Back to Journals » Patient Related Outcome Measures » Volume 12
Health Workers’ Practice Towards Smoking Cessation Intervention Based on 5A’s Model and Associated Factors in Public Hospitals, Hadiya Zone, Southern Ethiopia
Authors Tamirat T
Received 1 June 2021
Accepted for publication 1 September 2021
Published 16 September 2021 Volume 2021:12 Pages 291—298
DOI https://doi.org/10.2147/PROM.S322049
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Robert Howland
Temesgen Tamirat
Department of Public Health, Wachemo University, Hossana, Ethiopia
Correspondence: Temesgen Tamirat Email [email protected]
Background: The tobacco pandemic is one of the world’s most serious public health concerns, killing more than 8 million lives per year. The worst burden is in low- and middle-income countries. Unless appropriate action is taken, the burden may worsen. Health workers are among the actors to implement smoke cessation interventions. However, the level of intervention practices towards smoke cessation was not defined.
Objective: To determine health workers’ practice towards smoke cessation interventions based on 5A’s model and associated factors in public hospitals.
Methods: Facility-based cross-sectional design was used. All public hospitals found in the Hadiya zone were included in the study. From each public hospital, representative number of health workers, who fulfil inclusion criteria, were included in the study. A total of 323 sample size of health workers were used. A self-administered questionnaire was employed to collect data. Both descriptive and advanced analyses were performed using SPSS software version 20.0. In bivariable analysis, variables with p-value < 0.25 were considered for multivariable analysis. Finally, odds ratio with 95% CI and p-value < 0.05 were used to declare factors as significantly associated with the outcome variable.
Results: About 97% of health care workers had poor practice on smoking cessation interventions. About 7.4% (23) health workers reported as they were current smokers. Moreover, only 28% of health workers asked their patients about smoking status. Being females, having < 10 years of service, training and having good knowledge was significantly associated with the outcome variable.
Conclusion: Majority of the healthcare workers surveyed did not provide smoking cessation interventions. Identified statistically significant factors with the practice of smoke cessation interventions in this study were sex, knowledge, training and service years. Therefore, strategies should be designed and implemented to improve and equip the health workers towards practising of smoke cessation interventions by instituting smoke cessation programs.
Keywords: smoking, cessation, intervention, practice
A Letter to the Editor has been published for this article.
Background and Problem Statement
The tobacco epidemic is one of the world’s most serious public health concerns and takes the lives of more than eight million people each year.1 Tobacco production and consumption have shifted to developing nations, and around 80% of the 1.1 billion people aged 15 and above who smoke live in poor and middle-income nations. Tobacco production and consumption harm people’s health and the economies and environments of developing countries.2 Smoking also affects nearly every organ in the body, causes a variety of diseases, decreases smokers’ overall health and even causes preventable death.3
Quitting smoking lowers the risk of several health consequences, including poor reproductive health, cardiovascular disease, chronic obstructive pulmonary disease and cancer. Even people who have been diagnosed with heart disease or chronic obstructive pulmonary disease can benefit from quitting smoking.4 When compared to continuing to smoke, quitting can add up to ten years to a person’s life. Furthermore, quitting smoking when young can further reduce health risks, although quitting at any age can allow people to reclaim years of their lives that might otherwise be lost if they continue to smoke.5
Even though factors such as low awareness of quitting strategies and the smoking status of health-care workers as well as a lack of nicotine replacement therapy, cessation programs, formal training and loose anti-smoking violators laws all contribute to the failure of smoking cessation interventions, patients are likely to accept advice about changing their smoking habits from an acknowledged health-care expert; this can increase the likelihood of smoking cessation.6–8
Healthcare providers can assist patients by advising, providing brief counselling, prescribing cessation medication, referring them to additional services, such as a quitline, and providing ongoing support to help them avoid relapse.4
Tobacco control may require the participation of health professionals since health workers gain the public’s trust, as well as the media’s and opinion leaders, and their views are heard in a wide range of social, economic, and political arenas, particularly on health aspects.9
The annual death toll might surge to more than eight million by 2030 unless urgent action is taken. Parties to the World Health Organization Framework Convention on Tobacco Control are urged to take effective legislative, executive, administrative, and other measures at the national, regional, and international levels to reduce tobacco consumption, nicotine addiction, and tobacco smoke exposure.10
On June 23, 2014, Ethiopia became a party to the WHO Framework Convention on Tobacco Control. In all internal public areas, workplaces, and all modes of public transportation, smoking and the use of any tobacco product is prohibited.11
During a normal consultation and/or interaction with a physician or health care provider, all tobacco users are offered advice to quit smoking, which normally takes only a few minutes.12 Every clinic contact provides an opportunity to encourage smoking cessation by assessing each patient’s willingness to quit smoking. Using a model known as the “5 A’s” is one way to do this.13 Since this model contains 5A’s components (ask, advise, assess, assist and arrange) that help health workers to practice on smoke cessation intervention. As a result, in developing countries like Ethiopia, several factors including the unavailability of pharmacotherapy affect smoke cessation intervention. So, behavioural counselling based on the “5 A’s” model is the best option for quitting smoking. However, the level of smoking cessation therapy practised by health care personnel based on the “5 A’s” model was unknown. So, this study aimed to determine health workers’ practice towards tobacco cessation intervention based on the “5 A’s” model and associated factors in the Hadiya zone, southern Ethiopia.
Methods
Study Area and Study Period
The study was conducted in all the four public hospitals of the Hadiya zone, southern Ethiopia, from August 15th to October 21st 2020. Hadiya zone is found in southern Ethiopia and is located 232 km away from the capital of Ethiopia, Addis Ababa. The zone has 4 public hospitals including Wachemo University Nigest Ellen Mohammed memorial comprehensive specialized hospitals, that is three district hospitals and one comprehensive specialized hospital. These four hospitals serve more than two million population in the catchment areas and the surroundings.
Study design: A facility cross-sectional study design was employed to collect quantitative data.
Study population: All health care workers in public hospitals of Hadiya zone.
Sampled population: All sampled health care workers working in all the four public hospitals in the Hadiya zone and who were willing to participate in the study. Health workers working in each hospital whose work experience was less than six months were excluded.
Sample Size Determination and Sampling Procedure
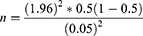
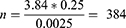
The sample size was determined by using a single population proportion formula as follows:
This gives the maximum possible sample size
Where,
P = proportion of health workers’ practice = 50%, since no study conducted on smoke cessation intervention particularly among health professionals.
d = Margin of error-5% (0.05)
α = Critical value at 95% CI (1.96)
Since, the number of total health workers in the study areas (N) were less than 10,000 (ie 1260); therefore, we used the correction formula. Finally, the final sample size (Nf) was estimated to be
By adding a 10% non-response rate, the final sample size was observed to be 323.
Sampling Technique
All 4 public hospitals in the Hadiya zone were purposively included in the study. In each included Hospital, the total number of health workers who should have primary contacts with patients were identified (medical doctors, public health officers, nurses, midwives and dentists). Then, the sample size was proportionally allocated to each hospital according to the number of health workers they had. Then, in each hospital, a total number of health workers in each cadre were determined, and representative samples were provided. Then, finally, simple random sampling techniques (lottery method) was used to collect data from participants based on the sampling frame prepared.
Study Variables
Dependent variable: Health workers’ practice.
Independent variables: Socio-demographic variables, professional categories, knowledge, and cessation activities (“5 A’s” model).
Data Collection Methods
The data were collected by a self-administered questionnaire that was adopted after reviewing relevant literature. It was first developed in English then translated into Amharic and translated back into English for appropriateness and easiness in approaching study participants.
The questionnaire aimed to assess health workers: socio-demographic characteristics, knowledge, current smoking cessation activities based on the five “A’s” model (Ask, Advise, Assess, Assist, and Arrange follow-up) to smoking cessation interventions among patients.
Data were collected by trained nurses and supervised by public health officers. Training aim was to enhance understanding of questionnaires, data collection methods and the way they handle challenges. The training was also supposed to deal with maintaining privacy and confidentiality.
Data Quality Assurance
One-day training was given for the data collectors and supervisors on the objective, methodology, and data collection methods. The data collection tool was translated to the local language Amharic and translated back to English. The pre-test was done on 5% of the actual sample size in the health facilities that were not included in the actual survey to ensure completeness, consistency and applicability of the methods or self-administered tools/questionnaires.
Data Processing and Analysis
The data were cross-checked for completeness, then entered into Epi-Data version 3.1 software and exported to SPSS version 20.0 software for further analysis. Descriptive statistics like percentages, proportions, and mean was used. The results were presented using tables, text, and charts. For the associated factors, binary logistic regression analysis was done since the outcome variable is binary. Both bi-variable and multivariable binary logistic regression analyses were employed. Model fitness was assessed using the Hosmer-Lemeshow test. Variables with a p-value of less than 0.25 in the bi-variable logistic regression were considered for the multivariable logistic regression analysis. In the multivariable logistic regression, adjusted odds ratio (AOR) with a 95% confidence interval and p-value of less than 0.05 was used to declare the factors significantly associated with health workers’ practice.
Ethical Consideration
Ethical approval committees of Wachemo University have approved this study according to the relevant guidelines and regulations of the university. A formal letter was obtained from Wachemo University and submitted to the hospital administrators. After permission was obtained, informed consent was obtained from all the subjects after clearly explaining the purpose of the study since there is no need to take a blood sample, body fluid or others, other than verbal responses. They have been told that we could withdraw from the involvement at any time without any restriction. The confidentiality of participants was also ensured throughout the research process.
Operational Definition
Knowledge of Smoking Cessation Intervention
Knowledge about smoking cessation therapy was derived from the 20 knowledge-based questions in the questionnaire. For each question, 1 point was assigned if the response is correct and zero points, if the response is incorrect or not known. Finally, after summation of all the points, if the total score found in between 0 and 9, the participant was categorized as having poor knowledge, 10–14 indicates having medium knowledge and 15–20 points indicate good knowledge of smoking cessation therapy.11
Practice Towards Smoking Cessation Intervention
This was derived from the 10 practice-based questions in the questionnaire. For each question, 2 points were assigned if the participant responds as “always”, 1 point if “sometimes”, and 0 points if the participant responds as “never”. Finally, after summation of points, if the total score is 0–9 the participant was categorized as having a practice poor practice and 10–20 points were categorized as having good practice.
Result
A total of 314 health workers participated in the study, providing a 97.2% response rate.
Socio-Demographic Characteristics of Health Workers
Out of 314 participants, 56% (N=177) female and 43.6% (N=137) were male. The majority (70.4%) of the participants were in the age range of 21–30 years, with a mean of 28.87 (±4.4) years, with 21 and 48 minimum and maximum age, respectively. Among the total respondents, more than half of the respondents were nurses (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Health Workers |
The Practice of Smoking Cessation Intervention
The health workers’ practice level was categorized as having a poor practice (score of 0–9) and having a good practice (score of 10–20). According to this study, about 97% (306) of the health workers were poorly practising smoking cessation intervention, which means only 3% of health workers had good practice towards smoking cessation intervention in the study area.
Health Care Workers’ Practice of Smoke Cessation Intervention Based on “5 A’s” Model
Health workers’ practice according to 5A’s model, 28% (88) health workers usually ask about the patients’ smoking status. However, the majority 68.5% (215) respondents enquire sometimes. But, the remaining 3.5% of the health care providers never ask about patient smoking status. Moreover, 20.4% (64) health workers usually ask about the number of cigarettes smoked per day by the patient, whereas 65.6% (206) inquired some time, but the remaining health workers never. Only 21.3% (67) of the respondents always keep a record of the patients’ smoking history in the medical records, 62.1% (195) respondents used to record sometimes, and the remaining 16.6% never.
In the advice components of 5A’s model, only 24.2% (76) respondents always advised their patients to quit, whereas 47.5% (149) individuals used to advise their patients rarely and 28.3% of them never advise.
Among the respondents, only 18.8% (59) of them always asked their patients about the previous attempt to quit smoking, while 38.9% (122) enquired sometimes, and the remaining did never. In the assessment components of 5A’s model, only 19.4% (61) of the respondents usually assessed if patients were willing to quit at that particular time, whereas 51.3% (161) of the respondents sometimes used to assess and the remaining 29.3% never enquire. In the arrange to follow-up components of 5A’s, about 9.6% (30) of the respondents did always set up a follow-up appointment to review the progress of patients on quitting smoking, whereas 57.6% (181) respondents did sometimes, and the remaining 32.8% never attempted (Table 2).
 |
Table 2 Health Care Workers’ Practice of Smoke Cessation Intervention Based on 5A’s Model |
Associated Factors with Smoking Cessation Intervention
In multivariable analysis, being female, receiving training, good knowledge score, and worked for less than 10 years were statistically significantly associated with health workers’ practice.
Among socio-demographic characters, male health workers were 2.25 times more likely to have good practice of smoking cessation intervention than female health workers (AOR = 2.25, 95% CI 1.31–6.23). Similarly, those health workers who worked <10 years were 4.75 times more likely to have good practising of smoking cessation intervention when compared to those who worked >10 years (AOR = 4.75, 95% CI 1.756–9.547).
In this study, health workers who were trained on smoking cessation intervention were 6.5 times more likely to have good practising of smoking cessation intervention as compared to health workers who were not trained (AOR = 6.5, 95% CI 2.366–11.557). Similarly, health workers with good knowledge levels were 3.25 times more likely to have good practice of smoking cessation intervention as compared to those with poor knowledge levels (AOR= 3.25, 95% CI 1.965–9.332) (Table 3).
 |
Table 3 Factors Associated with Health Workers’ Practice Towards Smoking Cessation Interventions |
Discussion
Despite health workers have an important role in providing evidence-based tobacco interventions for both smoking cessation and prevention, only 3% of the health workers practiced smoke cessation interventions in this study.
Practice Level in the Provision of Smoking Cessation Therapy
In the ask components of the 5A’s model, only 28% of the health workers asked about patient smoking status. This result was nearly similar with the study done in Kenya,6 only 34.9% of the health workers asked their patients’smoking status. Likewise, on the rest of 5A’s model components both in this study and in a study conducted in Kenya showed that health workers’ responses to the always choice were much lower than sometimes and never options. However, research conducted in Europe,6 Malta,6 and the United States14 indicated that a majority of health workers asked about their patients’ smoking status. In addition, most respondents’ responses were always on the option of each component of the model. In this study, The low level of performance in 5A’s delivery confirms that smoke cessation intervention practices are unlikely launched and implemented in the study setting. This might affected practice of smoke cessation intention.
In this study, gender of the health workers was significantly associated with the smoke cessation intervention in the study area. Male health workers were 2.25 times more likely to practice smoke cessation intervention than females. This finding was similar with studies conducted in India,15 Italy,17 Kenya,6 the Catalan Network of Smoke-Free Hospitals,16 and Malta.6 The reason for the discrepancy of practicing smoke cessation intervention in the study area might be due to the varying awareness between male and female health workers as a result of lack of training, guidelines and obligations.
A few number of health workers (3.5%) reported that they had received formal training on smoke cessation intervention in this study. This finding was similar with the studies conducted in Kenya,6 Italy17 and Saudi Arabia.18 In Kenya only 11%, in Italy only 5.8% and in Saudi Arabia 31.4% of the health workers had received formal training on smoke cessation intervention. The reason for this limited training on smoke cessation intervention might be due to lack of smoke cessation programs, guidelines, commitment from the concerned bodies to introduce and implement cessation intervention programs or misunderstanding of smoking burden.
Receiving training has statistically significant association with health workers’ practice towards smoke cessation intervention in this study. Those health workers received formal training were 6.5 times more likely to practice smoke cessation intervention as compared to health workers who did not receive formal training. This study matched findings from Kenya,6 the Catalan Network of Smoke-Free Hospitals,16 India,15 Europe,13 and America.7 Because training health workers on smoke cessation intervention might improve the level of knowledge, confidence and performance they had.
Health workers who had good knowledge were better practicing smoke cessation interventions more likely than the rest of the group. This finding was consistent with what was discovered in Kenya.6 This might be supported by evidence-based and effective smoke cessation interventions service delivery for their patients.
Similarly, health workers who had worked for less than ten years were 4.75 times more likely to have used a smoking cessation intervention than those who had worked for more than ten years. This result differed from that of a smoke-free hospital in the Catalan network.16 Smoke cessation interventions were performed better by health personnel with more than 14 years of experience than their counterparts. This difference might be due to the smoking cessation intervention is gaining better insights in the study area than in the past, or perhaps smoke cessation intervention was learned via experiences in Catalan health workers.
Conclusion
In conclusion, majority of the healthcare workers surveyed did not provide smoking cessation interventions to their patients in the study area.
There was minimum practice of all the smoking cessation interventions under 5A’s model. Since, majority of percentage scores in each component of the model was on sometimes and never practising options.
Identified statistically significant factors with the practice of smoke cessation interventions in this study were sex, knowledge, training and service years.
Therefore, strategies should be designed and implemented to improve and equip the health workers towards practicing of smoke cessation interventions by instituting smoke cessation programs and supportive materials like guidelines and providing regular training.
Data Sharing Statement
The datasets of this study are available on reasonable request.
Ethics Approval and Consent to Participant
Ethical approval committees of Wachemo University have approved this study according to the relevant guidelines and regulations of the university. A formal letter was obtained from Wachemo University and submitted to the hospital administrators. After permission was obtained, informed consent was signed from all the subjects after clearly explaining the purpose of the study. This study complies with the Declaration of Helsinki. They have been told that we could withdraw from the involvement at any time without any restriction. The confidentiality of participants was also ensured throughout the research process.
Acknowledgment
I would like to extend my gratitude to Wachemo University, my colleagues and data collectors for their valuable contribution to this study.
Disclosure
The author report no conflicts of interest in this work.
References
1. World health organization. World health organization(WHO)-report on tobacco pandemic. May 27, 2020.
2. ASH. Fact sheet: tobacco and the developing world. July, 2019. Available from: http://ash.org.uk/category/information-and-resources/.
3. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
4. A summary of smoking cessation: a report of the surgeon general – 2020. Smoking cessation – the role of healthcare professionals and health systems. 2020.
5. American Cancer Society. Health benefits of quitting smoking over time. cancer.org | 1.800.227.2345. 2020.
6. Gichuki JW, Opiyo R, Mugyenyi P, Namusisi K. Healthcare providers’ level of involvement in provision of smoking cessation interventions in public health facilities in Kenya. J Public Health Afr. 2015;6(2):523. doi:10.4081/jphia.2015.523
7. Stead M, Angus K, Holme I, Cohen D, Tait G; PESCE European Research Team. Factors influencing European GPs’ engagement in smoking cessation: a multi-country literature review. Br J Gen Pract. 2009;59(566):682–690. PMID: 19674514; PMCID: PMC2734357. doi:10.3399/bjgp09X454007
8. Greenhalgh EM, Jenkins S, Stillman S, Ford C. 7.7 factors that predict success or failure in quit attempts. In: Greenhalgh EM, Scollo MM, Winstanley MH, editors. Tobacco in Australia: Facts and Issues. Melbourne: Cancer Council Victoria; 2016. Available from: http://www.tobaccoinaustralia.org.au/7-7-personal-factors-associated-with-quitting.
9. WHO Tobacco Free Initiative. The Role of Health Professionals in Tobacco Control. 2005.
10. WHO regional office for Africa. Enforcement of and Compliance with Tobacco Control Legislation; 2016.
11. Tobacco control law. Legislation by Country Ethiopia; February 13th, 2020.
12. WHO. WHO Report on the Global Tobacco Epidemic; 2019.
13. Elyse R Park. UPTO DATE, Behavioral Approaches to Smoking Cessation; 2020.
14. Ganz O, Fortuna G, Weinsier S, Campbell K, Cantrell J, Furmanski WL. Exploring smoking cessation attitudes, beliefs, and practices in occupational health nursing. Workplace Health Saf. 2015;63(7):288–296. PMID: 26187173. doi:10.1177/2165079915578582
15. Martínez C, Castellano Y, Andrés A, et al. Factors associated with the implementation of the 5A’s smoking cessation model. Tob Induc Dis. 2017;15:41. doi:10.1186/s12971-017-0146-7
16. Binnal A, Gururaghavendran R, Denny C, Ahmed J, Tallada AK. Tobacco cessation scenarios among healthcare profession students: a Multidisciplinary Study. Asian Pac J Cancer Prev. 2018;19(4):1081–1088. doi:10.22034/APJCP.2018.19.4.1081
17. Thy T, Boker T, Gallefoss F, Bakke PS. Hospital doctors’ attitudes toward giving their patients smoking cessation help. Clin Respir J. 2007;1(1):30–36. doi:10.1111/j.1752-699X.2007.00005.x
18. Saudi Arabia: Jradi H. Awareness, practices, and barriers regarding smoking cessation treatment among physicians in Saudi Arabia. J Addict Dis. 2017;36(1):53–59. PMID: 26566876. doi:10.1080/10550887.2015.1116355
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.