Back to Journals » Journal of Pain Research » Volume 16
Eye Movement Abnormalities During Different Periods in Patients with Vestibular Migraine
Authors Li Y, Wang Y, Chen M, Jiang R, Ju Y
Received 21 May 2023
Accepted for publication 10 October 2023
Published 26 October 2023 Volume 2023:16 Pages 3583—3590
DOI https://doi.org/10.2147/JPR.S422255
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Houman Danesh
Yiqing Li,1,2 Yan Wang,2,* Meimei Chen,2,* Ruixuan Jiang,2,* Yi Ju2
1Department of Neurology, The First Affiliated Hospital of Fujian Medical University, Fuzhou, Fujian, People’s Republic of China; 2Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yi Ju, Email [email protected]
Purpose: The aim of this study was to assess abnormal eye movement signs during different periods, namely, ictal periods and symptom-free intervals, in patients with vestibular migraine.
Patients and Methods: We assessed oculomotor signs using videonystagmography in 90 patients with VM (40 during ictal periods and 50 during symptom-free intervals) according to validated diagnostic criteria.
Results: Abnormal saccades, smooth pursuit and optokinetic test results; spontaneous nystagmus; and positional nystagmus were all observed in vestibular migraine patients, and there was no significant difference between different periods. Positional nystagmus was the most common in both the ictal and asymptomatic periods (60% and 36%, respectively). Positional nystagmus was induced in a variety of positions during both periods, and the slow-phase velocity ranged from < 2 to 10°/s. The duration of positional nystagmus was over 60s in most cases. Overall, central oculomotor dysfunctions occurred in 27.5% of patients during VM attacks and 4% of patients during symptom-free intervals; this difference was statistically significant (p = 0.002).
Conclusion: In patients with VM, abnormal oculomotor signs can be found during both vertigo attacks and asymptomatic intervals. Positional nystagmus is the most common of these abnormalities and can be induced in different positions. The amplitude of these patients’ positional nystagmus tends to be low, and the duration tends to be long. Observing changes in eye movements by videonystagmography may be helpful in the diagnosis of VM.
Keywords: vestibular migraine, eye movements, periods, videonystagmography, positional nystagmus
Introduction
Vestibular migraine (VM) is a frequent variant of migraine characterized by episodic vertigo that may be accompanied by auditory symptoms. With a lifetime prevalence of 1%, VM is the most common cause of episodic vertigo.1 In recent years, many studies have described various aspects of VM, such as clinical characteristics, pathogenesis and examinations. However, the results of these studies are not specific. Oculographic studies during acute attacks indicate that VM mostly originates from central vestibular structures and only rarely involves the labyrinth. The current methods of examination included videonystagmography (VNG), caloric testing, vestibulo-ocular reflex (VOR) testing, vestibular evoked myogenic potential measurement, and magnetic resonance imaging. Ocular movements play an important role in the clinical diagnosis of vertigo-related diseases. A variety of ocular movement abnormalities can be found in VM patients during interictal periods; these abnormalities include horizontal or vertical saccades, positional nystagmus (PN), head-shaking nystagmus (HSN), gaze-evoked nystagmus (GEN), and spontaneous nystagmus (SN), among others. Furthermore, the incidence of these oculomotor signs has been found to increase after years of follow-up.2,3 These oculomotor signs can also be observed during VM attacks; PN is the most common, with an incidence of up to 100%. Most of these instances of PN consist of low-intensity, long-duration attacks of horizontal nystagmus, with a majority lasting more than 40s. However, all existing studies of eye movement in VM patients have small sample sizes, and no study has simultaneously described the oculomotor characteristics of patients with VM in different periods.
Materials and Methods
An assessment of VNG was performed in 90 patients with VM (14 men, 76 women; average age 49 years, range 20–74 years). These patients had presented to the Beijing Tiantan Hospital dizziness clinic between 2018.01 and 2019.10 and had been diagnosed with VM according to the criteria of the Barany Society.4
Patients with dizziness symptoms were excluded if they fulfilled the criteria for other dizziness-related diseases. If they had definite central neurological disorders, other severe accompanying diseases, or cognitive and mental disorders, they were excluded.
VNG examination was completed in the enrolled patients to measure the following: saccades; smooth pursuit; optokinetic nystagmus; SN; GEN; PN (roll test and Dix-Hallpike test); and caloric test results.
Each patient’s time of examination and latest time of vertigo onset were recorded. If less than 7 days had passed since the onset of the latest episode, the patient was considered to be having an attack; if more than 7 days had passed, the patient was considered to be in a symptom-free interval.
The criteria for the examination results were as follows. Smooth and regular square waves in the saccade test were judged as normal curves. Undershoot and overshoot were considered abnormal curves. In smooth pursuit, type I and II curves were classified as normal, and type III and type IV curves were classified as abnormal. The normal result of the optokinetic nystagmus test consisted of symmetrical left and right nystagmus, while an abnormal result was defined by left–right asymmetry, weakening or disorder of nystagmus. Slow-phase velocity (SPV) ≥6°/s was considered abnormal for SN and PN, and SPV < 2°/s was defined as low-amplitude nystagmus. The direction, SPV, and duration of nystagmus were recorded for each patient.
Central ocular motor dysfunction (COMD)2 was assumed to be present when 1 of the following findings was observed:
Statistical Analysis
For statistical analyses, SPSS 22.0 was used. Demographic data are presented with descriptive statistics. Measurement data are expressed as the mean ± standard deviation. The χ2 test or Fisher’s exact test was applied to determine differences in nominal variables, and Student’s t-test was used for differences in means. The Pearson method or the Spearman method was used for correlation analysis. A 2-sided significance criterion of p<0.05 was adopted.
Results
Characteristics and VNG Results in Patients with VM
VNG was completed in 90 patients (14 men, 76 women; average age 49 years, range 20~74 years), including 40 patients who were measured during attack periods and 50 patients who were measured during symptom-free intervals. There was no difference between the two groups in sex or age distribution. There was no difference in the rates of any type of ocular movement between the two groups, except for saccade (Table 1). Of the patients who were measured during attacks, 13 patients have no any oculomotor abnormality, 24 patients have one kind and 3 patients have 2 kinds. 32 patients during interictal have no any oculomotor abnormality, 15 patients have one kind, 1 patients have 2 kinds and 2 patients have ≥3 kinds (Table 2).
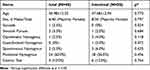 |
Table 1 Characteristics and VNG Results in Patients with VM |
 |
Table 2 Numbers of Oculomotor Abnormality in Patients with VM |
Oculomotor System Examination
Of the patients who were measured during attacks, 1 had abnormal saccades (undershoot), 2 had abnormal smooth pursuit (type III), and 1 had abnormal optokinetic nystagmus. Of the patients who were measured during interictal periods, 1 had abnormal smooth pursuit (type III), 2 had abnormal optokinetic nystagmus, and 1 had abnormal GEN.
Spontaneous Nystagmus
SN was observed in 2 patients during vertigo attacks, and the directions included both horizontal and vertical (down-beating). The intensity of nystagmus was 3°/s, and the duration was > 60s. In the interictal period, SN was observed in 3 patients; the direction was horizontal, the intensity of nystagmus was 2~3 °/s, and the duration was > 60s.
Positional Nystagmus
PN was present in 24 patients during attacks. In these patients, nystagmus could be induced by one or more positions, most commonly by the unilateral horizontal roll test. Different patients can show different directions of PN. For example, in the unilateral horizontal roll test, 5 patients showed geotropic nystagmus (Geo), and 4 patients showed apogeotropic nystagmus (Apo). Down-beating nystagmus (DBN) and torsional nystagmus (TN) were found in 2 patients and 1 patient, respectively. 8 patients have abnormal PN (SPV ≥6°/s) at least one position.
Similarly, PN in the interictal period was induced by a variety of positions, most commonly in the bilateral roll test. Some patients had bilateral Geo or bilateral Apo, and some had unilateral Geo that and changed to Apo when the patients rolled to the other side. No patient has abnormal PN. The amplitude of PN was small in both periods, and bouts of PN often lasted longer than 60s (Tables 3 and 4).
 |
Table 3 Analysis of PN in Interictal Patients |
 |
Table 4 Analysis of Positional Nystagmus in Ictal Patients |
Caloric Test
The results of the caloric test were abnormal in 4 patients (10%) during attacks; these patients had unilateral horizontal semicircular canal paresis. In the interictal period, 6 patients (12%) had abnormal results: 3 patients (6%) with unilateral horizontal semicircular canal paresis and 3 patients (6%) with bilateral horizontal semicircular canal paresis.
Central Ocular Motor Dysfunction
COMD was found in 11 patients (27.5%) in the ictal period and 2 patients (4.0%) in the interictal period, and this difference was statistically significant (χ2=9.588, p=0.002). Central PN, smooth pursuit and optokinetic nystagmus abnormalities were observed in both groups. Central PN (17.1%) was the most common abnormality in ictal patients, while optokinetic abnormalities were the most common type in interictal patients.
Incidence of Abnormal Ocular Movements in VM Patients During Different Periods
There were 23, 19, 21 and 27 patients with VM who completed the VNG examination at ≤3 days, 4–7 days, 8–14 days and > 14 days after vertigo attacks, respectively. The incidences of each abnormal ocular movement are shown in Table 5.
 |
Table 5 Incidence of Abnormal Ocular Movements in VM Patients During Different Periods |
Discussion
Oculomotor signs are an important part of physical examination in vertigo patients. During vertigo attacks, patients often have many abnormal oculomotor signs. Recognizing and capturing these signs is helpful for the diagnosis and differential diagnosis of vertigo-related diseases. This study assesses and compares eye movements in patients with VM at different periods. The attack period usually refers to a period of 7~14 days after the onset of dizziness or vertigo; the study by Polensek et al defines it as a period of 7 days after the onset of migraine.5 In our study, the first 7 days after the onset of vertigo was defined as the ictal period, and the period beyond 7 days was defined as the interictal period.
In recent years, there have been studies at home and abroad using VNG to record the ocular movements of VM patients, including nystagmus and non-nystagmus ocular movements. However, few studies have compared eye movement between VM patients in different periods; instead, most of them describe either ictal or interictal eye movement exclusively. Our study found that there were no differences in the incidence of any ocular movement between the two groups except for saccades. Oculomotor signs occurring in VM patients in the ictal period included SN (16~71.3%);5–8 GEN (10%);8 PN (40~100%);5–10 SP (25~92%);7,8 and HSN (35%).5 Oculomotor signs occurring in VM patients during the interictal period included SN (0~14.9%);6,11–15 GEN (0~27%);11–13,15 PN (8.3~55.4%);6,11,12,14 SP (8.6~48%);12,13 and HSN (15~38%).2,11,15,16
Non-nystagmus oculomotor abnormalities can also occur during VM attacks, the most common of which is saccadic pursuit.7,8 In addition, there are saccade test abnormalities, such as a prolonged incubation period, undershoot, and overshoot, but the incidence is low. In our study, it was observed that some patients had saccade undershoot, abnormal smooth pursuit test results, and abnormal optokinetic test results during attacks, but the proportion was small.
Studies have shown that the incidence of SN in VM patients during attacks is 16~45%, with both central and peripheral sources.7,8 The SPV of SN ranged from 3 to 33°/s, and the horizontal, vertical and rotational directions were all present, mainly in the horizontal direction. Spontaneous nystagmus has an incubation lasting ≥50 s and can be suppressed by gaze. The incidence of SN in interictal periods is 0~11%, but the characteristics were not described. In our study, SN was found in VM patients during different periods in the horizontal and/or vertical direction, with a nystagmus intensity of 2~3°/s and duration of > 60s. The characteristics of SN were similar in our study and a previous study.
The most common abnormal sign in VM patients during the attack period is PN, with an occurrence rate of 40~100%.5,7–9 All these studies found that the PN direction had horizontal, rotational, vertical and mixed components. The direction of the horizontal nystagmus is mainly apogeotropic, and PN can usually by induced by a variety of positions. The types of nystagmus are not consistent with semicircular canal disorders. The characteristics of PN are short latency or no latency, long duration and gaze suppression. When the evoked position is maintained, PN is mostly persistent. At least one component of nystagmus remains after the patient leaves the inducing position and returns to the supine position. Some studies have noted that the characteristic PN of VM patients has obvious clinical significance for the diagnosis of VM if their PN has the following characteristics: pure vertical (up-beating/down-beating) nystagmus, without torsion component; no latency, no fatigue; persistence of nystagmus with a constant intensity in the inducing position; gaze suppression; and effectiveness of antimigraine drugs in suppressing nystagmus and vertigo.10 Aside from this, studies have noted that compared with patients with horizontal semicircular canal benign paroxysmal positional vertigo (BPPV), patients with VM have a smaller maximum SPV, a longer latency to reach the maximum SPV and a slower change rate of nystagmus, which may be caused by an abnormal central integration mechanism that causes disorder of semicircular canal rotation information transmission in VM. This results in mixed nystagmus components and flat nystagmus induced by a variety of positions in the translocation test. The incidence of PN in interictal periods is 8.3~11%, but the characteristics were not described. Our study found that 60.0% of patients (attack periods) and 36.0% of patients (symptom-free periods) had PN. The most common trigger for positional nystagmus was the bilateral roll test. The directions were vertical (up-beating and down-beating), rotational, and horizontal (geotropic and apogeotropic nystagmus). Most patients had persistent, low-amplitude nystagmus.
The prevalence of caloric test abnormalities in our study is lower than previous estimates, which indicated unilateral canal paresis (UCP) in 8% to 22%12,13,17–23 and bilateral vestibular failure in up to 11%17,19,20,23 of patients with VM. Considerably increased rates of UCP have been reported in basilar-type migraine (55–60%).21–23 Patients with Meniere’s disease (MD) have been reported to have over 50% UCP prevalence in other studies.24,25
The incidence of oculomotor disorders in VM patients during the symptom-free period increased gradually with time. An average of 9 years of follow-up of VM patients in the non-seizure period showed that the rate of abnormal ocular movements increased from 16% to 41%; the most common was PN (28%), of which 18% was clear central PN. Interictal central-type PN may help distinguish VM from peripheral vestibular disorders such as MD.2 Another study found that the most common COMD in VM patients during the interictal period was saccadic pursuit, which could be vertical or horizontal. The incidence of COMD increased from 20% to 63% during follow-up. Our study is reported from different perspectives. The time of VNG examination was different among patients. The longer the time after the onset of vertigo, the lower the incidence of PN was, but the incidence never fell below 29%. This further supports the necessity of using VNG to check patients’ signs during interictal, especially PN. Other ocular movements were rare enough that we could not identify their trends in this study; however, it may be possible to identify trends by increasing the sample size.
Early studies showed that 77.5% of VM patients had definite vestibular and/or cochlear system dysfunction during attacks, among which 18.8% of cases were of central origin, 28.8% were of peripheral, and 30% were of unknown origin.17 Later, a study with a small sample size showed that 70% of VM patients had pathological nystagmus during the attack period, among which 50% of cases were of central origin, 15% were of peripheral origin, and 35% were of unclear origin.8 The presence of COMD had a positive predictive value of 90.5% for the diagnosis of VM during follow-up. However, cases were mostly mild and, once present, did not worsen or disappear over many years of follow-up. Prevention and treatment of migraine can effectively prevent the development and progression of COMD.3 In our study, COMD was found in 27.5% of patients in the ictal period and only 4% of patients in the interictal period. The most common eye movement abnormality in ictal patients was central PN.
Nystagmus during acute episodes of VM can be induced by a variety of stimuli (eg, horizontal head shaking or positional testing) or without any stimulation, while saccadic pursuit, prolonged saccade latency, undershoot, and overshoot can also be observed, suggesting that more than one anatomical site may be involved in causing the patient’s symptoms and signs. The spontaneous nystagmus or prolonged vestibular reaction time that occurs in some VM patients during episodes may be related to vestibular hyperexcitability.26,27 However, it is currently unknown whether this hyperexcitability is at the level of the anterior vestibular system or the brainstem, or whether it is related to the regulatory effects of the cerebellum or hemispheres on the vestibular system. At present, the pathogenesis of VM is not clear, but several mechanisms have been proposed to explain its symptoms; these putative mechanisms include cortical spreading depression, the trigeminovascular theory, abnormal central signal integration and genetic factors. Some scholars have observed both peripheral and central vestibular disorders in VM patients, and the mechanisms that include both central and peripheral components may be the most reasonable. Neuropeptides, especially calcitonin gene-related peptide (CGRP), are the putative molecular mediators. They have neuromodulatory effects in both the peripheral and central nervous systems.13 Nerve activity of the trigeminovascular system (TVS) is the main mechanism of migraine.28 Substance P and CGRP can cause vasodilatation and neurogenic inflammation, leading to migraine attacks.29–31 PET studies have shown that multiple sites in the brainstem are associated with migraine, such as the midbrain periaqueductal gray matter, dorsal raphe nucleus, and locus ceruleus, which are continuously activated during the migraine interictal period.32,33 Brainstem centers such as the midbrain periaqueductal gray matter and hypothalamus are also associated with the TVS and vestibular nuclei.34,35 These interconnections can modulate TVS and neural activity within the vestibular system; for example, stimulation of the trigeminal nerve has been shown to cause nystagmus in migraine patients.36 The wave of CSD could reach the vestibular cortex or the brainstem vestibular nuclei causing vestibular symptoms. A study demonstrates that the incidence of acute vestibular symptoms in supratentorial stroke is 3.7%, with being isolated in 1%. The widespread lesions responsible for acute vestibular symptoms implicate diffuse multisensory cortical-subcortical networks in the cerebral hemispheres without a lateralization.37 The absence of nystagmus during interictal may be due to CSD primarily in VM patients, given that supratentorial stroke has a low incidence of oculomotor abnormalities and CSD is predominantly supratentorial manifestations, according to the study described above.
This study was a single-center study with a small sample size, and the enrolled VM patients were not followed up further with VNG examination. The changes in VNG results in the same patient during the ictal and interictal periods should correspond to the changes in eye movement abnormalities among the patients overall.
Conclusion
Abnormal nystagmus electrogram results can be found in both the ictal and interictal periods in VM patients, and the most common is positional nystagmus. Nystagmus can be induced by different positions in the same patients and has a variable direction, a small amplitude, and a long duration. Therefore, it is recommended that patients undergo VNG during episodes to observe the pattern of eye movements, which may be helpful for the differential diagnosis of VM. Long-term follow-up of VM patients to observe the changes in nystagmus may be helpful for diagnosis and treatment evaluation.
Ethics Statement
This study was approved by the Institutional Review Board of Beijing Tiantan Hospital, Capital Medical University. Patient informed consent to review their medical records was waived by the Institutional Review Board of Beijing Tiantan Hospital, Capital Medical University, because this was a retrospective study, the data recorded from the patient file will be treated confidentially and data excludes the display of names and other personal information. No reference is made in written reports that could associate the participants with the study. The study was conducted in accordance with the principles set out in the Declaration of Helsinki.
Disclosure
The authors have no conflict of interest to report.
References
1. Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol. 2009;256(3):333–338. doi:10.1007/s00415-009-0149-2
2. Radtke A, von Brevern M, Neuhauser H, Hottenrott T, Lempert T. Vestibular migraine: long-term follow-up of clinical symptoms and vestibulo-cochlear findings. Neurology. 2012;79(15):1607–1614. doi:10.1212/WNL.0b013e31826e264f
3. Neugebauer H, Adrion C, Glaser M, Strupp M. Long-term changes of central ocular motor signs in patients with vestibular migraine. Eur Neurol. 2013;69(2):102–107. doi:10.1159/000343814
4. Lempert T, Olesen J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res. 2012;22(4):167–172. doi:10.3233/VES-2012-0453
5. Polensek SH, Tusa RJ. Nystagmus during attacks of vestibular migraine: an aid in diagnosis. Audiol Neurootol. 2010;15(4):241–246. doi:10.1159/000255440
6. Young AS, Nham B, Bradshaw AP, et al. Clinical, oculographic, and vestibular test characteristics of vestibular migraine. Cephalalgia. 2021;41(10):1039–1052. doi:10.1177/03331024211006042
7. ElSherif M, Reda MI, Saadallah H, Mourad M. Eye movements and imaging in vestibular migraine. Acta Otorrinolaringol Esp. 2020;71(1):1–6. doi:10.1016/j.otorri.2018.10.001
8. von Brevern M, Zeise D, Neuhauser H, Clarke AH, Lempert T. Acute migrainous vertigo: clinical and oculographic findings. Brain. 2005;128(Pt 2):365–374. doi:10.1093/brain/awh351
9. Hazzaa N, Mowafy SSE. Clinical features of vestibular migraine in Egypt. Egypt J Ear Nose Throat Allied Sci. 2016;17:17–21. doi:10.1016/j.ejenta.2015.12.002
10. El-Badry MM, Samy H, Kabel AM, Rafat FM, Sanyelbhaa H. Clinical criteria of positional vertical nystagmus in vestibular migraine. Acta Otolaryngol. 2017;137(7):720–722. doi:10.1080/00016489.2017.1318220
11. Beh SC, Masrour S, Smith SV, Friedman DI. The spectrum of vestibular migraine: clinical features, triggers, and examination findings. Headache. 2019;59(5):727–740. doi:10.1111/head.13484
12. Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol. 1999;246(10):883–892. doi:10.1007/s004150050478
13. Celebisoy N, Gokcay F, Sirin H, Bicak N. Migrainous vertigo: clinical, oculographic and posturographic findings. Cephalalgia. 2008;28(1):72–77. doi:10.1111/j.1468-2982.2007.01474.x
14. Vitkovic J, Paine M, Rance G. Neuro-otological findings in patients with migraine- and nonmigraine-related dizziness. Audiol Neurootol. 2008;13(2):113–122. doi:10.1159/000111783
15. Jeong SH, Oh SY, Kim HJ, Koo JW, Kim JS. Vestibular dysfunction in migraine: effects of associated vertigo and motion sickness. J Neurol. 2010;257(6):905–912. doi:10.1007/s00415-009-5435-5
16. Shin JE, Kim CH, Park HJ. Vestibular abnormality in patients with Meniere’s disease and migrainous vertigo. Acta Otolaryngol. 2013;133(2):154–158. doi:10.3109/00016489.2012.727469
17. Kayan A, Hood JD. Neuro-otological manifestations of migraine. Brain. 1984;107(Pt 4):1123–1142. doi:10.1093/brain/107.4.1123
18. Cutrer FM, Baloh RW. Migraine-Associated Dizziness. Headache. 1992;32(6):300–304. doi:10.1111/j.1526-4610.1992.hed3206300.x
19. Cass SP, Furman JM, Ankerstjerne K, Balaban C, Yetiser S, Aydogan B. Migraine-related vestibulopathy. Ann Otol Rhinol Laryngol. 1997;106(3):182–189. doi:10.1177/000348949710600302
20. Teggi R, Colombo B, Bernasconi L, Bellini C, Comi G, Bussi M. Migrainous vertigo: results of caloric testing and stabilometric findings. Headache. 2009;49(3):435–444. doi:10.1111/j.1526-4610.2009.01338.x
21. Olsson JE. Neurotologic findings in basilar migraine. Laryngoscope. 1991;101(S52):1–41. doi:10.1002/lary.1991.101.s52.1
22. Eviatar L. Vestibular testing in basilar artery migraine. Ann Neurol. 1981;9(2):126–130. doi:10.1002/ana.410090205
23. Chi-Te W, Mei-Su L, Yi-Ho Y. Relationship between basilar-type migraine and migrainous vertigo. Headache. 2008;49(3):426–434. doi:10.1111/j.1526-4610.2008.01283.x
24. Huppert D, Strupp M, Brandt T. Long-term course of Menie`re’s disease revisited. Acta Otolaryngol. 2010;130(6):644–651. doi:10.3109/00016480903382808
25. Park HJ, Migliaccio AA, Santina CCD, Minor LB, Carey JP. Search-coil head thrust and caloric test in Meniere’s disease. Acta Oto-Laryngologica. 2005;125(8):852–857. doi:10.1080/00016480510033667
26. Furman JM, Sparto PJ, Soso M, Marcus D. Vestibular function in migraine-related dizziness: a pilot study. J Vestib Res. 2005;15(5–6):327–332. doi:10.3233/VES-2005-155-608
27. King S, Wang J, Priesol AJ, Lewis RF. Central integration of canal and otolith signals is abnormal in vestibular migraine. Front Neurol. 2014;5:233. doi:10.3389/fneur.2014.00233
28. Pietrobon D, Moskowitz MA. Pathophysiology of migraine. Annu Rev Physiol. 2013;75(1):365–391. doi:10.1146/annurev-physiol-030212-183717
29. Durham PL. Calcitonin gene-related peptide (CGRP) and migraine. Headache. 2006;46(Suppl 1):S3–S8. doi:10.1111/j.1526-4610.2006.00483.x
30. Furman JM, Marcus DA, Balaban CD. Migrainous vertigo: development of a pathogenetic model and structured diagnostic interview. Curr Opin Neurol. 2003;16(1):5–13. doi:10.1097/00019052-200302000-00002
31. Schytz HW, Olesen J, Ashina M. The PACAP receptor: a novel target for migraine treatment. Neurotherapeutics. 2010;7(2):191–196. doi:10.1016/j.nurt.2010.02.003
32. Weiller C, May A, Limmroth V, et al. Brain stem activation in spontaneous human migraine attacks. Nat Med. 1995;1(7):658–660. doi:10.1038/nm0795-658
33. Bahra A, Matharu MS, Buchel C, Frackowiak RS, Goadsby PJ. Brainstem activation specific to migraine headache. Lancet. 2001;357(9261):1016–1017. doi:10.1016/S0140-6736(00)04250-1
34. Halberstadt AL, Balaban CD. Organization of projections from the raphe nuclei to the vestibular nuclei in rats. Neuroscience. 2003;120(2):573–594. doi:10.1016/S0306-4522(02)00952-1
35. Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci. 2011;12(10):570–584. doi:10.1038/nrn3057
36. Marano E, Marcelli V, Di Stasio E, et al. Trigeminal stimulation elicits a peripheral vestibular imbalance in migraine patients. Headache. 2005;45(4):325–331. doi:10.1111/j.1526-4610.2005.05069.x
37. Park J-Y, Choi J-H, Kwon J-H, et al. Incidence, characteristics, and neuroanatomical substrates of vestibular symptoms in supratentorial stroke. J Neurol. 2023;270(4):2174–2183. doi:10.1007/s00415-023-11566-9
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
