Back to Journals » Advances in Medical Education and Practice » Volume 15
Exploring Perceptions and Practices of Interprofessional Shared Decision-Making Education in Palliative Care Settings
Authors Sultan L , de Jong N , Alsaywid B, Khan MA , de Nooijer J
Received 16 November 2023
Accepted for publication 31 March 2024
Published 6 April 2024 Volume 2024:15 Pages 281—291
DOI https://doi.org/10.2147/AMEP.S450166
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Lama Sultan,1,2 Nynke de Jong,3 Basim Alsaywid,4,5 Muhammad Anwar Khan,6 Jascha de Nooijer7
1Department of Clinical Nutrition, Ministry of National Guard Health Affairs, King Abdulaziz Medical City, Jeddah, KSA, Saudi Arabia; 2School of Health Professions Education, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, Netherlands; 3Department of Health Services Research, School of Health Professions Education, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, NL, Saudi Arabia; 4Urology Department, King Faisal Specialist Hospital & Research Center, Riyadh, KSA, Saudi Arabia; 5Education and Research Skills Directory, Saudi National Institute of Health, Riyadh, KSA, Saudi Arabia; 6College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Jeddah, KSA, Saudi Arabia; 7Department of Health Promotion, School of Health Professions Education, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, Netherlands
Correspondence: Lama Sultan, Department of Clinical Nutrition, Ministry of National Guard Health Affairs- Jeddah, King Abdulaziz Medical City, Mail Code 6660, P.O. Box.9515, Jeddah, 21423, Kingdom of Saudi Arabia, Tel +966553343478, Email [email protected]; [email protected]
Background: Palliative care teams provide support to patients and their caregivers during terminal illness, which requires interprofessional collaboration. One of the foundational skills is to assist patients with decision-making. This can be facilitated through interprofessional shared decision-making (IP-SDM). So far, IP-SDM education frameworks have only been used to a limited extent in the area of palliative care.
Aim: This study aims to explore perceptions and practices of faculty members, health professionals, and students toward IP-SDM education in palliative care and to indicate associated factors to implement an IP-SDM in undergraduate health professions education in palliative care settings.
Methods: We used a cross-sectional study design in which the data was obtained via an online self-administered questionnaire adapted from existing validated tools. The questionnaire was distributed to faculty members and health professionals (n = 125) and students (n = 334) at King Abdulaziz Medical City in Jeddah, Saudi Arabia. The sampling technique was a non-probability convenience sampling. Bivariate statistics, such as independent sample t-tests, one-way ANOVA, correlation coefficient, and linear multiple regression were conducted.
Findings: The response rate was 54% (85 faculty members and health professionals and 164 students). Perceptions on IP-SDM did not differ between participants. From those who had previous experience with IP-SDM, the mean practices score was slightly higher for faculty members and health professionals (M = 83.1, SD = 15.9) than for students (M = 74.1, SD = 11.5), which was significant (p < 0.05). Factors such as gender, age, discipline, nationality, level of education, years of study, and previous experience that were associated with perceptions and practices were varied among participants.
Conclusion: The findings show high levels of perception with low levels of practice of IP-SDM in palliative care. Other factors that could be associated with the topic should be addressed in further studies.
Keywords: health professions education, interprofessional shared decision-making, palliative care
Introduction
Shared decision-making (SDM) is a process of integrating both the best available evidence and patients’ values and preferences in the clinical decision-making process, in which patients, caregivers, and health care teams discuss decisions regarding patient care.1 It is a continuous process due to changes in patients’ preferences, goals of care, and health conditions.2 SDM is essential with respect to palliative care due to complex medical care options and high emotional distress.3 Thus, effective collaboration in SDM is essential between health care professionals, patients, and caregivers. This can be facilitated through an interprofessional shared decision-making (IP-SDM) approach. Indeed, making a decision with palliative care patients is sometimes challenging because patients and their caregivers face many difficult decisions regarding a wide range of issues. For example, decisions needed for cardiopulmonary resuscitation, withholding or withdrawing therapies, artificial nutrition, or use of opioid and symptoms treatment.4 Caregivers are responsible for making decisions for patients who cannot communicate due to their illness.5 Disagreement on these decisions can cause conflicts with the palliative care team because of barriers, such as lack of communication and collaboration skills that could inhibit teamwork effectiveness.6 Thus, effective communication is essential in a palliative care settings, whereby a palliative care unit provides palliative care as a component of the overall care. The effect of SDM in palliative care has an impact on patients’ outcomes, including better quality of life, symptoms management, patient satisfaction, and less caregiver distress.7
Education in palliative care varies widely and internationally due to the lack of teaching staff,8 pressure on curricula,8 and lack of clinical context for education.9,10 Unfortunately, many physicians and other health care providers are graduating without having received adequate training in palliative care.11 Palliative care education in nursing and allied health professions is often covered in isolated lectures.12 Furthermore, new graduates in health professions reported insufficient experience and feel unprepared in the area of palliative care.13 Several schools lack a curriculum for palliative care education in health professions.14 The lack of interprofessional training during undergraduate education inhibits preparedness for collaborating in interprofessional teams.15 Yet, palliative care provides an appropriate setting for an interprofessional approach.16 The majority of interprofessional education (IPE)17 in palliative care settings offer workshops, training sessions, elective courses, or short seminars and not necessarily rotating in clinical settings, because undergraduate are not participating in rotations yet. The use of IPE brings together students from different health professions to learn with, from, and about each other.18 IPE is a promising approach in undergraduate health profession programs for developing interprofessional collaboration practices.19 Moreover, SDM is often part of the competencies acquired as a result of IPE.20 To explore the feasibility of an IP-SDM intervention, we interviewed deans, faculty members, and health profession students and found there is a high demand for IP-SDM education in palliative care but that staff did not always feel prepared for IPE or IP-SDM.21 This was also found in other studies.22–25 To further explore the feasibility of an intervention for IP-SDM in undergraduate health professions education in palliative care in the context of Saudi Arabia, in this study we aim to identify the perceptions and practices toward engaging in IP-SDM in palliative care and the factors associated with faculty members, health professionals, and students. Because the Saudi Arabian context is framed by cultural bounds and religious constraints in comparison to other contexts, this study might help in promoting diversity in research and in developing culturally competent health care professionals.
Methods
Study Setting
This study was conducted at the Oncology and Palliative Care Department at King Abdulaziz Medical City (KAMC) in the Ministry of National Guard Health Affairs (MNG-HA) in Jeddah, Saudi Arabia, which is a 751-bed hospital serving Ministry of National Guard employees and their families. Moreover, the study was also conducted at King Saud bin Abdul-Aziz University for Health Sciences (KSAU-HS) in Jeddah, Saudi Arabia.
Participants and Procedures
The participants included were faculty members and undergraduate students in the College of Medicine, the College of Nursing, and the College of Applied Medical Sciences (Respiratory Therapy, Occupational Therapy, and Clinical Nutrition) and health professionals working with oncology and palliative patients at KAMC. Students enrolled in the 2021–2022 academic year, year 5 and 6 College of Medicine students, year 3 and 4 College of Nursing and Applied Medical Sciences students, and postgraduate students of health professions (including interns, residents, and fellows) were included. All participants who fulfilled the inclusion criteria were invited to participate in this research after the objectives of the study were explained. All participants with an interest to participate read and signed an online consent form. This study design encompasses a quantitative approach by using an observational and analytical cross-sectional study design. The online questionnaire was sent to 459 participants (125 faculty members and health professionals and 334 health profession students) with a follow-up reminder using the non-probability convenience sampling technique.
Measurement Tool
Data were obtained by distributing a self-administrated, online, close-ended questionnaire in English adapted from existing validated tools.26,27 Data were collected in January and February 2022. The questionnaire has two versions, one for faculty members and health professionals (Figure S1) and one for health profession students (Figure S2), which contained the following sections:
- Section one: demographic data for faculty members and health professionals included age; gender; nationality; educational level; discipline; job title; years of teaching experience and clinical experience; and experience with IPE, interprofessional collaboration (IPC), SDM, and palliative care. For students, we included age; gender; nationality; educational level; discipline; academic year; and experience with IPE, SDM, and palliative care. Also, there were questions about familiarity with the topic, including one question on a Likert-type scale between 1 and 10, where 1 = poor knowledge and 10 = excellent knowledge. The other questions were answered on a categorical scale and included more than one answering option.
- Section two: the assessment of faculty members’, health professionals’, and students’ perceptions to engage in IP-SDM in palliative care was carried out by adapting the CPD-Reaction questionnaire,26 which consists of 12 items based on a socio-cognitive model. The questionnaire assesses five constructs: intention (two items), social influence (three items), beliefs about one’s capabilities (three items), moral norm (two items), and beliefs about consequences (two items). Scores per construct range from 1 = low to 7 = high (Figure S1 and S2). One item of the social influence construct is scored as a percentage category (0–20%, 21–40%, 41–60%, or 81–100%). The CPD-Reaction questionnaire26 has a reported internal consistency estimate for reliability of each subscale ranging from Cronbach’s alpha 0.79 to 0.89. This tool was used to assess the differences in perceptions related to SDM among different target groups (faculty members, health professionals and students) to be able to tailor an intervention to undergraduate health professions students.
- Section three: the assessment of faculty members’, health professionals’, and students’ practice in SDM was carried out by using the 19-item partnership/SDM scale in the Assessment of Interprofessional Team Collaboration Scale (AITCS; Figures S1 and S2).27 It consists of a five-item Likert-type scale, where 1 = never and 5 = always. The AITCS27 has an estimate for reliability of each subscale ranging from 0.80 to 0.97, with an overall reliability of 0.98. It has been used to measure cultural shifts toward IPC in organizations. Moreover, face validity and content validity had been done by the Palliative Care Department and Medical Education Department.
Data Analysis
SPSS version 23 was used for statistical analyses of the data. Descriptive statistics, such as frequency and percentages, were used to report participant’s characteristics and familiarity with the IP-SDM in palliative care. Mean and standard deviation (SD) were used to report the five constructs in the CPD-Reaction questionnaire and the perceptions rating and practices rating scores. The rating scores for each participant were calculated from the scores in the two domains (perception and practices), taking into account all assumptions required for a scoring system used in similar situations, and gave equal weight for each domain, even if the number of questions in each domain were different. This scoring system was then used in performing multiple regression analysis, allowing for better comparison of the total scores with the factors associated with IP-SDM in palliative care.
The Shapiro–Wilk test was used to assess normality, and the results showed the data was normally distributed. Thus, we utilized parametric statistical methods. To compare the rating scores with background factors (eg, gender, study experience, training experience), bivariate statistics such as independent sample t-tests were used. One-way ANOVA was used to compare each of the rating scores with nationality, discipline, years of study, level of education, teaching experience, and clinical experience factors. The correlation coefficient was used to measure the strength of the linear association between each of the rating scores with age. Linear multiple-regression analyses were conducted to compare perceptions and practices rating scores to other factors, including previous experience in IPE, IPC, SDM and palliative care. We have evaluated several assumptions to ensure accuracy of the results. The normality assumption was not violated for each variable included and the normal probability plot of standardized residuals indicated that linearity and homoscedasticity of residuals were met; Mahalanobis distance did not exceed critical value for any cases; and relatively high tolerances for both predictors indicated multicollinearity would not interfere with interpretation of results. P-values of <0.05 were considered statistically significant.
Results
Participants’ Characteristics
The response rate was 54% for 459 participants, of which 85 were faculty members or health professionals and 164 were health profession students. The mean age of the faculty members and health professionals was 38.2 years (SD = 8.7); for health profession students it was 23.9 years (SD = 3.0). Table 1 shows the participants’ characteristics. Seventy percent of faculty members and health professionals were trained or worked abroad. In regard to teaching experience, 34% had no experience, whereas 25% had 10 years’ experience or more. Thirty-nine percent of the faculty members and health professionals had experience with IPE during training and work. More than 70% of them had experience with IPC, SDM, and palliative care. However, more than half of the students had no experience with IPE during their training, 63% had experience with SDM during their training, and 68% studied about palliative care or encountered a palliative patient. Participants were asked about their level of knowledge toward IP-SDM in palliative care. The mean score out of 10 for faculty members and health professionals was 6 (SD = 2.3), and for health profession students it was 4 (SD = 2.4). Table 2 demonstrates the participants’ familiarity with IP-SDM in palliative care.
 |
Table 1 Participants’ Characteristics (n = 249) |
 |
Table 2 Participants’ Familiarity with the IP-SDM in Palliative Care |
Perceptions Toward IP-SDM Education in Palliative Care
Participants were asked about their perceptions to participate in IP-SDM education in palliative care. The mean score and SD of the five constructs were for intention (M = 74.8, SD = 22.7 vs M = 74.2, SD = 22.6 [for faculty members and health professionals vs students]), social influence (M = 65.8, SD = 21.9 vs M = 65.9, SD = 16.7), beliefs about one’s capabilities (M = 72.2, SD = 20.2 vs M = 72.9, SD = 18.9), moral norm (M = 77.9, SD = 18.8 vs M = 77.9, SD = 19.3), and beliefs about consequences (M = 80.6, SD = 18.7 vs M = 77.2, SD = 21.5). The perceptions did not differ between the faculty members and health professionals and the students.
Practices of IP-SDM in Palliative Care
Twenty-nine percent of the 52 participants from faculty members and health professionals had a very positive experience about IP-SDM in palliative care. Regarding students, 67% of the 70 participants had a more positive experience than negative. Tables 3 and 4 demonstrate the mean and SD of faculty members’, health professionals’, and students’ practice while working as a team in palliative care settings. More than 50% of faculty members and health professionals answered positively with “most of the time” or “always” in regard to working as a team. However, 30% of students answered “most of the time” or “occasionally.”
 |
Table 3 Faculty Members’ and Health Professionals’ Practices Toward IP-SDM in Palliative Care |
 |
Table 4 Students’ Practices Toward IP-SDM in Palliative Care |
Factors Associated with Perceptions and Practices Toward IP-SDM in Palliative Care
Regarding perceptions, 85 faculty members and health professionals displayed a mean perceptions rating score of 74.3 (SD = 18). The factors found to have a positive impact on perceptions levels were discipline (p-value = 0.017) and previous experience with IPC and SDM (the multivariate linear regression analysis indicated p-values of 0.006 and <0.001 for these two factors, respectively; Table 5). Nationality, level of education, teaching experience, clinical experience, IPE experience, and studying and training experience, however, were not associated with perceptions rating scores (p-value = 0.796). Additionally, the correlation coefficient showed a weak spherical relationship between age factor and perceptions rating scores (p-value = 0.277). There was no association between perceptions rating scores and gender (p-value = 0.796).
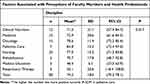 |
Table 5 Factors Associated with Perceptions of Participants Towards IP-SDM in Palliative Care |
The 164 students displayed a mean perception rating score of 73.6 and an SD of 17.6. The factors that were observed to have an impact on the perceptions rating score included previous experience with SDM (independent sample t-test = 5.5, P-value < 0.0001) and students with prior experience in palliative care (independent sample t-test = 3.7, p < 0.001). Females were found to have slightly higher perception scores, with a mean difference of 2.8 (SE = 2.62, 85% CI), indicating no association between perceptions and gender. Furthermore, the factors of discipline, year of study, previous experience with IPE and palliative care were all determined to have no association with the perceptions rating score. The multivariate linear regression analysis showed the p-value for the previous experience factor with IPE was 0.65, whereas the p-value for palliative care was 0.17; this could indicate that the two factors are related to each other and should be considered together when assessing perception scores.
Regarding practice, 30 faculty members and health professionals displayed a mean practice rating score of 83.1 and an SD of 15.9. The factors that were associated with practice were discipline (p-value = 0.001), teaching experience (p-value = 0.022; Table 6), and previous experience with SDM (p-value = 0.000). There was no significant association between age and practice (p-value = 0.605) and gender and practice (p-value = 0.734). Nationality, level of education, clinical experience, IPE experience, and training experience were also all determined to have no association with the practice level (p-value > 0.05). The multivariate linear regression analysis with previous experience with IPC (p-value = 0.113) and palliative care (p-value = 0.375) yielded no statistically significant results.
 |
Table 6 Factors Associated with Practices of Participants Towards IP-SDM in Palliative Care |
The 29 students displayed a mean practice rating score of 74.1 and an SD of 11.6. In bivariate analysis, all the factors had no association with practice level except for students with prior experience in palliative care (independent sample t-test = 3.23, p-value = 0.019). However, the multivariate linear regression analysis showed no significant difference in all factors: previous experience with IPE (p-value = 0.468), SDM (p-value = 0.796), and palliative care (P-value = 0.344).
Discussion
This study was conducted to explore the perceptions and practices from faculty members, health professionals, and students toward IP-SDM education in palliative care and to indicate the factors that were associated with perceptions and practices to implement IP-SDM education for health professions undergraduate students in palliative care. This study represents the first one of its kind among health profession universities in Saudi Arabia. It showed positive perceptions toward IP-SDM education in palliative care among faculty members, health professionals, and students with low levels of practice of IP-SDM. Factors associated with perceptions and practices of participants toward IP-SDM in palliative care varied per group of participants. For faculty members’ perceptions, these were discipline and previous experience with IPC and SDM. For students, it was previous experience with SDM and palliative care only. The factors associated with practice were discipline, teaching experience, and previous experience with SDM for faculty members. However, no associations were found between the factors and students’ practices. This could be due to the different levels of experience with the topic and number of participants.
With regard to familiarity of the topic, one-third of faculty members and health professionals knew a little bit about IP-SDM, but 45% of students had never heard about IP-SDM. This could be due to insufficient integration of the topic in the undergraduate health professions curricula. A study by Mathijssen et al also showed that nurses and physicians lacked full conceptual understanding of SDM.28 Furthermore, there are limited studies globally about the knowledge toward IP-SDM among health profession students.29
The positive perceptions for SDM were also noticed among health professionals regarding patients’ involvement and SDM skills,30 and positive attitudes of SDM were found in a study among health care professions and specialties,31 but these studies did not include health profession students. In a study among medical students, the dominant constructs were beliefs about consequences, social influence, and beliefs about capabilities.31 The factors that were associated with perceptions of faculty members and health professionals included discipline and previous experience with IPC and SDM, indicating that professionals from oncology and palliative care disciplines with previous experience with IPC and SDM had higher scores compared to those from clinical nutrition and nursing disciplines. However, for students, the factors that were related to their perceptions were previous experience with SDM and palliative care. As in our study, a study by Yen et al showed that perceptions did not vary with age, race, gender, school, school year, or country of education.32 Means of the perceptions toward IP-SDM education were highly similar between the group with experience (faculty and health professionals) and the group without (students), indicating that, independent of prior experience, participants were positive about engaging in IP-SDM and it was not a barrier to participating in IP-SDM activities in palliative care at MNGHA and KSAU-HS in Jeddah, Saudi Arabia. In a scoping review about embedded SDM in undergraduate education, researchers found that education had a positive impact on students’ attitude regarding SDM.33 Although the Legaré et al 12-item instrument26 targets health care professionals and is designed to evaluate the impact of CPD activities, it has been used in this study to provide context for the socio-cognitive perceptions towards IP-SDM education in palliative care settings.
With regard to IP-SDM practice, more than half of the faculty members and health professionals had a very positive experience, and two-thirds of students had a more positive than negative experience. A recent randomized controlled trial proved that training in SDM in palliative care is feasible and significantly improved trainees’ practices.34 In our study, participants were also asked about their experience regarding IP-SDM practice in palliative care. The number of faculty members and health professionals that had been involved in IP-SDM were 30 out of 85, and for health profession students the number was 29 out of 164. This could be due to the fact that currently there is no offering of this topic in our curricula. These results are in line with a study that showed limited opportunities for students within health professions to learn about SDM.35
Limitations
Survey designs are prone to common biases such as self-selection bias. The self-selection bias could be due to high motivation toward IP-SDM education in palliative care, which could have led to more favorable perceptions regarding IP-SDM. The questionnaire is originally developed to assess teams and that we now apply that for individuals. This could undermine the gist of the original version. However, we used this instrument to measure subjective perception of IP-SDM at the individual level. We are aware that the use of this questionnaire in this context requires further validity testing.
Additionally, the outcomes of the study may not be generalizable because it was conducted in a single university, thus posing potential limitations of the conclusions that can be drawn from the research. Despite these limitations, this is the first study in Saudi Arabian universities to explore the perceptions and practices of IP-SDM in palliative care for undergraduate health profession students.
Conclusions
Via this study, we gained insights into the perceptions of faculty members, health professionals, and students, showing there is interest for IP-SDM in palliative care for undergraduate health professions education. Based on the positive perceptions toward IP-SDM, we think there is room for an intervention. However, the number of participants who experienced or practiced IP-SDM in palliative care was low. Globally, there is limited research about knowledge toward IP-SDM among health profession students.32 Exploration of factors associated with perceptions and practices were varied among participants. Because limited factors were actually associated with the “practice rating score”, we could have missed other important factors, such as confidence and self-efficacy regarding IP-SDM. Other factors need to be addressed to assess the association between perceptions and practices toward IP-SDM education in palliative care. Nevertheless, this study functions as a useful needs assessment for educators planning to implement curricula around IP-SDM in palliative care for undergraduate health profession students.
Lessons of Practice
- There is limited research about the knowledge toward IP-SDM among health profession students.
- The factors that associated with perceptions and practices of participants toward IP-SDM in palliative care are varied.
- Other factors such as confidence and self efficacy need to be addressed to assess the association between perceptions and practices toward IP-SDM education in palliative care.
Ethical Approval
- Permission obtained from the Oncology and Palliative Care Departments and from the College of Medicine, the College of Nursing and the College of Applied Medical Sciences at King Abdul-Aziz Medical City in Jeddah, Saudi Arabia to start the study after approval given from King Abdullah International Medical Research Center (KAIMRC) with an IRB no. (RJ20/242/J).
- All the information was confidential. The identity of the participants was secured, and personal contact information was not gathered.
- Consent was taken from each participant.
- No marks were giving for participation in the study. The participation was completely voluntarily.
- Data were stored in workplace computer accessed only by the research team.
- Data were summarized and presented with honesty without any fabrication and falsification.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dang S. Shared decision making-the pinnacle of patient-centered care. J Indian Acad Geriatr. 2018;14(2):184.
2. Elwyn G, Laitner S, Coulter A, et al. Implementing shared decision making in the NHS. BMJ. 2010;341:341.
3. Cain CL, Surbone A, Elk R, et al. Culture and palliative care: preferences, communication, meaning, and mutual decision-making. J Pain and Symptom Manage. 2018;55(5):
4. Gramling R, Sanders M, Ladwig S, et al. Goal communication in palliative care decision-making consultations. J Pain and Symptom Manage. 2015;50(5):
5. Hirpara DH, Cleghorn MC, Sockalingam S, et al. Understanding the complexities of shared decision-making in cancer: a qualitative study of the perspectives of patients undergoing colorectal surgery. Can J Surg. 2016;59(3):197. doi:10.1503/cjs.013415
6. Covvey JR, Kamal KM, Gorse EE, et al. Barriers and facilitators to shared decision-making in oncology: a systematic review of the literature. Support Care Cancer. 2019;27(5):
7. Schram AW, Hougham GW, Meltzer DO, et al. Palliative care in critical care settings: a systematic review of communication-based competencies essential for patient and family satisfaction. Am J Hosp Palliat Care. 2017;34(9):
8. Iida K, Ryan A, Hasson F, et al. Palliative and end-of-life educational Interventions for staff working in long-term care facilities: an Integrative review of the literature. J Older People Nurs. 2021;16(1):e12347. doi:10.1111/opn.12347
9. Castro AA, Taquette SR, Pereira CR, et al. Palliative care in medical education: the students’ perception. Rev Bras Educ Med. 2021;46.
10. Thrane SE. Online palliative and end-of-life care education for undergraduate nurses. J Prof Nurs. 2020;36(1):42–46. doi:10.1016/j.profnurs.2019.07.002
11. Webb JA, Casarett D. A prescription for population-based palliative care education. Generations. 2017;41(1):
12. Dickinson GE. End-of-life and palliative care issues in medical and nursing schools in the United States. Death Studies. 2007;31(8):713–726. doi:10.1080/07481180701490602
13. Cheung NY, Gorelik A, Mehta P, et al. Perception of palliative medicine by health care professionals at a teaching community hospital: what is the key to a “palliative attitude”? J Multidiscip Healthc. 2019;12:
14. Dharmarajan KV, Wei R, Vapiwala N. Primary palliative care education in specialty oncology training: more work is needed. JAMA Oncol. 2016;2(7):
15. Hind M, Norman I, Cooper S, et al. Interprofessional perceptions of health care students. J Interprof Care. 2003;17(1):
16. Rokusek C, Chandan N. Palliative care - an ideal environment for interprofessional education and practice. Austin Palliat Care. 2016;1(2):1006.
17. Lie DA, Richter-Lagha R, Forest CP, et al. When less is more: validating a brief scale to rate interprofessional team competencies. Med Educ Online. 2017;22(1):1314751. doi:10.1080/10872981.2017.1314751
18. Centre for Advancement in Interprofessional Education (CAIPE). 2002. Interprofessional education – a definition.
19. Reeves S, Fletcher S, Barr H, et al. A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Med Teach. 2016;38(7):
20. Pereira J, Meadows L, Kljujic D, et al. Do learners implement what they learn? Commitment-to-change following an interprofessional palliative care course. Palliat Care. 2022;36(5):866–877.
21. Sultan L, de Jong N, Alsaywid S, et al. A qualitative study of stakeholders’ perspectives of implementing interprofessional shared decision-making education in palliative care. Cureus. 2023;15(8).
22. Loversidge J, Demb A. Faculty perceptions of key factors in interprofessional education. J of Interprof Care. 2015;29(4):
23. Christianson TM, Bainbridge L, Halupa C. A pilot study on interprofessional education: how prepared are faculty to teach? Prof Devt in Educ. 2019;45(4):
24. Cimino FM, Varpio L, Konopasky AW, et al. Can we realize our collaborative potential? a critical review of faculty roles and experiences in interprofessional education. Acad Med. 2022;97(11S):S87–S95. doi:10.1097/ACM.0000000000004909
25. Watkins KD. Faculty development to support interprofessional education in healthcare professions: a realist synthesis. J Interprof Care. 2016;30(6):695–701. doi:10.1080/13561820.2016.1209466
26. Légaré F, Borduas F, Freitas A, et al. Development of a simple 12-item theory-based instrument to assess the impact of continuing professional development on clinical behavioral intentions. PLoS One. 2014;9(3):
27. Orchard CA, King GA, Khalili H, et al. Assessment of interprofessional team collaboration scale (AITCS): development and testing of the instrument. J Contin Educ Health Prof. 2012;32(1):
28. Mathijssen EG, van den Bemt BJ, Wielsma S, et al. Exploring healthcare professionals’ knowledge, attitudes and experiences of shared decision making in rheumatology. RMD Open. 2020;6(1):e001121. doi:10.1136/rmdopen-2019-001121
29. Yen RW, Barr PJ, Cochran N, et al. Medical students’ knowledge and attitudes toward shared decision making: results from a multinational, cross-sectional survey. MDM Policy Pract. 2019;4(2):2381468319885871. doi:10.1177/2381468319885871
30. Kienlin S, Nytrøen K, Stacey D, et al. Ready for shared decision making: pretesting a training module for health professionals on sharing decisions with their patients. J Eval Clin Pract. 2020;26(2):
31. Forcino RC, Yen RW, Aboumrad M, et al. US-based cross-sectional survey of clinicians’ knowledge and attitudes about shared decision-making across healthcare professions and specialties. BMJ open. 2018;8(10):e022730. doi:10.1136/bmjopen-2018-022730
32. Yen RW, Barr PJ, Cochran N, et al. Medical students’ knowledge and attitudes toward shared decision making: results from a multinational, cross-sectional survey. MDM P & P. 2019;4(2):2381468319885871
33. Durand MA, DiMilia PR, Song J, et al. Shared decision making embedded in the undergraduate medical curriculum: a scoping review. PLoS One. 2018;13(11):e0207012. doi:10.1371/journal.pone.0207012
34. Henselmans I, van Laarhoven HW, de Haes HC, et al. Training for medical oncologists on shared decision‐making about palliative chemotherapy: a randomized controlled trial. oncologist. 2019;24(2):
35. Eaton G. Learning values in shared decision‐making in undergraduate paramedic education. J Eval Clin Pract. 2019;25(6):1094–1101. doi:10.1111/jep.13247
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
