Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Global, Regional, and National Burden of COPD Attributable to Occupational Particulate Matter, Gases, and Fumes, 1990–2019: Findings from the Global Burden of Disease Study 2019
Authors Su X, Gu H, Li F, Shi D, Wang Z
Received 24 August 2023
Accepted for publication 5 December 2023
Published 12 December 2023 Volume 2023:18 Pages 2971—2983
DOI https://doi.org/10.2147/COPD.S436879
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Xin Su,1,* Hengqiong Gu,1,* Fajun Li,2 Donglei Shi,3 Zhaojun Wang3
1Department of Respiratory, Hainan Hospital of PLA General Hospital, Sanya, People’s Republic of China; 2Department of Critical Care Medicine, The First People’s Hospital of Kunshan, Kunshan, People’s Republic of China; 3Department of Thoracic Surgery, The Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Donglei Shi; Zhaojun Wang, Department of Thoracic Surgery, The Seventh Affiliated Hospital, Sun Yat-sen University, 628 Zhenyuan Road, Shenzhen, 518107, People’s Republic of China, Tel/Fax +86-755-81206874, Email [email protected]; [email protected]
Background: A study aimed to estimate the burden of Chronic obstructive pulmonary disease (COPD) caused by occupational exposure to particulate matter, gases, and fumes in 204 countries from 1990 to 2019.
Methods: Data on the deaths number, age-standardized mortality rates (ASMR), and age-standardized disability-adjusted life years (DALYs) rates (ASDR) of COPD attributable to occupational particulate matter, gases, and fumes were collected from the GBD study 2019. We also investigated the association between the ASDR and SDI.
Results: There were 517.7 thousand deaths [95% UI: 413.9 to 634.5] in 2019. The number of deaths increased from 1990 to 2019. The ASMR and ASDR were 6.61 (5.24 to 8.17) and 143.02 (118.56 to 168.69) in 2019, respectively, representing a 46% and 44.5% decrease since 1990. China had the highest number of deaths [200,748.4 (151,897.6 to 260,703.9)], while Nepal had the highest ASMR [39 (27.7 to 50)] and ASDR [724.5 (549 to 894.2)]. Males and females 75– 79 and 80– 84 years old had the highest number of COPD deaths. A negative correlation was observed when SDI > 0.4, whereas a positive correlation was found when SDI < 0.4.
Conclusion: From 1990 to 2019, there was an increase in the number of deaths, but a decline in ASMR and ASDR globally. Besides, there was a heterogeneous burden of COPD attributable to occupational particulate matter, gases, and fumes across regions and countries. It is important to develop and implement strategies to prevent and reduce the burden of COPD attributable to occupational particulate matter, gases, and fumes.
Keywords: chronic obstructive pulmonary disease, occupational particulate matter, gases, fumes, global burden of disease, deaths number, age-standardized rates
Introduction
Chronic obstructive pulmonary disease (COPD) is a lung disorder characterized by airway obstruction that causes shortness of breath and coughing. It manifests after long-term inhalation of irritant gases such as cigarette smoke and chemicals.1 According to World Health Organization (WHO), COPD is the world’s third greatest cause of death, accounting for 3.23 million deaths in 2019.2 COPD is a major public health concern, particularly in poor and middle-income nations, where over 90% of COPD deaths occur.1,2 According to the latest Global Burden of Disease (GBD) study, the DALYs of COPD have risen from 13th in 1990 to 6th in 2019, globally.3 With the growing global population and the aging population, COPD is expected to become more common over the next several decades.4,5
Occupational exposure accounts for 15–20% of the burden of COPD in the population.6,7 Some of the risk factors for getting COPD include age, occupational exposure to dust and fumes, indoor and outdoor air pollution, genetic risk factors, and most notably, tobacco smoking.2,8 Over the last 40 years, scientific evidence on the link between workplace exposure and COPD has accumulated.9 Population-based studies provide evidence supporting a causal relationship between occupational exposures and COPD development.7 Several studies have found that occupational exposure to vapors, dusts, gases, and fumes impairs large airway function and raises the risk of COPD.7,10,11 Despite efforts to minimize dust exposure, the construction and building industry continues to pose a challenge for occupational health and safety protection.12,13 A study of Swedish construction workers found that occupational exposure to air pollution, such as inorganic dust, gases, and fumes, increases COPD incidence, especially among non-smokers.11 Jong et al reported that smokers and non-smokers both experience small airway obstruction due to exposure to gases, vapors, dusts, or fumes.10 However, there is no comprehensive assessment of the impact of occupational particulate matter, gases, and fumes on COPD.
The COPD burden attributed to risk factors has been reported using GBD 2019. These papers primarily discuss the burden of COPD associated with risk factors.14–16 Until now, there has not been a study examining the most recent changes in COPD attributed to occupational particulate matter, gases, and fumes burden based on GBD 2019. To estimate the global, regional, and national burdens of COPD attributed to occupational particulate matter, gases, and fumes across 204 nations and territories between 1990 and 2019, we used data from the GBD 2019 database for a second analysis. We scrutinized the temporal trends in COPD attributed to occupational particulate matter, gases, and fumes on a global and regional scale spanning from 1990 to 2019. This analysis aims to enhance our comprehension of the burden imposed by COPD attributed to occupational particulate matter, gases, and fumes. Furthermore, we delved into exploring the correlation between COPD and the Social Demographic Index (SDI), attributing this relationship to the burden posed by occupational particulate matter, gases, and fumes. The results would raise awareness of occupational particulate matter, gases, and fumes among people worldwide and contribute to the development of tailored preventative and intervention plans for these workers in various geographical areas.
Methods
Overview
The GBD study, led by the Institute for Health Metrics and Evaluation (IHME), is the largest global observational epidemiological study conducted to date.17 More than 7000 researchers gather and examine data for the Global Burden of Disease in 156 nations and territories.18 From 1990 to 2019, the GBD 2019 investigated 369 diseases and injuries and 87 risk factors globally, regionally, and nationally.3,19,20 The methods used to determine the disease burden and analyze each measure in GBD 2019 have been described in detail previously.3 The general framework established for comparative risk assessment (CRA), used in GBD since 2002, was followed for the GBD 2019 estimation of attributable burden.3,21,22
Data Sources
Data on COPD prevalence, incidence, and remission are obtained from literature provided by collaborators or systematic reviews. Other sources of data include vital registrations for cause of death and hospital claims for non-fatal estimates. Measures based on spirometry are included in all data.3 In GBD 2019, there are four risk factor hierarchies: behavioral, environmental, occupational, and metabolic risk factors are at level 1; twenty risks or groups of risks are included in level 2, 52 risks or groups of risks are included in level 3, and 69 specific risk factors are included in level 4.19 Occupational particulate matter, gases, and fumes belong to level 3.19 Five categories–high SDI, high-middle SDI, middle SDI, low-middle SDI, and low SDI–are used to classify countries and territories according to the SDI, which ranges from 0 to 1.0 represents the lowest level of development and 1 represents the highest. The SDI is a composite indicator of a nation’s lag-distributed per capita income, average years of schooling, and fertility rate among females under 25.23 The data used in this study on the burden of COPD attributable to occupational particulate matter, gases, and fumes were derived from the GBD Results Tool (https://vizhub.healthdata.org/gbd-results/). We downloaded SDI data from this website (https://ghdx.healthdata.org/record/ihme-data/gbd-2019-socio-demographic-index-sdi-1950-2019). According to the GBD 2019, the estimates are based on age-standardized rates per 100,000 population.
Definitions
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification, COPD is defined as a measurement of <0.7 FEV1/FVC (one second of forceful exhalation/total forceful expiration) in a person.3 COPD severity was also graded based on the GOLD classification. It is characterized as mild (I), moderate (II), or severe or very severe combined (III, IV) when the FEV1 score is 80%, 50–79%, or 50% of the normal value, respectively.3,14 COPD included diseases coded J41, J42, J43, J44, and J47 in the International Classification of Diseases (ICD) version 10 and 491–492, and 496 in ICD version 9.
Statistical Analysis
The deaths number, and ASMR and ASDR were the main indices used to evaluate the burden of COPD attributable to occupational particulate matter, gases, and fumes. All estimates were reported with a 95% uncertainty interval (UI). To visualize the geographic variation regarding COPD attributable to occupational particulate matter, gases, and fumes in the number of deaths, ASMR, and ASDR in 2019, we generated maps of COPD attributable to occupational particulate matter, gases, and fumes. Percentage changes in COPD attributable to occupational particulate matter, gases, and fumes deaths number, ASMR and ASDR from 1990 to 2019 were defined as (Number2019-Number1990)/Number1990 ×100%. We assessed the relationship between the burden of COPD attributable to occupational particulate matter, gases, and fumes and SDI based on location and year. We used R statistical software (version 4.1.2) to analyze and visualize the data.
Results
Global Level
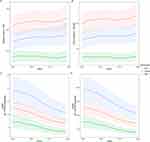
Between 1990 and 2019, Figure 1 shows global trends for deaths, DALYs, ASMR, and ASDR due to COPD attributable to occupational particulate matter, gases, and fumes. The deaths and DALYs of COPD attributable to occupational particulate matter, gases, and fumes increased from 1990 to 2019 in both sexes and males, but not significantly in females. On the other hand, the ASMR, and ASDR decreased gradually. The deaths and DALYs of COPD attributable to occupational particulate matter, gases, and fumes were lower in females than in males. The ASMR and ASDR of COPD attributable to occupational particulate matter, gases, and fumes were higher in males than in females (Figure 1).
Globally, the total deaths of COPD attributable to occupational particulate matter, gases, and fumes increased by 18.6%, from 436.4 thousand (95% UI: 340.3 to 518.2) in 1990 to 517.7 thousand (413.9 to 634.5) in 2019. The ASMR decreased by 46% from 12.23 (9.47 to 14.57) in 1990 to 6.61 (5.24 to 8.17) in 2019 per 100,000 population. Meanwhile, the ASDR of COPD attributable to occupational particulate matter, gases, and fumes was 257.92 (206.41 to 302.34) per 100,000 population in 1990 and 143.02 (118.56 to 168.69) per 100,000 population in 2019, with a percentage change of −44.5% (Table 1).
Regional Level
Among 21 GBD regions based on geography, the deaths of COPD attributable to occupational particulate matter, gases, and fumes were highest in East Asia 206.7 thousand (95% UI: 157.9 to 267.4) and South Asia 172.9 thousand (130.7 to 215.8) in 2019. Oceania 0.7 thousand (0.5 to 0.9) and Australasia 0.9 (0.7 to 1.2) had the lowest number of deaths in 2019. Compared to 1990, the deaths number of COPD attributable to occupational particulate matter, gases, and fumes in most regions increased in 2019, the highest rise was seen in Central Latin America (158.1%). However, the deaths number of COPD attributable to occupational particulate matter, gases, and fumes was deceased in only three regions [Central Europe (−17.3%), East Asia (−17.8%), and Eastern Europe (−42.4%)]. The highest ASMR of COPD attributable to occupational particulate matter, gases, and fumes in 2019 occurred in South Asia [14.82 (10.95 to 18.65)], Oceania [12.73 (9.15 to 16.6)], and East Asia [11.79 (8.81 to 15.45)] per 100,000 population. The ASMR of COPD attributable to occupational particulate matter, gases, and fumes increased in the Caribbean (9.4%) and High-income North America (7.3%) between 1990 and 2019 and decreased in other 21 GBD regions. South Asia 304.05 (239.42 to 370.44), Oceania 259.19 (195.41 to 332.92), and East Asia 210.73 (168.47 to 263.54) had the highest ASDR per 100,000 population in 2019, while High-income Asia Pacific had the lowest ASDR [24.07 (18.38 to 30.94)] per 100,000 population. Only the Caribbean region has seen an increase in ASDR (12.3%) from 1990 to 2019, at the same time, the remaining 20 regions were all decreased, the biggest decline in East Asia (−69.3%) from 1990 to 2019 (Table 1).
National Level
Among 204 countries and territories, China [200,748.4 (95% UI: 151,897.6 to 260,703.9)] and India [148,380.2 (106,620.1 to 187,390.9)] were the two countries with the highest deaths number of COPD attributable to occupational particulate matter, gases, and fumes in 2019. The deaths number of COPD attributable to occupational particulate matter, gases, and fumes was less than 1 in some countries (Antigua and Barbuda, San Marino, Cook Islands, Tuvalu, Nauru, Niue, and Tokelau) (Figure 2A and Supplementary Table 1). The highest ASMR in 2019 occurred in Nepal [39 (27.7 to 50)] per 100,000 population, followed by Bhutan [16.9 (11.3 to 24.5)], Nepal is more than twice as many as Bhutan. The ASMR of COPD attributable to occupational particulate matter, gases, and fumes was less than 1 in 11 countries (Figure 2B and Supplementary Table 2). The highest ASDR in 2019 were observed in Nepal [724.5 (549 to 894.2)] and Democratic People’s Republic of Korea [329.5 (253.7 to 410.7)] per 100,000 population (Figure 2C and Supplementary Table 3).
Age and Sex Patterns
The number of deaths and DALYs was lower in females than males in 2019, except 95-plus-year-old age group. In 2019, the deaths number of COPD attributable to occupational particulate matter, gases, and fumes was highest in the 75–79-year-old and 80–84-year-old age group for males and females, respectively. The ASMR of COPD attributable to occupational particulate matter, gases, and fumes started increasing in the early age groups and peaked in the 85–89-year-old and 95-plus-year-old age groups for males and females, respectively. The number of age-specific DALYs peaked in 70–74-year-old in males and females. Age-specific rates of DALYs increased during the middle ages in both genders, and peaked in the 85–89-year-old and 80–84-year-old age group for males and females, then decreased in both genders (Figure 3).
Association with the SDI
Middle SDI had the highest deaths number of COPD attributable to occupational particulate matter, gases, and fumes [180.7 thousand (95% UI: 143.6 to 226.9)] in 2019. High SDI had the lowest deaths number of COPD attributable to occupational particulate matter, gases, and fumes [40.2 (30.3 to 52)]. Compared with 1990, the deaths number of COPD attributable to occupational particulate matter, gases, and fumes was declined only in High-middle SDI (−23.9%) in 2019, while the remain SDI all increased, with the highest increased in Low SDI (79.3%). Low-middle SDI had the highest ASMR [14.55 (11.08 to 18.1)] and ASDR [292.95 (236.01 to 349.52)] per 100,000 population in 2019. High SDI had the lowest ASMR [1.92 (1.48 to 2.43)] and ASDR [52.97 (43.48 to 62.87)] per 100,000 population in 2019. The ASMR and ASDR of COPD attributable to occupational particulate matter, gases, and fumes were declined between 1990 and 2019 (Table 1).
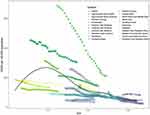
Our study examined the relationship between SDI and the corresponding ASDR of COPD attributable to occupational particulate matter, gases, and fumes in 21 GBD regions between 1990 and 2019. On the whole, a non-linear-shaped relationship was observed between the ASDR of COPD attributable to occupational particulate matter, gases, and fumes and SDI from 1990 to 2019. The SDI and ASDR of COPD attributable to occupational particulate matter, gases, and fumes were negatively associated when SDI exceeded 0.4. However, there is a positive correlation when SDI is less than 0.4. Western Sub-Saharan Africa, North Africa and Middle East, Central Latin America, Caribbean, Andean Latin America, Tropical Latin America, Southern Latin America, and High-income Asia Pacific all had lower than expected ASDR, from 1990 to 2019. East Asia, South Asia, Oceania, and High-income North America had higher than expected from 1990 to 2019. A higher burden of ASDR was observed in Australasia, Eastern Sub-Saharan Africa, and Central Sub-Saharan Africa during the early years, but it declined in the latter years (Figure 4).
Discussion
This study was carried out to assess the global burden of COPD caused by occupational particulate matter, gases, and fumes. The number of deaths and DALYs of COPD attributable to occupational particulate matter, gases, and fumes increased from 1990 to 2019, while the ASMR and ASDR showed a declining trend. The number of COPD deaths attributed to occupational particulate matter, gases, and fumes increased by 18.6% compared to 1990. We also found that the burden of COPD attributable to occupational particulate matter, gases, and fumes was considerably higher among the elderly and males. Moreover, a non-linear relationship was observed between the SDI and the ASDR of COPD attributable to occupational particulate matter, gases, and fumes, with a negative association when the SDI exceeded 0.4 and a positive correlation when the SDI was less than 0.4.
Clinical and scientific advances have resulted in a better knowledge of COPD and improved patient treatment. Although there is no cure for COPD,2 COPD is still a preventable and avoidable disease.2,9 Treatment can help control symptoms, halt disease development, and enhance a person’s quality of life. Common COPD therapies included: a combination of medications such as bronchodilators and corticosteroids to open airways and reduce inflammation; oxygen therapy for severe cases; pulmonary rehabilitation to improve muscle strength and lung function; surgery in some cases such as lung volume reduction or transplantation; and lifestyle changes such as quitting smoking and avoiding irritants.24,25
Despite the knowledge that tobacco smoking, secondhand smoking, air pollution, and exposure to fuel oil fumes are the primary risk factors for COPD.26 Pollutants in the workplace, particularly inorganic dust, can cause airway injury and inflammation, which are hallmarks of COPD etiology.9 Studies have shown that workers in industries such as mining, construction, and agriculture who are exposed to high amounts of particulate matter, dust, and fumes are at a higher risk of getting COPD.9,27,28 Additionally, exposure to chemicals such as nitrogen oxides and sulfur dioxide can cause COPD in employees in particular sectors such as petrochemical and steel manufacture.29 These findings imply that occupational exposure to particulate matter, gases, and fumes can have long-term consequences on lung health and contribute to the development of COPD. Besides, according to Plaat et al, occupational exposures may induce differential methylation of gene expression regulating genes and thereby may induce other adverse health effects.30 A study found that smoking and occupational exposure together yielded an additive effect on incidence of COPD.31 Similarly, a study from Swiss worker found that long-term exposure to occupational exposures to biological dusts, mineral dusts, gases/fumes, and VGDF at high levels were associated with increased incidence of moderate COPD in a population of Swiss working adults.7 COPD is already an underdiagnosed condition, and occupational COPD is less common than would be predicted.9 The reasons for occupational COPD underdiagnosis are several. General practitioners frequently believe that occupational medicine training is insufficient,32 some patients who are still working may fail to report a specific job exposure.33 To solve this problem, employers must offer a safe working environment and safeguard their employees from hazardous chemicals. Ventilation systems, personal protection equipment (eg, masks), and regular air quality monitoring are examples of such measures. Besides, workers should also be appropriately taught to wear protective equipment and understand the dangers involved with their employment.34 Workers must report any COPD symptoms to their doctor. Even though self-reported exposure to VGDF may have overestimated the risk of occupational COPD.35
The present research found that the deaths number increased from 1990 to 2019, while the ASMR and ASDR showed a declined. The cause can be due to several factors, including: Rise in population: Even if the ASMR and ASDR is decreasing, an increase in the total population size might contribute to an increase in the number of COPD fatalities. Improved diagnosis and treatment: Even if the number of fatalities from COPD is growing as individuals live longer with the illness, improved diagnosis and treatment can lead to a decrease in the ASMR and ASDR. Changes in risk factors: Changes in the distribution of COPD risk variables such as age, gender, and smoking status can also have an impact on the number of fatalities, ASMR, and ASDR. Improved data collection: Improved data collection methods and increasing knowledge of COPD can also contribute to a rise in the number of fatalities ascribed to occupational particulate matter, gases, and fumes, while the ASMR and ASDR decreases as healthcare improves.
At the regional level, this study observed a non-linear-shaped relationship between SDI with the ASDR of COPD attributable to occupational particulate matter, gases, and fumes. A positive association was observed between SDI and the DALY rates at SDI levels lower than 0.4. South Asia and Oceania are the regions where SDI is lower than 0.4 in a certain period of time, and their burden is higher than expected. SDI is a composite measure of income per capita, years of education, and total fertility rate. This could be due to the fact that South Asia and Oceania likely stems from the poor working conditions, lack of awareness, and underdeveloped healthcare systems prevalent in these regions during that time period.
This research also found that the ASMR and ASDR of COPD attributable to occupational particulate matter, gases, and fumes rose with age in both sexes and was greatest in persons over the age of 80. COPD can have a long latency period, meaning it may take years or even decades for the disease to develop after exposure to pollutants.36 The length of time particulate matter, gases, and fumes exposure leads to COPD can vary, depending on various factors such as frequency, duration, and level of exposure, as well as individual factors such as genetics and overall health. The specific reason remains to be further studied.
A recent study found that low- and middle-income countries shoulder 62.6% of the world’s COPD and lung cancer burden, which is projected to escalate in the coming decades due to aging populations and inadequate control of tobacco and air pollution.3 Therefore, policymakers can adopt a multifaceted approach to preventing COPD attributable to occupational particulate matter, gases, and fumes, including legislation, supporting safe work practices, stimulating research, increasing awareness, and offering assistance to affected persons. It is critical to safeguard employees by enacting laws that define limits for permissible amounts of occupational particulate matter, gases, and fumes exposure in the workplace and provide consequences for noncompliance. Fundamentally, increase funding for research into the causes and effects of occupational particulate matter, gases, and fumes exposure and COPD, as well as ways to prevent it, is necessary to address this issue effectively. Raising public awareness about the dangers of occupational particulate matter, gases, and fumes exposure and the importance of protecting workers is crucial. Finally, providing support, treatment, and compensation for individuals affected by COPD related to occupational particulate matter, gases, and fumes exposure is necessary to address the impact of this disease on those who are affected. COPD is a preventable and treatable chronic lung disease.2 Individuals with COPD must collaborate with their healthcare physician to design a treatment plan that is appropriate for them. To avoid future loss in lung function and to lessen the health and socioeconomic burden of COPD, early diagnosis and identification of occupational causes is critical.9
There were some limitations to our study. First, GBD 2019 uses modeling tools to achieve data for locations and years that cannot be obtained, and there is a possibility of deviation. Second, GBD 2019 was generated using the DisMod-MR method after summarizing and cleaning the collected data, specific statistics on mortality and DALY trends from 1990 to 2019 were lacking. Third, there are also limits to COPD registries, particularly in less developed countries, which may contribute to under reporting. Fourth, the statistics on COPD caused by occupational particulate matter, gases, and fumes were based on self-reports, which may contain inconsistencies and biases.
Conclusion
From 1990 to 2019, the number of deaths due to COPD caused by occupational particulate matter, gases, and fumes increased, while the ASMR and ASDR showed a declining trend globally. The focus should be on employees who are exposed to particulate matter, gases, and fumes for extended periods, providing them with protection and guidance. To prevent COPD caused by occupational particulate matter, gases, and fumes, the government should enact legislation.
Data Sharing Statement
The datasets presented in this study can be found in online database. The names of the database can be found below: https://vizhub.healthdata.org/gbd-results/.
Ethics Statement
This study was approved by the Ethics Committee of the Seventh Affiliated Hospital, Sun Yat-sen University in line with the Declaration of Helsinki.
Acknowledgments
We are grateful for the work of the GBD 2019 collaborators.
Funding
Not funded.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Ammous O, Feki W, Lotfi T, et al. Inspiratory muscle training, with or without concomitant pulmonary rehabilitation, for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2023;1(1):CD013778.
2. World Health Organization. Chronic obstructive pulmonary disease (COPD). Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
3. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
4. Li HY, Gao TY, Fang W, et al. Global, regional and national burden of chronic obstructive pulmonary disease over a 30-year period: estimates from the 1990 to 2019 Global Burden of Disease Study. Respirology. 2023;28(1):29–36. doi:10.1111/resp.14349
5. Li H, Liang H, Wei L, et al. Health inequality in the global burden of chronic obstructive pulmonary disease: findings from the Global Burden of Disease Study 2019. Int J Chron Obstruct Pulmon Dis. 2022;17:1695–1702. doi:10.2147/COPD.S369120
6. Balmes J, Becklake M, Blanc P, et al; Environmental and Occupational Health Assembly, American Thoracic Society. American thoracic society statement: occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. 2003;167(5):787–797.
7. Mehta AJ, Miedinger D, Keidel D, et al; SAPALDIA Team. Occupational exposure to dusts, gases, and fumes and incidence of chronic obstructive pulmonary disease in the Swiss Cohort Study on air pollution and lung and heart diseases in adults. Am J Respir Crit Care Med. 2012;185(12):1292–1300. doi:10.1164/rccm.201110-1917OC
8. Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765–773. doi:10.1016/S0140-6736(07)61380-4
9. Murgia N, Gambelunghe A. Occupational COPD-the most under-recognized occupational lung disease? Respirology. 2022;27(6):399–410. doi:10.1111/resp.14272
10. de Jong K, Boezen HM, Kromhout H, Vermeulen R, Postma DS, Vonk JM; LifeLines Cohort study. Pesticides and other occupational exposures are associated with airway obstruction: the LifeLines cohort study. Occup Environ Med. 2014;71(2):88–96. doi:10.1136/oemed-2013-101639
11. Torén K, Järvholm B. Effect of occupational exposure to vapors, gases, dusts, and fumes on COPD mortality risk among Swedish construction workers: a longitudinal cohort study. Chest. 2014;145(5):992–997. doi:10.1378/chest.13-1429
12. Kirkeskov L, Hanskov DJ, Brauer C. Total and respirable dust exposures among carpenters and demolition workers during indoor work in Denmark. J Occup Med Toxicol. 2016;11:45. doi:10.1186/s12995-016-0134-5
13. Borup H, Kirkeskov L, Hanskov DJA, Brauer C. Systematic review: chronic obstructive pulmonary disease and construction workers. Occup Med. 2017;67(3):199–204. doi:10.1093/occmed/kqx007
14. Feizi H, Alizadeh M, Nejadghaderi SA, et al. The burden of chronic obstructive pulmonary disease and its attributable risk factors in the Middle East and North Africa region, 1990–2019. Respir Res. 2022;23(1):319. doi:10.1186/s12931-022-02242-z
15. Zou J, Sun T, Song X, et al. Distributions and trends of the global burden of COPD attributable to risk factors by SDI, age, and sex from 1990 to 2019: a systematic analysis of GBD 2019 data. Respir Res. 2022;23(1):90. doi:10.1186/s12931-022-02011-y
16. Safiri S, Carson-Chahhoud K, Noori M, et al. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990–2019: results from the Global Burden of Disease Study 2019. BMJ. 2022;378:e069679. doi:10.1136/bmj-2021-069679
17. The lancet. Global burden of disease. Available from: https://www.thelancet.com/gbd.
18. IHME. About GBD. Available from: https://www.healthdata.org/gbd/about.
19. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi:10.1016/S0140-6736(20)30752-2
20. Safiri S, Nejadghaderi SA, Abdollahi M, et al. Global, regional, and national burden of cancers attributable to tobacco smoking in 204 countries and territories, 1990–2019. Cancer Med. 2022;11(13):2662–2678. doi:10.1002/cam4.4647
21. Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: global Burden of Disease Study. Lancet. 1997;349(9063):1436–1442. doi:10.1016/S0140-6736(96)07495-8
22. Murray CJ, Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S. Comparative quantification of health risks conceptual framework and methodological issues. Popul Health Metr. 2003;1(1):1. doi:10.1186/1478-7954-1-1
23. Li H, Guo J, Liang H, et al. The burden of trachea, bronchus, and lung cancer attributable to occupational exposure from 1990 to 2019. Front Public Health. 2022;10:928937. doi:10.3389/fpubh.2022.928937
24. National Health Service (NHS). Treatment: chronic obstructive pulmonary disease (COPD). Available from: https://www.nhs.uk/conditions/chronic-obstructive-pulmonary-disease-copd/treatment/.
25. Centers for Disease Control and Prevention (CDC). Basics about COPD. Available from: https://www.cdc.gov/copd/basics-about.html.
26. The Global Initiative for Chronic Obstructive Lung Disease. 2022 GOLD REPORTS: 2022 global strategy for prevention, diagnosis and management of COPD. Available from: https://goldcopd.org/2022-gold-reports/.
27. Peng C, Yan Y, Li Z, Jiang Y, Cai Y. Chronic obstructive pulmonary disease caused by inhalation of dust: a meta-analysis. Medicine. 2020;99(34):e21908. doi:10.1097/MD.0000000000021908
28. Vanka KS, Shukla S, Gomez HM, et al. Understanding the pathogenesis of occupational coal and silica dust-associated lung disease. Eur Respir Rev. 2022;31(165):210250. doi:10.1183/16000617.0250-2021
29. Henneberger PK, Lax MB, Bg F
30. van der Plaat DA, Vonk JM, Terzikhan N, et al. Occupational exposure to gases/fumes and mineral dust affect DNA methylation levels of genes regulating expression. Hum Mol Genet. 2019;28(15):2477–2485. doi:10.1093/hmg/ddz067
31. Pallasaho P, Kainu A, Sovijärvi A, Lindqvist A, Piirilä PL. Combined effect of smoking and occupational exposure to dusts, gases or fumes on the incidence of COPD. COPD. 2014;11(1):88–95. doi:10.3109/15412555.2013.830095
32. Gök AS, Yilmaz TE, Kasim İ, Şencan İ, Özkara A. Occupational health and disease knowledge and practices of family physicians. J Occup Environ Med. 2020;62(11):e625–e629. doi:10.1097/JOM.0000000000002010
33. Lamprecht B, Soriano JB, Studnicka M, et al; BOLD Collaborative Research Group, the EPI-SCAN Team, the PLATINO Team, and the PREPOCOL Study Group. Determinants of underdiagnosis of COPD in national and international surveys. Chest. 2015;148(4):971–985. doi:10.1378/chest.14-2535
34. Fishwick D, Sen D, Barber C, Bradshaw L, Robinson E, Sumner J; COPD Standard Collaboration Group. Occupational chronic obstructive pulmonary disease: a standard of care. Occup Med. 2015;65(4):270–282. doi:10.1093/occmed/kqv019
35. Sadhra S, Kurmi OP, Sadhra SS, Lam KB, Ayres JG. Occupational COPD and job exposure matrices: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2017;12:725–734. doi:10.2147/COPD.S125980
36. Carder M, Darnton A, Gittins M, et al. Chest physician-reported, work-related, long-latency respiratory disease in Great Britain. Eur Respir J. 2017;50(6):1700961. doi:10.1183/13993003.00961-2017
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.