Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Gender Differences in the Relationship of Waist Circumference to Coronary Artery Lesions and One-Year Re-Admission Among Coronary Artery Disease Patients with Normal Body Mass Index
Authors Luan H, Song Y, Cao L, Wang P, Zhu D, Tian G
Received 26 July 2021
Accepted for publication 11 September 2021
Published 23 September 2021 Volume 2021:14 Pages 4097—4107
DOI https://doi.org/10.2147/DMSO.S330194
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Hui Luan,1 Yan Song,2 Lifei Cao,1 Ping Wang,1 Danjun Zhu,1 Gang Tian1
1Department of Cardiovascular Medicine, The First Affiliated Hospital of Xi’an Jiao Tong University, Xi’an, Shaanxi Province, People’s Republic of China; 2Department of Ultrasound, The First Affiliated Hospital of Xi’an Jiao Tong University, Xi’an, Shaanxi Province, People’s Republic of China
Correspondence: Gang Tian
Department of Cardiovascular Medicine, The First Affiliated Hospital of Xi’an Jiao Tong University, No. 277 Yenta West Road, Xi’an, Shaanxi Province, 710061, People’s Republic of China
Tel +86 29-85323112
Fax +86 29-85252580
Email [email protected]
Purpose: The study explored the association of waist circumference (WC) with the severity of cardiovascular diseases and hospital readmission of coronary artery disease (CAD) patients with normal body mass index (BMI).
Patients and Methods: 213 female and 431 male normal-BMI CAD patients were enrolled and assigned in three groups based on their gender-specific WC tertiles. Their cardiovascular risk factors and coronary angiography characteristics were analyzed in a cross-sectional study, and the gender-specific relationship between WC and one-year re-admission rate was prospectively explored.
Results: The cross-sectional analysis showed that for male normal-BMI CAD patients, diabetes and dyslipidemia prevalence, Apo B/A1, hs-CRP, and uric acid levels triglycerides-glucose index, the incidence of left main disease, three vessel disease, calcification lesion, total occlusive lesion, and complex lesion, as well as Gensini score was in the order of WC tertile 3 > WC tertile 2 > WC tertile 1. In addition, male normal-BMI CAD patients in the highest WC tertile were at an increased risk of severe CAD (OR=2.21), and the correlation was still statistically significant even after adjusting for potential cardiovascular risk factors (OR=1.87). For female normal-BMI CAD patients, as the WC tertiles increased, uric acid level, the prevalence of three vessel disease, diffuse lesion, and complex lesion gradually increased (P < 0.05), but no significant difference was found in the risk of severe CAD among different WC groups (all P > 0.05). Prospective analyses showed that the higher the WC tertile was, the higher the one-year re-admission rate in men, but not in women, and after adjusting for other risk factors, men with the highest WC tertile showed more than twice the risk of patients with the lowest WC tertile.
Conclusion: Male but not female, normal-BMI CAD patients with increased WC had more severe CAD and a higher risk of one-year re-admission rate.
Keywords: normal body mass index, waist circumference, coronary artery disease, severe CAD, one-year re-admission with adverse cardiovascular event
Introduction
The incidence of obesity-related coronary artery disease (CAD) increases due to the rapidly increased obese population worldwide.1 Obesity is an independent risk factor for CAD development and is associated with insulin resistance, hyperlipidemia, and hypertension to increase the risk of CAD indirectly.2,3 The increased accumulation of fat in the abdominal cavity or visceral obesity is highly correlated with the risk of poor coronary arteries.4 In patients at risk for CAD, the treatment of obesity results in an improved coronary risk profile.5
Although obesity is defined as excess body fat, clinicians and epidemiologists usually quantify adiposity or obesity based on anthropometricindexes such as body weight index (BMI) and waist circumference (WC).6,7 However, WC and BMI are not entirely identical, although positively correlated. BMI can only be used to assess general obesity, while WC can be used to assess central obesity (or abdominal obesity) and more accurately describe the distribution of body fat and better predict obesity-related health risk.8–10 Furthermore, in CAD patients, mortality has been reported to vary inversely with BMI (“obesity paradox”), while central obesity (assessed by WC) is directly associated with mortality.11,12
Some individuals with a normal BMI can still have abdominal obesity or a large WC.13 The prevalence of central obesity (defined by WC) in people with normal BMI has increased in China in recent years.14,15 Some epidemiologic shreds of evidence indicate an independent relationship between WC level and mortality of cardiovascular (CV) diseases in both normal-BMI healthy individuals and CAD patients.16,17 However, the possible correlations in normal-BMI patients between WC levels and the extent, severity, and complexity of CAD have not been adequately studied. The early risk stratification and management of CAD patients are crucial for improving their prognosis. The severity of coronary artery lesions is an important index for risk stratification of CAD patients and directly determines the optimal treatment strategy. In addition, due to differences in adipose tissue distribution, the association between WC and coronary artery lesions may vary by gender.18 Therefore, in this study, we aimed to examine the association of WC with coronary artery lesions and one-year re-admission in normal-BMI CAD patients in men and women.
Methods
Study Subjects
Patients who were newly diagnosed with CAD by coronary angiography from January 2017 to January 2019 at the First Affiliated Hospital of Xi’an Jiao Tong University were prospectively enrolled if they had normal BMI (18.5–23.9 kg/m2) during hospitalization.19 The exclusion criteria were pregnancy, recent trauma, cancer, cardiomyopathy, rheumatic heart disease, severe heart failure, chronic lung disease, hepatic or renal disease, immune disease, chronic gastrointestinal disease, chronic pancreatitis, a history of myocardial infarction and stroke, and a history of any malignant diseases. All patients have signed written informed consent agreeing to the coronary angiography. The study protocol was approved by the Ethical Committee of the First Affiliated Hospital of Xi’an Jiao Tong University and conducted in line with the Declaration of Helsinki.
Grouping
Patients were divided by sex-specific tertiles of WC: tertile 1 (< 87.0 cm in men and < 81.0 cm in women); tertile 2 (87.0-92.9 cm in men and 81.0–86.9 cm in women); and tertile 3 (> 92.9 cm in men and > 86.9 cm in women).
Anthropometric Measurements
Anthropometric measurements were performed by previously trained personnel strictly following the protocol. Weight was measured to the nearest 0.01 kg in light clothing by using a calibrated beam scale, and height was measured to the nearest 0.1 cm without shoes by using a fixed stadiometer. Waist and hip circumference were measured by a non-elastic tape positioned at the midpoint between the lowest rib and the iliac crest in a horizontal plane and at the greatest circumference of the buttocks. The measurement was made with minimal respiration to the nearest 0.1 cm, with the tape snug but not compressing the skin. BMI was calculated as weight in kilograms divided by squared height in meters (kg/m2) and the waist-to-hip ratio was defined as the result of the waist circumference divided by the hip circumference.
Patient Characteristics and Biochemical Measurements
Patients’ standard medical records were used to extract patients’ baseline characteristics and clinical data, including age, gender, history of diabetes, history of hypertension, family history of CAD, smoking status, and menopause status.
Venous blood samples were taken on the second day of hospitalization after a 12-h overnight fast and used for baseline laboratory examinations, including high-density lipoprotein (HDL), and low-density lipoprotein (LDL), triglycerides, total cholesterol, apolipoprotein A1, apolipoprotein B, fasting glucose, HbA1c, uric acid, and high-sensitivity C-reactive protein (hs-CRP).
Insulin resistance marker triglycerides-glucose index (TyG index) was calculated as ln(fasting TGs [mg/dL] × fasting glucose [mg/dL]/2).20
Definition of Cardiovascular Risk Factors
Patients who were currently taking lipid medications, previously diagnosed with hypercholesterolemia, and/or had HDL-cholesterol <1.04 mmol/L (40 mg/dL) in men and <1.30 mmol/L (50 mg/dL) in women, and/or triglycerides ≥1.7 mmol/L (150 mg/dL), and/or LDL-cholesterol ≥4.10 mmol/L (160 mg/dL) were considered to have dyslipidaemia. Patients taking antihypertensive medications, previously diagnosed with hypertension or having systolic pressure ≥140 mmHg or diastolic pressure ≥90 mmHg were considered hypertensive. Patients who were taking anti-diabetic medications (insulin and oral medications), were previously diagnosed with diabetes, and/or had fasting morning plasma glucose ≥7.0 mmol/L (126 mg/dL) or HbA1c ≥ 6.5% were considered to have diabetes. Patients were considered as never or ever smokers based on their answers to the question that “have you ever smoked more than 100 cigarettes in your life?”
Coronary Angiography
CAD was diagnosed based on the presence of at least 50% coronary stenosis in at least one major coronary artery according to the CAG results assessed by at least two experienced interventional cardiologists. In this study, the main culprit coronary artery, the number of diseased vessels, lesion morphology, and Gensini score were used to assess angiographic severity.
The diseased vessels were coded as 1, 2, or 3 based on the number of major coronary arteries with luminal diameter stenosis ≥ 50%. Lesions were categorized into Type A, Type B, or Type C based on the determination of a joint American College of Cardiology/American Heart Association (ACC/AHA) task force. Among them, Type A lesion was defined as simple, and Types B and C lesions were defined as complex.21 The Gensini score was assigned with consideration of the degree of luminal narrowing and the importance of the site of coronary stenosis, as previously described.22
Length of Stay (LOS), Treatment, and Follow Up
LOS refers to the time, expressed in days, from admission to discharge from hospital for an inpatient episode of care.23 Drug usage and dosage for patients with dyslipidemia, hypertension, and diabetes, and the treatment schemes for patients after discharge were based on the current practice guidelines. Patients were systematically followed up for one year to assess one-year re-admission with adverse cardiovascular events and inquired whether they were compliant with the prescribed drug regimen.
Definition of Severe CAD and One-Year Re-Admission with Adverse Cardiovascular Events
The severe CAD was defined as the top Gensini score tertile in men and women. One-year re-admission with adverse cardiovascular events was defined as re-admission within one year after discharge due to adverse cardiovascular events, including cardiac death, myocardial infarction, unstable angina pectoris, malignant arrhythmia, cardiac arrest, cardiogenic shock, cardiogenic syncope, coronary revascularization, and stroke, which were ascertained by reviewing the medical records and confirmed by directly talking to the patients, their families, and physicians following discharge. Only the first re-hospitalization was considered if the patient was re-admitted to the hospital more than once within one year after discharge.
Statistical Analysis
Shapiro–Wilk normality test was used to analyze the distribution normality of continuous variables. Continuous variables with normal distribution and abnormal distribution were expressed as the mean ± standard deviation and as the medians (interquartile ranges), respectively. Categorical variables were expressed as frequencies and percentages. Significant differences among the groups with normal distribution and abnormal distribution were determined using one-way analysis of variance and Mann–Whitney U and Kruskal–Wallis H-tests, respectively. Statistical significance of categorical variables between two groups was compared using Chi-square tests and Fisher’s exact tests. Association of WC with the prevalence of severe CAD was assessed using univariate and multivariate logistic regression analyses. The rate of one-year re-admission with adverse cardiovascular events was assessed using Kaplan–Meier analysis. Association of WC with one-year re-admission with adverse cardiovascular events was estimated using Cox proportional hazard regression model. Variables that were considered potential confounders and/or predictors of events based on univariable analysis, clinical judgment and data from the scientific literature were selected for multivariate analysis. All analyses were performed using the SPSS software program version 23.0. Two-sided P values < 0.05 were considered statistically significant.
Results
Anthropometric Indicators and Cardiovascular Risk Factors According to Waist Circumference
The study included 431 (66.9%) men and 213 (33.1%) women at the mean age of 61.7 ± 9.13 years in the range from 28 to 83 years. Baseline characteristics, angiographic characteristics of male and female subjects are shown in Table 1. Length of stay, medications at discharge, and patient compliance of male and female subjects are shown in Table S1.
 |
Table 1 Baseline Characteristics and Angiographic Characteristics in Male and Female Subjects |
They were classified based on WC into three sex-specific tertiles: tertile 1 (<87.0 cm in men and <81.0 cm in women), tertile 2 (87.0-92.9 cm in men and 81.0–86.9 cm in women), and tertile 3 (> 92.9 cm in men and > 86.9 cm in women).
According to WC tertiles, anthropometric indicators and cardiovascular risk factors of men and women are summarized in Table 2. With the increase in WC tertile, all anthropometric indicators (weight, height, BMI, WC, hip circumference, and waist-to-hip ratio) for men and women increased significantly (all P <0.05). In male normal-BMI CAD patients, differences in the prevalence of diabetes and dyslipidemia, the levels of Apo B/A1, hs-CRP, and uric acid, and triglycerides-glucose index among different WC groups were significant and increased with WC tertile increasing (P <0.05), but the differences in age, family cardiovascular disease history, smoking history and the prevalence of hypertension were not significant and varied without a trend. In female normal-BMI CAD patients, only uric acid levels increased with WC tertile (P <0.05), and other indicators varied without a trend.
 |
Table 2 Anthropometric and Cardiovascular Risk Factors in Male and Female Subjects with a Normal Body Mass Index by Waist Circumference Tertiles |
Angiographic Characteristics According to Waist Circumference
We assessed angiographic severity by the main culprit coronary artery, the number of diseased vessels, lesion morphology, and Gensini score. The angiographic characteristics of men and women are shown in Table 3.
 |
Table 3 Angiographic Characteristics in Male and Female Subjects with a Normal Body Mass Index by Waist Circumference Tertiles |
In male normal-BMI CAD patients, as WC tertile increased, the prevalence of left main disease, three-vessel disease, and complex lesion gradually increased (P <0.05). The difference in Gensini score among the three WC groups was statistically significant, and as the WC tertile increased, the Gensini score gradually increased [39(18–57) vs. 45(20–71) vs. 48(20–104), P < 0.05]. For the morphology of coronary artery lesions, as the WC tertile increased, except for diffuse lesion, the prevalence of calcification lesion and total occlusive lesion showed a gradually increasing trend (P <0.05).
In female normal-BMI CAD patients, as the WC tertile increased, the prevalence of three-vessel disease and complex lesion gradually increased (P <0.05), while the prevalence of left main disease did not change (P >0.05). The differences in Gensini scores among the three WC groups were not statistically significant [32(9–55) vs. 27(8–51) vs. 27(6–54), P=0.897]. For the morphology of coronary artery lesions, as the WC tertile increased, the prevalence of diffuse lesion showed a gradually increasing trend (P <0.05), while the prevalence of calcification lesion and total occlusive lesion showed no such trend (P >0.05).
Severe CAD According to Waist Circumference
The severe CAD was defined as the top Gensini score tertile in men and women. Table 4 shows the results of univariable and multivariable logistic regression analyses for the risk of severe CAD by WC tertiles. Among male normal-BMI CAD patients, the risk of severe CAD in the highest WC tertile group was 2.21 times of that in the lowest WC tertile group (OR: 2.21, 95% CI: 1.36–3.59). After further adjusting for age, family cardiovascular disease history, diabetes, hypertension, dyslipidemia, smoking status, Apo B/A1, hs-CRP, uric acid, and triglycerides-glucose index, the risk of severe CAD for patients with the highest WC tertile was 1.87 times of that for patients with the lowest WC tertile (OR: 1.87, 95% CI: 1.09–3.20). Among female normal-BMI CAD patients, with the lowest WC tertile as a reference, the risk of severe CAD was not significantly different between patients with the middle and the highest WC tertiles. Further adjusting for age, family cardiovascular disease history, diabetes, hypertension, dyslipidemia, Apo B/A1, hs-CRP, uric acid, and triglycerides-glucose index showed no statistical difference in risk of severe CAD among women with different WC tertiles.
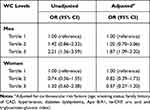 |
Table 4 Severe CAD in Male and Female Subjects with a Normal Body Mass Index by Waist Circumference Tertiles |
Analysis of One-Year Re-Admission with Adverse Cardiovascular Events After Discharge
The results of the Kaplan-Meier analysis are shown in Figure 1A and B. The cumulative incidence of one-year re-admission with adverse cardiovascular events was higher in men with the highest WC tertile than in men with the middle and lowest WC tertiles (9.3% vs. 14.7% vs. 21.6%, Breslow test P = 0.0068), but no significant difference was observed among women with different WC tertiles (Breslow test P = 0.7534).
Table 5 shows the results of univariable and multivariable Cox regression analyses for the risk of one-year re-admission with adverse cardiovascular events in men and women by WC tertiles. Among male normal-BMI CAD patients, without considering adjustment factors, the risk of one-year re-admission with adverse cardiovascular events for patients with the highest WC tertile was 2.54 times of that for patients with the lowest WC tertile (HR 2.54, 95% CI 1.33–4.83). After adjustment for age, smoking status, family history of CAD, hypertension, diabetes dyslipidemia, Apo B/A1, hs-CRP, uric acid, and triglycerides-glucose index (Model 1), the risk of one-year re-admission with adverse cardiovascular events for patients with the highest WC tertile was 2.13 times of that for patients with the lowest WC tertile (HR 2.13, 95% CI 1.06–4.27). After further adjustment for menopause status, length of stay, and patient compliance (Model 2), the risk of one-year re-admission with adverse cardiovascular events slightly increased (HR 2.16, 95% CI 1.08–4.31). Further adjustment for BMI showed that the risk of one-year re-admission with adverse cardiovascular events for patients with the highest WC tertile was 2.33 times of that for patients with the lowest WC tertile (HR 2.33, 95% CI 1.04–5.21). Compared to male patients, with or without adjustment, no significant difference in one-year re-admission with adverse cardiovascular events was observed among female normal-BMI CAD patients.
 |
Table 5 One-Year Re-Admission with Adverse Cardiovascular Events After Discharge in Male and Female Subjects with a Normal Body Mass Index by Waist Circumference Tertiles |
Discussion
Our results showed that the relationship of WC to coronary artery injury and one-year re-admission varies by gender in the normal-BMI CAD patients whose overweight problem is easy to be ignored. Among normal-BMI CAD patients, men with higher WC often have more severe CAD and a higher one-year re-admission rate than men with lower WC, but this relationship does not exist in women.
Some normal-BMI people have increased WC in the population.24 However, the obesity problem of these populations is easy to be ignored. Song et al reported that the prevalence of central obesity among ordinary Chinese adults with normal weight increased from 6.65% to 13.24% from 1993 to 2011.15 A study of 9,447 people in Jilin Province, China, reported that 55.6% of the normal-BMI population did not recognize their obesity, and only 12.7% tried to lose weight.25 In our study, the proportion of abdominal obesity men and women was 45.5% (n = 196 /431) and 42.7% (n = 91/213), respectively, based on the criteria of WC ≥ 90 cm for men and WC ≥ 85 cm for women, the proposed cut-off for the diagnosis of abdominal obesity in China.19 The proportion of normal-BMI CAD patients with abnormal WC in this study was significantly higher than that of the general population. The possible reason is that obesity is associated with higher cardiovascular disease risk factors and higher cardiovascular disease prevalence.26 Normal-BMI people with higher WC are more likely to develop CAD. The obesity guidelines did not make reliable recommendations on the WC cut-off for normal-BMI CAD patients.27 To better clarify the relationship between WC and CAD, we analyzed the CAD risk based on the gender-specific WC tertiles rather than the cut-off value of abdominal obesity.
Sun et al reported that among normal-BMI women, the all-cause death risk was 30% higher in people with central obesity than without central obesity.28 Sharma et al analyzed 7057 CAD patients from 5 cohort studies and found that normal BMI but higher WC or waist-to-hip ratio increased the risk of mortality for CAD patients.17 Previous studies have paid more attention to the relationship between WC and cardiovascular death and all-cause death in CAD patients with normal BMI or involved only women or men; very few have compared the risks between different genders. Our study was conducted in male and female normal-BMI CAD patients, focusing on the status of coronary artery lesions. The coronary angiographic characteristics of CAD patients with different WC were evaluated from the aspects of location, number, and morphologic characteristics. We also utilized Gensini scoring method, which not only considers the degree of coronary artery stenosis degree, location, and number, but also the weight of the coronary blood supply area and the scope of the disease, to assess the degree of CAD objectively and accurately and further analyze the risk of severe CAD. In general, in male but not female, normal-BMI CAD patients, as the WC increases, CAD becomes more severe, and the risk of severe CAD is higher. Specifically, in male normal-BMI CAD patients, as the WC tertile increases, the prevalence of left main disease, three-vessel disease, calcification lesion, total occlusive lesion, complex lesion, and Gensini score gradually increase. By contrast, among female normal-BMI CAD patients, as the WC tertile increases, the prevalence of three-vessel disease, diffuse lesion, and complex lesion gradually increases, while the prevalence of left main disease, calcified lesion, total occlusive lesion, and Gensini score showed no such trend. The higher Gensini score in male normal-BMI CAD patients with higher WC is probably due to the higher prevalence of left main disease and the higher prevalence of total occlusion lesion, which have the highest weight and highest score, respectively, in calculating Gensini score.22
One possible explanation for this gender difference is the difference in risk factors for cardiovascular diseases. In this study, male normal-BMI CAD patients with higher WC had chronic low-grade inflammation, glucose, and lipid metabolism disorders, and increased uric acid levels, while female normal-BMI CAD patients with higher WC only had increased uric acid levels. However, when we adjusted the underlying cardiovascular risk factors, the association weakens, but the difference still exists. Therefore, we speculate that it may also relate to other mechanisms, such as different abdominal fat distribution. WC is a better indicator of abdominal fat accumulation than BMI.29 Abdominal fat can be divided into abdominal subcutaneous fat and abdominal visceral fat.30 However, the measurement of WC alone cannot distinguish subcutaneous and visceral obesity. Men are prone to storing visceral fat, while women are likely to develop subcutaneous fat.31 Men with higher WC may have more visceral fat than women. Compared with subcutaneous fat, visceral fat is more related to insulin resistance, dyslipidemia, and vascular endothelium inflammation, which are all risk factors for cardiovascular and cerebrovascular diseases.32 A study showed that the ratio of visceral fat to subcutaneous fat measured by CT is higher in men than in women.33 Therefore, using more accurate methods to detect central obesity, such as hydrostatic pressure, dual-energy X-ray absorption, computed tomography, and magnetic resonance imaging, is very important to explore further the underlying mechanisms of gender differences in cardiovascular risk factors. It is also possible that components produced in adipose tissue, such as adipokines, play a role in the pathophysiology of coronary atherosclerosis.34 Further research is needed to confirm the gender-specific association between increased WC and CAD so that interventions can be targeted to appropriate populations. Studies on adipokines and other biomarkers may further reveal the underlying pathogenesis.
Our study has several potential limitations. First, WC criteria for the diagnosis of abdominal obesity do not apply uniformly to all populations and ethnic groups. There is also no consensus on an optimal site for the measurement of WC. We believe that the use of WC tertiles to classify those with a relatively high WC is more valid than using an arbitrary cut-off that is not previously validated. Second, WC was assessed on the first day of hospitalization; subjects could have had changes in their body composition during the follow-up period, while the extent of adiposity and/or loss of muscle mass may be an evolving process with the progression of the disease. However, this concern is genuine for most epidemiologic studies that only use baseline information on the exposure variable, including those evaluating BMI. Third, we did not have direct adiposity quantification or distribution measures, such as dual-energy x-ray absorptiometry or computed tomography. Nevertheless, WC can be measured easily and inexpensively. Fourth, we also did not have data on cytokines or adipokines, which would help us understand the pathophysiology behind our observations. Residual measured or unmeasured confounding variables may have influenced some or all the findings. Finally, this was a single-center study with a short follow-up time. Hence, future longitudinal studies in a large-scale population are necessary.
Conclusions
In short, male normal-BMI CAD patients with higher WC had higher risks of severe CAD, severe cardiovascular diseases, and one-year re-admission rate, but not women. When managing CAD patients, it is very important to pay more attention to “invisible obesity” and understand the potential gender-related differences.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author (e-mail: [email protected]) upon reasonable request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Nature Science Foundation of China (Grant Nos. 81873513, 81600574, and 30871042), Key Projects of Shaanxi Science and Technology Research and Development Plan (Grant No. 2018ZDXM-SF-049), Key Project of Clinical Research in the First Affiliated Hospital of Xi’an Jiao tong University (Grant No. XJTU1AF-CRF-2018-005) and Shaanxi Science and Technology Research and Development Plan of International Science and Technology (Grant No. 2012 kw-40-01 and 2014 JM2-8145).
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
References
1. Bastien M, Poirier P, Lemieux I, Després J-P. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56(4):369–4107. doi:10.1016/j.pcad.2013.10.016
2. De Schutter A, Lavie CJ, Milani RV. The impact of obesity on risk factors and prevalence and prognosis of coronary heart disease-The obesity paradox. Prog Cardiovasc Dis. 2014;56:401–408.
3. Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53:1925–1932.
4. Reis JP, Macera CA, Araneta MR, et al. Comparison of overall obesity and body fat distribution in predicting risk of mortality. Obesity. 2009;17:1232–1239.
5. Brochu M, Poehlman ET, Ades PA. Obesity, body fat distribution, and coronary artery disease. J Cardiopulm Rehabil. 2000;20:96–108.
6. WHO. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452.
7. Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10.
8. Kim SH, Després JP, Koh KK. Obesity and cardiovascular disease: friend or foe? Eur Heart J. 2016;37:3560–3568.
9. Pischon T, Boeing H, Hoffmann K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359:2105–2120.
10. Poirier P. Adiposity and cardiovascular disease: are we using the right definition of obesity? Eur Heart J. 2007;28(17):2047–2048. doi:10.1093/eurheartj/ehm321
11. Angerås O, Albertsson P, Karason K, et al. Evidence for obesity paradox in patients with acute coronary syndromes: a report from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J. 2013;34:345–353.
12. McAuley PA, Artero EG, Sui X, et al. The obesity paradox, cardiorespiratory fitness, and coronary heart disease. Mayo Clin Proc. 2012;87:443–451.
13. Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality. Eur Heart J. 2010;31:737–746.
14. Du T, Sun X, Yin P, et al. Increasing trends in central obesity among Chinese adults with normal body mass index, 1993-2009. BMC Public Health. 2013;13:327.
15. Song P, Li X, Bu Y, et al. Temporal trends in normal weight central obesity and its associations with cardiometabolic risk among Chinese adults. Sci Rep. 2019;9:5411.
16. Sahakyan KR, Somers VK, Rodriguez-Escudero JP, et al. Normal-weight central obesity: implications for total and cardiovascular mortality. Ann Intern Med. 2015;163:827–835.
17. Sharma S, Batsis JA, Coutinho T, et al. Normal-weight central obesity and mortality risk in older adults with coronary artery disease. Mayo Clin Proc. 2016;91:343–351.
18. Poorthuis MHF, Sherliker P, de Borst GJ, et al. Joint associations between body mass index and waist circumference with atrial fibrillation in men and women. J Am Heart Assoc. 2021;10:e019025.
19. Health and Family Planning Commission of the People’s Republic of China. WS/T 428-2013. Health Industry Standards of the People’s Republic of China: Adult Weight Determination. Beijing, China: China Standards Publishing House; 2013.
20. Alizargar J, Bai CH, Hsieh NC, Wu SV. Use of the triglyceride-glucose index (TyG) in cardiovascular disease patients. Cardiovasc Diabetol. 2020;19:8.
21. Cannon CP, Battler A, Brindis RG, et al. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee). J Am Coll Cardiol. 2001;38:2114–2130.
22. Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606.
23. Chin CT, Weintraub WS, Dai D, et al. Trends and predictors of length of stay after primary percutaneous coronary intervention: a report from the CathPCI registry. Am Heart J. 2011;162:1052–1061.
24. Oliveros E, Somers VK, Sochor O, Goel K, Lopez-Jimenez F. The concept of normal weight obesity. Prog Cardiovasc Dis. 2014;56:426–433.
25. Zhang P, Wang R, Gao C, et al. Prevalence of central obesity among adults with normal BMI and Its association with metabolic diseases in Northeast China. PLoS One. 2016;11:e0160402.
26. Piché ME, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity and body fat distribution to cardiovascular disease: an update. Prog Cardiovasc Dis. 2018;61:103–113.
27. Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16:177–189.
28. Sun Y, Liu B, Snetselaar LG, et al. Association of normal-weight central obesity with all-cause and cause-specific mortality among postmenopausal women. JAMA Netw Open. 2019;2:e197337.
29. Klein S, Allison DB, Heymsfield SB, et al. Waist circumference and cardiometabolic risk: a Consensus Statement from Shaping America’s Health: association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Obesity. 2007;15:1061–1067.
30. Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr. 2002;75:683–688.
31. Tchernof A, Després JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93:359–404.
32. Koenen M, Hill MA, Cohen P, Sowers JR. Obesity, adipose tissue and vascular dysfunction. Circ Res. 2021;128:951–968.
33. Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 2020;8:616–627.
34. Weschenfelder C, Schaan de Quadros A, Lorenzon Dos Santos J, Bueno Garofallo S, Marcadenti A. Adipokines and adipose tissue-related metabolites, nuts and cardiovascular disease. Metabolites. 2020;10:32.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

