Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Exploring the Presence of Implicit Bias Amongst Healthcare Professionals Who Refer Individuals Living with COPD to Pulmonary Rehabilitation with a Specific Focus Upon Smoking and Exercise
Authors Barradell AC , Robertson N, Houchen-Wolloff L, Singh SJ
Received 9 September 2022
Accepted for publication 30 April 2023
Published 21 June 2023 Volume 2023:18 Pages 1287—1299
DOI https://doi.org/10.2147/COPD.S389379
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Amy C Barradell,1– 3 Noelle Robertson,4 Linzy Houchen-Wolloff,1,2 Sally J Singh1,2
1Department of Respiratory Sciences, University of Leicester, Leicester, UK; 2Centre for Exercise and Rehabilitation Science, University Hospitals of Leicester NHS Trust, Leicester, UK; 3Multiple Long Term Conditions, National Institute for Health Research (NIHR) Applied Research Collaboration (East Midlands), Leicester, UK; 4Department of Neuroscience, University of Leicester, Leicester, UK
Correspondence: Amy C Barradell, Email [email protected]
Background: We are developing a shared decision-making intervention for individuals with COPD who are deciding between Pulmonary Rehabilitation (PR) programme options. Previously, we identified Healthcare Professional (HCP) beliefs about the characteristics of COPD individuals as a barrier to PR conversations. Beliefs can lead to implicit biases which influence behaviour. To inform our shared decision-making intervention, we aimed to measure the presence of implicit bias amongst HCPs who refer individuals with COPD to PR.
Methods: We utilised the Implicit Association Test to measure HCPs response times when categorising words related to smoking or exercise (eg stub, run) to matching concepts or evaluations of concepts (eg “smoking, unpleasant” or “exercise, pleasant”) and unmatching concepts or evaluations of concepts (eg “smoking, pleasant” or “exercise, unpleasant”). We approached HCPs across the UK. Following consent, we collected demographic data and then administered the test. The primary outcome was the standardised mean difference in response times from the matching and unmatching categorisations (D4-score), measured using a one-sample Wilcoxon Signed Rank Test. We explored the relationship between HCP demographics and their D4-scores using Spearman Rho correlation analysis and logistic regression.
Results: Of 124 HCPs screened, 104 (83.9%) consented. Demographic data were available for 88 (84.6%). About 68.2% were female and most (28.4%) were in the 45– 54 years age category. Test data were available for 69 (66.3%) participants. D4-scores ranged from 0.99 to 2.64 indicating implicit favouring of matching categorisation (MD-score = 1.69, SDD-score = 0.38, 95% CID-score 1.60– 1.78, p < 0.05). This was significantly different from zero, z = − 7.20, p < 0.05, with a large effect size (r = 0.61, (28)). No demographic predictors of implicit bias were identifiable.
Conclusion: HCPs demonstrated negative bias towards smoking and positive bias towards exercising. Since implicit bias impacts behaviour, we plan to develop intervention components (eg decision coaching training) to enable HCPs to fully and impartially support shared decision-making for a menu of PR options.
Keywords: implicit bias, COPD, healthcare professionals, pulmonary rehabilitation
Introduction
Individuals living with chronic obstructive pulmonary disease (COPD) frequently experience symptoms of breathlessness, cough, wheeze, and the production of excess sputum.1 Due to its chronic and progressive nature, individuals often experience significant changes to their physical, social and mental wellbeing.2–4
A holistic management strategy is Pulmonary Rehabilitation (PR); a behaviour change intervention involving tailored and progressive exercise training and disease education. The programme is evidenced to improve individuals’ breathlessness, emotional functioning, exercise capacity and perceived sense of control over their health.5 However, despite its health benefits, uptake to and engagement with the programme is below the target proposed by national guidelines.6
To tackle some of the barriers to engagement in PR, numerous remote options have been developed and evaluated, for example, a PR manual with telephone support from healthcare professionals (HCPs), SPACE for COPD,7,8 and an online PR programme, myPR.9 These options are deemed non-inferior to traditional PR8,9 and therefore facilitate choice when individuals are referred to the service. Despite the availability of alternative programmes, national data indicate that 97.9% of individuals are enrolled onto a traditional centre-based programme.10
To support informed and value-based PR decision-making between individuals living with COPD and healthcare professionals (HCPs), we are developing and evaluating a shared decision-making intervention.11 Shared decision-making encourages HCPs and individuals to jointly share information about the available treatment options, deliberate between them, and then come to a decision which is personalised to the individuals’ needs and preferences.12 Importantly, it requires HCPs to take a non-directive approach offering each available treatment option in turn and without bias towards one over the other. The intervention development process involves a comprehensive needs analysis to understand the decisional needs of individuals. We began to explore this via interviews with individuals living with COPD and HCPs who refer to our PR service.13 We found that offering a choice of programmes creates increased opportunity for individuals to engage in a programme which is acceptable and appropriate for them (ie that shared decision-making was an appropriate intervention). However, we also found that HCPs do not view the options as equal and often have a personal preference for traditional centre-based PR over remote options. HCPs also felt that certain characteristics associated with individuals living with COPD were a barrier to them accepting PR, for example, individuals’ negative beliefs and intentions towards exercise and self-management (ie continuing to smoke despite cessation advice from HCPs). These findings highlight strong HCP beliefs which, if expressed during PR conversations, would be incongruent with a shared decision-making approach. Beliefs stem from conscious (ie explicit) and unconscious (ie implicit) logical and rational appraisals of different life experiences. Within the unconscious mind lies a pool of thoughts, feelings, and memories which, without our knowledge, positively or negatively influence judgements, feelings, and behaviour.14 In time, these form systematic patterns of beliefs and preferences, known as biases, which may or may not be reasonable or accurate. These biases are known to consistently influence our behaviours.15 In the context of healthcare, there is evidence to show that HCPs have negative implicit biases for many individual characteristics, for example, disability, mental health, health behaviours (eg recreational drug use), weight, and socioeconomic status and these biases are frequently associated with a lower quality of patient care.16 What we do not know is if implicit biases also exist for specific characteristics associated with individuals living with COPD and therefore the potential impact these may have when HCPs undertake shared decision-making with an individual.
Due to the link between implicit bias and behaviour we aimed to measure the presence of implicit bias amongst HCPs who refer to PR. This would be used to inform the need for specific HCP components within our shared decision-making intervention development. This article adheres to the STROBE checklist;17 a tool to guide the report of observational research.
Methods
Study Design
This was a single centre, cross-sectional, observational study measuring the presence of HCPs implicit bias towards the characteristics of individuals living with COPD. Participants were recruited to the study for a single visit which they completed remotely using an online consent and test form.
Setting
This study was conducted within a university teaching hospital in the East Midlands. We recruited HCPs from the host site and around the UK. This research was given ethical approval by South Leicester – Research Ethics Committee, reference 21/EM/0084 and is registered on Clinical Trials.gov (NCT04990180). All research practices complied with the Declaration of Helsinki.18
Participants
Eligibility Criteria
Eligible participants were those who were happy to provide informed consent to participate, practiced healthcare in the UK, and referred individuals living with COPD to PR.
Participant Recruitment
At the host site, respiratory leads were approached and asked to disseminate an electronic study advert and participant information sheet to their colleagues. To reach a wider, national audience, the study advert and participant information sheet was shared with professional groups (eg Primary Care Respiratory Society, Association of Chartered Physiotherapists in Respiratory Care, Royal College of Occupational Therapists, Royal College of Nursing) and posted on Twitter. Participants were able to express interest by clicking a weblink in the study advert. By doing this, they accessed a Google Form screening tool which assessed their eligibility. Any participant who did not meet the eligibility criteria received an automatic notification to thank them for their interest in the study and inform them of their ineligibility. Those eligible were directed to the electronic consent form where participants recorded their name, date of enrolment and electronic signature. Consent was obtained and documented in accordance with the host site’s consent standard operating procedure and Good Clinical Practice guidelines.19 Following completion, they were then able to click the weblink to access the online test platform.
The online test platform began with a baseline questionnaire which captured participant demographics including their age, gender, smoking status, frequency of exercise engagement, profession, and number of years having worked with individuals living with COPD. Once completed, participants were prompted to complete the Implicit Association Test.
The Implicit Association Test (IAT)
The IAT is a measure of implicit associations between concepts (eg specific characteristics) and evaluations of those concepts (eg pleasant, unpleasant).20 It measures the difference in association between two target concepts. Participants are presented with word stimuli which they are asked to categorise as quickly as possible into those predefined concepts or evaluations of concepts. It assumes that those which are implicitly associated are easier and therefore quicker to categorise. The test uses participants’ reaction times as a measure of the strength of association (ie the shorter the time to categorise the word stimuli the stronger the association and vice versa).
This IAT was a computerised and simplified IAT.20 Delivery of this was facilitated by PsyToolkit’s online platform.21,22 The two chosen characteristics were smoking and exercise because HCPs have previously identified these characteristics as positive and negative influencers of individuals’ engagement with PR.13 The evaluations of the concepts were pleasant and unpleasant. The IAT was framed to encourage HCPs perceptions of the concepts. The chosen word stimuli were those used by previous IAT studies for smoking23–25 and exercise.26–29 The test required sixteen additional word stimuli and so all authors contributed to the systematic selection of words which captured a broader sense of the smoking and exercise concepts (eg craving, cough, and drag for smoking and healthy, energising, and restorative for exercise). The pleasant and unpleasant word stimuli were those used in the original IAT.20 The full list of IAT word stimuli is provided in the Supplementary Material (Supplementary Tables S1–S3).
Our IAT contained five test blocks. Blocks one, two, and four were training blocks to allow participants to practice the categorisation process. In blocks one and four, participants were presented with a concept (ie exercise, smoking) categorisation task. In block 2, participants were presented with an evaluation of concept (pleasant, unpleasant) categorisation task. They were required to categorise the word stimuli presented in the middle of the screen to the associated concept/evaluation of concept by pressing the keyboard letter “e” for left and “i” for right. After each answer, a happy or sad face appeared to feedback whether the categorisation was correct or not.
Blocks three and five were the experimental blocks. In one of these blocks, participants were asked to categorise word stimuli (eg stub) with a concept (eg smoking) and an evaluation of the concept (eg unpleasant) using the “e” and “i” keyboard letters. This is an example of congruent categorisation (Figure 1).
 |
Figure 1 Experimental block (congruent categorisation). |
The other experimental block asked participants to repeat the task, but this time participants saw the concept “exercise” above the evaluation of the concept, “unpleasant”, and the concept “smoking” above the evaluation of the concept, “pleasant.” Participants were asked to categorise the word stimuli (eg staining) with a concept (eg smoking) and an evaluation of the concept (eg pleasant) using the “e” and “i” keyboard letters. This is an example of incongruent categorisation (Figure 2).
 |
Figure 2 Experimental block (incongruent categorisation). |
The block order was randomly assigned to ensure training effects were minimised. Participants were required to complete all five test blocks (ie all of the training and the congruent and incongruent categorisations). At the end of the test, they saw a final screen which informed them the test was complete and thanked them for taking part in the study.
Sample Size
To capture a representative sample of HCPs involved in the care of individuals living with COPD, we calculated a sample size using the online platform Raosoft.30 This tool is widely used to calculate sample sizes for surveys. The calculation assumed a margin of error of 5%, a confidence level of 95%, a population size of 128 (ie the number of HCPs who refer individuals with COPD to PR at the host site), and a response distribution of 50%. The calculated sample size was 97 participants to consent to the study.
Data Analysis
Data Preparation
Only complete IAT data sets were eligible for analysis. Data was downloaded from the PsyToolkit test portal21,22 and then uploaded to IBM SPSS (V26) for statistical analysis. A random 10% sample of the IAT datasets was reviewed to ensure accuracy in data entry.
Data were prepared as per the recommendations of Greenwald et al for the improved scoring algorithm using the standardised mean difference calculation, D4.31 This included the retention of all data from the congruent and incongruent categorisation blocks, to recode response latencies <300ms to 300ms and >3000ms to 3000ms (this was automatically conducted by the PsyTookit test portal) and to compute the mean of correct response latencies for congruent and incongruent word stimuli, and to replace each incorrect response with the block mean + 600ms. Incorrect responses were categorisation errors or no response in the time limit (ie 3000ms).
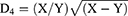
The primary outcome was the difference in response latencies of the experimental blocks. The strength of association is measured by the standardised mean difference score of a participant’s congruent categorisation and their incongruent categorisation. This is presented as a D4-score. The D4-scores were calculated using the algorithm described by Greenwald et al31 by computing a new variable in SPSS:
This formula involves averaging the resulting values for each congruent and incongruent categorisation block (ie the experimental blocks) and computing the difference between them. X is the mean of congruent categorisation latencies, and Y is the mean of incongruent categorisation latencies. Where the X value was smaller than the Y value, the values were reversed. A positive D4-score indicated an implicit preference for congruent categorisation, a negative D4-score indicated an implicit preference incongruent categorisation, and a D4-score of 0 indicated a lack of implicit preference in either direction.
Statistical Analysis
Fisher’s Exact Probability Test was used to explore differences in participant demographics from those who completed the IAT to those who did not. A one sample Wilcoxon Signed Rank Test was conducted to evaluate the experimental hypothesis. The null hypothesis was that D4 = 0. The experimental hypothesis was that D4 ≠ 0.
Spearman Rho correlation analysis was conducted to explore the relationship between the participants’ demographics and their D4-scores. Logistic regression was conducted to understand univariate and multivariable associations between the participant demographics and their response latency. As response latency is a continuous variable, D4-scores were converted to categorical variables using the following criteria: D4-score <1.69msecs = to indicate bias lower than the mean, D4-score ≥1.69msecs = to indicate bias greater than or equal to the mean.
It was not possible to identify a similar procedure previously undertaken in the literature and so it was decided that to provide a meaningful result the data should be separated into scores below and scores equal to or above the population mean. This was also conducted for the population median (1.68), and we report any significantly different results.
The threshold for significance was set at p < 0.05.
Results
Data was collected between June 2021 and April 2022. Of the 124 HCPs screened, 20 (16.1%) were excluded. A total of 104 participants (83.9%) consented to participate. Demographic data were available for 88 participants (84.6%), and IAT data were available for 69 participants (66.3%; Figure 3).
 |
Figure 3 Participant flow diagram. Abbreviations: UK, United Kingdom; PR, Pulmonary Rehabilitation; IAT, Implicit Association Test. |
Participant demographics are displayed in Table 1. “Other” professions included a Lab Technician, Clinical Pharmacist, Speech and Language Therapist, Occupational Therapist, Paramedic, and one who did not disclose their profession. There were no significant differences between those who completed the IAT and those who did not.
 |
Table 1 Participant Demographics |
IAT Results
Data Preparation
Incorrect Responses
Prior to replacing the incorrect responses, the mean (SD) number of incorrect responses for congruent word pairings was 1.2 (1.7) and for incongruent word pairings was 3.9 (3.2).
Amending the Incorrect Responses
The mean for all correct congruent categorisation was 812.53ms and for all correct incongruent categorisation was 1081.70ms. As per the recommendations by Greenwald (2003) for the improved scoring algorithm, 600ms was added to each of these figures and was used to replace incorrect responses.
Primary Outcome: Response Latency
The mean (SD) time to complete the IAT was 17.4 (14.17) minutes. The mean response latency for congruent categorisation (mean (SD) = 840.5ms (190.1)) and incongruent categorisation (mean (SD) = 1164.6ms (185.8)) is presented in Figure 4.
 |
Figure 4 Response latencies for congruent and incongruent word pairings. |
D-scores ranged from 0.99 to 2.64 indicating all HCPs had implicit favouring of congruent categorisation (MD-score = 1.69, SDD-score = 0.38, 95% CID-score 1.60–1.78, p < 0.05). This was significantly different from zero, z = −7.20, p < 0.05, with a large effect size (r = 0.61),32 meaning there was a statistically significant difference between congruent and incongruent categorisation.
Since only 69 (66.3%) out of 104 recruited participants completed the IAT, a post-hoc power calculation was conducted to examine the reliability of these findings. The mean (SD) D-score from Waters et al’s study was used to calculate this (MD-score = 0.49, SDD-score = 0.73).33 This study involved an IAT measuring smokers’ implicit associations to smoking. The scores from Water et al’s study and this current study were input into the ClinCalc post-hoc power calculator34 along with the study group design (ie two independent study groups), the nature of the primary endpoint (ie continuous), the number of participants (ie for Waters et al’s study, n = 57, for the current study, n = 69), and error rate (ie 0.05). The calculation indicated that the current study results had 100% power.
Sub-Group Analysis
The Spearman Rho’s correlational analysis identified statistically significant associations between participants' age and their professional status and number of years they had worked with COPD individuals (Table 2). There were no other significant correlations.
 |
Table 2 Correlation Analysis for Participant Demographics |
Univariate logistic regression was performed to ascertain the effects of age, gender, professional status, years worked with COPD individuals, exercise, and smoking status on the likelihood that participants have lower or higher than average D-scores using the population mean as the cut-offs (<1.69 and ≥1.69). The only statistically significant model was that containing gender, χ2 = 12.19, p < 0.05, indicating the model was able to distinguish between participants who had a D-score above or below the mean. The model explained between 16.2% (Cox and Snell R square35) and 21.6% (Nagelkerke R square36) of the variance in D-scores and correctly classified 69.6% of cases. However, none of the gender categories were significantly able to distinguish between participants (OR = 0, 95% CI = 0.00–0.00, p > 0.05).
The professional status model was not significant, χ2 = 5.39, p > 0.05; however, the sub-category “Doctor” was significantly able to distinguish between participants who had a D-score above or below the mean (OR = 4.29, 95% CI = 1.14–16.18, p < 0.05). The odds ratio indicated that if a HCP was a Doctor, they were 4.29 times more likely to have a D-score above the population mean when all other factors are equal. However, when the population median was used, the model and all variables became insignificant χ2 = 5.67, p > 0.05. No other univariate models or sub-categories were significant.
Adjusted multivariable regression analysis was conducted to explore the effects of gender and professional status on participants’ D-scores. This model was statistically significant, χ2 = 14.45, p < 0.05 and explained between 18.9% (Cox and Snell R square) and 25.2% (Nagelkerke R square) of the variance in D-scores and correctly classified 69.6% of cases. However, as shown in Table 3, none of the independent variables made a statistically significant contribution to the model. When replicated using the population median, the model and all variables became insignificant, χ2 = 10.98, p > 0.05.
 |
Table 3 Logistic Regression Analysis of D-Scores |
Discussions
The results indicate that HCPs who refer individuals with COPD to PR have implicit bias; they demonstrate a significant preference when associating exercise and pleasant attributes and smoking and unpleasant attributes. This suggests they have negative attitudes towards smoking and positive attitudes towards exercising. Due to the strong correlation between implicit bias and behaviour,14,15 this may explain disparity in HCPs PR referral behaviours when posed with individuals expressing these characteristics Due to the considerable heterogeneity of the results, no demographic predictors of implicit bias were identifiable.
Whilst implicit bias has been identified amongst HCPs previously, this is the first study to show that HCPs who refer individuals with COPD to PR have implicit bias for the characteristics smoking and exercising. Outside of healthcare, several studies using IATs have previously identified that university students have implicit negative biases towards smoking, irrespective of their own smoking status23,24 which the authors postulate may be due to smoking being a stigmatised behaviour. Additionally, university students have also shown implicit positive bias towards exercise26,37 and to a greater extent if they identify themselves as regular exercisers.27 The present data is unable to rule out the possibility that other variables may predict HCP attitudes towards smoking and exercise, however, a more balanced population sample would be required to address this (ie greater sample sizes for smokers and those within the differing exercise frequency categories). It may also be worth exploring and comparing the presence of bias between non-referrers and referrers to PR.
Returning to the healthcare setting, and as previously mentioned, HCPs have demonstrated significant implicit bias for multiple characteristics, namely socioeconomic status and disability which resulted in lower quality of patient care.16 Whilst HCPs in that review were not solely delivering care to individuals living with COPD, it does shed some light on why HCPs may hold biases towards them. To exemplify, the prevalence of COPD is higher in those with lower socioeconomic status38 and those with lower socioeconomic status are four times more likely to be smokers,39 significantly more likely to engage in sedentary behaviours40 and twice as likely to suffer disability, morbidity and mortality.41,42 Additionally, we previously found that HCPs believe smoking and exercise behaviours in individuals with COPD can create barriers and facilitators to conversations about PR.13 In terms of the potential impact on HCP behaviour, it is known that ex-smokers have 41% higher odds of being referred to PR than current smokers43 which could be explained by individual choice, HCP bias or a combination of both. The relationship between individuals’ socioeconomic status and HCP bias is therefore complex and requires more investigation. We can merely conclude that the influence of characteristics (eg smoking, exercising) is a piece of this complex puzzle.
Knowing that HCPs have implicit bias towards the characteristics smoking and exercising, it is likely that when they are presented with patients expressing these health behaviours, they change their behaviour accordingly.14,15 This means that when implementing shared decision-making into PR conversations with individuals with COPD, they may not have the same standardised informed and value-based discussions with all individuals. This is incongruent with a shared decision-making approach. To provide equality in our shared decision-making intervention delivery it is worth considering possible solutions. A systematic review of interventions aimed at reducing implicit bias and stereotypes was conducted.44 Whilst there were no interventions specifically to target bias towards the characteristics smoking and exercising, the review did conclude that there may be value in giving HCPs instructions to implement intentional strategies to override or suppress bias, exposure to an exemplar who contradicts the stereotype, tasks which minimise the barriers between themselves and an outgroup, tasks to increase counter-stereotype associations, and tasks to induce emotion. One intervention which used several of these techniques was explored in a study by Sukhera et al.45 They interviewed paediatric physicians following their completion of a mental illness IAT. The authors found that when physicians recognised their idealised attitudes did not correlate with their actual attitudes, this created tension which they felt could be used as a learning tool to stimulate recognition and action to change their implicit bias. This suggests that the use of targeted interventions may be useful to lessen or override HCPs bias. We have therefore feel it would be worth embedding targeted components within our shared decision-making intervention, namely a decision coaching training session for HCPs and a consultation prompt.11
Strengths and Limitations
These findings are the first to indicate that HCPs demonstrate implicit bias towards specific characteristics associated with individuals living with COPD. They therefore provide an argument for the implementation of targeted interventions to support HCPs in overcoming or overriding their bias, so they can fully engage in shared decision-making between the menu of PR options. The IAT is unlike explicit measures of bias as it does not need to directly probe individuals. This means it is less affected by individuals’ conscious intentions, deliberate mental processing and thereby social desirability.46,47 However, the IAT is not a definitive method to diagnose implicit bias, it is merely an indication. The main limitation of the IAT is that the methodology cannot obtain conclusive evidence of bias on the proposed construct(s). The constructs measured here have been measured previously but never together and so there is no data on the internal validity or reliability of this IAT. Reliability and validity of IATs are often critiqued, particularly regarding the impacts of measurement artefacts (eg responding via a computer screen), the lack of clarity in the underlying cognitive processes involved in responding to the test, and variables which may confound individuals’ responses.47–49 It has the best predictive validity for highly socially sensitive topics (eg racial bias), outperforming self-reported measures.50 One may hypothesise smoking behaviours to be a highly socially sensitive topic due to its associated stigma, although it may be a stretch to suggest exercise behaviours are the same. The original IAT authors recommend the use of self-reported measures in conjunction with an IAT to predict individuals’ behaviour more accurately. Therefore, these results should be reviewed in tandem with explicit measures of bias (eg interviews or standardised questionnaires completed by HCPs).
One further consideration is that we explored just two concepts (smoking and exercising) when others could well have been considered. Our justification was that we had previously identified HCP beliefs about smoking and exercising influenced PR conversations and therefore wanted to explore the presence of bias within these concepts.
Considering the study population, whilst there were similarities between completers and those who did not complete the IAT, the results are not generalisable. The sample only contained UK HCPs and was predominantly female. It also incurred a high dropout rate (27.5%) for those who consented but did not complete the IAT. However reassuringly, the post-hoc power calculation indicated that the results retained 100% power.
Conclusions
These results demonstrate the presence of implicit negative bias towards smoking and implicit positive bias towards exercising amongst HCPs who refer individuals with COPD to PR. Due to the correlation between beliefs and behaviour, this provides a rationale for the inclusion of components targeting HCP communication (eg decision coaching training, consultation prompt) in our shared decision-making intervention to enable HCPs to fully and impartially support individuals’ decision-making for PR.
Data Sharing Statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Funding
This study contributes to ACB’s PhD. It is funded by the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC: East Midlands) and the Centre for Exercise and Rehabilitation Science (CERS) at the University Hospitals of Leicester NHS Trust. SJS is ACB’s senior PhD supervisor and a Senior Investigator for the NIHR. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Disclosure
Professor Sally J Singh reports grants from NIHR, grants from Wellcome, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. GOLD. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease; 2020. Available from: www.goldcopd.org.
2. Yohannes AM, Alexopoulos GS. Depression and anxiety in patients with COPD. Vol. 23, European respiratory review. European Respiratory Society; 2014:345–349. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4523084/.
3. Alahmari AD, Patel ARC, Kowlessar BS, et al. Daily activity during stability and exacerbation of chronic obstructive pulmonary disease. BMC Pulm Med. 2014;14(1):98. doi:10.1186/1471-2466-14-98
4. Grønseth R, Erdal M, Tan WC, et al. Unemployment in chronic airflow obstruction around the world: results from the BOLD study. Eur Respir J. 2017;50(3):1700499. doi:10.1183/13993003.00499-2017
5. Mccarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2. doi:10.1002/14651858.CD006927.pub4
6. NACAP. National COPD Audit Programme: Pulmonary Rehabilitation: Time to Breathe Better. NACAP; 2015.
7. Wagg K, Warrington V, Apps L, et al. A self-management programme of activity coping and education (SPACE) for COPD: 6 week results from a randomised controlled trial. Eur Respir J. 2012;40(Suppl 56):1.
8. Horton E, Mitchell K, Johnson-Warrington V, Apps L, Young H, Singh S. Results of the SPACE FOR COPD programme in comparison to pulmonary rehabilitation at 6 months. Eur Respir J. 2014;44(Suppl 58):1.
9. Bourne S, DeVos R, North M, et al. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomised controlled trial. BMJ Open. 2017;7(7):e014580. doi:10.1136/bmjopen-2016-014580
10. NACAP. National asthma and COPD audit programme: pulmonary rehabilitation clinical and organisational audit report 2019; 2020.
11. Barradell AC, Singh SJ, Houchen-Wolloff L, Robertson N, Bekker HL, Singh S. A pulmonary rehabilitation shared decision-making intervention for patients living with COPD: PReSent: protocol for a feasibility study. ERJ Open Res. 2022;8(2):00645–2021. doi:10.1183/23120541.00645-2021
12. Charles C, Gafni WT. Shared decision-making in the medical encounter: what does it mean? (Or it takes at least two to tango). Soc Sci Med. 1997;44:681–692. doi:10.1016/S0277-9536(96)00221-3
13. Barradell A, Bourne C, Alkhathlan B, Larkin M, Singh S. A qualitative assessment of the pulmonary rehabilitation decision-making needs of patients living with COPD. NPJ Prim Care Respir Med. 2022;32(1):1–11. doi:10.1038/s41533-022-00285-9
14. Wilson S. Psi, perception without awareness, and false recognition. J Parapsychol. 2002;66(3):271–289.
15. Banaji MR, Greenwald AG, Bhaskar R, et al. Implicit Gender Stereotyping in Judgments of Fame for Providing Oppor-Tunities for Classroom Testing; and Coomi. BarghPerdue & Gurtman; 1995.
16. Fitzgerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19. doi:10.1186/s12910-017-0179-8
17. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi:10.1016/j.jclinepi.2007.11.008
18. WMA. WMA Declaration of Helsinki – ethical principles for medical research involving human subjects – WMA – the World Medical Association; 2013. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
19. HRA. Good clinical practice; 2020 Available from: https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/good-clinical-practice/.
20. Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–1480. doi:10.1037/0022-3514.74.6.1464
21. Stoet G. PsyToolkit: a software package for programming psychological experiments using Linux. Behav Res Methods. 2010;42(4):1096–1104. doi:10.3758/BRM.42.4.1096
22. Stoet G. PsyToolkit: a novel web-based method for running online questionnaires and reaction-time experiments. Teach Psychol. 2017;44(1):24–31. doi:10.1177/0098628316677643
23. Swanson JE, Rudman LA, Greenwald AG. Using the implicit association test to investigate attitude-behaviour consistency for stigmatised behaviour. Cogn Emot. 2001;15(2):207–230. doi:10.1080/02699930125706
24. Huijding J, De Jong PJ, Wiers RW, Verkooijen K. Implicit and explicit attitudes toward smoking in a smoking and a nonsmoking setting. Addict Behav. 2005;30(5):949–961. doi:10.1016/j.addbeh.2004.09.014
25. Bardin B, Perrissol S, Py J, Fos Y, Souchon N. Testing of a paper-and-pencil personalized single category implicit association test (SC-IAT-P). Int Rev Soc Psychol. 2016;29(1):31–44. doi:10.5334/irsp.35
26. Conroy DE, Hyde AL, Doerksen SE, Ribeiro NF. Implicit attitudes and explicit motivation prospectively predict physical activity. Ann Behav Med. 2010;39(2):112–118. doi:10.1007/s12160-010-9161-0
27. Berry TR, Spence JC, Clark ME. Exercise is in! Implicit exercise and sedentary-lifestyle bias held by in-groups. J Appl Soc Psychol. 2011;41(12):2985–2998. doi:10.1111/j.1559-1816.2011.00857.x
28. Forrest LN, Smith AR, Fussner LM, Dodd DR, Clerkin EM. Using implicit attitudes of exercise importance to predict explicit exercise dependence symptoms and exercise behaviors. Psychol Sport Exerc. 2016;22:91–97. doi:10.1016/j.psychsport.2015.06.006
29. Chevance G, Héraud N, Guerrieri A, Rebar A, Boiché J. Measuring implicit attitudes toward physical activity and sedentary behaviors: test-retest reliability of three scoring algorithms of the implicit association test and single category-implicit association test. Psychol Sport Exerc. 2017;31:70–78. doi:10.1016/j.psychsport.2017.04.007
30. Raosoft. Sample size calculator by Raosoft, Inc; 2004. Available from: http://www.raosoft.com/samplesize.html.
31. Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. an improved scoring algorithm; 2003. Available from: http://www.yale.edu/implicit/.
32. Cohen J. The effect size: r. In: Statistical Power Analysis for Behavioural Sciences.
33. Waters AJ, Carter BL, Robinson JD, Wetter DW, Lam CY, Cinciripini PM. Implicit attitudes to smoking are associated with craving and dependence. Drug Alcohol Depend. 2007;91(2–3):178. doi:10.1016/j.drugalcdep.2007.05.024
34. ClinCalc LLC. Post‐hoc power calculator; 2018. Available from: https://clincalc.com/stats/Power.aspx.
35. Cox DR, Snell EJ. Analysis of Binary Data.
36. Nagelkerke NJD. A note on a general definition of the coefficient of determination. Biometrika. 1991;78(3):691–692. doi:10.1093/biomet/78.3.691
37. Hyde AL, Doerksen SE, Ribeiro NF, Conroy DE. The independence of implicit and explicit attitudes toward physical activity: introspective access and attitudinal concordance. Psychol Sport Exerc. 2010;11(5):387–393. doi:10.1016/j.psychsport.2010.04.008
38. Snell N, Strachan D, Hubbard R, Gibson J, Gruffydd-Jones K, Jarrold I. S32 epidemiology of chronic obstructive pulmonary disease (COPD) in the UK: findings from the British lung foundation’s “respiratory health of the nation” project. Thorax. 2016;71(Suppl 3):A20.1–A20. doi:10.1136/thoraxjnl-2016-209333.38
39. Hiscock R, Bauld L, Amos A, Platt S. Smoking and socioeconomic status in England: the rise of the never smoker and the disadvantaged smoker. J Public Health (Bangkok). 2012;34(3):390–396. doi:10.1093/pubmed/fds012
40. Stevens D, Andreou P, Rainham D. Environmental correlates of physical activity, sedentary behavior, and self-rated health in chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2022;42(3):190–195. doi:10.1097/HCR.0000000000000628
41. Gershon AS, Dolmage TE, Stephenson A, Jackson B. Chronic obstructive pulmonary disease and SocioEconomic status: a systematic review. COPD. 2012;9(3):216–226. doi:10.3109/154125552011648030
42. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2163–2196. doi:10.1016/S0140-6736(12)61729-2
43. Stone PW, Hickman K, Steiner MC, Roberts CM, Quint JK, Singh SJ. Predictors of referral to pulmonary rehabilitation from UK primary care. Int J Chron Obstruct Pulmon Dis. 2020;15:2941. doi:10.2147/COPD.S273336
44. Fitzgerald C, Martin A, Berner D, Hurst S. Interventions designed to reduce implicit prejudices and implicit stereotypes in real world contexts: a systematic review. BMC Psychol. 2019;7(1):1–12. doi:10.1186/s40359-019-0299-7
45. Sukhera J, Milne A, Teunissen PW, Lingard L, Watling C. The actual versus idealized self: exploring responses to feedback about implicit bias in health professionals. Acad Med. 2018;93(4):623–629. doi:10.1097/ACM.0000000000002006
46. Kim DY. Voluntary controllability of the implicit association test (IAT). Soc Psychol Q. 2003;66(1):83–96. doi:10.2307/3090143
47. Nosek BA, Greenwald AG, Banaji MR. The implicit association test at age 7: a methodological and conceptual review. - PsycNET. In: Social Psychology and the Unconscious: The Automaticity of Higher Mental Processes. Psychology Press; 2007:265–292.
48. Rezaei AR. Validity and reliability of the IAT: measuring gender and ethnic stereotypes. Comput Human Behav. 2011;27(5):1937–1941. doi:10.1016/j.chb.2011.04.018
49. Schimmack U. The implicit association test: a method in search of a construct. Perspect Psychol Sci. 2019;16(2):396–414. doi:10.1177/1745691619863798
50. Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41. doi:10.1037/a0015575
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.