Back to Journals » Advances in Medical Education and Practice » Volume 11
Integrating High-Fidelity Simulation into a Medical Cardiovascular Physiology Curriculum
Authors Zheng J , Lapu R , Khalid H
Received 10 September 2019
Accepted for publication 3 November 2019
Published 15 January 2020 Volume 2020:11 Pages 41—50
DOI https://doi.org/10.2147/AMEP.S230084
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Md Anwarul Azim Majumder
Jinjie Zheng, 1 Rigobert Lapu, 2 Hammad Khalid 3
1Department of Medical Education, Morehouse School of Medicine, Atlanta, GA, USA; 2Department of Medicine, Morehouse School of Medicine, Atlanta, GA, USA; 3MD Program, Morehouse School of Medicine, Atlanta, GA, USA
Correspondence: Jinjie Zheng
Morehouse School of Medicine, 720 Westview Drive, SW, Atlanta, GA 30310, USA
Tel +1404 752 1565
Fax +1404 752 1064
Email [email protected]
Introduction: The challenges of transitioning from basic sciences to clerkships are well identified in medical education. High-fidelity simulations, which have established a track record of improving clinical reasoning and clinical skills, have been proposed as a viable approach to bridge the gap between basic sciences and clerkships. However, little is known about the results of using simulation to address the gap.
Methods: In 2018, Morehouse School of Medicine enhanced the first-year cardiovascular physiology curriculum by integrating the high-fidelity simulation iStan into the cardiovascular physiology curriculum, with the purpose of early clinical exposure, cardiovascular concept mastery, and increased clinical associations. The integration included three structural design elements: (a) simulated clinical case introduction; (b) simulated clinical case development; and (c) student-led clinical case study.
Results: The first-year medical (MD1) students’ cardiovascular physiology learning outcomes have significantly improved compared to the last two cohorts of MD1 students, and the students’ test-taking time was significantly reduced compared to the performance of the last two counterpart cohorts. Students reported increased engagement in the simulation-enhanced cardiovascular physiology curriculum.
Conclusion: The findings provide preliminary evidence to suggest that the structural integration of high-fidelity simulation in the cardiovascular physiology curriculum proved successful in terms of students’ learning experience and learning outcomes. The three central elements of high-fidelity simulation integration can inform future endeavor as a structural solution to effectively bridge the gaps between basic science concepts and clinical reasoning by using high-fidelity simulations.
Keywords: high-fidelity simulation, preclinical curriculum integration, evaluation, simulation case development
Introduction
The ongoing national efforts of medical curriculum redesign feature a creative use of various instructional methods and state-of-the-art technologies to close healthcare competency gaps.1–3 A successful knowledge transfer from basic science concepts to clinical reasoning to clinical skills has been identified as a challenging area that can be benefited from this endeavor.4–6 Specifically, high-fidelity simulations have been proposed as a viable approach to enhance basic science concepts and clinical reasoning skills at an early stage of medical student training and demonstrated the evidence of effectiveness.4,7,8
Existing research and teaching literature present promising evidence in this regard: high-fidelity simulation has been described as an avenue to educate medical students in third-year clerkships and residents by providing a low-risk, safe learning environment.9,10,11 Varied small-group activities have been designed to integrate simulation into the cardiovascular physiology curriculum to provide students with hands-on simulation experience and to improve clinical reasoning skills.12,13 An effective integration of high-fidelity simulation in a lecture-hall-based preclinical curriculum requires robust data-driven evidence from varied approaches to establish and inform practices.14 Many of the research studies on this topic were published about a decade ago. Several constraints may have contributed to the lack of sustained literature in this domain: for example, overwhelming design and implementation decisions and execution, juggling choices of multiple teaching methods, small-group simulation scheduling conflicts in preclinical years, and concerns of learning outcomes against the return on time and effort investment.
This paper studied the outcomes of structuraly integrating high-fidelity simulation in a cardiovascular physiology curriculum. Specifically, we purposefully integrated three structural elements into the cardiovascular physiology curriculum: a simulated clinical case introduction; simulated clinical case development; and a small-group student-centered case study. In this paper, we detailed clinical case revision decisions, step-by-step high-fidelity simulation-integration approaches, as well as the students’ learning experiences and learning outcomes. Through detailing the replicable steps and providing the framework of this simulation integration, we hope to inform future practice and encourage a renewed discussion on using high-fidelity simulations to close the competency gaps between basic sciences and clinical correlations.
Methods
Study Design
The study was approved by the Institutional Review Board (IRB) at Morehouse School of Medicine in 2018 as category four Exempt. The study used a non-experimental cohort study with historical controls. One hundred and one first-year medical (MD1) students in the 2018 cohort participated in a simulation-integrated cardiovascular physiology curriculum as a convenient sample. Their curriculum learning outcomes were compared with that of the students in 2017 and 2016 cohorts who experienced a traditional lecture-based curriculum. The participating students responded to the simulation-integration curriculum survey anonymously. The study sought to answer two research questions: firstly, what are the outcomes of integrating high-fidelity simulation into the cardiovascular physiology curriculum, comparing with the unintegrated curriculum? And second, what are the students’ feedback and learning experience on the simulation-integrated curriculum?
Curriculum Setting and Intervention
The purposes of integration are three-fold: familiarize students early to the clinical setting; improve cardiovascular physiology concept mastery; and enhance clinical reasoning skills. Through multiple planning and design sessions, the following three structural elements were intentionally designed and integrated into the curriculum. Figure 1 illustrates the details of these three elements, followed by a detailed explanation of each one.
 |
Figure 1 Flowchart of our step-by-step high-fidelity simulation integrative approach (simulation-based learning and problem-based learning). |
The cardiovascular physiology curriculum entailed eight 90-minute class lectures across a 4-week time span. We implemented Element A in the second cardiovascular physiology lecture when the simulated patient case was introduced to the first-year medical (MD1) students via a real-time tele-stream from the simulation center to the lecture hall. The physician instructor (RL) presented the case in the lecture as well as the simulated real-time vital signs and electrocardiogram (ECG) of the high-fidelity simulator (iStan) that was set to portray high blood pressure (hypertension) and subsequently developed myocardial infarction. Element B entailed a 90-minute, interactive, problem-based solving lecture-hall session at the 7th lecture slot of the cardiovascular physiology curriculum. The instructor (RL) utilized three pre-designed iStan-interaction videos to present and model the simulated standardized patient encounter, clinical case presentation, and case development as a clinical trigger for large class-size lecture-hall problem-based learning sessions. Element C, which consisted of a student-led, small-group case study, concluded the cardiovascular physiology curriculum. Each element is further explained below.
Element A: Initial iStan-Clinical Case Introduction
The initial iStan clinical case introduction was conducted via real-time streaming from the simulation center to the lecture hall with the purposes of creating an authentic learning environment and bringing the sentiments of “immediacy” and “reality” of a clinical patient case to the classroom. After the introduction of the lecture objective, the instructor introduced the use of the simulation center, followed by a real-time phone call from the classroom to the simulation center. The scene of the clinical setting was presented via a classroom projector through a clinical skill teaching software entitled “Learning Space”. The physician simulation director presented the iStan patient case, along with the baseline vital signs, high-risk patient case, and the vital signs for the case scenario of interest (shock). The first integration episode concluded after the iStan-case presentation. The iStan high-fidelity simulator was selected because of three reasons: (1) iStan is equipped with physiology models and responsive abnormal physiology for the teaching purpose; (2) iStan has a wireless microphone to simulate physician–patient encountering, and (3) iStan is housed in a room with a two-way mirror for the simulator center director to conveniently role-play the patient encountering verbally.
Element B: iStan-Clinical Case Development
The purpose of Element B is to use iStan to: (a) role model a standardized patient encounter process as part of the clinical development case presentation process; (b) present case-development vital signs; and (c) provide immediate clinical reasoning result feedback to students’ problem-solving process. This time, the iStan curricular integration was achieved through three pre-designed and pre-recorded videos integrated into a full 90-minute instructor-led, problem-solving session. These three videos are referenced below to further elucidate key steps in the teaching flow:
- Initial Standardized Simulated Patient Encounter Video A
- Standardized Patient Vital Signs/EKG Video B
- Shock Simulated Patient of Interest Vital Signs/EKG Video C
The teaching flow below captures the step-by-step approach of: simulation video integration; patient encounter debriefing; comprehensive review of cardiovascular physiology concepts in the context of clinical case developments; and interactive questioning.
- Recall the last simulation center patient case.
- Invite students to revisit the simulated patient case as a physician.
- Students watch the instructor’s encounter with the standardized simulated patient, and the simulated patient presents the case development and chief complaints (Video A).
- Instructor guided students’ analysis of the simulated standardized patient encounter.
- Summary of the simulated patient encounter.
- Instructor interactively guided students’ probing of patient history, case development, and screening process.
- Instructor interactively questioned students using basic science concepts for clinical reasoning.
- The baseline vital signs/EKG from the simulated patient were shown in order to confirm the clinical reasoning process (Video B).
- Instructor questioned students using basic science concepts to solve the clinical prediction of case development.
- The shock case vital signs/EKG from the simulated patient were shown to confirm the validity of the clinical reasoning process (Video C).
- Instructor reviewed the basic science concepts and clinical reasoning process involved in the simulated patient case development.
- Instructor presented an additional PowerPoint presentation on using the same clinical reasoning process for other clinical cases.
- End of the clinical correlation integration session and bridging (introduction) to the cardiovascular physiology small-group student-centered clinical case study as discussed briefly below.
The purpose of this modified case scenario was to help students apply the basic cardiovascular principles they have learned from the previous classes in a clinical setting as follows: (1) Concept: Long-standing/poorly controlled blood pressure (BP) or hypertension (HTN) and related effect of increased afterload (i.e., increase in aortic pressure) on the heart (i.e., pressure-volume loop of the ventricle). We discussed how afterload is the pressure against which the ventricles of the heart must eject blood. Afterload of the left ventricle is aortic pressure. To open the aortic valve and eject blood, left ventricular pressure must increase to a level greater than aortic pressure. Thus, if afterload increases, as in the case scenario of this patient with long-standing HTN, the left ventricle must work harder than usual to overcome this higher pressure. This results in a decrease in stroke volume (SV), cardiac output (CO), ejection fraction (EF) and an increase in end-systolic volume (ESV). (2) Reasoning at a glance: ↑BP → ↑AFTERLOAD → ↑heart muscle, a condition called left ventricular hypertrophy (LVH) → myocardial O2 deprivation by supply/demand imbalance → myocardial ischemia/infarct → death of heart muscle → compromised systolic heart function as a pump [↓contractility → ↓SV/CO/EF → ↓BP].
Our debriefing covered the history of patients with acute chest pain syndrome who are at increased risk for multiple heart complications, including repetitive ischemia. In the case study described here, a patient with poorly controlled high BP/HTN and LVH had developed a heart attack (i.e., myocardial infarction) with recurrent/repetitive myocardial ischemia, ultimately leading to hemodynamic compromise and cardiogenic shock. The patient had LV wall infarction secondary to myocardial ischemia. This damage to the left ventricle compromised its function as a pump. The left ventricle could no longer generate enough pressure to eject blood normally. We discussed conventional high-risk factors predisposing to atherosclerotic cardiovascular disease (CVD) in this patient presenting with acute chest pain, including older age and uncontrolled HTN [as in our case study]. The resulting change in cardiac muscle (i.e., LVH) was the most critical predisposing factor for heart attack (i.e., myocardial infarction). Other risk factors we discussed included smoking, obesity and associated lipid abnormalities, such as low HDL cholesterol.
Element C: Student-Led Small-Group Case Study
Element C concluded the cardiovascular physiology curriculum with a student-led, small-group case study. Each case study group consisted of eight students and two faculty facilitators (one basic scientist and one clinician). The purpose of the student-led small-group case study is to help students transition from the instructor-led problem-solving process to an independent problem-solving process. During this process, students completed two activities. First, students completed the case study questions individually and submitted their answers through an online discussion board on Canvas (the school’s e-Learning management system). Then, they participated in the small-group case study session. The student-led case study session took 45 mins, during which the student group took the lead on solving the clinical case. During this time, faculty facilitators were instructed not to intervene or teach the problem-solving process, but rather to observe, guide, and ask thought-provoking questions, and redirect the conversation when it lost focus. A different student leader is selected for each small-group session to facilitate the progress of the case study.
Data Collection and Procedure
The study data came from four sources: (1) students’ quiz scores at the end of the curriculum; (2) students’ quiz taking time; (3) students’ final course grades from the proceeding MD course Basic Principles of Human Biology, and (4) students’ survey response on the experience and perceived value of simulation integration. The 2018 participating students’ quiz scores, quiz taking time, Basic Principles final grades, along with the data from the previous two cohorts were retrieved from the school’s secure exam system Examsoft (www.examsoft.com), and the 2018 MD1 students’ survey response data were collected through the school’s Learning Management System Canvas (www.instructure.com). The cardiovascular physiology quiz consisted of 10 questions, covering 10 cardiovascular physiology concepts of interest. The same set of concepts from the quiz questions were administered to 2016, 2017, and 2018 cohorts of Year 1 MD students at the conclusion of the cardiovascular physiology curriculum, which allowed consistent measures of learning outcomes across three cohorts of students.
A 15-item post-simulation evaluation survey gauging students’ learning experiences and their perceived value of the simulation-integrated curriculum was administered. Specifically, three dimensions of the perceived value of the simulation-integrated curriculum were asked: perceived learning experience which included relevant aspects such as motivation, enjoyment and engagement; perceived value in medical learning which included aspects such as retention, concept understanding, communication, and clinical reasoning; and overall perceived value. The survey items were first brainstormed by the research team to identify the original intention of the simulation integration and the desired class experience. The survey underwent two rounds of revisions after an external review by the simulation director and the Organ System II course director before implementation. The students rated each Likert-scaled survey item from strongly disagree (1 point) to strongly agree (5 points). The survey was administered at the end of the fall semester of 2018, 2 months after the conclusion of the simulation-integrated cardiovascular physiology curriculum, for the purpose of measuring more lasting experience feedback and perceived value from the students.
Statistical Analysis
The impact of this simulation integration into the cardiovascular physiology curriculum was evaluated by comparing the students’ testing results of this year 2018 cohort to those from the previous two cohorts of students (2016 and 2017 cohorts), controlling for the course grades from Basic Principles of Human Biology. Collected data were tabulated and imported into SPSS 23 and then statistically analyzed. Regression models were computed after the statistical assumptions for each model are tested and satisfied. The survey results were reported descriptively with mean scores for each survey item.
Results
Altogether, 294 students’ testing data including 101 students from the 2018 cohort, 101 students from the 2017 cohort, and 92 students from the 2016 cohort were analyzed in this study. The study results were reported below from three aspects: (1) students’ cardiovascular physiology concept mastery; (2) students’ test response time, and (3) students’ learning experience and perceived value of the simulation integration.
Students’ Cardiovascular Physiology Concept Mastery
As Levene’s Test of Homogeneity of Variance was statistically significant (F=26.214, p<0.000), the students’ test scores were transformed into a binary variable. Concept mastery was determined with the full quiz score coded as “1” and partial scores coded as “0”. Table 1 presents the partial and full concept mastery distribution across the three study cohorts. A logistic regression model with student cohorts and their Basic Principles of Human Biology (BP) scores were entered into the model as predictors. The results showed that when comparing the 2018 and 2017 cohorts, BP course scores were not a significant predictor for concept mastery. By contrast, the cohort itself was a significant predictor. Holding BP grades at a fixed value, the odds of achieving full cardiovascular physiology concept mastery for 2018 MD1 students (cohort=1) over 2017 students (cohort=0) was 4.068. In other words, the odds for 2018 cohort students to achieve full concept mastery was 306% higher than the students in the 2017 cohort. Table 2 shows the logistic model statistics. Similar results emerged when comparing the students’ performance of the 2018 cohort with that of the 2016 cohort. While the BP score was not a significant predictor of students’ cardiovascular concept mastery, the odds of achieving full concept mastery for 2018 MD1 students over 2016 MD1 students is 4.319. Overall, the results suggested that 2018 MD1 students who had experienced this simulation-integration cardiovascular physiology curriculum had a significantly higher probability of achieving full concept mastery. Table 3 shows the associated logistic model statistics.
 |
Table 1 Concept Mastery Distribution Across Three Study Cohorts |
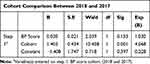 |
Table 2 Logistic Model: Effects of Basic Principles (BP) Score and Cohort (2018 Vs 2017) on Concept Mastery |
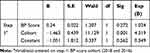 |
Table 3 Logistic Model: Effect of BP Score and Cohort (2018 Vs 2016) on Concept Mastery |
Students’ Test Response Time
Comparisons among average test-taking time for each individual test item showed that students in the 2018 cohort took the least amount of time to answer each of the 10 test items. Figure 2 illustrates the average test-taking time for each test item among these three cohorts of students (in seconds).
 |
Figure 2 Individual quiz item response time across cohorts. |
Again, Levine’s test was significant (F= 12.429, p<0.001) for the test-taking times among the three cohorts. The non-parametric Kruskal–Wallis test was performed to identify the differences among groups, followed by a Mann–Whitney test for between-group comparisons with Bonferroni correction for multiple comparisons. The test results showed a significant difference in test-taking time among these three cohorts of students (chi-square=102.672, p<0.001), with a mean rank score of 79.49 s spent per test item for the 2018 cohort, 193.40 s for the 2017 cohort, and 171.78 s for the 2016 cohort. Follow-up Mann–Whitney tests with Bonferroni corrections showed that 2018 students took significantly less time to complete the cardiovascular physiology test when compared to the 2016 students (z=−8.148, p<0.001) and 2017 students (z =−9.041, p=0.000), respectively.
Students’ Feedback on Learning Experience
Out of 101 students in the 2018 cohort, 45 students completed the survey with a response rate of 44.5%. The results showed that first-year MD students reported a positive learning experience (M=4.41) from the simulation-integrated cardiovascular physiology curriculum. Furthermore, the students reported the well-perceived value of the simulation-integrated curriculum in medical learning (M=4.20) and more future integration (M=4.17). Table 4 presents the detailed results of the learning experience evaluation and perceived value.
 |
Table 4 Student Perceived Value of Simulation-Integrated Cardiovascular Physiology Curriculum |
Discussion
This paper reported the approach and the results of integrating high-fidelity simulation into a cardiovascular physiology curriculum. Our three-pronged simulation-curriculum integration approach, which included case introduction, case development, and case studies, sketched a preliminary repeatable model with an increasing level of conceptual complexity for future iteration and improvement. The methodology identified the immediate and potential teaching values of integrating simulation into the curriculum. The comparison of learning outcomes reflected in the students’ quiz scores showed that after the simulation integration, the 2018 cohort of MD1 students displayed significant improvements in concept mastery compared with the previous two counterpart cohorts after controlling for individual differences measured by their preceding course scores. Student test-taking time was also significantly reduced compared to MD1 students in the previous two cohorts. Furthermore, the post-evaluation data indicated that the simulation-integrated curriculum brought a meaningful and enjoyable learning experience, and students realized the intended value of simulation integration into their medical education. These findings are consistent with prior research reports that integrating simulation in a preclinical curriculum is beneficial for medical students.3,4,9–11
Study Limitations
There are some limitations to this simulation-integration effort. First, we want to caution the interpretation of the significantly improved student learning outcomes compared to the last two cohorts of MD1 students, controlling for the preceding course grade. As the study is not randomized, the causal relationship was not directly established. Because these factors were obtained at one point of time, we also could not determine their temporal association with the overall perceived positive value or outcomes. Second, the study used cardiovascular quiz scores which measured 10 cardiovascular concepts as learning outcomes. Although all three cohorts of MD1 students were tested by the same set of concepts or questions, the quiz itself is not quite a comprehensive testing of the mastery of the full range of cardiovascular concepts. Third, given the fact that the experience survey was administered 2 months after the simulation integration and via Internet invitation, the students were focused on other curriculum contents, and the survey response rate was 44.5%, which though was an adequate sample size to capture the overall range of feedback, can run the risk of biased sampling. Fourth, the intervention is designed to increase earlier clinical exposure, enhance basic science concept mastery, and clinical reasoning. In this paper, we detailed the approach to enhance basic science concept mastery and clinical reasoning and presented the curriculum outcomes from concept mastery, test-taking time, and student feedback. The 2018 students’ written answers to the case study questions in Element C-Activity One can serve as a data source. Currently, the authors are developing and validating the scoring rubrics to measure clinical reasoning skills. Although in the design of the intervention, clinical reasoning was intentionally integrated and executed in Element B and Element C, this study lacked direct measurement of students’ clinical reasoning outcome data.
Educational Implications
Despite the above limitations, these preliminary observations underscore the need for further evaluation of the relative role of this MD1 integrated curriculum enhancement approach in cardiovascular physiology as an attractive model that could be expanded to not only other groups of learners but also to other pathophysiologic conditions or disease processes. This is our first endeavor of simulation integration into a cardiovascular physiology curriculum to enhance clinical reasoning, clinical exposure, and cardiovascular concept mastery. There may be similar opportunities in other aspects of the curriculum where we can leverage more clinical cases and technologies to further enhance learning. The three elements articulated in this simulation-curriculum integration (case introduction + case-development + student-centered small-group case study) have the potential to serve as a testing model to integrate simulation in a broader basic science curriculum with a succession of added complexities and students’ independence. Expanding to subjects such as pharmacology, microbiology and pathophysiology in a systematic way can generate further empirical evidence to better inform future simulation-enhanced educational endeavors.
The simulation-curriculum integration in the large classroom setting indicated its capacity to accommodate a diverse body of medical students with varied levels of academic standing. At-risk learners can benefit from contextualized learning, guided, iterative basic science concept review, and clinical reasoning. Advanced learners can particularly benefit from earlier clinical setting exposure, standardized patient encounter modeling, debriefing, and independent case study. Students’ high level of enthusiasm and acceptance validated its meaningful incorporation into educational curricula to build a solid foundation for their future success as physicians. It may also serve as an illustrative case and methodology to bridge existing gaps between medical education, technology, teaching methodologies, and outcomes.
Conclusion
This simulation integration in a cardiovascular physiology curriculum provides an empirical case and approach to integrating basic science curricula, simulation technology, and varied teaching methods to achieve desirable medical learning outcomes and experiences.
Acknowledgments
Many people have contributed to this ongoing project. We especially thank the staff at the Office of Digital Learning (ODL), especially Ms. Allison Legister, Michelle McIver, and N’Dieye Danavall for coordinating and providing technical solutions. The authors also appreciate the work of Dr. Fung Yu mei and the staff at the Clinical Skills Center for iSTAN setup.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40(3):254–262. doi:10.1111/j.1365-2929.2006.02394.x
2. Elisseou S, Puranam S, Nandi M. A novel, trauma-informed physical examination curriculum for first-year medical students. MedEdPORTAL. 2019;15:10799. doi:10.15766/mep_2374-8265.10799
3. Tan G, Ti L, Suresh S, Ho B, Lee T. Teaching first-year medical students physiology: does the human patient simulator allow for more effective teaching? Singapore Med J. 2002;43(5):238–242.
4. Gordon J, Brown D, Armstrong E. Can a simulated critical care encounter accelerate basic science learning among preclinical medical students? A pilot study. Simul Healthc. 2006;1(Inaugural):13–17. doi:10.1097/01266021-200600010-00005
5. McGaghie W, Issenberg S, Cohen E, Barsuk J, Wayne D. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86(6):706–711. doi:10.1097/acm.0b013e318217e119
6. McGaghie W, Issenberg S, Petrusa E, Scalese R. A critical review of simulation-based medical education research: 2003–2009. Med Educ. 2010;44(1):50–63. doi:10.1111/j.1365-2923.2009.03547.x
7. Harris DM, Ryan K, Rabuck C. Using a high-fidelity patient simulator with first-year medical students to facilitate learning of cardiovascular function curves. Adv Physiol Educ. 2012;36(3):213–219. doi:10.1152/advan.00058.2012
8. Issenberg B, McGaghie W, Petrusa E, Lee Gordon D, Scalese R. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi:10.1080/01421590500046924
9. Okuda Y, Bryson E, DeMaria S, et al. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med. 2009;76(4):330–343. doi:10.1002/msj.20127
10. Prince K, Boshuizen H, van der Vleuten C, Scherpbier A. Students’ opinions about their preparation for clinical practice. Med Educ. 2005;39(7):704–712. doi:10.1111/j.1365-2929.2005.02207.x
11. McKinney J, Cook D, Wood D, Hatala R. Simulation-based training for cardiac auscultation skills: systematic review and meta-analysis. J Gen Intern Med. 2012;28(2):283–291. doi:10.1007/s11606-012-2198-y
12. Mueller MP, Christ T, Dobrev D, et al. Teaching antiarrhythmic therapy and ECG in simulator-based interdisciplinary undergraduate medical education. Br J Anaesth. 2005;95(3):300–304. doi:10.1093/bja/aei174
13. Nguyen K, Khallouq BB, Schuster A, et al. Developing a tool for observing group critical thinking skills in first-year medical students: a pilot study using physiology-based, high-fidelity patient simulations. Adv Physiol Educ. 2017;41(4):604–611. doi:10.1152/advan.00126.2017
14. Gordon J, Hayden E, Ahmed R, Pawlowski J, Khoury K, Oriol N. Early bedside care during preclinical medical education: can technology-enhanced patient simulation advance the flexnerian ideal? Acad Med. 2010;85(2):370–377. doi:10.1097/acm.0b013e3181c88d74
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
