Back to Journals » International Journal of General Medicine » Volume 15
Extent of Ejection Fraction Improvement After Revascularization Associated with Outcomes Among Patients with Ischemic Left Ventricular Dysfunction
Authors Wang S , Cheng S, Zhang Y, Lyu Y, Liu J
Received 28 June 2022
Accepted for publication 29 August 2022
Published 13 September 2022 Volume 2022:15 Pages 7219—7228
DOI https://doi.org/10.2147/IJGM.S380276
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Shaoping Wang,1 Shujuan Cheng,1 Yuchao Zhang,1 Yi Lyu,2 Jinghua Liu1
1Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University, Beijing Institute of Heart Lung and Blood Vessel Diseases, Beijing, People’s Republic of China; 2Department of Anesthesiology, Minhang Hospital, Fudan University, Shanghai, People’s Republic of China
Correspondence: Jinghua Liu, Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University, No. 2 Anzhen Road, Chaoyang District, Beijing, 100029, People’s Republic of China, Tel +86 10 64456998, Fax +86 1064456998, Email [email protected] Yi Lyu, Department of Anesthesiology, Minhang Hospital, Fudan University, No. 180 Xinsong Road, Minhang District, Shanghai, 201199, People’s Republic of China, Email [email protected]
Purpose: Ejection fraction (EF) has been reported to be a major predictor of improved survival in patients with heart failure. However, it is largely unknown whether the extent of improvement in EF affects the subsequent risk of mortality. This study sought to investigate change in EF after revascularization and the implication of these changes on clinical outcomes among patients with ischemic left ventricular dysfunction.
Patients and Methods: We conducted a cohort study (No. ChiCTR2100044378) of patients with reduced EF (≤ 40%) who received revascularization and had EF reassessment by echocardiography 3 months after revascularization. Patients were categorized according to the absolute change in EF: 1) EF worsened group (absolute decrease in EF > 5%); 2) EF unchanged group (absolute change in EF − 5% to 5%); 3) EF improved group (absolute increase in EF > 5%).
Results: Of 974 patients, 84 (8.6%) had EF worsened, 317 (32.5%) had EF unchanged and 573 (58.8%) had EF improved. The median follow-up time was 3.5 years, during which 143 patients died. For each 5-unit increments in EF, the risk of death decreased by 20% (hazard ratio, HR, per 5% increases, 0.80; 95% CI, 0.73– 0.86; P< 0.001). Compared with EF improvement group, patients with EF worsened (HR, 3.35; 95% CI, 2.07– 5.42; P< 0.001) and patients with EF unchanged (HR, 2.05; 95% CI, 1.40– 3.01; P< 0.001) had significantly higher risk of all-cause death.
Conclusion: Changes in EF were inversely associated with the risk of mortality. The extent of EF improvement after revascularization might be a potential factor which defines clinical outcomes.
Keywords: ejection fraction, left ventricular dysfunction, heart failure, revascularization
Introduction
The cornerstone of treatment of patients with heart failure (HF) and reduced ejection fraction (EF) continues to be optimal medical therapy, which is associated with significant improvement in survival and quality of life.1,2 Partial congestive HF patients with reduced EF have an opportunity for recovery of EF to a normal level after a period of appropriate therapy. Patients with recovered EF might have more favorable outcomes, including a lower risk of mortality,3–7 HF hospitalization4,6,7 and better quality of life8 compared to patients with persistently reduced EF. EF has been reported to be a major predictor of improved survival in patients with HF and reduced EF.9–11 For example, it has been demonstrated that after a period of appropriated therapy, patients with recovered EF (from EF <35% to EF >40%3 or from EF <45% to EF ≥45%5) has a lower risk of long-term mortality compared to patients with unrecovered EF (EF remained ≤40% or <45%). However, the association between EF improvement and survival benefit is not consistent from literatures. One observational study indicated lack of improvement in EF after CABG was not associated with poorer outcome compared with that of patients with improved EF.12 From the STICH (Surgical Treatment for Ischemic Heart Failure) trial, it was revealed that there was no relationship between changes in EF and subsequent death.13 Whether the improvement in EF affects the subsequent risk of mortality needs to be further investigated.
Ischemic etiology is one of important risk factors for lack of EF improvement among patients with HF.3,6,14 Revascularization including coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) may attenuate the ischemic state and reversing left ventricular (LV) remodeling,15–18 thus improve the long-term outcomes of patients with LV dysfunction.19–22 However, revascularization therapy among patients with LV dysfunction is not always effective. The extent and determinants of EF improvement after revascularization have not been well investigated.16,23–27 The presence of myocardial viability might be one of correlates of EF improvement after coronary revascularization.23,28,29 However, in different studies, about 12%29 to 64%23 patients remained EF unimproved after revascularization. We recently reported that diabetes mellitus (DM) associated with greater EF improvement after revascularization among patients with reduced EF.30 The predictive factor associated with change in EF after revascularization needs to be further clarified.
Therefore, this study was performed to investigate 1) the extent of EF improvement following revascularization in patients with coronary artery disease (CAD) and preoperative EF ≤40%; 2) the determinants of absolute change in EF after revascularization; 3) the association between absolute change in EF and clinical outcomes.
Materials and Methods
Patient Selection
This was a real-world cohort study that used data from Beijing Anzhen Hospital. The study was registered in Chinese Clinical Trial Registry (No. ChiCTR2100044378). The study protocol was approved by the hospital’s ethics committee.
CAD patients with reduced EF (≤40%) who underwent CABG or PCI with a drug-eluting stent between January 2005 and December 2014, and with repeated EF measurements during follow-up were enrolled. Patients were excluded if they had concomitant noncoronary surgery, were diagnosed as ST-segment elevation myocardial infarction and had only one record of EF follow-up reassessment within 3 months after revascularization. The final study sample included patients who had EF reassessment by echocardiography 3 months after revascularization. Patients were then categorized according to the absolute change in EF: 1) EF worsened group (absolute decrease in EF >5%); 2) EF unchanged group (absolute change in EF −5% to 5%); 3) EF improved group (absolute increase in EF >5%).31
Data Collection and Definitions
Baseline demographic, clinical, laboratory, angiographic parameters, and medical therapy for the study patients were ascertained from Beijing Anzhen Hospital medical records. Baseline EF was captured within 30 days before PCI or CABG. Follow-up EF values were defined as the first EF measurement 3 months32 after revascularization assessed in Beijing Anzhen Hospital. Complete revascularization was defined as successful PCI (residual stenosis of <30%) of all angiographically significant lesions (≥70% diameter stenosis) in 3 coronary arteries and their major branches. A staged procedure within 90 days after discharge was acceptable For CABG, grafting of every primary coronary artery with ≥70% diameter stenosis was accepted as complete revascularization.
Outcome data were obtained from medical records at Beijing Anzhen Hospital and through telephone follow-up. Death was regarded as cardiovascular in origin unless obvious non-cardiovascular causes could be identified. Any death during hospitalization for repeat coronary revascularization was regarded as cardiovascular death. The follow-up time for patients started at the time of the first available EF measurement.31,33,34
Statistical Analysis
Categorical variables were summarized as frequencies with percentages and continuous variables were expressed as mean ± SD. Baseline characteristics were compared among the EF worsened, EF unchanged and EF improved groups by using Chi-Square test for categorical variables and one-way ANOVA for continuous variables. Multinomial logistic regression was used to identify independent correlates of patients in the three EF categories as defined above: worsened, unchanged or improved EF. Outcome with improved EF was set as the reference category to calculate the relative risk ratios (RRR) of variables to have worsened EF or unchanged EF. Variables of demographics and history, preoperative echocardiography values, angiography and medical therapies as well as clinical chemistry were included in the analysis. Cumulative incidences were estimated by the Kaplan–Meier method and compared by Log rank test. The risks of outcomes were analyzed with a Cox proportional hazards regression model. The proportional hazards assumption was tested for individual covariates and globally on the basis of Schoenfeld residuals. All statistical analyses were based on 2-tailed tests. P<0.05 was considered statistically significant. Statistical analyses were performed with Stata version 14.0 (StataCorp).
Results
Patients Characteristics
Among 1816 initially identified patients, 78 patients who died within 3 months after revascularization, 764 patients were further excluded because EF was not evaluated 3 months after revascularization. Finally, 974 patients who had an initial EF ≤40% and had echocardiography reassessment 3 months after revascularization were enrolled in this study. The differences of the characteristics at baseline between enrolled and excluded patients are indicated in Supplemental Table 1.
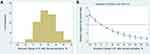
The average age at baseline was 64.7±10.9 years (Table 1). Men comprised 83.5% of all subjects. Five hundred and fifty-six (57.1%) received PCI and 418 (42.9%) underwent CABG. After revascularization, 84 (8.6%) had EF worsened, 317 (32.5%) had EF unchanged and 573 (58.8%) had EF improved (Figure 1A). Age at baseline and sex distribution were similar among three groups (Table 1). The EF improved group had a significantly highest prevalence of DM (P=0.008) and lowest prevalence of myocardial infarction (MI) (P=0.001) compared with other two groups. The anatomic severity of coronary artery disease was similar among three groups. There was no significant difference in the proportions undergoing revascularization by PCI or CABG, and the groups had similar percentages of complete revascularization. The EF improved group had a significantly highest proportion of use of clopidogrel or ticagrelor compared with other two groups (P=0.031).
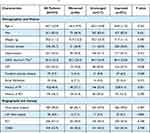 |
Table 1 Patient Characteristics at Baselinea |
Echocardiographic Characteristics
In the EF improved group, the preoperative EF was lowest compared with other two groups (P<0.001) (Table 2). Mean (SD) EF improved significantly, from 35.8% (4.7%) to 52.0% (8.6%), in the EF improved group (P<0.001). In the EF unchanged group, the change in EF was small but statistically significant, from 36.8% (3.7%) to 37.6% (4.7%) (P<0.001). In contrast, EF decreased significantly, from 37.3% (2.8%) to 27.5% (4.1%) in the EF worsened group (P<0.001). Both preoperative and postoperative LV end-diastolic diameter (LVEDD) (P<0.001) as well as end-systolic diameter (LVESD) (P<0.001) were smallest in EF improved group compared with other two groups. With the most reduction of LV size, the severity of mitral regurgitation was lowest in EF improved group (P<0.001). The mean duration between the preoperative and follow-up EF measurements in three groups was comparable (worsened group: 5.0±3.6 months; unchanged group: 6.1±2.0 months; improved group: 5.9±2.6 months, P=0.203).
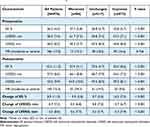 |
Table 2 Echocardiographic Characteristics a |
Predictors of Change in EF
Compared to patients with EF improved, patients who had history of DM had less likely to have worsened EF (relative risk ratios [RRR], 0.48; 95% confidence interval [CI], 0.28–0.83; P = 0.008) or unchanged EF (RRR, 0.74; 95% CI, 0.55–0.99; P = 0.043) (Table 3). Compared to patients with EF improved, patients who had history of MI had higher likely to have worsened EF (RRR, 1.88; 95% CI, 1.18–2.98; P = 0.008) or unchanged EF (RRR, 1.55; 95% CI, 1.17–2.04; P = 0.002). Patients with higher preoperative EF had greater likely of being in the EF worsened group (RRR per 1% increase in EF, 1.10; 95% CI, 1.03–1.17; P = 0.005) or EF unchanged group (RRR per 1% increase in EF, 1.06; 95% CI, 1.02–1.09; P = 0.002). Severity of LV remodeling as indicated by LVESD and LVEDD also significantly associated with change in EF. Neither anatomic severity of coronary vessels (as indicated by multivessel disease and left main disease) nor extent of revascularization (complete vs incomplete) was an independent correlate of change in EF. Compared to patients with EF improved, patients who had clopidogrel or ticagrelor had less likely to have unchanged EF (RRR, 0.67; 95% CI, 0.49–0.91; P = 0.011).
 |
Table 3 Baseline Factors Associated with Worsened EF or Unchanged EF in Comparison with Improved EF |
Outcomes
The median follow-up time was 3.5 years, during which 143 patients died and 117 patients were cardiac death. Greater extent of EF improvement after revascularization was significantly associated with lower risk of all-cause death. For each 5-unit increments in EF, the risk of death decreased by 20% (hazard ratio, HR, per 5% increases, 0.80; 95% CI, 0.73–0.86; P<0.001) (Figure 1B). Compared with EF improvement group, patients with EF worsened had significantly higher risk of all-cause death (HR, 3.35; 95% CI, 2.07–5.42; P<0.001) and cardiovascular death (HR, 4.12; 95% CI, 2.45–6.93; P<0.001) (Table 4, Figure 2A and B). Similarly, compared with EF improvement group, patients with EF unchanged had significantly higher risk of all-cause death (HR, 2.05; 95% CI, 1.40–3.01; P<0.001) and cardiovascular death (HR, 2.23; 95% CI, 1.44–3.45; P<0.001). Furthermore, patients with EF worsened had significantly higher risk of all-cause death (HR, 1.63; 95% CI, 1.00–2.66; P=0.048) and cardiovascular death (HR, 1.85; 95% CI, 1.10–3.11; P=0.020) compared with EF unchanged group. Those findings persisted in adjusted model.
 |
Table 4 Risk of Outcomes |
In addition, there were 123 (14.6%) patients had repeated revascularization by either PCI or CABG during follow-up. The EF improved group (17.1%) had a significantly highest proportion of repeated revascularization compared with EF unchanged group (12.2%) and EF worsened group (6.9%) (P=0.030).
Discussion
Available data suggest that HF might not always be a progressive disease. Several therapies including guideline-directed medical therapy,14 cardiac resynchronization therapy31 and revascularization17,18,23 might improve EF for patients with LV dysfunction. Ischemic etiology is one of important risk factors for lack of EF improvement among patients with HF.3,6,14 However, the extent of EF improvement after revascularization has not been well-established. A study enrolled 47 CAD patients with initial EF <50% who underwent coronary revascularization demonstrated that 42.6% had EF improved ≥10%.17 In the current study, after revascularization in patients with reduced EF (≤40%), about 10% remained follow-up EF worsened (absolute decrease in EF >5%), about 30% had follow-up EF unchanged (absolute change in EF −5% to 5%) and about 60% had EF improved (absolute increase in EF >5%).
In the current study, DM, no prior MI, lower preoperative EF and less LV enlargement were identified as factors associated with greater EF improvement after revascularization. The mismatch between blood supply and cardiac metabolic requirements in ischemic heart was more severe in diabetic compared with non-diabetic myocardium. Thus, revascularization might have greater effect on LV remodeling in patients with DM.30 Patients with history of MI might have less viable myocardium which resulted in less opportunity to have EF improvement following revascularization. It has been reported that preoperative EF less than 27% was one of three prognostic factors which associated with greater survival benefit from CABG.27 Lower preoperative EF and less LV enlargement might represent a critical cardiac stage that might benefit more from revascularization. In the current study, no guideline-directed medical therapy for HF was found to be predictive of EF improvement. One potential reason was that the effect of medication was attenuated by revascularization. After revascularization, only 200 (20.5%) had a follow-up EF ≤35%. Furthermore, although complete revascularization did not associate with EF improvement, the EF improvement group had highest proportion of repeated revascularization during follow-up. Considering the course of the disease, a possibility can be that EF initially improves after successful revascularization but subsequently worsens, and this feature is suspicious of recurrence of significant coronary stenosis. The association between repeat revascularization and EF improvement needs to be further investigated. In this study that extent of EF improvement was firstly identified, to our knowledge, as a factor associated with clinical outcomes after revascularization among CAD patients with reduced EF. For each 5-U increments in EF, the risk of death decreased by 20%. Compared with EF improvement group, patients with EF worsened or unchanged had significantly higher risk of all-cause death and cardiovascular death. Whether extent of EF improvement has clinical implication for ICD implantation-decision making needs to be further investigation.
All patients in the current study underwent isolated CABG. Moderate to severe mitral regurgitation were not treated simultaneously. However, mitral regurgitation might have a great impact on cardiac function recovery and outcomes.35 This needs to be further investigated.
Since the present study was designed as a single-center and observational study, there is a possibility of patients selection bias. Since institutions and specific methods for measuring EF vary, only EF measurements by echocardiography in Anzhen Hospital were adopted. This restriction improved the accuracy of the EF measurements but increased the number of excluded patients. Of 1948 person-time EF measurements, 948 (97.3%) EF measurements before revascularization and 898 (92.2%) EF measurements during follow-up were by Simpson. It would be better to have myocardial viability test before PCI/CABG, nevertheless, it was sometimes difficult to perform for HF patients. There was little data of myocardial viability in current study cohort. Minimal patients (n = 11) had ICD therapy during the follow-up. This might overestimate the mortality especially for patients with EF worsened according to the current therapeutic strategy.
Conclusion
After revascularization in patients with reduced EF (≤40%), about 10% remained follow-up EF worsened, about 30% had EF unchanged and about 60% had EF improved. Patients with EF improvement were more likely to have DM, have no prior MI, have lower preoperative EF and have less LV enlargement. Changes in EF were inversely associated with the risk of mortality. The extent of EF improvement after revascularization might be a potential factor which defines clinical outcomes.
Data Sharing Statement
The datasets are available from the corresponding author (Jinghua Liu) upon reasonable request.
Ethical Approval and Informed Consent
The Ethics Committee of the Beijing Anzhen Hospital approved the study. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki. Because this was a retrospective cohort study and waiver of informed consent will not adversely affect the rights and welfare of the subjects, written informed consent from the patients was waived.
Acknowledgments
We express our gratitude to all participated staffs for completing the CRISIS Project.
Funding
There is no funding to report.
Disclosure
All authors declare that they have no conflicts of interest in this work.
References
1. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC.. Eur Heart J. 2016;37(27):2129–2200. doi:10.1093/eurheartj/ehw128
2. Wang X, Hu D, Dang S, et al. Effects of Traditional Chinese Medicine Shensong Yangxin capsules on heart rhythm and function in congestive heart failure patients with frequent ventricular premature complexes: a randomized, double-blind, multicenter clinical trial. Chin Med J. 2017;130(14):1639–1647. doi:10.4103/0366-6999.209906
3. Florea VG, Rector TS, Anand IS, Cohn JN. Heart failure with improved ejection fraction: clinical characteristics, correlates of recovery, and survival: results from the valsartan heart failure trial. Circ Heart Fail. 2016;9(7). doi:10.1161/CIRCHEARTFAILURE.116.003123
4. Basuray A, French B, Ky B, et al. Heart failure with recovered ejection fraction: clinical description, biomarkers, and outcomes. Circulation. 2014;129(23):2380–2387. doi:10.1161/CIRCULATIONAHA.113.006855
5. de Groote P, Fertin M, Duva Pentiah A, Goeminne C, Lamblin N, Bauters C. Long-term functional and clinical follow-up of patients with heart failure with recovered left ventricular ejection fraction after beta-blocker therapy. Circ Heart Fail. 2014;7(3):434–439. doi:10.1161/CIRCHEARTFAILURE.113.000813
6. Kalogeropoulos AP, Fonarow GC, Georgiopoulou V, et al. Characteristics and outcomes of adult outpatients with heart failure and improved or recovered ejection fraction. JAMA Cardiol. 2016;1(5):510–518. doi:10.1001/jamacardio.2016.1325
7. Lupon J, Diez-Lopez C, de Antonio M, et al. Recovered heart failure with reduced ejection fraction and outcomes: a prospective study. Eur J Heart Fail. 2017;19(12):1615–1623. doi:10.1002/ejhf.824
8. Joyce E, Chung C, Badloe S, et al. Variable contribution of heart failure to quality of life in ambulatory heart failure with reduced, better, or preserved ejection fraction. JACC Heart Fail. 2016;4(3):184–193. doi:10.1016/j.jchf.2015.12.011
9. John Sutton M S, Pfeffer MA, Moye L, et al. Cardiovascular death and left ventricular remodeling two years after myocardial infarction: baseline predictors and impact of long-term use of captopril: information from the Survival and Ventricular Enlargement (SAVE) trial. Circulation. 1997;96(10):3294–3299. doi:10.1161/01.CIR.96.10.3294
10. Solomon SD, Skali H, Anavekar NS, et al. Changes in ventricular size and function in patients treated with valsartan, captopril, or both after myocardial infarction. Circulation. 2005;111(25):3411–3419. doi:10.1161/CIRCULATIONAHA.104.508093
11. Gula LJ, Klein GJ, Hellkamp AS, et al. Ejection fraction assessment and survival: an analysis of the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT). Am Heart J. 2008;156(6):1196–1200. doi:10.1016/j.ahj.2008.08.007
12. Samady H, Elefteriades JA, Abbott BG, Mattera JA, McPherson CA, Wackers FJ. Failure to improve left ventricular function after coronary revascularization for ischemic cardiomyopathy is not associated with worse outcome. Circulation. 1999;100(12):1298–1304. doi:10.1161/01.CIR.100.12.1298
13. Panza JA, Ellis AM, Al-Khalidi HR, et al. Myocardial Viability and Long-Term Outcomes in Ischemic Cardiomyopathy. N Engl J Med. 2019;381(8):739–748. doi:10.1056/NEJMoa1807365
14. Wilcox JE, Fonarow GC, Yancy CW, et al. Factors associated with improvement in ejection fraction in clinical practice among patients with heart failure: findings from IMPROVE HF. Am Heart J. 2012;163(1):49–56 e42. doi:10.1016/j.ahj.2011.10.001
15. Michler RE, Rouleau JL, Al-Khalidi HR, et al. Insights from the STICH trial: change in left ventricular size after coronary artery bypass grafting with and without surgical ventricular reconstruction. J Thorac Cardiovasc Surg. 2013;146(5):1139–1145 e1136. doi:10.1016/j.jtcvs.2012.09.007
16. Vakil K, Florea V, Koene R, Kealhofer JV, Anand I, Adabag S. Effect of coronary artery bypass grafting on left ventricular ejection fraction in men eligible for implantable cardioverter-defibrillator. Am J Cardiol. 2016;117(6):957–960. doi:10.1016/j.amjcard.2015.12.029
17. Adachi Y, Sakakura K, Wada H, et al. Determinants of left ventricular systolic function improvement following coronary artery revascularization in Heart Failure Patients With Reduced Ejection Fraction (HFrEF). Int Heart J. 2016;57(5):565–572. doi:10.1536/ihj.16-087
18. Wang S, Lyu Y, Cheng S, Liu J, Borah BJ. Clinical outcomes of patients with coronary artery diseases and moderate left ventricular dysfunction: percutaneous coronary intervention versus coronary artery bypass graft surgery. Ther Clin Risk Manag. 2021;17:1103–1111. doi:10.2147/TCRM.S336713
19. Velazquez EJ, Lee KL, Jones RH, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374(16):1511–1520. doi:10.1056/NEJMoa1602001
20. Yang JH, Choi SH, Song YB, et al. Long-term outcomes of drug-eluting stent implantation versus coronary artery bypass grafting for patients with coronary artery disease and chronic left ventricular systolic dysfunction. Am J Cardiol. 2013;112(5):623–629. doi:10.1016/j.amjcard.2013.04.035
21. Lee DH, Jeong MH, Rhee JA, et al. Predictors of long-term survival in acute coronary syndrome patients with left ventricular dysfunction after percutaneous coronary intervention. Korean Circ J. 2012;42(10):692–697. doi:10.4070/kcj.2012.42.10.692
22. Kunadian V, Pugh A, Zaman AG, Qiu W. Percutaneous coronary intervention among patients with left ventricular systolic dysfunction: a review and meta-analysis of 19 clinical studies. Coron Artery Dis. 2012;23(7):469–479. doi:10.1097/MCA.0b013e3283587804
23. Bax JJ, Poldermans D, Elhendy A, et al. Improvement of left ventricular ejection fraction, heart failure symptoms and prognosis after revascularization in patients with chronic coronary artery disease and viable myocardium detected by dobutamine stress echocardiography. J Am Coll Cardiol. 1999;34(1):163–169. doi:10.1016/S0735-1097(99)00157-6
24. Funaro S, La Torre G, Madonna M, et al. Incidence, determinants, and prognostic value of reverse left ventricular remodelling after primary percutaneous coronary intervention: results of the Acute Myocardial Infarction Contrast Imaging (AMICI) multicenter study. Eur Heart J. 2009;30(5):566–575. doi:10.1093/eurheartj/ehn529
25. Rizzello V, Poldermans D, Biagini E, et al. Prognosis of patients with ischaemic cardiomyopathy after coronary revascularisation: relation to viability and improvement in left ventricular ejection fraction. Heart. 2009;95(15):1273–1277. doi:10.1136/hrt.2008.163972
26. Yoo JS, Kim JB, Jung SH, Choo SJ, Chung CH, Lee JW. Coronary artery bypass grafting in patients with left ventricular dysfunction: predictors of long-term survival and impact of surgical strategies. Int J Cardiol. 2013;168(6):5316–5322. doi:10.1016/j.ijcard.2013.08.009
27. Panza JA, Velazquez EJ, She L, et al. Extent of coronary and myocardial disease and benefit from surgical revascularization in ischemic LV dysfunction [Corrected]. J Am Coll Cardiol. 2014;64(6):553–561. doi:10.1016/j.jacc.2014.04.064
28. Cuocolo A, Petretta M, Nicolai E, et al. Successful coronary revascularization improves prognosis in patients with previous myocardial infarction and evidence of viable myocardium at thallium-201 imaging. Eur J Nucl Med. 1998;25(1):60–68. doi:10.1007/s002590050195
29. Ragosta M, Beller GA, Watson DD, Kaul S, Gimple LW. Quantitative planar rest-redistribution 201Tl imaging in detection of myocardial viability and prediction of improvement in left ventricular function after coronary bypass surgery in patients with severely depressed left ventricular function. Circulation. 1993;87(5):1630–1641. doi:10.1161/01.CIR.87.5.1630
30. Wang S, Borah BJ, Cheng S, et al. Diabetes associated with greater ejection fraction improvement after revascularization in patients with reduced ejection fraction. Front Cardiovasc Med. 2021;8:751474. doi:10.3389/fcvm.2021.751474
31. Zhang Y, Guallar E, Blasco-Colmenares E, et al. Changes in follow-up left ventricular ejection fraction associated with outcomes in primary prevention implantable cardioverter-defibrillator and cardiac resynchronization therapy device recipients. J Am Coll Cardiol. 2015;66(5):524–531. doi:10.1016/j.jacc.2015.05.057
32. Russo AM, Stainback RF, Bailey SR, et al. ACCF/HRS/AHA/ASE/HFSA/SCAI/SCCT/SCMR 2013 appropriate use criteria for implantable cardioverter-defibrillators and cardiac resynchronization therapy: a report of the American College of Cardiology Foundation appropriate use criteria task force, Heart Rhythm Society, American Heart Association, American Society of Echocardiography, Heart Failure Society of America, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2013;61(12):1318–1368. doi:10.1016/j.jacc.2012.12.017
33. Stankovic I, Belmans A, Prinz C, et al. The association of volumetric response and long-term survival after cardiac resynchronization therapy. Eur Heart J Cardiovasc Imaging. 2017;18(10):1109–1117. doi:10.1093/ehjci/jex188
34. Stankovic I, Prinz C, Ciarka A, et al. Relationship of visually assessed apical rocking and septal flash to response and long-term survival following cardiac resynchronization therapy (PREDICT-CRT). Eur Heart J Cardiovasc Imaging. 2016;17(3):262–269. doi:10.1093/ehjci/jev288
35. Virk SA, Tian DH, Sriravindrarajah A, et al. Mitral valve surgery and coronary artery bypass grafting for moderate-to-severe ischemic mitral regurgitation: meta-analysis of clinical and echocardiographic outcomes. J Thorac Cardiovasc Surg. 2017;154(1):127–136. doi:10.1016/j.jtcvs.2017.03.039
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.