Back to Journals » Nature and Science of Sleep » Volume 15
Impact of Obstructive Sleep Apnea on Disease Severity and Adverse Outcomes in Patients with Acute Pulmonary Embolism
Authors Huang Z , Duan A, Zhao Z, Zhao Q, Zhang Y, Li X, Zhang S, Gao L, An C, Luo Q, Liu Z
Received 28 May 2023
Accepted for publication 10 September 2023
Published 18 September 2023 Volume 2023:15 Pages 705—717
DOI https://doi.org/10.2147/NSS.S423221
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Valentina Alfonsi
Zhihua Huang,* Anqi Duan,* Zhihui Zhao, Qing Zhao, Yi Zhang, Xin Li, Sicheng Zhang, Luyang Gao, Chenhong An, Qin Luo, Zhihong Liu
Center for Respiratory and Pulmonary Vascular Diseases, Department of Cardiology, Fuwai Hospital, National Clinical Research Center for Cardiovascular Diseases, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qin Luo; Zhihong Liu, Center for Respiratory and Pulmonary Vascular Diseases, Department of Cardiology, Fuwai Hospital, National Clinical Research Center for Cardiovascular Diseases, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, No. 167 Beilishi Road, Xicheng District, Beijing, 100037, People’s Republic of China, Tel +86 010 8832859, Email [email protected]; [email protected]
Purpose: Acute pulmonary embolism (PE) poses a life-threatening risk with high mortality rates. While the coexistence of PE and obstructive sleep apnea (OSA) is gaining recognition, its influence on PE severity and prognosis remains uncertain. This study aims to investigate the associations between OSA and disease severity, as well as outcomes, in patients with acute PE.
Patients and Methods: We conducted a retrospective cohort study on patients diagnosed with acute PE who had undergone previous cardiorespiratory polygraphy. OSA severity was assessed using the apnea-hypopnea index (AHI) derived from cardiorespiratory polygraphy. The severity of acute PE was evaluated using the simplified Pulmonary Embolism Severity Index (sPESI) score. Logistic regression analysis was performed to investigate the associations between AHI and the risk of belonging to the sPESI≥ 1 group. Cox regression analysis was used to examine the relationship between AHI and long-term adverse events, defined as a composite of all-cause mortality and non-fatal cardiovascular events.
Results: Among 145 acute PE patients (mean age 62.2 years, 49.7% male), 94 (64.8%) had OSA. Patients with OSA had a significantly higher proportion of sPESI≥ 1 (89.4% vs 68.6%, p=0.002) than non-OSA patients. Each unit increase in AHI was associated with a 15% increased risk of severe PE (sPESI≥ 1) (odds ratio: 1.15, 95% CI 1.05– 1.26, p=0.002) after adjusting for confounders. During a median follow-up of 15.2 months, 27 (18.6%) patients experienced adverse events. Increased AHI independently predicted a higher risk of adverse events (hazard ratio: 1.03, 95% CI: 1.00– 1.05, p=0.026), even after adjusting for potential confounders. AHI ≥ 8 events/h was associated with a significantly higher adjusted hazard ratio of 2.56 (95% CI: 1.15– 5.72, p=0.022) for adverse events compared to AHI < 8 events.
Conclusion: OSA is common in acute PE patients and is linked to increased disease severity and adverse outcomes. Implementing routine OSA screening and management may aid risk stratification and improve outcomes in acute PE patients.
Keywords: sleep apnea, pulmonary embolism, outcomes, prognosis, cardiovascular
Introduction
Acute pulmonary embolism (PE) is a life-threatening condition characterized by the obstruction of one or more pulmonary arteries due to blood clots. It represents the most severe form of venous thromboembolism and ranks as the third leading cause of cardiovascular mortality, following coronary heart disease and stroke.1 Despite the widespread adoption of risk stratification and anticoagulant therapy, the mortality rate among high-risk acute PE patients remains alarmingly high, with reported 30-day mortality rates of up to 22%.2 Therefore, it is crucial to actively screen for risk factors that impact the prognosis of PE patients and strengthen management approaches to improve their outcomes.
Obstructive sleep apnea (OSA) is a prevalent sleep-breathing disorder that affects millions of individuals worldwide. It is estimated that approximately 20–30% of the global population experiences OSA, with over 1 billion patients affected.3 OSA is characterized by recurrent episodes of complete or partial upper airway obstruction during sleep, resulting in hypoxemia, hypercapnia, sympathetic activation, and fluctuations in intrathoracic pressure.4 OSA has been associated with various adverse health outcomes, including hypertension, coronary artery disease, stroke, and type 2 diabetes.5 Recent epidemiological data indicates a high prevalence of OSA in patients with PE, ranging from 54.5% to 74.4%,6 and reaching as high as 81.0% in moderate-to-high risk PE patients.7 The increased co-occurrence of PE and OSA can be attributed to several factors, such as obesity, prolonged periods of sitting, aging, and hypercoagulability.8–10
The significance of OSA in the prognosis of patients with acute PE has increasingly gained attention in recent years. Although several studies have examined the association between OSA and adverse outcomes in PE patients, the results have been conflicting. A large-scale international study, involving an analysis of over 750,000 cases of acute PE patients, identified an annual increase in the in-hospital mortality rate among patients with concurrent OSA.11 Another study indicated that when the Apnea-Hypopnea Index (AHI) exceeded 10, the risk of PE recurrence within a five-year period increased more than fourfold.12,13 However, the findings from Ghiasi et al study14 demonstrated that the 30-day mortality rate of PE patients with concomitant OSA did not exhibit an increase.15 Furthermore, a recent study revealed that untreated OSA was not a significant predictor of adverse cardiovascular events in patients with acute PE.16 Collectively, these conflicting findings necessitate a comprehensive analysis of sleep parameters and an exploration of their influence on disease severity and adverse outcomes in PE patients.
Hence, the objective of this study is to examine the correlations between different parameters of OSA and their influence on the disease severity and the incidence of adverse cardiovascular events in patients diagnosed with acute PE.
Materials and Methods
Study Population
This retrospective cohort study included patients who were diagnosed with acute PE at a large hospital between November 2020 and January 2022. All patients with acute PE were identified using the ICD-10-CM codes as per the 2019 guidelines.17 The inclusion criteria were as follows: patients aged 18 years or older, a confirmed diagnosis of acute PE, and availability of nocturnal cardiorespiratory polygraphy results within 3 months before the diagnosis of acute PE. Patients with missing data or incomplete medical records or receiving ongoing therapy for a previous diagnosed OSA were excluded from the study. Out of the 153 patients diagnosed with PE who had undergone previous cardiorespiratory polygraphy, three patients were already receiving continuous positive airway pressure therapy for OSA prior to hospitalization. Additionally, five patients had incomplete data for analysis, resulting in a final inclusion of 145 patients for the study. The study received ethical approval from the ethical committee of Fuwai Hospital, and informed consent was obtained from all studied patients.
Clinical Characteristics
A diverse array of clinical characteristics pertaining to the patients in this retrospective cohort study was obtained from electronic medical records. Demographic information including age, gender, and body mass index (BMI), and vital signs such as blood pressure and heart rate at admission were collected and recorded. To evaluate daytime sleepiness, the Epworth Sleepiness Scale was utilized, providing a quantitative measure based on a standardized scoring system. Comorbid conditions, such as atrial fibrillation, hypertension, diabetes mellitus, and hyperlipidemia, were identified and documented based on medical health records. Laboratory tests were conducted to analyze specific biomarkers, including D-dimers, troponin, cytokine kinase-MB, and N-terminal pro-B type natriuretic peptide. Echocardiographic data were collected to evaluate the left atrium diameter, left ventricular end-diastolic diameter, right ventricle, left ventricular ejection fraction, and pulmonary arterial systolic pressure.
Nocturnal Cardiorespiratory Polygraphy
Patients who had undergone overnight cardiorespiratory polygraphy prior to the diagnosis of PE due to suspected sleep-disordered breathing within 3 months were included in this retrospective cohort. The overnight cardiorespiratory polygraphy was conducted using the Embletta system (Medcare Flaga, Reykjavik, Iceland), a level III device used to assess the presence and severity of OSA. Key parameters collected included oxygen saturation (SpO2) measured by fingertip oximetry, nasal airflow, and thoraco-abdominal movements. Nocturnal respiratory events were evaluated and scored following guidelines by the American Academy of Sleep Medicine.18 A minimum recording duration of 4 hours was considered sufficient. Apnea events were recorded as ≥90% reduction in respiratory airflow for ≥10 seconds. Hypopnea events were defined as ≥30% drop in peak signal excursions using nasal airflow pressure, lasting ≥10 seconds, with a ≥3% oxygen desaturation. The AHI was quantified as the sum of apnea and hypopnea events per recorded hour. Obstructive events were determined when a respiratory event coincided with abdominal or thoracic movements. OSA diagnosis required AHI≥5 events/h, with obstructive events ≥50% of total. Nocturnal hypoxemia severity was assessed using the percentage of cumulative time with SpO2 below 90% in total recorded time (T90). The oxygen desaturation index (ODI) indicated frequency of ≥3% desaturation from pre-event baseline per recorded hour. Other hypoxemia parameters included mean and minimum SpO2 levels, as well as the duration of the longest or the mean hypopnea and apnea events. The longest apnea duration was determined as the maximum period of time during sleep when breathing ceased. An experienced technician, blinded to patients’ clinical characteristics, evaluated and scored all respiratory events.
Risk Stratification of Pulmonary Embolism
The severity of acute PE was assessed using the simplified Pulmonary Embolism Severity Index (sPESI) to assess the 30-day all-cause mortality risk.19 The sPESI score was calculated based on the following criteria: age ≥ 80 years, history of cancer, history of chronic heart failure, history of chronic cardiopulmonary disease, heart rate ≥ 110 beats per minute, systolic blood pressure < 100 mmHg, and arterial oxygen saturation < 90%. Patients with a sPESI score of 1 or higher were considered to have a high risk of 30-day all-cause mortality risk. Clinically, risk stratification in acute PE involves three steps: identifying high-risk patients requiring immediate reperfusion treatment, identifying low-risk patients suitable for outpatient management, and identifying intermediate-risk patients requiring hospitalization and close monitoring. High risk patients are characterized by hemodynamic instability, which includes the presence of cardiac arrest requiring resuscitation, obstructive shock, or persistent hypotension (systolic blood pressure <90 mmHg or a decrease of at least 40 mmHg from baseline for at least 15 minutes), not caused by other pathologies. Among hemodynamically stable patients, PE is categorized as low risk when there is no evidence of right ventricular dysfunction observed through computed tomography, echocardiography, or myocardial strain (ie, cardiac troponin I >0.05 ng/mL or brain natriuretic peptides >100 pg/mL). If right ventricular dysfunction is present, PE is considered intermediate risk. If there is further evidence of myocardial strain, patients are classified as intermediate-high risk. Patients without myocardial strain are classified as intermediate-low risk.17 The risk stratification based on these criteria was also recorded for the individuals in this study.
Outcomes Assessment
The primary outcome of the study was a composite of endpoints including all-cause mortality and non-fatal cardiovascular events. Non-fatal cardiovascular events consisted of recurrent venous thromboembolism, chronic thromboembolic pulmonary hypertension, re-hospitalization due to heart failure, stroke, or acute coronary syndrome requiring revascularization. The follow-up period began at the time of acute PE diagnosis and concluded either when adverse events occurred or when the study period ended, whichever happened first. Outcome measures were obtained through a thorough review of medical records and interview with patients or their relatives via mail or phone.
Statistical Analysis
Continuous variables were presented as means ± standard deviations or medians with interquartile ranges, depending on their distribution. Categorical variables were reported as frequencies and percentages. To compare categorical data between groups, we employed chi-square or Fisher’s exact tests, while the Shapiro–Wilk test assessed the normal distribution of continuous data. Unpaired t-tests were used for comparing parametric continuous data between two unpaired groups, and the Mann–Whitney U-test for non-parametric data comparisons. Logistic regression models were utilized to assess the associations between various nocturnal sleep parameters and severe acute PE (sPESI≥1), adjusting for potential confounders in the univariable logistic regression analysis. Proportional Cox hazards models were employed to estimate the risk of adverse events based on cardiorespiratory parameters. The selection of adjusted covariates for the models was based on their univariable statistical significance or clinical relevance. Restricted cubic splines, adjusted for potential confounders, were employed to examine the linear associations between AHI and explore the optimal cut-off value for predicting the risk. Kaplan-Meier curves were constructed between different AHI groups using the Log rank test to compare adverse events rates. Subgroup analyses were performed to investigate potential effect modification by variables such as age, sex, BMI, and other relevant factors on the association between OSA and adverse events. All statistical analyses were performed using R software (version 4.1.2, R Foundation for Statistical Computing, Vienna, Austria), and statistical significance was defined as a two-tailed P value < 0.05.
Results
Clinical Characteristics
Among 145 diagnosed acute PE patients (mean age: 62.2 ± 13.8 years, 49.7% male), 94 (64.8%) had OSA. The OSA group had a higher heart rate at acute PE diagnosis compared to the non-OSA group (107.1 ± 13.5 bpm vs 100.0 ± 10.5 bpm, p = 0.001) (Table 1). Significant differences in risk stratification based on hemodynamic stability, right ventricular dysfunction, and cardiac injury biomarkers were observed between OSA and non-OSA patients (p=0.029). A larger proportion of the OSA group (89.4%) had an sPESI score ≥1 compared to the non-OSA group (68.6%, p=0.002). Troponin levels were slightly higher in acute PE patients with comorbid OSA (p=0.046). No significant acute changes in echocardiographic features were noted between OSA and non-OSA patients.
 |
Table 1 Comparison of Clinical Characteristics Between Patients with OSA and Non-OSA in Acute PE |
Sleep Parameters and Risk of Severe Acute PE
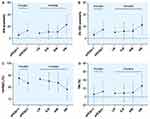
The majority of patients did not experience excessive daytime sleepiness, as reflected by an Epworth Sleepiness Scale score of less than 10. Significant differences in sleep parameters were observed between OSA and non-OSA patients, with the OSA group experiencing more severe respiratory events and profound hypoxemia (p<0.05). For example, the OSA group demonstrated a lower minimum oxygen saturation (minSpO2) of 81.8 ± 7.1% compared to the non-OSA group (88.5 ± 5.5%, p<0.001) (Table 2). No significant differences in nocturnal heart rate parameters were observed. Detailed data comparisons among patients with different sPESI risk groups are provided in Tables S1 and S2. Figure 1 displays the distribution of important cardiorespiratory parameters across various risk groups of PE. The findings reveal that the AHI, 3% ODI, and T90 levels, escalate as the clinical risk-stratification of PE increases (p<0.05). In contrast, the hypoxemia parameters, specifically minSpO2, exhibit a decline as the severity of PE risk groups worsens.
 |
Table 2 Comparison of Overnight Cardiorespiratory Parameters Between Patients with OSA and Non-OSA in Acute PE |
To evaluate the influence of OSA variables on the risk of sPESI≥1, multiple logistic regression models were employed, incorporating factors found to be statistically correlated with the sPESI≥1 group (refer to Table S3) as well as essential demographic information such as age, gender, and BMI. The model was therefore adjusted for confounding variables including age, gender, body mass index, hyperlipidemia, diabetes mellitus, hypertension, and use of oral anticoagulants. Even after adjusting for these potential confounders, AHI (odds ratio [OR]: 1.15, 95% confidence interval [CI]: 1.05–1.26, p=0.002), ODI (OR: 1.13, 95% CI: 1.04–1.22, p=0.004), minSpO2 (OR: 0.86, 95% CI: 0.77–0.95, p=0.004), meanSpO2 (OR: 0.84, 95% CI: 0.71–0.99, p=0.035), and T90 (OR: 1.03, 95% CI: 1.00–1.06, p=0.044) displayed significant associations with the risk of severe acute PE (sPESI ≥1) (Table 3). There were no statistically significant associations found between the longest duration of apnea or hypopnea episodes and the risk of sPESI≥1 (P>0.05). Likewise, no significant associations were observed between the mean duration of these respiratory events and an increased risk of sPESI≥1. Moreover, elevated levels of nocturnal heart rate parameters were also found to be associated with an increased risk of sPESI≥1 (OR range: 1.08–1.20, all p<0.05).
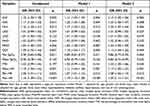 |
Table 3 Logistic Regression Analysis of Nocturnal Cardiorespiratory Parameters Predicting sPESI≥1 |
Sleep Parameters and Risk of Adverse Events in PE
During a median follow-up period of 15.2 months (interquartile range: 4 to 19 months) after acute PE diagnosis, 27 (18.6%) patients experienced adverse events. Cox regression analysis, adjusted for sPESI, and pulmonary artery systolic pressure (as identified risk factors in Table S4), demonstrated that the severity of OSA, as measured by AHI, independently predicted adverse events in acute PE patients (hazard ratio [HR]=1.03, 95% CI: 1.00–1.05, p=0.026) (Table 4). Furthermore, the duration of the longest apnea was also positively associated with the risk of adverse events (HR=1.02, 95% CI: 1.00–1.04, p=0.001).
 |
Table 4 Cox Regression Analysis for Predicting Adverse Events Based on Nocturnal Cardiorespiratory Parameters |
Restrictive cubic splines analysis indicated that an AHI cutoff of 8 events/h better represented the non-linear trend of adverse event risk (Figure 2A). Patients with an AHI ≥8 events/h had a higher incidence of adverse events compared to those with an AHI <8 events/h (24.7% [n=18/73] vs 12.5% [n=9/72], log-ranked p=0.0174) (Figure 2B). In comparison to individuals with an AHI <8 events/h, those with ≥8 events/h exhibited a higher hazard ratio (HR) of 2.56 (95% CI: 1.15–5.72, p=0.022) for adverse events, after adjusting for sPESI and pulmonary artery systolic pressure. To assess the robustness of the results, subgroup analyses were conducted to explore the relationships between AHI and adverse events. The subgroups were categorized based on age, gender, BMI, smoking status, and cardiovascular comorbidities. Interestingly, the associations between AHI and adverse events appeared consistent among examined subgroups, as indicated by a non-significant P value for interaction (>0.05) (Figure 3).
Discussion
The present cohort study has identified that OSA was common among patients who have recently been diagnosed with acute PE, indicating a significant burden of this disease. Furthermore, patients with more severe OSA, as measured by an increase in AHI per unit, demonstrated a 15% higher risk of being categorized in the sPESI≥1 group, as well as a nearly 2% higher risk of experiencing adverse cardiovascular events. Importantly, these associations remained significant even after adjusting for potential confounders, and the findings appeared consistent across various examined sub-groups. In light of these findings, our study underscores the clinical significance of early screening and comprehensive management of OSA in the routine care of patients presenting with acute PE.
The current study revealed a notable proportion of OSA in patients with acute PE. Using an AHI cutoff of ≥5 events/h, the detection rate was approximately 65% (94 out of 145 patients), while utilizing an AHI cutoff of ≥15 events/h yielded a rate of 31% (45 out of 145 patients). These estimates align with a previous study reporting a similarly high prevalence of OSA (63%) in PE patients,20 whereas most studies have reported lower prevalence rates ranging from 5% to 15%.21,22 Discrepancies in prevalence can be attributed to variations in study design, timing of nocturnal sleep assessments, diagnostic criteria, utilized devices, and the clinical characteristics of the study population. The high occurrence rate of OSA observed in our study may be attributed to the retrospective design of our cohort, which relied on the availability of sleep study data prior to PE diagnosis. It is also plausible that transient abnormalities detected during acute cardiovascular events may contribute to a higher rate of false-positive OSA diagnoses.23 However, in our study, sleep study results were predominantly obtained prior to the diagnosis of PE, despite the retrospective design. In this regard, our findings suggest the biologically plausible notion that OSA may precede PE, indicating a significant occurrence of PE in individuals with OSA.
The association between OSA and the severity of PE in patients has been a topic of debate. Toledo-Pons et al24 reported that patients with moderate-severe OSA (AHI≥15) and PE exhibited greater pulmonary artery obstruction and PE severity, as assessed by the PESI, similar to our findings. However, their study conducted sleep studies 6 to 12 months after the index PE event, potentially introducing confounding factors and diluting the true associations between OSA and PE severity. A previous meta-analysis involving 9 studies and 1570 PE patients showed that individuals with OSA presented with more severe PE compared to those without OSA.25 Likewise, a recent meta-analysis26 consisting of 12 studies (8 being cohort studies) demonstrated significantly higher sPESI scores and pulmonary artery obstructive index in patients with OSA compared to controls. It is worth noting that they also did not observe any significant differences in the right ventricle-to-left ventricle short-axis diameter between the two groups. Our findings provide additional support for these observations. There may not be a direct impact of OSA on the echocardiographic parameters which could potentially be attributed to the chronic-phase effects of OSA leading to right ventricular dysfunction.
Conversely, several studies have reported contrasting findings regarding the role of OSA in exacerbating the severity of PE or its impact on post-diagnosis outcomes. For instance, Ghiasi et al14 found no association between OSA and 30-day mortality in PE patients. However, this study utilized STOP-BANG questionnaires to screen for high-risk OSA, potentially leading to an inaccurate estimate of the true prevalence and diagnosis of OSA. Similarly, a recent prospective cohort study by Barbero et al16 failed to establish a relationship between untreated OSA and the incidence of adverse cardiovascular events in patients with symptomatic acute PE. It has been proposed that the preconditioning effect of chronic intermittent hypoxia may confer a protective role in the disease course of PE, which could explain these negative findings.27,28 However, it is worth noting that Barbero et al study16 specifically excluded patients with hemodynamic instability, and only hemodynamically stable individuals with acute PE were included, potentially limiting the ability to demonstrate the true impact of OSA on severity in non-high-risk patients and affecting the overall findings.
Our study adds to the existing literature by conducting a comprehensive evaluation of OSA parameters, analyzing cardiac injury biomarkers and echocardiographic data, and exploring potential cutoff values for predicting adverse events. Beyond traditional metrics such as AHI or ODI, we also found a significant association between obstructive apnea or hypopnea index, minimal or mean SpO2 and a higher risk of sPESI≥1 group. Our findings suggested that the obstructive apnea or hypopnea index may have a stronger association with sPESI>1, as indicated by larger odds ratios compared to AHI. However, it is important to note that AHI, which includes both apnea and hypopnea episodes, remains a valuable measure for capturing the key physiological sequelae of OSA. Additionally, patients with OSA at PE diagnosis demonstrated elevated heart rates, potentially explaining the higher proportion of patients classified as sPESI≥1. Furthermore, we observed elevated levels of cardiac troponins in OSA patients with PE, indicating concurrent cardiac injury within the context of acute PE and hypoxemia. These findings were in accordance with prior research highlighting the association between OSA and severe myocardial injuries. Regarding long-term outcomes, frequency indices such as AHI and ODI showed a correlation with adverse cardiovascular events. By analyzing the adverse event trend and utilizing AHI as a key predictor, we propose a cutoff value of 8 as the optimal threshold for predicting adverse events. Notably, our study conducted sensitivity analyses across various subgroups (sex, age, BMI, and comorbidities), further reinforcing the consistent association between AHI and long-term adverse events. Of note, our study diverges from previous research focusing on the impact of OSA on short-term mortality.14,16 Instead, we aimed to explore long-term adverse outcomes due to potential limitations in the accuracy of in-hospital mortality data from registry-based studies, which are prone to record-keeping and data entry errors.
The pathophysiological link between the severity of OSA and the severity of PE, as well as adverse cardiovascular outcomes, is complex and interconnected. It is hypothesized that reduced oxygen saturation in patients with OSA may exacerbate myocardial injury, thereby contributing to high-risk PE.7,29 Moreover, apnea events and desaturation episodes in OSA patients can promote a prothrombotic state, leading to elevated levels of blood coagulability markers. Consequently, this may result in a higher pulmonary thrombus burden and increased strain on the right ventricle, ultimately contributing to the development of high-risk or severe PE.30 Simultaneously, desaturation episodes in OSA patients induce changes in intrathoracic pressure and pulmonary hypertension, which can directly impact right heart function. Additionally, the severity of OSA and the associated hypoxemia are known to exacerbate right ventricular dysfunction.31,32 Interestingly, there was no apparent correlation between the longest duration of apnea and a higher risk of sPESI≥1. However, our findings suggest that it may have implications for long-term adverse events in patients with PE. It is presumed that prolonged apnea episodes may potentially contribute to increased pulmonary vascular resistance, right ventricular strain, and impaired gas exchange in the later stages following the acute onset of PE. Over the long term, these factors contribute to increased right ventricular workload, the onset of heart failure, and potentially even mortality. The complex relationship between OSA severity, hypoxemia, right ventricular dysfunction, and adverse cardiovascular outcomes highlights the need for a comprehensive understanding of the underlying mechanisms. Further research is warranted to elucidate these intricate interactions and their implications for patient management and outcomes.
The present study has implications for clinical practice, emphasizing the potential impact of addressing OSA in patients with acute PE. The treatability of OSA underscores the importance of considering OSA screening and treatment as an integral part of routine care for acute PE patients. Moving forward, it is crucial to conduct further research that specifically investigates the effectiveness of OSA management in enhancing outcomes among patients with acute PE. Such studies would provide valuable insights into the benefits of OSA treatment and guide evidence-based approaches to optimize patient care in this context. By focusing on the evaluation of OSA management strategies and their impact on outcomes, we may advance our understanding of the potential benefits and refine clinical guidelines for the management of acute PE patients.
The findings of our study should be interpreted with caution due to several limitations. Firstly, the relatively small sample size might have limited the statistical power to comprehensively assess the composite outcomes and adequately adjust for confounding factors, indicating the need for larger studies in the future. Secondly, the retrospective design of this cohort, based on the availability of cardiorespiratory polygraphy, introduces a selection bias and may overestimate the occurrence rate of OSA in APE. Further large prospective studies are needed to validate our findings. Furthermore, although polysomnography is considered the gold-standard test for capturing a comprehensive range of sleep parameters, our study utilized portable monitoring devices instead. It is important to note that portable monitoring devices offer convenience, mitigate the first-night effect observed in polysomnography, and have demonstrated comparable efficacy.33 Another potential limitation of our study is the lack of detailed information on OSA treatment, which could have provided further insights into the impact of treatment on the observed associations. Lastly, it is worth considering alternative echocardiographic measures for assessing right ventricular dysfunction, such as tricuspid annular plane systolic excursion, right ventricular/right atrial gradient, et al These measures have the potential to reveal associations between OSA and the severity of acute PE. However, it is important to acknowledge that these echocardiography criteria often suffer from issues of subjective assessment, reproducibility, and reliability.
Conclusions
In conclusion, OSA is common among acute PE patients and is associated with an elevated risk of disease severity and adverse outcomes. Implementing early screening and management of OSA as a routine part of care may aid in mitigating the disease burden and improving outcomes in individuals diagnosed with acute PE.
Abbreviations
AHI, apnea-hypopnea index; BMI, body mass index; ODI, oxygen desaturation index; OSA, obstructive sleep apnea; PE, pulmonary embolism; sPESI, simplified Pulmonary Embolism Severity Index; SpO2, oxygen saturation by pulse oximetry; T90, the percentage of cumulative time with SpO2 below 90% in total recorded time.
Data Sharing Statement
The data will be shared on reasonable request to the corresponding author, Zhihong Liu.
Ethical Approval and Informed Consent
This study was performed in line with the principles of the Declaration of Helsinki, and approval was granted by the Fuwai Hospital Ethics Committee. Informed consent was obtained from all patients included in the study.
Consent for Publication
The participant has consented to the submission of this article to the journal.
Acknowledgments
The authors would like to express their gratitude to all the participants for their cooperation and acknowledge the technical support (Embletta system) provided by Fuwai hospital, Chinese Academy of Medical Sciences and Peking Union Medical College.
Funding
This research article was supported by Beijing Municipal Science and Technology Project [Z181100001718200]; Beijing Municipal Natural Science Foundation [7202168]; CAMS Innovation Fund for Medical Sciences (CIFMS) [2020-I2M-C&T-B-055, 2021-I2M-C&T-B-032]; “Double First-Class” Discipline Construction Fund of Peking Union Medical College and Chinese Academy of Medical Sciences [2019E-XK04-02]; the Capital’s Funds for Health Improvement and Research (CFH) [2020-2-4033, 2020‐4‐4035]; National High Level Hospital Clinical Research Funding [2022-GSP-GG-35]; and Artificial Intelligence and Information Technology Application Fund of Fuwai Hospital, Chinese Academy of Medical Sciences [2022-AI01]. The funding sources were not involved in study design or in the collection, analysis or interpretation of data or in the writing of the report or in the decision to submit the article for publication.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Centers for Disease Control and Prevention (CDC). Venous thromboembolism in adult hospitalizations - United States, 2007–2009. MMWR Morb Mortal Wkly Rep. 2012;61(22):401–404.
2. Becattini C, Agnelli G, Lankeit M, et al. Acute pulmonary embolism: mortality prediction by the 2014 European Society of Cardiology risk stratification model. Eur Respir J. 2016;48(3):780–786. doi:10.1183/13993003.00024-2016
3. Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310–318. doi:10.1016/s2213-2600(15)00043-0
4. Javaheri S, Barbe F, Campos-Rodriguez F, et al. Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol. 2017;69(7):841–858. doi:10.1016/j.jacc.2016.11.069
5. Yeghiazarians Y, Jneid H, Tietjens JR, et al. Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;144(3):e56–e67. doi:10.1161/cir.0000000000000988
6. García Suquia A, Alonso-Fernández A, de la Peña M, et al. High D-dimer levels after stopping anticoagulants in pulmonary embolism with sleep apnoea. Eur Respir J. 2015;46(6):1691–1700. doi:10.1183/13993003.02041-2014
7. Konnerth D, Schwarz F, Probst M, et al. Is acute pulmonary embolism more severe in the presence of obstructive sleep apnea? Results from an observational cohort study. J Thromb Thrombolysis. 2018;46(2):253–259. doi:10.1007/s11239-018-1665-7
8. Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543–603. doi:10.1093/eurheartj/ehz405
9. Shitrit D, Peled N, Shitrit AB, et al. An association between oxygen desaturation and D-dimer in patients with obstructive sleep apnea syndrome. Thromb Haemost. 2005;94(3):544–547. doi:10.1160/TH05-02-0103
10. Hui DS, Ko FW, Fok JP, et al. The effects of nasal continuous positive airway pressure on platelet activation in obstructive sleep apnea syndrome. Chest. 2004;125(5):1768–1775. doi:10.1378/chest.125.5.1768
11. Joshi AA, Hajjali RH, Gokhale AV, et al. Outcomes of patients hospitalized for acute pulmonary embolism by obstructive sleep apnea status. Pulm Circ. 2021;11(2):2045894021996224. doi:10.1177/2045894021996224
12. Xie J, Wei YX, Liu S, Zhang W, Zhang XF, Li J. Obstructive sleep apnea hypopnea syndrome as a reason for active management of pulmonary embolism. Chin Med J. 2015;128(16):2147–2153. doi:10.4103/0366-6999.162498
13. Alonso-Fernández A, Suquia AG, de la Peña M, et al. OSA is a risk factor for recurrent VTE. Chest. 2016;150(6):1291–1301. doi:10.1016/j.chest.2016.07.011
14. Ghiasi F, Ahmadpoor A, Amra B. Relationship between obstructive sleep apnea and 30-day mortality among patients with pulmonary embolism. J Res Med Sci. 2015;20(7):662–667. doi:10.4103/1735-1995.166212
15. Berghaus TM, Faul C, von Scheidt W, Schwaiblmair M. The prevalence of sleep-disordered breathing among survivors of acute pulmonary embolism. Sleep Breath. 2016;20(1):213–218. doi:10.1007/s11325-015-1209-8
16. Barbero E, Mañas E, Bikdeli B, et al. Untreated obstructive sleep apnea and cardiovascular outcomes in patients with acute symptomatic pulmonary embolism. Thromb Res. 2022;214:87–92. doi:10.1016/j.thromres.2022.04.017
17. Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): the task force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J. 2019;54(3). doi:10.1183/13993003.01647-2019
18. Berry AC, Harding SM; American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.5. Darien, IL: American Academy of Sleep Medicine; 2018.
19. Roy PM, Penaloza A, Hugli O, et al. Triaging acute pulmonary embolism for home treatment by Hestia or simplified PESI criteria: the HOME-PE randomized trial. Eur Heart J. 2021;42(33):3146–3157. doi:10.1093/eurheartj/ehab373
20. Arnulf I, Merino-Andreu M, Perrier A, Birolleau S, Similowski T, Derenne JP. Obstructive sleep apnea and venous thromboembolism. JAMA. 2002;287(20):2655–2656. doi:10.1001/jama.287.20.2655
21. Le Mao R, Jiménez D, Bikdeli B, et al. Prognostic impact of obstructive sleep apnea in patients presenting with acute symptomatic pulmonary embolism. Thromb Haemost. 2021;121(6):808–815. doi:10.1055/s-0040-1721506
22. Olson LG, King MT, Hensley MJ, Saunders NA. A community study of snoring and sleep-disordered breathing. prevalence. Am J Respir Crit Care Med. 1995;152(2):711–716. doi:10.1164/ajrccm.152.2.7633731
23. Skinner MA, Choudhury MS, Homan SD, Cowan JO, Wilkins GT, Taylor DR. Accuracy of monitoring for sleep-related breathing disorders in the coronary care unit. Chest. 2005;127(1):66–71. doi:10.1378/chest.127.1.66
24. Toledo-Pons N, Alonso-Fernández A, de la Peña M, et al. Obstructive sleep apnea is associated with worse clinical-radiological risk scores of pulmonary embolism. J Sleep Res. 2020;29(2):e12871. doi:10.1111/jsr.12871
25. Xu J, Wang X, Meng F, et al. The role of obstructive sleep apnea on the prognosis of pulmonary embolism: a systemic review and meta-analysis. Sleep Breath. 2021;25(3):1419–1426. doi:10.1007/s11325-020-02258-z
26. Zhang W, Ding Y. Impact of obstructive sleep apnea on outcomes of pulmonary embolism: a systematic review and meta‑analysis. Exp Ther Med. 2023;25(3):120. doi:10.3892/etm.2023.11819
27. Sforza E, Roche F. Chronic intermittent hypoxia and obstructive sleep apnea: an experimental and clinical approach. Hypoxia. 2016;4:99–108. doi:10.2147/hp.S103091
28. Ferdinandy P, Schulz R, Baxter GF. Interaction of cardiovascular risk factors with myocardial ischemia/reperfusion injury, preconditioning, and postconditioning. Pharmacol Rev. 2007;59(4):418–458. doi:10.1124/pr.107.06002
29. Querejeta Roca G, Redline S, Punjabi N, et al. Sleep apnea is associated with subclinical myocardial injury in the community. The ARIC-SHHS study. Am J Respir Crit Care Med. 2013;188(12):1460–1465. doi:10.1164/rccm.201309-1572OC
30. Hong SN, Yun HC, Yoo JH, Lee SH. Association between hypercoagulability and severe obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2017;143(10):996–1002. doi:10.1001/jamaoto.2017.1367
31. Akyol S, Cortuk M, Baykan AO, et al. Biventricular myocardial performance is impaired in proportion to severity of obstructive sleep apnea. Tex Heart Inst J. 2016;43(2):119–125. doi:10.14503/thij-14-4868
32. Huang Z, Duan A, Hu M, et al. Implication of prolonged nocturnal hypoxemia and obstructive sleep apnea for pulmonary hemodynamics in patients being evaluated for pulmonary hypertension: a retrospective study. J Clin Sleep Med. 2023;19(2):213–223. doi:10.5664/jcsm.10286
33. Vat S, Haba-Rubio J, Tafti M, Tobback N, Andries D, Heinzer R. Scoring criteria for portable monitor recordings: a comparison of four hypopnoea definitions in a population-based cohort. Thorax. 2015;70(11):1047–1053. doi:10.1136/thoraxjnl-2014-205982
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.