Back to Journals » Infection and Drug Resistance » Volume 15
Incidence, Prophylaxis and Prognosis of Acute Postoperative Endophthalmitis After Cataract Surgery: A Multicenter Retrospective Analysis in Northern China from 2013 to 2019
Authors Jiang X, Wan Y, Yuan H, Zhao L, Sun M, Xu Y, Xin X, Dong J, Hu D, Chen D, Li X
Received 10 August 2021
Accepted for publication 20 July 2022
Published 27 July 2022 Volume 2022:15 Pages 4047—4058
DOI https://doi.org/10.2147/IDR.S332997
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Xiaodan Jiang,1,2,* Yu Wan,1,2,* Hao Yuan,1,2,* Liming Zhao,3,* Min Sun,4,* Yanhui Xu,5,* Xiangyang Xin,6,* Jing Dong,7,* Die Hu,8,* Dongmei Chen,9,* Xuemin Li1,2
1Department of Ophthalmology, Peking University Third Hospital, Beijing, People’s Republic of China; 2Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Peking University Third Hospital, Beijing, People’s Republic of China; 3Department of Ophthalmology, Beijing Fengtai Hospital, Beijing, People’s Republic of China; 4Department of Ophthalmology, Huabei Petroleum General Hospital, Renqiu, Hebei, People’s Republic of China; 5Department of Ophthalmology; Hebei Provincial Eye Hospital, Xingtai, Hebei, People’s Republic of China; 6Department of Ophthalmology, Inner Mongolia Baogang Hospital, Baotou, Inner Mongolia, People’s Republic of China; 7Department of Ophthalmology, the First Affiliated Hospital of Baotou Medical College, Baotou, Inner Mongolia, People’s Republic of China; 8Department of Ophthalmology, Baoding Zhuozhou GEM Flower Hospital, Zhuozhou, Hebei, People’s Republic of China; 9Department of Ophthalmology, Baoding GEM Flower Eastern Hospital, Zhuozhou, Hebei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xuemin Li, Department of Ophthalmology, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Peking University Third Hospital, No. 49 Huayuan North Road, Haidian District, Beijing, 100191, People’s Republic of China, Tel +86 10 8226 6312, Fax +86 10 8208 9951, Email [email protected]
Objective: To investigate the incidence of acute postoperative endophthalmitis (POE) after cataract surgery in Northern China from 2013 to 2019, evaluate the efficacy of prophylaxis and analyze the predictors of visual prognosis among POE patients.
Methods: The study was conducted as a retrospective multi-center research, with seven hospitals in Northern China enrolled. The diagnosis of acute-onset POE was made on the basis of clinical manifestations within six weeks after initial surgery. By reviewing electronic medical system, the number of cataract surgeries and acute POE cases were recorded to estimate the overall incidence and incidences by different years and hospitals. Perioperative measures for preventing infection in different hospitals were collected. The correlations between unfavorable final vision and potential factors including basic information and clinical characteristics were examined to determine the predictive factors for final visual prognosis.
Results: Of 72,255 cataract surgeries performed during seven years in the seven hospitals, 19 cases developed acute POE, yielding an overall incidence of 0.026%. The average incidence of acute POE among seven hospitals significantly declined annually during the past 7 years (p = 0.021). In Hospital-D, the incidence of acute POE significantly decreased after the application of 0.5% povidone-iodine (PVP-I) for conjunctival washing (p = 0.003). Two hospitals adopting tobramycin in the irrigation solution achieved a significant lower incidence of POE than the other hospitals (p = 0.044). The positive rate of pathogen culture was just 17.6% (3/19). Patients with presenting BCVA of CF or better were more likely to present with unfavorable final vision than those with worse presenting BCVA (p = 0.003).
Conclusion: The overall incidence of acute POE after cataract surgery from 2013 to 2019 in Northern China was 0.026%, and the incidence declined annually over the period. Presenting BCVA could be a significant prognosis factor for predicting the final visual outcomes of acute POE patients.
Keywords: endophthalmitis, cataract surgery, infection prophylaxis, prognosis predictors
A Letter to the Editor has been published for this article.
Introduction
Cataract is globally considered as the most prevalent cause of visual impairment,1 and cataract surgery with an intraocular lens2 implantation has become a very commonly performed ophthalmic surgical procedure in the world.3 In China, the largest developing country with nearly 1.4 billion people, cataract surgical rate has increased to 2662 cases per one million per year by 2020 (statistics reported by the Ministry of Health of PR China (http://www.moheyes.com)).4 Therefore, it is of much significance to avoid the occurrence of operation complications. Currently, with more mature surgical technique, complications of cataract surgery have been relatively rare. However, postoperative endophthalmitis (POE), which is caused by postoperative infection, remains a devastating complication with severe vision loss and extremely poor visual prognosis. According to previous studies,5,6 nearly half of POE patients achieved best corrected visual acuity (BCVA) worse than 20/400 at the final follow-up visit, and a few patients eventually developed blindness. Moreover, some patients had to receive eyeball enucleation in order to prevent intraorbital and intracranial infection.7 Consequently, POE is regarded as the most horrible nightmare for cataract surgeons.
Due to the rarity and severity of POE, it is essential for surgeons to figure out the incidence of POE after cataract surgery in their own regions, thereby being sensitive and keeping alerting to the occurrence of POE. On the basis of recent large-scale studies, incidence of POE after cataract surgery ranged from 0.03% to 0.15% worldwide.6,8–11 However, most of these investigations were conducted in developed countries. Based on a literature review by Sheng et al, several small-scale and single-center studies investigated the incidence of POE after cataract surgery in China from 1995 to 2009, yielding different incidences varying from 0.02% to 0.4%.12 Nevertheless, in the past ten years, Chinese health care has been rapidly developed, operation method and incision type of cataract surgery has been greatly changed, which all could exert huge impacts on the incidence of POE. On the one hand, povidone iodine (PVP-I), a broad-spectrum antiseptic compound, has been preoperatively applied widespread in cataract surgery,13 and the choice of perioperative prophylactic antibiotics has been enriched, which might reduce the risk of POE. On the other hand, the wide use of clear corneal incisions and sutureless technique may contribute to the instability of the incision and increase the risk of POE.14–16 With millions of cataract surgeries performed in China every year, even a small change in the incidence of POE could have significant impacts on a population basis. Taking these into consideration, it is also necessary to update our insight into the occurrence of POE after cataract surgery in recent China.
Therefore, we conducted this large-scale multicenter research with seven hospitals enrolled, to determine the incidence of acute POE after cataract surgery from January 1, 2013 to December 31, 2019 in Northern China. Additionally, our research also aimed to explore the effectiveness of perioperative measures for infection prevention and evaluate the potential prediction factors for final visual prognosis.
Methods
Study Population and Data Collection
The study was designed as a retrospective multi-center research. It was approved by Peking University Third Hospital Medical Science Research Ethics Committee and conformed to the tenets of the Declaration of Helsinki. Seven hospitals from five different regions in Northern China (Beijing, Xingtai, Baotou, Cangzhou and Zhuozhou) were enrolled, including the Peking University Third Hospital (Hospital-A), the Hebei Provincial Eye Hospital (Hospital-B), the Inner Mongolia Baogang Hospital (Hospital-C), the Huabei Petroleum General Hospital (Hospital-D), the Baoding Zhuozhou GEM Flower Hospital (Hospital-E), the First Affiliated Hospital of Baotou Medical College (Hospital-F) and the Baoding GEM Flower Eastern Hospital (Hospital-G). The number of cataract surgeries and patients who were diagnosed with acute POE within six weeks after cataract surgery between January 1, 2013 and December 31, 2019 were recorded by reviewing the electronic medical records in the seven hospitals. Meanwhile, demographic information, clinical characteristics and follow-up results of acute POE patients were also collected for further analysis.
Cataract surgery in our research included phacoemulsification (PHACO) and extracapsular cataract extraction (ECCE) with IOL implantation. Patients who underwent combined surgical procedures, such as cataract surgery combined with penetrating keratoplasty, trabeculectomy or vitrectomy were excluded, for the incidence of endophthalmitis after these combined procedures was proven to be higher.8,11 The diagnosis of acute-onset postoperative endophthalmitis was mainly made on the basis of clinical manifestations, including worsening visual acuity, complaint of ocular pain and signs of intraocular inflammation (kerato-precipitates, anterior chamber fibrin exudation or hypopyon) within six weeks after initial surgery. The diagnosis in all cases was determined by two or more experienced doctors. Patients with suspected endogenous endophthalmitis or traumatic endophthalmitis were excluded from our study.
The treatments in our study largely followed the Endophthalmitis Vitrectomy Study (EVS) guidelines,7 which provided optimal management for POE. All POE patients received intravitreal injection of vancomycin or vancomycin combined ceftazidime as the main initial treatment. According to the EVS guidelines, pars plana vitrectomy (PPV) was not routinely required and mainly recommended to be performed in the cases with VA of light perception. However, patients with VA of hand motions or better might also undergo PPV if intraocular inflammation was proven persistent and VA worsened dramatically. During the course of management, vitreous humor or aqueous fluid samples were obtained by needle aspiration or vitrectomy, and then microbiologically cultivated to identify the specific pathogen. Samples were cultured in blood agar, chocolate agar or thioglycolate broth, which were all incubated at 37°C for bacterial growth and anaerobic condition for anaerobe culture. Room-temperature cultures on Sabouraud agar without cycloheximide were used to grow fungi. A positive culture was defined as growth of an organism on two or more media, or confluent growth on any solid medium. For the assessment of infection prophylaxis, detailed pre-, intra- and post-operative measures for preventing infection in seven hospitals were collected for analysis.
In summary, the data collected from patients with acute-onset endophthalmitis after cataract surgery included: demographic characteristics (age, gender, systemic disease), the information about initial operation (hospital, type and incision of cataract surgery, intraoperative complications), postoperative endophthalmitis (onset date of endophthalmitis, time interval from initial surgery to onset, BCVA on presentation, management, microculture results) and follow-up data (final BCVA, follow-up time). Two reviewers (JXD and WY) independently scanned the electronic medical information and collected the records of each acute POE patient. To ensure the accuracy of the data, the third reviewer (YH) subsequently checked the information and solved the disagreements through discussion.
Statistical Analysis
SPSS statistics software version 25 (SPSS, Inc., Chicago, IL, USA) was used for data analysis. The overall incidence of acute-onset endophthalmitis after cataract surgery in seven centers was calculated with its 95% confidence intervals (CIs), as well as the incidences among different years and centers. Chi-square test and Fisher’s exact test were performed to compare the incidences among groups. The Mantel–Haenszel test was applied to examine the changing trend of annual incidences. The demographic information, clinical characteristics and final VA outcomes of POE patients were tabulated and descriptively analyzed.13 According to the standards for characterization of vision loss updated by WHO (World Health Organization) in 2003, we set criteria that the unfavorable vision was considered as final BCVA was less than 20/400 in POE cases. Fisher's exact test was applied to determine the potential predictive factor for the prognosis of visual acuity. A p value less than 0.05 was considered statistically significant.
Results
Incidences of Endophthalmitis
From January 1, 2013 to December 31, 2019, a total of 72,255 cataract surgeries with IOL implantation were performed in the seven hospitals. The average cataract operation volume was 10,322 per year. During the seven-year period, 19 eyes of 19 patients developed acute POE within six weeks after initial surgery. Hence, in our research, the overall incidence of acute endophthalmitis after cataract surgeries from 2013 to 2019 in Northern China was 0.026% (19/72,255, 95% CI 0.015% to 0.038%).
The annual number of cataract surgeries and occurrence rate of postoperative endophthalmitis are presented in Table 1 and Figure 1. Taken together, the number of cataract surgeries in the seven hospitals raised year by year. However, the annual incidence of acute POE showed markedly declining tendency over the period (p=0·021 for Mantel–Haenszel test), from 0.056% (4/7207, 95% CI 0.001% to 0.110%) in 2013 to 0.007% (1/13,844, 95% CI 0 to 0.021%) in 2019.
 |
Table 1 Incidence of Acute POE Among Different Years and Hospitals |
The incidence of POE in each hospital is also demonstrated in Table 1. Among the seven hospitals, Hospital-F presented with the highest incidence with a proportion of 0.196% (5/2555, 95% CI 0.024% to 0.367%). Apart from Hospital-F, the incidences in all the other six hospitals were within 0.04 per 100 cataract surgeries. Particularly, there were no reported postoperative endophthalmitis cases among 454 procedures in Hospital-E and 371 procedures in Hospital-G.
Perioperative Infection Prophylaxis
The detailed information of perioperative infection prophylaxis is shown in Table 2. To prevent the occurrence of infection, pre- and post-operational topical antibiotics (levofloxacin, gatifloxacin or tobramycin), and intraoperative ophthalmic ointment containing tobramycin and dexamethasone were routinely applied in seven hospitals. Different concentrations of PVP-I were applied for conjunctival washing in all the centers, and especially, two centers (Hospital-A and F) brought PVP-I into use just during our investigation period (Hospital-A in January 1, 2017 and Hospital-F in January 1, 2016). For this reason, we compared the incidences of POE before and after the usage of PVP-I in the two hospitals, intending to evaluate the preventive effectiveness of PVP-I on the occurrence of endophthalmitis by before-after self-control methods. Our results revealed that the incidence of POE significantly decreased in Hospital-F (0.6435% vs 0; p=0.003) after the application of 0.5% PVP-I, while no remarkable difference was observed since 5% PVP-I was applied in Hospital-A (0.0364% vs 0.0129%; p=0.29). In addition, only two hospitals added antibiotics in the irrigation solution: 4mg/1000mL tobramycin was used in Hospital-B and 8mg/1000mL tobramycin was used in Hospital-E. Interestingly, they presented with a significant lower incidence than the other hospitals where no antibiotics were administrated in the irrigation solution (0.0126% vs 0.0371%; p=0.044).
 |
Table 2 Perioperative Infection Prophylaxis in Each of Hospitals |
Clinical Characteristics and Visual Outcome
There were totally 19 eyes of 19 patients from five hospitals developed postoperative endophthalmitis in the seven years. Their demographic characteristics and information about initial operation were shown in Supplementary material (eTable 1). The mean age of endophthalmitis patients was 69.4 years (median 71, range 26–83). There were ten males (52.6%) and nine right eyes (47.4%). Sixteen patients (84.2%) reported the history of systemic disorders, and ten of them (52.6%) suffered diabetes mellitus. Phacoemulsification was performed in 18 cases (94.7%) and ECCE was underwent in only one case (5.3%). The operative incisions included eleven clear cornea incisions (57.9%), seven limbus tunnel incisions (36.8%) and one scleral tunnel incision (5.3%). Intraoperative complication was observed in only one case (5.3%) with the rupture of posterior capsule.
Clinical features, management, culture results and visual outcomes were shown in Supplementary material (eTable 2). The average time interval from initial surgery to endophthalmitis was 5.4 days (median 4, range 1–20), with 16 patients (84.2%) diagnosed within one week after the operation. At the onset of endophthalmitis, the best BCVA presented was 20/70 and only four patients (21.1%) achieved BCVA better than CF. For the management, intravitreal and intravenous antibiotics were applied in all patients, including vancomycin only in 12 patients (63.2%) and vancomycin combined ceftazidime in seven patients (36.8%). PPV was performed in ten patients (52.6%). Intraocular specimens were collected from 17 patients (89.5%), of which 15 were sampled from aqueous humor and nine were sampled from vitreous fluid. However, with only three culture-positive cases, the positive rate of pathogen culture was just 17.6% in our study. Staphylococcus hominis was isolated in two cases and Streptococcus was cultured in one case.
After the exclusion of four patients who were lost to follow up, final BCVA was obtained from the remaining 15 patients and the average follow-up time was 4.3 months (median 1, range 1–22). To explore the predictors of final visual outcome, final BCVA were calculated and compared based on each potential prognostic factor in Table 3, including sex, age, diabetes mellitus, time to onset of endophthalmitis, presenting BCVA, antibiotics, PPV and culture results. Only presenting BVCA was found to be significantly associated with the final BCVA. Patients with presenting BCVA of CF or better were less likely to present with unfavorable final vision than those with presenting BCVA of HM or worse (p=0.046).
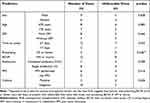 |
Table 3 Analysis of Potential Prognostic Factors for Final Visual Outcome in POE Patients |
Discussion
As the first large-scale multicenter survey on the incidence and clinical characteristics of acute POE after cataract surgery in Northern China, our research identified four key findings. Firstly, with 72,255 cataract surgical procedures performed in 7 hospitals between 2013 and 2019, the overall incidence of acute POE after cataract surgery in our investigation was 0.026%. Secondly, the average incidence of acute POE after cataract operation markedly decreased annually during this 7-year period, from 0.056% in 2013 to 0.007% in 2019. Thirdly, final visual outcomes of acute POE patients were generally poor, and presenting BCVA of CF or better could be a potential prognosis factor for predicting the final visual acuity. Moreover, under the pandemic of COVID-19, many experts have proposed the possible change in the incidence of acute POE after cataract surgery.17 The alterations in expiratory airflow and possibly bacterial dispersion with patient mask use during operation might increase the risk of POE, but on the opposite, additional infectious control precautions such as room sterilization, air filtration and more strict observance to sterile technique could avoid the occurrence of POE.17 Our results provided the incidence and clinical features of POE patients before the pandemic, which could be used to compare with those after COVID-19 outbreak.
As summarized in Supplementary material (eTable 3), several previous studies have investigated the incidence of acute POE after cataract surgery in different regions of China, ranging from 0.01% to 0.15%,5,12,18–21 and our incidence was just within this range. However, the incidences in these studies differed obviously, which might be attributed to the varied studied regions. Lin et al.5 Sun et al22 and Wu et al19 explored the incidence of POE after cataract surgery in a single eye center, while Lin et al and Sun et al concluded much lower incidences with higher annual mean surgery volume than Wu et al. One possible explanation is that higher surgical volume generally represents higher-level hospitals with advanced equipment, well-trained surgeons, and standard infection prophylaxis, which could thus avoid the occurrence of postoperative infection.21 The explanation was also verified in two previous multicenter studies by Yao et al18 and Zhu et al.21 With only eight top eye centers in China enrolled, the occurrence rate of POE in Yao’s study was far lower than Zhu’s study that only sampled 30 small-scale departments of ophthalmology whose cataract surgery volume was under 100 cases per month. However, in our research, two small-scale hospitals (Hospital-E and G) whose cataract surgery volume was less than 100 cases per year did not show higher risk of POE, and even no cases of POE were reported. The conflict might be due to the instability caused by small sample size in the two small eye centers and higher rate of missed diagnosis led by low postoperative follow-up rate in small-scale hospitals. Therefore, on account of the potential higher risk of POE in small hospitals, much more effort should be made to improve the sanitary conditions and prophylaxis standards in these small eye centers which actually represented the general medical treatment level in the majority regions of China. On the other hand, we could conclude that the incidence of POE differed widely due to the geographic variations, and thereby it is necessary to investigate the specific incidence in different regions. Taking this into consideration, our study firstly revealed the incidence of acute post-cataract surgery endophthalmitis in Northern China, and found it was moderate when compared with previous studies in China. This result was of great benefit for ophthalmologists in Northern China to figure out the status of POE in their own region and thus be sensitive enough to POE after cataract surgery.
Additionally, another major finding of our study was the growing number of cataract surgery and the decreasing incidence of acute POE after cataract surgery in recent Northern China. With fast aging process of population and extensive development of surgical technique, there is no doubt that a continual increasing trend could be observed on the number of cataract surgery. However, it has always been debated that how the occurrence rate of acute POE after cataract surgery changed in the last few years. To answer this controversial question, we revealed that the incidence of acute POE after cataract operation actually decreased annually during this 7-year period in Northern China, from 0.056% in 2013 to 0.007% in 2019. The majority of studies in other regions yielded similar conclusions.2,11 Although most of recent studies showed a falling trend of the incidence of POE after cataract surgery, cataract surgeons have to bear in mind that the occurrence of POE is actually under combination action of multiple factors which often differ among regions, and we suggest that it is essential to investigate the trend of incidence in specific regions.
Effective perioperative measures for preventing infection play a key part in avoiding the occurrence of POE. Among all the anti-infection practice, povidone-iodine is the only one recommended by level I evidence,23,24 and there has already been global general consensus to use PVP-I preoperatively for preventing POE. In our study, 2 hospitals coincidentally started to apply PVP-I for conjunctival washing in place of BBS during the period of research, providing us the opportunity to evaluate the effectiveness of PVP-I by before-after self-control methods. In Hospital-F, a dramatic decline of incidence was observed after the application of 0.5% PVP-I since 2015. Without strict controlling of confounding factors, we cannot rule out the possibility that the decline was actually a result of multiple associated factors instead of PVP-I only, including operation methods, incision type and surgical technique. However, considering such a dramatical decrease of the incidence after PVP-I application (from 0.64% in 2013–2015 to 0 in 2016–2019), we still believed that the more effective preoperative disinfection from 0.5% PVP-I application was the leading cause. Interestingly, with a higher concentration, 5% PVP-I did not lead to a significant decrease in the incidence of POE in Hospital-A. A similar conclusion was drawn in a previous study, demonstrating that diluted PVP-I (0.1–1%) was more rapidly bactericidal than a full-strength solution (10%).25 One hypothesis was that the concentration of free iodine significantly increased when diluted and contributed to the bactericidal activity.25 Due to the toxicity of PVP-I to the corneal epithelium and endothelium, the Chinese Cataract Society has recommended a low concentration application of PVP-I before cataract operation.26 Here, our results also supported that 0.5% PVP-I was already beneficial for POE prophylaxis for effectively reducing the risk of POE, which was consistent with the conclusion in Rosario’s study.27 It seems that a low concentration PVP-I might realize financial savings as well as improved antisepsis at the same time, which is worth promoting. However, further large-scale randomized controlled trials were needed to evaluate the optimum concentration of PVP-I.
Moreover, it is worth noting that only two centers applied intraoperative antibiotics that added tobramycin in irrigation solutions (4mg/1000mltobramycin in Hospital-B and 8mg/1000mL tobramycin in Hospital-E), and they presented with a significant lower incidence than all the other centers. A previous study by Sobaci et al investigated bacterial contamination rates of aqueous humor samples taken at the end of cataract operation, and they found that intraoperative antibiotic irrigation group (20 micrograms/mL vancomycin and 8 micrograms/mL gentamicin) could significantly decreased the rates of culture-positivity than BSS-only group, indicating the effectiveness of antibiotic irrigation in preventing intraocular bacterial contamination during cataract surgery.28 Whereas, the lower incidence of POE in the two hospitals should be analyzed by logistic regression because of many confounding variables including patients’ age, basic disease, incision type, capsule rupture and topic antibiotics. However, due to the operation limitation of medical records system, only POE patients’ medical information could be completely acquired, and we could not obtain relevant information from the other patients. Without strict controlling of confounding factors, we cannot rule out the possibility that the decline was actually a result of multiple associated factors instead of tobramycin only. Considering the lack of robustness, it should be emphasized the popularization of tobramycin in irrigation should be very cautious and multivariate analysis should be conducted in further research. Actually, since the intracameral injection of cefuroxime (1mg) at the close of cataract surgery was recommended by European Society of Cataract & Refractive Surgeons (ESCRS) multicenter study,29 intracameral cefuroxime has been introduced to be a standard prophylactic intervention in Western countries. A Spanish study observed a dramatic drop of approximately 15-fold in POE rates after using intracameral cefuroxime,30 and a meta-analysis conducted by Wang et al revealed that anterior chamber injection of moxifloxacin could effectively prevent the occurrence of endophthalmitis after cataract surgery.31 However, in China, the application of intracameral antibiotic injection in cataract surgery is controversial and not widely promoted in most regions, mainly due to the lack of commercialized products and some devastating complications including hemorrhagic occlusive retinal vasculitis.32,33 Hence, we propose that antibiotic irrigation might be an alternative method to replace intracameral cefuroxime with a similar mechanism, and a further study could be conducted to compare the effectiveness and safety between the two methods.
The time interval from initial surgery to the onset of endophthalmitis plays an essential role in the prevention and diagnosis of POE. In our research, nearly half of POE patients (9/19, 47.4%) developed symptoms of endophthalmitis with three days after the operation, and a majority of patients (16/19, 84.2%) did within one week after initial surgery. This result suggested that the time interval within three days to one week after cataract surgery was a high-risk period for onset of acute POE, when surgeons should keep alert to the occurrence of POE and patients should be closely followed up. Regardless, there were still three patients suffering POE at 11, 16 and 20 days after operation, respectively. Therefore, surgeons should bear in mind the possibility of delayed onset of acute POE to avoid misdiagnosis. However, most hospitals in China only routinely apply postoperative prophylactic antibiotics therapy within two weeks after cataract operation, and some patients are even lost to follow up after two weeks.18,21 Considering this, we propose that postoperative topical antibiotics should be strictly administrated for at least two weeks after cataract surgery in patients with risk factors like wound leak and PCR, to cover the potential incubation period of acute POE, and those patients should be closely followed up during this period.
Identification of the causative organism by culturing intraocular samples is instructive in the diagnosis and prognosis of endophthalmitis. Unfortunately, the incidence of culture positivity in our study was 17.6%, which was lower than previous investigations conducted in other regions of China.5,19,20,22 Moreover, it is worth noting that culture-positive rates reported in China as shown in Supplementary material (eTable 3) were almost lower than developed countries, such as Australia (67% reported by Lertsumitkul et al),34 the United States (69.3% in EVS)7 and Sweden (85.2% reported by Friling et al).35 One possible reason for the low culture positivity might be the non-standardized method of microbial isolates. The phenomenon that antibiotics were initially delivered prior to intraocular sampling existed in our included hospitals. Due to the administration of antibiotics, the decreased quantity of pathogen available in samples might produce only modest organism growth, leading to negative results. Therefore, to improve the identification of pathogen and promote a laboratory diagnosis of microbial infection, we recommend direct smear staining on the intraocular samples to be conducted simultaneously if possible. Meanwhile, combing culturing and staining might be another way to identify the pathogen and increase the positive rate. Ding et al found, by using the Gram, GMS, or PAS staining methods, positive smear staining results were available in 73.9% of the post-cataract surgery endophthalmitis cases, which was significantly higher than the positive-culture rate of 50%.36 Besides, more fungal infection patients could be confirmed through GMS and PAS staining than culturing.36
According to previous studies, coagulase-negative Staphylococcus (CoNS), Staphylococcus aureus and Staphylococcus epidermidis were the most common organism associated with postoperative endophthalmitis.18 In our study, Staphylococcus hominis was isolated in two cases and Streptococcus was cultured in one patient. Among CoNS species, Staphylococcus hominis was the third most frequent one and regarded as the core composition of the microbiota in the human host’s skin and mucous membrane surfaces.37 Our previous study detected Staphylococcus hominis in the conjunctival sac and meibomian gland secretions of normal subjects,38 which might explain the source of infection in the two cases and thus emphasized the importance of adequate disinfection on conjunctival sac and eyelid margin before cataract surgery. Additionally, the use of a surgical adhesive membrane to cover the orifices of meibomian glands is also essential since the secretions of meibomian glands containing bacteria might gradually contaminate the sterilized area intraoperatively and lead to POE.38 However, Staphylococcus hominis was less commonly reported than other CoNS species in endophthalmitis-associated pathogens, and it was often associated with cases of nosocomial infections.39
The final visual outcomes in our study were generally poor; only one (6.7%) of 15 patients achieved a visual acuity >20/40, and seven (46.7%) of 15 patients had a visual aacuity >0/200. This visual prognosis was comparable to Ding’s study finding only three (7.0%) of 46 patients had a final VAVA >/40 at a local hospital in Southern China.36 However, it was significantly worse than EVS which reported 53% of patients achieved 20/40 or better VA in Western countries.7 This difference may be partly explained by the exclusion criteria in the EVS. Patients presenting with VA of NLP or significant opacification of the anterior chamber were excluded from the EVS. As such, more severe infections or virulent organisms were probably excluded from the EVS analysis. In spite of this, it is unquestionable that there is still a huge lag between China and developed countries in the recognition and standardization of POE treatment, which eventually lead to the poor final visual outcome. The gap might partially result from inadequate popularization of vitrectomy, lower positive-culture rate and the lack of targeted and precise anti-infection measures. In addition, our analysis revealed that visual acuity at presentation was a good predictor of final visual prognosis in POE patients. Patients with presenting BCVA of CF or better were more likely to achieve a better final BCVA than those with worse presenting BCVA. The result was in accordance with several previous studies.5,18,19,21 Better presenting VA means the possibility of earlier disease course, or less damage to the intraocular tissue, and thus patients may have more chance to achieve a good visual outcome.
Several potential limitations in our investigation should be considered. Firstly, it is impossible for us to collect medical information from all the eye centers in the region of Northern China to yield a totally accurate incidence. However, we included the representative ophthalmic centers in different cities, and more centers would be enrolled for comprehensive assessment in the future. Secondly, due to the limitation of electric medical records, we could not obtain some relevant information from all the patients, such as surgical time, posterior capsular rupture and the type of cataract extraction and IOL. Therefore, we had no chance to completely evaluate the potential risk factors and the efficacy of preventive measures for POE after cataract surgery by multivariable analysis. Thirdly, on account of the extremely low incidence of postoperative endophthalmitis, the sample size of POE patients in our research was still limited, even though we had conducted a multicenter investigation. Hence, we could only analyze the prognosis factors by single factor methods, which could be disturbed by the confound factors. Considering all this, a better-designed large-scale multicenter investigation should be conducted in the future to estimate a more accurate incidence of POE after cataract surgery in Northern China, and assess the factors associating with the occurrence of POE and final visual prognosis.
Conclusion
As the first large-scale multicenter survey on the incidence and clinical characteristics of acute POE after cataract surgery in Northern China, we revealed that the incidence of acute POE after cataract surgery from 2013 to 2019 in Northern China was 0.026%, and the annual incidence declined significantly year by year over the 7 years. For the prognostic prediction, presenting BCVA of CF or better could be a significant predictor for the final visual acuity outcome in acute POE patients.
Ethical Statement
Due to the non-interventional nature of retrospective research and strict confidentiality of our data, patients’ consent to review their medical records was waived that was approved by the ethics committee. We declared that we would cover the privacy of the participants, and the data in our research was anonymized and maintained with confidentiality.
Acknowledgments
We gratefully acknowledge Beijing Municipal Science and Technology Commission for supporting our research; the Peking University Third Hospital, the Hebei Provincial Eye Hospital, the Inner Mongolia Baogang Hospital, the Huabei Petroleum General Hospital, the Baoding Zhuozhou GEM Flower Hospital, the First Affiliated Hospital of Baotou Medical College and the Baoding GEM Flower Eastern Hospital for providing the electrical medical information.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This project was supported by Beijing Municipal Natural Science Foundation (7202229).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lee CM, Afshari NA. The global state of cataract blindness. Curr Opin Ophthalmol. 2017;28:98–103. doi:10.1097/ICU.0000000000000340
2. Nowak MS, Grzybowski A, Michalska-Malecka K, et al. Incidence and characteristics of endophthalmitis after cataract surgery in Poland, during 2010–2015. Int J Environ Res Public Health. 2019;16(12):2188. doi:10.3390/ijerph16122188
3. Thompson J, Lakhani N. Cataracts. Prim Care. 2015;42:409–423. doi:10.1016/j.pop.2015.05.012
4. Cataract surgical rate in 2020 in China. Statistics reported by the ministry of health of PR China. Available from: http://www.moheyes.com.
5. Lin M, Zhang W, Liu Y, et al. Nosocomial acute-onset postoperative endophthalmitis at a university teaching hospital in China. J Hosp Infect. 2011;79:323–327. doi:10.1016/j.jhin.2011.07.009
6. Wykoff CC, Parrott MB, Flynn HW, Shi W, Miller D, Alfonso EC. Nosocomial acute-onset postoperative endophthalmitis at a university teaching hospital (2002–2009). Am J Ophthalmol. 2010;150:392–8.e2. doi:10.1016/j.ajo.2010.04.010
7. Johnson MW, Doft BH, Kelsey SF, et al. The endophthalmitis vitrectomy study. Relationship between clinical presentation and microbiologic spectrum. Ophthalmology. 1997;104:261–272. doi:10.1016/S0161-6420(97)30326-1
8. Pershing S, Lum F, Hsu S, et al. Endophthalmitis after cataract surgery in the United States: a report from the intelligent research in sight registry, 2013–2017. Ophthalmology. 2019;127(2):151–158.
9. Ness T, Kern WV, Frank U, Reinhard T. Postoperative nosocomial endophthalmitis: is perioperative antibiotic prophylaxis advisable? A single centre’s experience. J Hosp Infect. 2011;78:138–142. doi:10.1016/j.jhin.2011.02.004
10. Freeman EE, Roy-Gagnon MH, Fortin E, Gauthier D, Popescu M, Boisjoly H. Rate of endophthalmitis after cataract surgery in Quebec, Canada, 1996–2005. Arch Ophthalmol. 2010;128:230–234. doi:10.1001/archophthalmol.2009.380
11. Creuzot-Garcher C, Benzenine E, Mariet AS, et al. Incidence of acute postoperative endophthalmitis after cataract surgery: a nationwide study in France from 2005 to 2014. Ophthalmology. 2016;123:1414–1420. doi:10.1016/j.ophtha.2016.02.019
12. Sheng Y, Sun W, Gu Y, Lou J, Liu W. Endophthalmitis after cataract surgery in China, 1995–2009. J Cataract Refract Surg. 2011;37:1715–1722. doi:10.1016/j.jcrs.2011.06.019
13. Ahmed Y, Scott IU, Pathengay A, Bawdekar A, Flynn HW. Povidone-iodine for endophthalmitis prophylaxis. Am J Ophthalmol. 2014;157:503–504. doi:10.1016/j.ajo.2013.12.001
14. Lundstrom M, Wejde G, Stenevi U, Thorburn W, Montan P. Endophthalmitis after cataract surgery: a nationwide prospective study evaluating incidence in relation to incision type and location. Ophthalmology. 2007;114:866–870. doi:10.1016/j.ophtha.2006.11.025
15. Nagaki Y, Hayasaka S, Kadoi C, et al. Bacterial endophthalmitis after small-incision cataract surgery. Effect of incision placement and intraocular lens type. J Cataract Refract Surg. 2003;29:20–26. doi:10.1016/S0886-3350(02)01483-9
16. Cooper BA, Holekamp NM, Bohigian G, Thompson PA. Case-control study of endophthalmitis after cataract surgery comparing scleral tunnel and clear corneal wounds. Am J Ophthalmol. 2003;136:300–305. doi:10.1016/S0002-9394(03)00202-2
17. Patel SN, Tang PH, Storey PP, et al. The influence of universal face mask use on endophthalmitis risk after intravitreal anti-vascular endothelial growth factor injections. Ophthalmology. 2021;128(11):1620–1626. doi:10.1016/j.ophtha.2021.05.010
18. Yao K, Zhu Y, Zhu Z, et al. The incidence of postoperative endophthalmitis after cataract surgery in China: a multicenter investigation of 2006–2011. Br J Ophthalmol. 2013;97:1312–1317. doi:10.1136/bjophthalmol-2013-303282
19. Wu Y, Yan XM. Retrospective analysis of the clinical characteristics and visual outcomes of postoperative endophthalmitis of cataract between 2001 and 2012. J Peking Univ Health Sci. 2014;46:215–219.
20. Cheng JH, Chang YH, Chen CL, Chen YH, Lu DW, Chen JT. Acute endophthalmitis after cataract surgery at a referral centre in Northern Taiwan: review of the causative organisms, antibiotic susceptibility, and clinical features. Eye. 2010;24:1359–1365. doi:10.1038/eye.2010.39
21. Zhu Y, Chen X, Chen P, Wu J, Hua H, Yao K. The occurrence rate of acute-onset postoperative endophthalmitis after cataract surgery in Chinese small- and medium-scale departments of ophthalmology. Sci Rep. 2017;7:40776. doi:10.1038/srep40776
22. Sun J, Guo Z, Li H, Yang B, Wu X. Acute infectious endophthalmitis after cataract surgery: epidemiological characteristics, risk factors and incidence trends, 2008–2019. Infect Drug Resist. 2021;14:1231–1238. doi:10.2147/IDR.S304675
23. Ciulla TA, Starr MB, Masket S. Bacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based update. Ophthalmology. 2002;109:13–24. doi:10.1016/S0161-6420(01)00899-5
24. Haripriya A. Antibiotic prophylaxis in cataract surgery - an evidence-based approach. Indian J Ophthalmol. 2017;65:1390–1395. doi:10.4103/ijo.IJO_961_17
25. Berkelman RL, Holland BW, Anderson RL. Increased bactericidal activity of dilute preparations of povidone-iodine solutions. J Clin Microbiol. 1982;15:635–639. doi:10.1128/jcm.15.4.635-639.1982
26. Cataract and intraocular lens group of Ophthalmology branch of Chinese Medical Association. consensus of experts on the prevention and treatment of infectious endophthalmitis after cataract extraction in China (2017). Chin J Ophthalmol. 2017;53:810–813.
27. Musumeci R, Troiano P, Martinelli M, et al. Effectiveness of 0.66% povidone-iodine eye drops on ocular surface flora before cataract surgery: a Nationwide Microbiological Study. J clin med. 2021;10(10):2198. doi:10.3390/jcm10102198
28. Sobaci G, Tuncer K, Tas A, Ozyurt M, Bayer A, Kutlu U. The effect of intraoperative antibiotics in irrigating solutions on aqueous humor contamination and endophthalmitis after phacoemulsification surgery. Eur J Ophthalmol. 2003;13:773–778. doi:10.1177/1120672103013009-1007
29. Grasso C. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33:978–988. doi:10.1016/j.jcrs.2007.02.032
30. Rodriguez-Caravaca G, Garcia-Saenz MC, Villar-Del-Campo MC, Andres-Alba Y, Arias-Puente A. Incidence of endophthalmitis and impact of prophylaxis with cefuroxime on cataract surgery. J Cataract Refract Surg. 2013;39:1399–1403. doi:10.1016/j.jcrs.2013.03.031
31. Wang XL, Huang XY, Wang Z, Sun W. The anterior chamber injection of moxifloxacin injection to prevent endophthalmitis after cataract surgery: a meta-analysis. J Ophthalmol. 2020;2020:7242969. doi:10.1155/2020/7242969
32. Naseri A, Melles RB, Shorstein NH. Intracameral antibiotics in the shadow of hemorrhagic occlusive retinal vasculitis. Ophthalmology. 2017;124:580–582. doi:10.1016/j.ophtha.2017.02.019
33. Chang DF, Rhee DJ. Antibiotic prophylaxis of postoperative endophthalmitis following cataract surgery: results of the 2021 ASCRS member survey. J Cataract Refract Surg. 2021;48(1):3–7.
34. Lertsumitkul S, Myers PC, O’Rourke MT, Chandra J. Endophthalmitis in the western Sydney region: a case-control study. Clin Experiment Ophthalmol. 2001;29:400–405. doi:10.1046/j.1442-9071.2001.d01-20.x
35. Friling E, Lundstrom M, Stenevi U, Montan P. Six-year incidence of endophthalmitis after cataract surgery: Swedish national study. J Cataract Refract Surg. 2013;39:15–21. doi:10.1016/j.jcrs.2012.10.037
36. Ding Y, Lin M, Liu H, Zhang W, Wang L, Li Y. Outcomes of post-cataract surgery endophthalmitis referred to a tertiary center from local hospitals in the south of China. Infection. 2011;39:451–460. doi:10.1007/s15010-011-0138-0
37. Pereira EM, de Mattos CS, Dos Santos OC, et al. Staphylococcus hominis subspecies can be identified by SDS-PAGE or MALDI-TOF MS profiles. Sci Rep. 2019;9:11736. doi:10.1038/s41598-019-48248-4
38. Jiang X, Deng A, Yang J, et al. Pathogens in the Meibomian gland and conjunctival sac: microbiome of normal subjects and patients with Meibomian gland dysfunction. Infect Drug Resist. 2018;11:1729–1740. doi:10.2147/IDR.S162135
39. Frickmann H, Hahn A, Skusa R, et al. Comparison of the etiological relevance of Staphylococcus haemolyticus and Staphylococcus hominis. Eur j Clin Microbiol Infect Dis. 2018;37:1539–1545. doi:10.1007/s10096-018-3282-y
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

