childhood obesity in community-based healthcare program: a case series. Medicine. 2020;99(26):e20817. doi:10.1097/md.0000000000020817
11. Kim JH, Yun S, Hwang S-S, et al. The 2017 Korean National Growth charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018;61(5):135. doi:10.3345/kjp.2018.61.5.135
12. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Academic press; 2013.
13. Jung SM, Kwon SE, Kang SY, Kim SJ, Jung HW, Park Y-K. Anti-obesity and anti-diabetic effects of a polyherbal extract consisting of Coptidis rhizoma, Salviae miltiorrhizae radix, and Cinnamomi cortex in high fat diet-induced obesity mice. J Korean Med Obes Res. 2021;21(2):59–68. doi:10.15429/jkomor.2021.21.2.59
14. Shin MK. Professors of formula study of Korean Medicine School. In: Clinical Traditional Herbalogy. Seoul: Yeong-lim Press; 2016:236.
15. Hwang M-J, Shin H-D, Song M-Y. Literature review of herbal medicines on treatment of obesity since 2000; mainly about ephedra herba. J Korean Med Obes Res. 2007;7(1):39–54.
16. World Health Organization. Taking action on childhood obesity. No. WHO/NMH/PND/ECHO/18.1; 2018.
17. Han KS, Lee MJ, Kim HJ. Systematic review on herbal treatment for obesity in adults. J Korean Med Rehabil. 2016;26(4):23–35. doi:10.18325/jkmr.2016.26.4.23
18. Shim SB, Lee HH, Ahn HL, Lee JA, Lee HL. Effectiveness and safety of herbal medicine on children with simple obesity: a protocol for systematic review and meta-analysis. Medicine. 2021;2(8):e0132.
19. Shannon JR, Gottesdiener K, Jordan J, et al. Acute effect of ephedrine on 24-h energy balance. Clin Sci. 1999;96(5):483–491. doi:10.1042/cs0960483
20. Jang I-S, Yang C-S, Hwang E-H. The need for clinical practice guidelines in usage of Mahuang in weight loss. J Korean Med Obesity Res. 2007;7(1):23–29.
21. Nam SH, Kim DH, Choi HM, Kang JH, Hyun MK. A case report of lumbar spinal stenosis improved with diarrhea-inducing treatment by Gamsui-mal and Korean medicine treatment. J Korean Med Rehabil. 2017;27(1):67–75. doi:10.18325/jkmr.2017.27.1.67
22. Lee DE, Yoo JH, Kim DH, Ahn SY, Lee B-C, Ahn YM. A case report on the effect of a short-term intensive obesity treatment on an obese patient. J Intern Korean Med. 2017;38(5):681–688. doi:10.22246/jikm.2017.38.5.681
23. Kim HJ, Han CH, Lee EJ, Song YK, Shin BC, Kim YK. A clinical practice guideline for Ma-huang (Ephedra sinica) prescription in obesity. J Korean Med Obes Res. 2007;7(2):27–37.
24. Song YK, Lim HH. Clinical application of Ma Huang in the obesity treatment. J Korean Med Obes Res. 2007;7(1):1–7.
25. Jo GW, Ok JM, Kim SY, Lim YW. Review on the efficacy and safety of mahuang and ephedrine in the treatment of obesity-focused on RCT. J Korean Med. 2017;38(3):170–184. doi:10.13048/jkm.17034
26. Kwak H-Y, Kim J-H, Seon J-I, et al. The effects and adverse events of Gamiwolbigachultang on the changes of body composition and musculoskeletal pain in 28 overweight patients: a retrospective observational study. J Acupunct Res. 2011;28(5):103–110.
27. Gao BZ, Chen JC, Liao LH, Xu JQ, Lin XF, Ding SS. Erchen decoction prevents high-fat diet induced metabolic disorders in C57BL/6 mice. Evid Based Complement Alternat Med. 2015;2015:501272. doi:10.1155/2015/501272
28. Choi J, Cho J, Jang J, Lee K. The effects of Yi-Jin Tang on body weight and ovarian reaction in obesity mice. J Korean Obstet Gynecol. 2003;162:68–75.
29. Kwak J-Y, Ahn T-W. The effects of taeeumjowi-tang extract granule on metabolic syndrome risk factors with obesity: a single group, prospective, multi-center trial. J Sasang Constitut Med. 2020;32(2):48–60.
30. Hwang M, Shin H, Song M. Review of literature on herbal medicines for the treatment of obesity in Korea: mainly papers since 2000. J Oriental Rehab Med. 2006;16(3):65–81.
31. Maffeis C, Provera S, Filippi L, et al. Distribution of food intake as a risk factor for childhood obesity. Int J Obes Relat Metab Disord. 2000;24(1):75–80. doi:10.1038/sj.ijo.0801088
32. Hong I, Coker-Bolt P, Anderson KR, Lee D, Velozo CA. Relationship between physical activity and overweight and obesity in children: findings from the 2012 national health and nutrition examination survey national youth fitness survey. Am J Occup Ther. 2016;70(5):7005180060p1–8. doi:10.5014/ajot.2016.021212
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
