Back to Journals » Journal of Pain Research » Volume 16
Factors Related to the Deterioration of Postoperative Lower Back Pain in Hemilaminectomy Approach for Lumbar Spinal Schwannoma Resection
Authors Gao L, Ye L, Zhang Y, Zhang K, Wang X, Cheng BC, Cheng H
Received 23 February 2023
Accepted for publication 3 August 2023
Published 17 August 2023 Volume 2023:16 Pages 2861—2869
DOI https://doi.org/10.2147/JPR.S409773
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Rushna Ali
Lu Gao, Lei Ye, Yiquan Zhang, Ke Zhang, Xianxiang Wang, Bao Chun Cheng, Hongwei Cheng
Department of Neurosurgery, First Affiliated Hospital of Anhui Medical University, Hefei, Anhui Province, People’s Republic of China
Correspondence: Hongwei Cheng; Bao Chun Cheng, Department of Neurosurgery, First Affiliated Hospital of Anhui Medical University, Jixi Road 218, Hefei, Anhui Province, 230022, People’s Republic of China, Email [email protected]; [email protected]
Objective: This study aimed to explore the related risk factors in patients who underwent hemilaminectomy for lumbar spinal schwannoma resection and who experienced deterioration of postoperative lower back pain in comparison to preoperative pain levels.
Methods: This retrospective study recruited 61 patients from the First Affiliated Hospital of An Hui Medical University between January 2018 and June 2019. All data were collected from clinical records and analyzed at 1-month and at 1-year follow-up. The visual analog scale (VAS) was used to evaluate pain, and neurologic function was assessed using the Modified McCormick Scale. Intraoperative neurophysiological monitoring was used to assess neuronal integrity and mitigate injury. Statistical analysis of the data was performed using the SPSS version 19 software.
Results: Preoperative pain improved dramatically in the 1-year follow-up (VAS: preoperative, 3.84± 2.19; 1-year follow-up, 2.13± 2.26; P< 0.001). The pain-improved group and worsened group showed a significant difference at 1-month (VAS: 1.76± 1.56; 5.54± 1.26; P< 0.05) and at 1-year (VAS: 0.83± 1.09; 4.80± 1.58; P< 0.05) follow-up. The pain-improved and worsened groups had a significant difference in tumor size and hemilaminectomy removal segments at 1-month and 1-year follow-up, but A-train occurrence on electromyography could only be seen as a statistical difference in the 1-month follow-up. Logistic regression analysis revealed that tumor size was an independent risk factor for postoperative lower back pain deterioration.
Conclusion: The hemilaminectomy approach is a safe and effective method that can dramatically relieve pain in spinal lumbar schwannoma resection. Tumor size is an independent risk factor for postoperative lower back pain. A-train on spontaneous electromyography has been shown to be a reliable predictive factor for the evaluation of postoperative lower back pain. However, further detailed analysis of A-train characteristics can provide a more accurate warning during surgery.
Keywords: lumbar spinal schwannoma, lower back pain, hemilaminectomy, electromyography, intraoperative monitoring
Introduction
Spinal schwannomas are the most common intradural extramedullary spinal tumors, which commonly occur in the cervical and lumbar regions and arise from Schwann cell progenitors.1 The incidence of spinal schwannoma is approximately 0.3–0.5/100,000 individuals annually, and the prevalence is almost similar in males and females.2,3 A majority of spinal schwannomas are benign and develop intradurally; however, they can also grow extradurally or a combination of intradural and extradural growth.4 The clinical symptoms of lumbar spinal schwannomas are usually related to their size and anatomical location. The onset of symptoms is frequently marked by pain followed by neurological function disorders.5,6
Currently, the gold standard treatment for symptomatic lumbar spinal schwannoma is gross total resection, which halts symptom progression, promotes recovery of neurological function, and decreases tumor recurrence. The unilateral hemilaminectomy approach for spinal intradural tumor resection was first introduced in 1989 and 1991 by Chiou and Yasargil.7,8 This approach has been advocated for most intradural tumors, which could potentially reduce the risk of postoperative instability and kyphosis.9 Recent data have shown beneficial clinical outcomes regarding blood loss, length of hospital stay, operative time, complications, and most importantly, postoperative instability when utilizing a hemilaminectomy approach.1,10–12
As we all know, the severity of the symptoms of lumbar spinal schwannomas mainly depends on the degree of compression of the cauda equina or nerve root. Pain is usually the first presenting symptom of intradural lumbar schwannoma.13 Pain can be characterized as lower back pain, which may be local or radiate to the legs due to the tumor invading nerve roots.14 Surgical management of patients with spinal lumbar tumors has resulted in an overall pain reduction and an improved quality of life.15 However, we frequently encountered some patients who suffered from deterioration of pain or without pain improvement in comparison to preoperative pain in the late follow-up. Only one of the published papers elucidated postoperative and delayed pain. In this article, they reported approximately 59.6% with residual pain or operative site pain after 1 year.16
Intraoperative neurophysiological monitoring (IOM) is widely used in spinal surgery. Multimodality IOM is essential to detect and evaluate spinal function, which can identify nerve roots that give rise to the tumor because the nerve fibers may have a complex relationship with the tumor mass.17,18 Complete tumor removal with functional preservation of the cauda equina or nerve roots remains the goal of surgery. Electrical stimulation to localize the nerve and evaluate its function cannot provide continuous monitoring, which may miss critical episodes during the surgical procedure. A-train was first described in 2000 for vestibular schwannoma excision. The A-train is a distinct electromyography (EMG) waveform with a sinusoidal pattern that produces high-frequency sounds from the loudspeaker. The A-train has a frequency of up to 210 Hz, whereas the amplitudes range from 100 to 200 mV and never exceed 500 mV.19 It has been demonstrated that the occurrence of A-train is a highly reliable predictor of postoperative facial palsy.20 However, the effect of the A-train has not been explored in lumbar spinal schwannoma resection.
Postoperative deterioration of lower back pain in lumbar spinal schwannomas is easy to ignore in our clinical work. Unfavorable lower back pain is more likely to cause medical disputes and decreases a patients’ quality of life. Thus, this study aimed to investigate the deterioration of postoperative lower back pain-related risk factors and assess the predictive value of A-train for the early detection of deterioration of postoperative lower back pain in lumbar spinal schwannoma resection.
Methods
Data Source
This retrospective study recruited 61 patients who underwent hemilaminectomy for lumbar and sacral spinal schwannoma resection between January 2018 and June 2019 at the First Affiliated Hospital of An Hui Medical University. All data were collected from clinical records, and follow-up included demographic, preoperative, intraoperative, and postoperative variables. The following inclusion criteria were used: 1) the pathology of schwannoma was identified after surgery and 2) all participants had at least 1 year of clinical and radiological follow-up. The exclusion criteria were as follows: 1) severe cardiopulmonary dysfunction; 2) other central nervous system diseases that could lead to neurological deficits; 3) serious lumbar spine degenerative diseases, such as disc herniation, lumbar spondylolisthesis, spinal canal stenosis, and osteoporosis; 4) existing debilitating musculoskeletal disorders; and 5) recurrence of tumor for further surgery. To maintain the stability of the study, patients who received long-term analgesics, physiotherapy, or rehabilitation treatment for lower back pain were also excluded from the study. (Supplement 1) The study complies with the Declaration of Helsinki and the protocol was approved by the Ethics Committee of An Hui Medical University. All participants agreed to participate in this study and signed an informed consent form.
Clinical Data Collection
All patient data were obtained from clinical records and were classified based on demographic characteristics, clinical presentation, image features, intraoperative parameters, and surgical outcomes. Tumors were classified according to their location and extent of growth. The tumor location was divided into three types: ventrolateral, lateral, and lateral-dorsal. Tumor typing was as follows: localized exclusively intradural, type I; intradural localization with extradural extension to the nerve root foramina, but restricted to the spinal canal, type II; and intradural dumbbell-shaped tumor in the spinal canal extending to the extraforaminal region, type III.21 Lower back pain was assessed preoperatively, at 1-month, and at 1-year follow-up using the numerical visual analog scale (VAS) for pain and the Modified McCormick Scale for neurological function. Patients were prescribed short-acting oral analgesics with significant postoperative pain for up to one week. Our suggested pain medication for inpatient patients when requested, was Paracetamol 2000–3000mg/day. After discharge, the patients did not receive any long-term analgesics or neurorehabilitation training. Based on the postoperative lower back pain outcome compared to the preoperative outcome, we divided the patients into two groups: the improved group (group A) and the worsened group (group B).
Surgery Technique and Intraoperative Neurophysiologic Monitoring
All tumors were resected using the posterior hemilaminectomy approach. Patients were placed in a prone position under general anesthesia after application of the neuromonitoring electrodes. Intraoperative fluoroscopy was performed to confirm the surgical level. A midline skin incision was made, and the paraspinal muscles were detached from the site and retracted. Hemilaminectomy decompression segments are based on the tumor size and location. The dura matter was opened using a midline incision (midway between the edges of the hemilaminectomy) and sutured to the both sides of the surgical field to maintain sufficient exposure. The tumor was removed en bloc or piecewise. Multimodality intraoperative monitoring was conducted by two experienced neurologists. Somatosensory evoked potentials (SSEP), motor evoked potentials (MEP), and EMG were monitored continuously during surgery. We preserved the nerve root involved in the tumor when possible. Electrical stimulation was applied when the original tumor nerve was resected. The dura was closed using 6–0 resorbable sutures. All tumor specimens were sent for pathological diagnosis.
Statistical Analysis
SPSS version 19.0 was used for statistical analysis. Univariate analyses of continuous variables were performed using Student’s t-test, and categorical variables were tested using the chi-square test or Fisher’s exact test. Multivariate logistic regression models were employed, statistical difference variables of univariate analysis were included, and the stepwise method was used to analyze the risk factors related to the deterioration of lower back pain. A value of p<0.05 (two-tailed) was considered statistically significant.
Results
Pre- and Postoperative Clinical Characteristics
A total of 61 patients were included in this study, with a mean age of 53 years (range 12–78 years). In terms of sex, there were 31 (50.8%) males and 30 (49.2%) females, whose mean body mass index is 24.38 kg/m2 (range 21.35–26.34 kg/m2). Of the 61 tumors, 49 (80.3%) were in the lumbar spinal region and 12 (19.7%) were in the sacral spinal region. According to our classification of tumors mentioned in the Methods section, 42 (68.8%) were lateral, 14 (23.0%) were lateral-dorsal, and five (8.2%) were ventrolateral; 35 (57.4%) tumors were categorized as type I, 15 (24.6%) as type II, and 11 (18.0%) as type III tumors. The size of the tumor ranged from 1.24 to 4.84 cm3 (mean size, 2.93 cm3). The medical history from the onset of symptoms to diagnosis was 6 to 18 months (mean time, 11.6 months).
Symptoms at presentation included pain in 50 (82.0%) patients, motor deficits in nine (14.8%), and sensory deficits in five (8.2%). Among these, 57 (93.4%) tumors were completely removed, and only four (6.6%) tumors were sub-totally removed. The hemilaminectomy decompression levels based on tumor size and location were 21 (34.4%) in the one-segment removal, 35 (57.4%) in the two-segment removal, and five (8.2%) in the three-segment removal. The operation time ranged from 78 min to 147 min (mean time, 114.10 min). Twelve complications were observed in patients, including three (4.9%) cases of leakage of cerebrospinal fluid, four (6.6%) pulmonary infections, and five (8.2%) urinary tract infections (Table 1). At the 1-year follow-up, no patients showed tumor recurrence. Neurological deficits, as evaluated at 1-year follow up, improved completely in all nine patients who had preoperative neurological motor impairment, while two of five patients had minimal lower extremity numbness. None of the patients developed iatrogenic kyphosis or required any delayed instrumental fixation/fusion due to lumbar spinal instability at follow-up (Figure 1).
 |
Table 1 Demographic and Clinical Characteristics of Patients |
Pre- and Postoperative Pain
Pain is always the first main presenting symptom requiring patients with a lumbar spinal tumor to visit a hospital. In our study, 50 patients (82.0%) presented with lower back pain before surgery. The pain symptom aggravated in 28 patients at 1-month follow-up, and the symptom exacerbated in 20 patients at 1-year follow-up compared to the preoperative follow-up. The VAS scores were 3.84±2.19 preoperatively and exhibited no statistical difference at 1-month follow-up (3.49±2.39; P>0.05), but showed a significant difference at 1-year follow-up (2.13±2.26; P<0.001). We observed that some of the patients showed no change or experienced worsening pain compared to before surgery. According to the postoperative VAS score, patients were grouped into two: the VAS improved group (group A) and the VAS indicated no change and worsened group (group B). Preoperative VAS scores did not show any difference between the two groups at 1-month (group A, 3.48±2.20; group B: 4.25±2.15) and at 1-year (group A 3.68±2.20; group B 4.15±2.21) follow-up (P>0.05). However, we found a significant difference in postoperative VAS scores between the two groups at 1-month (group A, 1.76±1.56; group B, 5.54±1.26) and at 1-year (group A 0.83±1.09; group B 4.80±1.58) follow-up (P<0.05) (Table 2).
 |
Table 2 Pre- and Postoperative VAS Scores in Two Groups |
IOM
In our study, all patients underwent IOM. The SSEP, MEP, and EMG were recorded before patient positioning until the end of the surgical procedure. Of these patients, only six showed transient SSEP and MEP changes (four including SSEP, two including MEP 2), but no patient had a postoperative neurological deficit. A-train clusters were examined using EMG in 24 patients who underwent IOM. However, A-train clusters were identified in only half of the patients (Figure 1). The occurrence of this pattern was significantly associated with lower back pain improvement at 1-month follow-up; however, it was not significantly associated with the 1-year follow-up (Table 3).
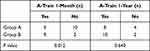 |
Table 3 A-Train Occurrence Intraoperative on IOM |
Risk Factors in Multivariate Logistic Regression
To investigate the risk factors related to postoperative pain recovery, we conducted a comparison of predictive factors in groups A and B after 1-month and 1-year of follow-ups. We observed significant differences in tumor size and length of hemilaminectomy segment removal between the two groups after 1-month and 1-year follow-up (Table 4 and Table 5). However, multivariate analysis demonstrated that tumor size was the only independent risk factor for the deterioration of postoperative lower back pain in the hemilaminectomy approach for lumbar spinal schwannoma resection (Table 6).
 |
Table 4 Factors Analysis of 1-Month Follow-Up Outcome |
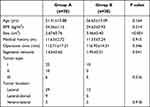 |
Table 5 Factors Analysis of 1-Year Follow-Up Outcome |
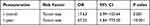 |
Table 6 Multivariate Analysis of Risk Factors for Deteriorated Postoperative Lower Back Pain |
Discussion
In this retrospective analysis conducted in 2018–2019 in our single-center database, we found that a portion of patients who underwent hemilaminectomy resection for lumbar spinal schwannoma suffered from aggravated postoperative lower back pain in comparison to preoperative pain levels. Significant factors for unfavorable outcomes included tumor size and length of hemilaminectomy resection segments; however, tumor size was predicted as an independent risk factor in the multivariate logistic analysis.
Over the past three decades, minimally invasive surgery, such as hemilaminectomy procedures for resection of intraspinal schwannomas, has been gaining popularity due to the shorter length of hospital stay, less operative blood loss, minimal tissue injury, reduction of the impact of surgical approach on spine stability, and improvement of postoperative pain and neurological function.22,23 Thus, hemilaminectomy has become one of the preferred surgical approaches for intradural spinal tumors and chronic degenerative diseases.24,25 Our surgical series on lumbar spinal schwannomas also demonstrated the safety and efficacy of the hemilaminectomy approach. Our study, which is in line with a recently reported series,24,26 showed a dramatically alleviated lower back pain and improvement in neurological function deficit at 1-year of follow-up. Based on our surgical experience, hemilaminectomy can provide sufficient visualization for tumor resection and dural closure through a narrow corridor. As far as the results of our series were demonstrated, the total tumor resection rate was high and the complication rate was low. Remarkably, none of the patients had spinal deformity, even in patients who had undergone a three-segment resection of the hemilamina.
In our cohort, the most common symptoms were local back and radiating pain. Although pain was relieved in the majority of patients after tumor removal, we observed that some patients had residual lower back pain, which worsened postoperatively after lumbar spinal schwannoma resection in our clinical work. In this study, we categorized the patients into two groups: pain-improved and worsened groups. We found no significant difference between the two groups in the preoperative VAS scores, while a significant statistical difference was detected between the two groups at 1 month and 1 year postoperatively. According to one published study, the occurrence rate of postoperative neuropathic pain ranges from 20% to 40%, depending on the type and location of the surgical approach.27 As suggested by the authors, especially in nerve sheath tumors, the loss of Schwann cell guidance resulting in random sprouting of neurons was assumed to be a possible underlying cause for the development of neuropathic pain.28 Only a few studies have addressed the incidence and cause of neuropathic pain after spinal tumor resection,29,30 while patients presenting with postoperative pain aggravation have rarely been explored and easily neglected in our daily clinical work. Neuropathic pain has been associated with a reduced ability to work and markedly impaired quality of life.31 Unfortunately, pain remained in tumor resection patients during the late follow-up, commonly requiring long-term medication interventions. Thus, it is essential to identify the significant potential risk factors that lead to postoperative deterioration of lower back pain and improve the quality of life of our patients.
IOM has been extensively used in spinal surgery to avoid intragenic injury and protect neurological function. A large prospective study conducted by Sutter et al evaluated prognostic multimodality monitoring in patients undergoing spine surgery and demonstrated a sensitivity of 89% and a specificity of 99% in the detection of postoperative neurological deficits.32 However, SSEP is limited to monitoring the dorsal columns and related pathways, providing indirect information about the integrity of the lateral corticospinal tracts.33,34 MEPs can provide direct monitoring and are highly sensitive to lateral and ventral corticospinal tract injuries; however, false-positive results are frequent.35 SSEP and MEP are not available to provide continuous monitoring of the spinal nerve tract and may miss important information during surgery. Continuous spontaneous EMG (sEMG) recording is often used to monitor spontaneous activity in lower motor neurons that might appear with nerve root manipulation. Unlike MEPs, no stimulation is necessary to record sEMG, and recordings are continuous, rather than intermittent. Spontaneous activity can be initiated by traction, pressure, ischemia, or nerve root injury. In 2000, Romstöck et al developed an A-train on free-running EMG and described its waveform characteristics, frequencies, and amplitudes, and investigated the reliability of train time as a quantitative parameter to indicate nerve paresis after surgery.20,36 Our results show that in patients with deterioration of postoperative lower back pain, high amounts of A-train occur frequently, with a significant difference between the two groups at 1 month postoperatively. The occurrence frequency of the A-train might reflect the extent of disturbance of the nerve root and would thus support a decision for incomplete tumor removal. While a large amount of A-train is exhibited on sEMG intraoperatively, the surgeon should stop manipulating the nerve and look for compression or injury to ensure that corrections can be performed before the injury becomes permanent. In this study, we investigated the occurrence of A-train on sEMG in a portion of patients, and further investigation should be performed to explore the detailed information of A-train, such as the total train time and association of train time and lower back pain, while also estimating how to avoid the occurrence of A-train, alleviate lower back pain postoperatively, and improve the quality of life.
While most published articles focus on overall morbidity and mortality and postoperative neurological function deficit,24,37 postoperative pain and related risk factors are often underestimated. The findings of this study identified predictors of adverse lower back pain after lumbar spinal schwannoma resection, which included the length of hemilamina removal and tumor size in the univariate analysis. Furthermore, we verified that tumor size was an independent risk factor for deterioration of postoperative lower back pain using multivariate logistic analysis. As demonstrated in the literature, a larger tumor size is the more likely associated with higher postoperative complications and neurological deficits.38,39 During tumor excision, especially in large tumors, many nerve fibers are involved, some running over the surface of a tumor and some penetrating the tumor mass. Thus, separation of these nerve fibers around the tumor usually gives rise to fiber traction, compression, and even injury. Our study illustrated an association between tumor size and a high rate of postoperative aggravated lower back pain. This highlights the importance of carefully dissecting tumors and separating nerve fibers to allow comprehensive surgical planning aimed at reducing postoperative lower back pain and improving neurological function. In addition, a prospective study is necessary to further validate the influence of tumor size on postoperative pain and complications.
Conclusion
In summary, the hemilaminectomy surgical approach is an effective method to excise lumbar intradural schwannomas with a high rate of pain relief and a low rate of postoperative complications. Tumor size has been validated as an independent risk factor associated with adverse postoperative lower back pain. The A-train on the sEMG cluster could be a reliable indicator in the evaluation of postoperative lower back pain and guide the intraoperative manipulation of nerve fibers. However, further detailed analysis of A-train characteristics and tumor size is essential for the management of lumbar intradural tumors and to improve the quality of life of patients in future clinical practice.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Safavi-Abbasi S, Senoglu M, Theodore N, et al. Microsurgical management of spinal schwannomas: evaluation of 128 cases. J Neurosurg Spine. 2008;9(1):40–47. doi:10.3171/SPI/2008/9/7/040
2. Zuckerman SL, Chotai S, Devin CJ, et al. Surgical resection of intradural extramedullary spinal tumors: patient reported outcomes and minimum clinically important difference. Spine. 2016;41(24):1925–1932. doi:10.1097/BRS.0000000000001653
3. Jinnai T, Koyama T, Koyama T. Clinical characteristics of spinal nerve sheath tumors: analysis of 149 cases. Neurosurgery. 2005;56(3):510–515. doi:10.1227/01.NEU.0000153752.59565.BB
4. Ozawa H, Kokubun S, Aizawa T, Hoshikawa T, Kawahara C. Spinal dumbbell tumors: an analysis of a series of 118 cases. J Neurosurg Spine. 2007;7(6):587–593. doi:10.3171/SPI-07/12/587
5. Zhai X, Zhou M, Chen H, et al. Differentiation between intraspinal schwannoma and meningioma by MR characteristics and clinic features. Radiol Med. 2019;124(6):510–521. doi:10.1007/s11547-019-00988-z
6. Nambiar M, Kavar B. Clinical presentation and outcome of patients with intradural spinal cord tumours. J Clin Neurosci. 2012;19(2):262–266. doi:10.1016/j.jocn.2011.05.021
7. Chiou SM, Eggert HR, Laborde G, Seeger W. Microsurgical unilateral approaches for spinal tumour surgery: eight years’ experience in 256 primary operated patients. Acta Neurochir. 1989;100(3–4):127–133. doi:10.1007/BF01403599
8. Keller T, Holland MC. Some notable American spine surgeons of the 19th century. Spine. 1997;22(12):1413–1417. doi:10.1097/00007632-199706150-00022
9. Goodarzi A, Clouse J, Capizzano T, Kim KD, Panchal R. The optimal surgical approach to intradural spinal tumors: laminectomy or hemilaminectomy. Cureus. 2020;12(2):e7084. doi:10.7759/cureus.7084
10. Gandhi RH, German JW. Minimally invasive approach for the treatment of intradural spinal pathology. Neurosurg Focus. 2013;35(2):E5. doi:10.3171/2013.5.FOCUS13163
11. Turel MK, D’Souza WP, Rajshekhar V. Hemilaminectomy approach for intradural extramedullary spinal tumors: an analysis of 164 patients. Neurosurg Focus. 2015;39(2):E9. doi:10.3171/2015.5.FOCUS15170
12. Raygor KP, Than KD, Chou D, Mummaneni PV. Comparison of minimally invasive transspinous and open approaches for thoracolumbar intradural-extramedullary spinal tumors. Neurosurg Focus. 2015;39(2):E12. doi:10.3171/2015.5.FOCUS15187
13. Hermann DM, Barth A, Porchet F, Hess CW, Mumenthaler M, Bassetti CL. Nocturnal positional lumboischialgia: presenting symptom of lumbar spinal tumours. J Neurol. 2008;255(11):1836–1837. doi:10.1007/s00415-008-0998-0
14. Arnautovic K, Arnautovic A. Extramedullary intradural spinal tumors: a review of modern diagnostic and treatment options and a report of a series. Bosn J Basic Med Sci. 2009;9(Suppl 1):40–45. doi:10.17305/bjbms.2009.2755
15. Pompili A, Caroli F, Crispo FG, et al. Unilateral laminectomy approach for the removal of spinal meningiomas and schwannomas: impact on pain, spinal stability and neurological results. World Neurosurg. 2016;85:282–291. doi:10.1016/j.wneu.2015.09.099
16. Tarantino R, Donnarumma P, Nigro L, Rullo M, Santoro A, Delfini R. Surgery of intradural extramedullary tumors: retrospective analysis of 107 cases. Neurosurgery. 2014;75(5):509–514. doi:10.1227/NEU.0000000000000513
17. Ghadirpour R, Nasi D, Iaccarino C, et al. Intraoperative neurophysiological monitoring for intradural extramedullary tumors: why not. Clin Neurol Neurosurg. 2015;130:140–149. doi:10.1016/j.clineuro.2015.01.007
18. Ghadirpour R, Nasi D, Iaccarino C, et al. Intraoperative neurophysiological monitoring for intradural extramedullary spinal tumors: predictive value and relevance of D-wave amplitude on surgical outcome during a 10-year experience. J Neurosurg Spine. 2018;30(2):259–267. doi:10.3171/2018.7.SPINE18278
19. Romstöck J, Strauss C, Fahlbusch R. Continuous electromyography monitoring of motor cranial nerves during cerebellopontine angle surgery. J Neurosurg. 2000;93(4):586–593. doi:10.3171/jns.2000.93.4.0586
20. Prell J, Rampp S, Romstöck J, Fahlbusch R, Strauss C. Train time as a quantitative electromyographic parameter for facial nerve function in patients undergoing surgery for vestibular schwannoma. J Neurosurg. 2007;106(5):826–832. doi:10.3171/jns.2007.106.5.826
21. Sun I, Pamir MN. Non-syndromic spinal schwannomas: a novel classification. Front Neurol. 2017;8:318. doi:10.3389/fneur.2017.00318
22. Iacoangeli M, Nasi D, Colasanti R, et al. Endoscopic endonasal odontoidectomy with anterior C1 Arch preservation in rheumatoid arthritis: long-term follow-up and further technical improvement by anterior endoscopic C1-C2 screw fixation and fusion. World Neurosurg. 2017;107:820–829. doi:10.1016/j.wneu.2017.08.063
23. Oktem IS, Akdemir H, Kurtsoy A, Koç RK, Menkü A, Tucer B. Hemilaminectomy for the removal of the spinal lesions. Spinal Cord. 2000;38(2):92–96. doi:10.1038/sj.sc.3100963
24. Dobran M, Paracino R, Nasi D, et al. Laminectomy versus unilateral hemilaminectomy for the removal of intraspinal schwannoma: experience of a single institution and review of literature. J Neurol Surg a Cent Eur Neurosurg. 2021;82(6):552–555. doi:10.1055/s-0041-1722968
25. Iacoangeli M, Gladi M, Di Rienzo A, et al. Minimally invasive surgery for benign intradural extramedullary spinal meningiomas: experience of a single institution in a cohort of elderly patients and review of the literature. Clin Interv Aging. 2012;7:557–564. doi:10.2147/CIA.S38923
26. Lee SE, Jahng TA, Kim HJ. Different surgical approaches for spinal schwannoma: a single surgeon’s experience with 49 consecutive cases. World Neurosurg. 2015;84(6):1894–1902. doi:10.1016/j.wneu.2015.08.027
27. Sughrue ME, Levine J, Barbaro NM. Pain as a symptom of peripheral nerve sheath tumors: clinical significance and future therapeutic directions. J Brachial Plex Peripher Nerve Inj. 2008;3:6.
28. Tyner TR, Parks N, Faria S, et al. Effects of collagen nerve guide on neuroma formation and neuropathic pain in a rat model. Am J Surg. 2007;193(1):e1–6. doi:10.1016/j.amjsurg.2006.08.026
29. Celli P. Treatment of relevant nerve roots involved in nerve sheath tumors: removal or preservation. Neurosurgery. 2002;51(3):684–692. doi:10.1097/00006123-200209000-00012
30. Klekamp J. Treatment of intramedullary tumors: analysis of surgical morbidity and long-term results. J Neurosurg Spine. 2013;19(1):12–26. doi:10.3171/2013.3.SPINE121063
31. Onishi-Kato Y, Nakamura M, Iwanami A, et al. Perioperative factors associated with chronic central pain after the resection of intramedullary spinal cord tumor. Clin J Pain. 2017;33(7):640–646. doi:10.1097/AJP.0000000000000438
32. Sutter M, Eggspuehler A, Muller A, Dvorak J. Multimodal intraoperative monitoring: an overview and proposal of methodology based on 1017 cases. Eur Spine J. 2007;16(Suppl 2):S153–61.
33. Kim SM, Kim SH, Seo DW, Lee KW. Intraoperative neurophysiologic monitoring: basic principles and recent update. J Korean Med Sci. 2013;28(9):1261–1269. doi:10.3346/jkms.2013.28.9.1261
34. Strike SA, Hassanzadeh H, Jain A, et al. Intraoperative neuromonitoring in pediatric and adult spine deformity surgery. Clin Spine Surg. 2017;30(9):E1174–E1181. doi:10.1097/BSD.0000000000000388
35. Acharya S, Palukuri N, Gupta P, Kohli M. Transcranial motor evoked potentials during spinal deformity corrections-safety, efficacy, limitations, and the role of a checklist. Front Surg. 2017;4:8. doi:10.3389/fsurg.2017.00008
36. Rampp S, Strauss C, Scheller C, Rachinger J, Prell J. A-trains for intraoperative monitoring in patients with recurrent vestibular schwannoma. Acta Neurochir. 2013;155(12):2273–2279. doi:10.1007/s00701-013-1891-x
37. Viereck MJ, Ghobrial GM, Beygi S, Harrop JS. Improved patient quality of life following intradural extramedullary spinal tumor resection. J Neurosurg Spine. 2016;25(5):640–645. doi:10.3171/2016.4.SPINE151149
38. Yu NH, Lee SE, Jahng TA, Chung CK. Giant invasive spinal schwannoma: its clinical features and surgical management. Neurosurgery. 2012;71(1):58–66. doi:10.1227/NEU.0b013e31824f4f96
39. Malik AT, Jain N, Scharschmidt TJ, Mayerson JL, Khan SN. Factors associated with post-operative sepsis following surgery for spinal tumors: an analysis of the ACS-NSQIP database. Clin Neurol Neurosurg. 2018;172:1–7. doi:10.1016/j.clineuro.2018.06.019
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.