Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Incidence of Cardiovascular Complications and Nephropathy in Patients with Type 2 Diabetes in a Primary Care Setting in Riyadh, Saudi Arabia
Authors Alsaidan M , Alkhenizan A , Amber ST, Alsoghayer S , AlFakhri L, Abudaia J
Received 19 January 2021
Accepted for publication 17 March 2021
Published 15 April 2021 Volume 2021:14 Pages 1663—1667
DOI https://doi.org/10.2147/DMSO.S301933
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Muath Alsaidan,1 Abdullah Alkhenizan,2 Shammama Tul Amber,2 Suad Alsoghayer,2 Lama AlFakhri,3 Jamil Abudaia4
1King Saud University College of Medicine, Department of Family and Community Medicine, Riyadh, Saudi Arabia; 2King Faisal Specialist Hospital and Research Center, Family Medicine and Polyclinic, Riyadh, Saudi Arabia; 3King Saud University Medical City, Department of Emergency Medicine, Riyadh, Saudi Arabia; 4AlFaisal University, College of Medicine, Riyadh, Saudi Arabia
Correspondence: Abdullah Alkhenizan
King Faisal Specialist Hospital and Research Center, Family Medicine and Polyclinic, P.O. Box 3354, Riyadh, 11211, Saudi Arabia
Email [email protected]
Background: Diabetes mellitus is prevalent in Saudi Arabia. Our study aims to estimate the rate and time of developing macrovascular and microvascular complications in diabetic patients in a primary care setting.
Methodology: This is a retrospective cohort study. All collected data were retrieved using medical files and the electronic patient records of all diabetics having regular follow-ups in Family Medicine clinics, King Faisal Specialist Hospital & Research Centre in Riyadh, Saudi Arabia, from the beginning of January 2002 to the end of December 2018. The data included the demographics of patients diagnosed with diabetes mellitus, their HbA1c, and the follow-up duration of the development of complications, which included cardiovascular complications and diabetic nephropathy.
Results: We included 365 patients, of whom 47.1% males and 52.9% were females. The mean age of diabetes mellitus diagnosis in our population was 50 years (SD± 11.3). The mean duration of follow-up was 7.14 years (SD± 3.9). The rate of developing cardiovascular complications and diabetic nephropathy was 11.2% and 10.4%, respectively. The mean time to develop cardiovascular complications and diabetic nephropathy was 6 (SD± 3.9) and 5.24 (SD± 3.2) years, respectively. The mean time to develop the first diabetes complication was 5.5 years (SD± 3.6). There was no statistical significance in the mean of HbA1c between patients who developed diabetic complications and those who did not.
Conclusion: Diabetes complications are common in the Saudi community. The duration of the development of cardiovascular complications and diabetic nephropathy was shorter than that indicated in international and national reports. Robust screening programs to diagnose and improve the control of diabetes mellitus should be established in the Kingdom.
Keywords: diabetes, complications, primary care
Introduction
Diabetes is a Globally acknowledged chronic disease. According to data on the global burden of this disease, the worldwide prevalence of diabetes is 8.5%, which represents 422 million people in 2014 among adults over 18 years of age.1 In Saudi Arabia, according to the national Saudi Health Interview Survey, the diabetes prevalence is 11.7% in females and 14.8% in males.2
Diabetes is associated with many complications, such as cardiovascular, renal, neural, and ophthalmological consequences of chronic hyperglycemia, resulting in a twofold increase in medical costs compared with the case of non-diabetic individuals.3 According to the Saudi Burden of Disease 2010 study, the fourth leading cause of years lived with a disability is diabetes.4
Local studies have not addressed the rate of developing diabetes complications and its relation to the control of diabetes in a primary care setting. The aim of our study, therefore, is to ascertain the rate of developing macrovascular and microvascular complications in diabetic patients in relation to its control in a primary care setting in Saudi Arabia.
Methods
The research project was conducted under the policies of the Research Advisory Committee (RAC) at King Faisal Specialist Hospital and Research Centre and the laws of the Kingdom of Saudi Arabia. Ethical approval reference number (RAC # 2181-065). As a start, we obtained a waiver of informed consent from Research Advisory Committee at King Faisal Specialist Hospital and Research Centre from the data warehouse as raw data maintaining patients confidentiality. Our study was a retrospective cohort study. All collected data were retrieved using medical files and the electronic patient records of all diabetics having regular follow-ups in Family Medicine clinics, King Faisal Specialist Hospital & Research Centre in Riyadh, Saudi Arabia, from the beginning of January 2002 to the end of December 2018.
The start of enrollment in our study was the date of diagnosis of type 2 diabetes mellitus. The collected data included the patients’ demographics, duration of diabetes, body mass index, blood pressure, low-density lipoprotein, fasting blood glucose, hemoglobin A1c, creatinine, glomerular filtration rate, and urine albumin–creatinine ratio. The diagnosis of cardiovascular complications was based on clinical, electrophysiological, radiological, and biochemical tests. Cardiovascular complications are defined as coronary artery disease, arrhythmia, stroke, peripheral vascular disease, and CV death. The development of diabetic nephropathy was based on developing microalbuminuria (Urine albumin to creatinine ratio (ACR) = 3–30 mg/mmol or 27–265 mg/g), macroalbuminuria (ACR > 30 mg/mmol or > 265 mg/g), chronic kidney disease (ACR > 300 mg/mmol or > 2652 mg/g), or estimated glomerular filtration rate < 60 mL/min/1.73 m2) for three or more months.5 Types of treatment the patients received were not available. Also, data on ophthalmological complications and diabetic neuropathy were not available. Patients having prior diagnoses with cardiovascular disease, nephropathy, hypertension, type 1 diabetes, gestational diabetes, and dyslipidemia were excluded from our study.
Variables used in our regression analysis to assess the relationship between being diabetic and developing cardiovascular complications and nephropathy are (age, gender, body mass index, hypertension, dyslipidemia, hypothyroidism, and middle hemoglobin a1c from time of diagnosis as cutoff points less than 7, 7.5, 8, and 9).
Statistical analysis was managed using the software package SPSS, version 22, by IBM. The descriptive data for the continuous variables were reported as mean, and the categorical variables were described as frequencies and percentages. Continuous variables were analyzed using the Student’s t-test, whereas categorical variables were compared using the Chi-square test. We used logistic regression to assess the effect of diabetes mellitus on the possibility of developing complications. Statistical significance was set at p < 0.05.
Results
Of the 365 subjects included in our study, 47.1% were males, and 52.9% were females. Table 1 displays the general traits of our studied population. The patients’ mean age of diagnosis of diabetes mellitus was 50 years (SD±11.3, p-value = 0.03), and the mean duration of continuation of care was 7.14 years (SD±3.9).
 |
Table 1 General Characteristics (Original) |
Table 2 shows the frequency of complications and comorbidities among our studied population. Twenty-seven subjects had hypertension, and 16 had dyslipidemia before their diagnosis of diabetes mellitus. A previous diagnosis of cardiovascular disease was found in one subject, and nephropathy was found in eight subjects. We excluded these patients from our analysis because of the pre-existence of these complications. Two cases of mortality were documented.
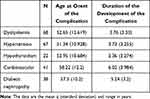 |
Table 2 Frequency of Complications and Comorbidities Among Patients with Type 2 Diabetes Mellitus (n=365) (Original) |
The earliest diabetes mellitus complication developed after a mean of 5.5 years (SD±3.6) from the time of diagnosis. The rate of developing complications is shown in Figure 1. In particular, the rate of developing cardiovascular complications was 11.2% with a duration of 6 years (SD±3.9) from the time of diagnosis of diabetes. In the group of subjects who developed cardiovascular complications, males (53.7%) were affected more than females were; however, this difference was not statistically significant (p-value = 0.374). The rate of developing diabetic nephropathy was 10.4%, with a mean duration of 5.24 years (SD±3.2) to develop it. Similarly, in the group of subjects who developed diabetic nephropathy, males (60.7%) were affected more than females were, with no statistically significant difference (p-value = 0.080).
 |
Figure 1 Rate of developing cardiovascular and diabetic nephropathy among patients with type 2 diabetes mellitus. |
With hemoglobin A1c used as the marker, controlled diabetes mellitus (HbA1c < 7) was evident in 49.7% of our studied population; hemoglobin A1c was less than 7.5 in 62.4% and less than 8 in 75.3% of the population. No statistically significant association was found between hemoglobin A1c at any level and the development of any diabetic complications.
Logistic regression analysis of all diabetes mellitus complications showed that the age of onset of diabetes was statistically significant (p-value = 0.003, odds ratio: 1.034); we found a statistically significant association between all diabetes mellitus complications and hypertension diagnosis with an odds ratio of 2.2 (p-value = 0.007).
Discussion
This study elaborates the estimated rate and time of developing macrovascular/microvascular (diabetic nephropathy) complications in patients with diabetes in a primary care setting in Saudi Arabia. The mean age of diabetes onset in our study was 50, which was similar to that in a local study, a regional report from Palestine, and the United Kingdom Prospective Diabetes Study (UKPDS).6–8
The earliest diabetic complication was evident as early as 5.5 years from the time of diagnosis, which is longer than what was reported in a hospital-based study.6 The rate of developing cardiovascular complications and diabetic nephropathy was similar to that in the UKPDS study and the Saudi National Diabetes Registry.8–10 However, in a hospital-based setting, Al-Wakeel found that the Saudi population had a high prevalence of diabetic complications. These were more aggressive forms similar to other international secondary and tertiary care settings.11–13 The time to develop diabetic nephropathy was almost the same as that in the UKPDS report but was shorter than a local hospital-based study.8,11 This may be explained by differences between the primary care and hospital settings in terms of early screening, treatment, and follow-up.6,9
The duration of the development of cardiovascular complications was shorter in our studied population than in local hospital-based study and European reports.6,9,11 Our study showed that males had a high prevalence of cardiovascular and diabetic nephropathy, similar to what was reported in the literature.6,14 This may be attributed to men’s sedentary lifestyle, more elevated blood sugar levels, higher blood pressure, dyslipidemia, and a lack of understanding about the significance of controlling these illnesses.
The UKPDS showed no glycemic threshold for a substantial change in risks for any clinical outcomes investigated.15 A recent meta-analysis showed that randomized controlled trials could not allow us to have a definite conclusion on the suitability of intensively targeting HbA1c to decrease the rate of cardiovascular complications. It advocates a level less than 7%, especially in patients not known to have past cardiovascular events, long life expectancy, and short duration of diagnosis.16 Similarly, in patients developing diabetic nephropathy, receiving tight control compared to a more relaxed one will only affect developing microalbuminuria and delay progression, but not major renal events.17–19 In our study, no statistical significance was observed in the mean of HbA1c between patients who developed diabetic complications and those who did not despite having more controlled diabetes than others reported.13,15,20–22
Our research was a retrospective cohort study. The benefit of the electronic health record system enabled us to decrease the risk of potential confounding factors. Although our population size was small, it represents an appropriate sample from the local population who seeks medical advice in a primary care setting. These subjects had access to regular follow-ups with well-trained physicians; therefore, diabetic complications were identified in a timely manner in these individuals. A limitation to our study is that information about types of therapy was not available with the growing evidence that different glucose-lowering drugs are associated with a diverse incidence of complications independently of glycaemic control.23–26 However, with the widespread prevalence of this disease in Saudi Arabia and the changes in lifestyle it requires, more extensive studies on it are needed in the community or primary care setting for a better understanding of the progression of this disease, how it can be controlled, and its complications in our unique population. This can guide us toward introducing more structured screening and follow-up programs in our community. Our study showed that males had a higher prevalence of both cardiovascular complications and diabetic nephropathy. This interesting finding needs further investigation.
In conclusion, diabetes complications are common in our community. Duration of cardiovascular complications and diabetic nephropathy was shorter than that indicated in international and national reports. There was no statistical significance in the mean of HbA1c between patients who developed diabetic complications and those who did not. The introduction of structured programs for health education and screening for chronic health conditions, such as diabetes mellitus, is warranted. Robust health programs are needed in the primary care setting to diagnose and improve diabetes mellitus in Saudi Arabia.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Mathers CD, Loncar D, Samet J. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;28(11):e442. doi:10.1371/journal.pmed.0030442
2. El Bcheraoui C, Basulaiman M, Tuffaha M, et al. Status of the diabetes epidemic in the Kingdom of Saudi Arabia, 2013. Int J Public Health. 2014;59(6):1011–1021. doi:10.1007/s00038-014-0612-4
3. Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Division of Diabetes Translation, US Department of Health and Human Services; Vol. 20, 2017 July 17.
4. Memish ZA, Jaber S, Mokdad AH, AlMazroa MA, Murray CJ, Al Rabeeah AA. Peer-reviewed: burden of disease, injuries, and risk factors in the Kingdom of Saudi Arabia, 1990–2010. Prev Chronic Dis. 2014;11(1):140176. doi:10.5888/pcd11.140176
5. Levin AS, Bilous RW, Coresh J. Chapter 1: definition and classification of CKD. Kidney Int Suppl. 2013;3(1):19–62.
6. Alwakeel JS, Sulimani R, Al-Asaad H, et al. Diabetes complications in 1952 type 2 diabetes mellitus patients managed in a single institution in Saudi Arabia. Ann Saudi Med. 2008;28(4):260–266. doi:10.5144/0256-4947.2008.260
7. Ghandour R, Mikki N, Rmeileh NM, et al. Complications of type 2 diabetes mellitus in Ramallah and al-Bireh: the Palestinian diabetes complications and control study (PDCCS). PCDE. 2018;12:547–557.
8. Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR; UKPDS Group. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63(1):225–232. doi:10.1046/j.1523-1755.2003.00712.x
9. Turner RC, Millns H, Neil HA, et al. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: united Kingdom Prospective Diabetes Study (UKPDS: 23). BMJ. 1998;316(7134):823–828. doi:10.1136/bmj.316.7134.823
10. Al-Rubeaan K, Youssef AM, Subhani SN, et al. Diabetic nephropathy and its risk factors in a society with a type 2 diabetes epidemic: a Saudi National Diabetes Registry-based study. PLoS One. 2014;9(2):e88956. doi:10.1371/journal.pone.0088956
11. Al-Wakeel JS, Hammad D, Al Suwaida A, Mitwalli AH, Memon NA, Sulimani F. Microvascular and macrovascular complications in diabetic nephropathy patients referred to nephrology clinic. Saudi J Kidney Dis Transpl. 2009;20:77.
12. Bukhsh A, Khan TM, Nawaz MS, Ahmed HS, Chan KG, Goh BH. Association of diabetes knowledge with glycemic control and self-care practices among Pakistani people with type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2019;12:1409. doi:10.2147/DMSO.S209711
13. Afroz A, Zhang W, Loh AJ, Lee DX, Billah B. Macro-and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab Syndr. 2019;13(5):2939–2946. doi:10.1016/j.dsx.2019.07.046
14. Arambewela MH, Somasundaram NP, Jayasekara HB, et al. Prevalence of chronic complications, their risk factors, and the cardiovascular risk factors among patients with type 2 diabetes attending the diabetic clinic at a Tertiary Care Hospital in Sri Lanka. J Diabetes Res. 2018;2018:2018. doi:10.1155/2018/4504287
15. Stratton IM, Adler AI, Neil HA, et al. Association of glycemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi:10.1136/bmj.321.7258.405
16. Prattichizzo F, de Candia P, De Nigris V, Nicolucci A, Ceriello A. Legacy effect of intensive glucose control on major adverse cardiovascular outcome: systematic review and meta-analyses of trials according to different scenarios. Metabolism. 2020;110:154308. doi:10.1016/j.metabol.2020.154308
17. Valensi P, Prévost G, Schnell O, Standl E, Ceriello A. Targets for blood glucose: what have the trials told us. Eur J Prev Cardiol. 2019;26(2_suppl):64–72. doi:10.1177/2047487319885456
18. Ruospo M, Saglimbene VM, Palmer SC, et al. Glucose targets for preventing diabetic kidney disease and its progression. Cochrane Database Syst Rev. 2017;(6).
19. Zoungas S, Arima H, Gerstein HC, et al. Effects of intensive glucose control on microvascular outcomes in patients with type 2 diabetes: a meta-analysis of individual participant data from randomised controlled trials. Lancet Diabetes Endocrinol. 2017;5(6):431–437. doi:10.1016/S2213-8587(17)30104-3
20. Alsulaiman TA, Al-Ajmi HA, Al-Qahtani SM, et al. Control of type 2 diabetes in King Abdulaziz Housing City (Iskan) population, Saudi Arabia. J Family Community Med. 2016;23(1):1. doi:10.4103/2230-8229.172221
21. Abouammoh NA, Alshamrani MA. Knowledge about diabetes and glycemic control among diabetic patients in Saudi Arabia. J Diabetes Res. 2020;2020:1–6. doi:10.1155/2020/1239735
22. Alramadan MJ, Magliano DJ, Almigbal TH, et al. Glycaemic control for people with type 2 diabetes in Saudi Arabia–an urgent need for a review of management plan. BMC Endocr Disord. 2018;18(1):62. doi:10.1186/s12902-018-0292-9
23. Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA. SUSTAIN-6 Investigators. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;2016:375.
24. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–322. doi:10.1056/NEJMoa1603827
25. Mann JF, Ørsted DD, Brown-Frandsen K, et al. Liraglutide and renal outcomes in type 2 diabetes. N Engl J Med. 2017;377(9):839–848. doi:10.1056/NEJMoa1616011
26. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–2128. doi:10.1056/NEJMoa1504720
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
