Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Exacerbations and Real-World Outcomes After Single-Inhaler Triple Therapy of Budesonide/Glycopyrrolate/Formoterol Fumarate, Among Patients with COPD: Results from the EROS (US) Study
Authors Strange C , Tkacz J, Schinkel J, Lewing B, Agatep B, Swisher S, Patel S, Edwards D, Touchette DR, Portillo E, Feigler N, Pollack M
Received 5 August 2023
Accepted for publication 1 October 2023
Published 12 October 2023 Volume 2023:18 Pages 2245—2256
DOI https://doi.org/10.2147/COPD.S432963
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Charlie Strange,1 Joseph Tkacz,2 Jill Schinkel,2 Benjamin Lewing,2 Barnabie Agatep,2 Sean Swisher,3 Sushma Patel,3 Devechio Edwards,3 Daniel R Touchette,4 Edward Portillo,5 Norbert Feigler,3 Michael Pollack3
1College of Medicine, The Medical University of South Carolina, Charleston, SC, USA; 2Data Solutions, Inovalon, Bowie, MD, USA; 3BioPharmaceuticals Medical, AstraZeneca, Wilmington, DE, USA; 4College of Pharmacy - Pharmacy Systems Outcomes and Policy, University of Illinois Chicago, Chicago, IL, USA; 5Pharmacy Practice & Translational Research Division, University of Wisconsin-Madison, Madison, WI, USA
Correspondence: Michael Pollack, BioPharmaceuticals Medical, AstraZeneca, 1800 Concord Pike, Bldg A1C, Wilmington, DE, 19850, USA, Tel +1 302-886-1253, Email [email protected]
Purpose: Triple therapy to prevent exacerbations from chronic obstructive pulmonary disease (COPD) is associated with improved health compared to single and dual-agent therapy in some populations. This study assessed the benefits of prompt administration of budesonide/glycopyrrolate/formoterol fumarate (BGF) following a COPD exacerbation.
Patients and methods: EROS was a retrospective analysis of people with COPD using the MORE2 Registry®. Inclusion required ≥ 1 severe, ≥ 2 moderate, or ≥ 1 moderate exacerbation while on other maintenance treatment. Within 12 months following the index exacerbation, ≥ 1 pharmacy claim for BGF was required. Primary outcomes were the rate of COPD exacerbations and healthcare costs for those that received BGF promptly (within 30 days of index exacerbation) versus delayed (31– 180 days) and very delayed (181– 365 days). The effect of each 30-day delay in initiation of BGF was estimated using a multivariable negative binomial regression model.
Results: 2409 patients were identified: 434 prompt, 1187 delayed, and 788 very delayed. The rate (95% CI) of total exacerbations post-index increased as time to BGF initiation increased: prompt 1.52 (1.39– 1.66); delayed 2.00 (1.92– 2.09); and very delayed 2.30 (2.20– 2.40). Adjusting for patient characteristics, each 30-day delay in receiving BGF was associated with a 5% increase in the average number of subsequent exacerbations (rate ratio, 95% CI: 1.05, 1.01– 1.08; p< 0.05). Prompt initiation of BGF was also associated with lower post-index annualized COPD-related costs ($5002 for prompt vs $7639 and $8724 for the delayed and very delayed groups, respectively).
Conclusion: Following a COPD exacerbation, promptly initiating BGF was associated with a reduction in subsequent exacerbations and reduced healthcare utilization and costs.
Keywords: COPD, triple therapy, exacerbations, delayed therapy, budesonide/glycopyrrolate/formoterol fumarate
Introduction
Chronic obstructive pulmonary disease (COPD) is common and costly, disproportionately affecting those with lower income and public insurance.1–4 It has been estimated that the national annual COPD-attributable medical expenditure was $31.3 billion in 2019, and projections have estimated that US national medical costs could approach $50 billion by 2026.2–4
People living with COPD often have periods of acute worsening of symptoms, known as exacerbations.5 Moderate exacerbations require treatment with antibiotics and/or systemic corticosteroids, whereas severe exacerbations require hospitalization, which account for an estimated 50–70% of COPD-related medical expenditures.3,6–8
Current guidelines for the treatment of COPD recommend initial therapy aimed at controlling symptoms and reducing exacerbations, based on symptom severity and exacerbation history.9,10 Among COPD patients who have experienced COPD exacerbations, the recent (2023) Global Initiative for Chronic Obstructive Lung Disease (GOLD) report recommends considering initial treatment with or escalation to triple therapy, consisting of inhaled corticosteroids/long-acting β2-agonists/long-acting muscarinic antagonists (ICS/LABA/LAMA).9,10 Compared to both single agent and dual-therapy combinations, triple therapy has been demonstrated to reduce the rate of exacerbations and improve lung function among COPD patients, in addition to demonstrating potential benefits related reducing all-cause mortality as acknowledged recently by GOLD.11–14 In July 2020, the US Food and Drug Administration (FDA) approved the fixed-dose single-inhaler combination therapy of budesonide/glycopyrrolate/formoterol fumarate (BGF), as a maintenance treatment for COPD. The BGF registrational study, called ETHOS, demonstrated statistically significant reductions in the rate of moderate or severe exacerbations among COPD patients randomized to BGF compared to dual-combination therapies.15 In addition to reductions in exacerbations, analyses from the final retrieved data set of ETHOS demonstrated a 49% (hazard ratio, 0.51; 95% confidence interval, 0.33–0.80) reduction in all-cause mortality with BGF compared to LAMA-LABA over 52 weeks.14
Over the past decade, several real-world studies have assessed the relationship between COPD maintenance treatment initiation and health outcomes. Results indicate that prompt initiation of maintenance therapy after an exacerbation is associated with reduced healthcare utilization and expenditures, in addition to lower risk for subsequent exacerbations.16–22 Emerging evidence indicates that promptly initiating triple therapy following an exacerbation is associated with decreased morbidity and healthcare costs relative to delayed initiation.23–25 Because there is limited real-world evidence assessing the relationship between the timing of BGF following an exacerbation and the appearance of subsequent exacerbations, the aim of this study was to assess patient characteristics, health outcomes, and costs associated with prompt, delayed, and very delayed use following a COPD exacerbation.
Methods
Study Population
This study was a retrospective analysis of de-identified claims data of COPD patients experiencing a disease exacerbation followed by treatment with BGF. This analysis utilized the MORE2 Registry (data spanning July 2019 to March 2022), a real-world closed claims database that is inclusive of medical and pharmacy claims, representing all 50 states and includes major US payer lines of business, including commercial, Medicare Advantage, and managed Medicaid. All patient records were de-identified and certified to be in full compliance with the confidentiality requirements outlined in the Health Insurance Portability and Accountability Act of 1996 in the United States. Per Title 45 of CFR, Part 46, the administrative claims data analysis of our study was exempt from the IRB review as it was a retrospective analysis of existing data (hence no patient intervention or interaction), and no patient-identifiable information was included in the claims dataset.
All patients had at least one claim for BGF and at least one of the three categories of exacerbation events in the 12-month period preceding initiation of BGF. To be included in the study, patients must have presented at least one moderate exacerbation while being treated with COPD inhaled maintenance, two moderate exacerbations, or one severe exacerbation. Exacerbations were categorized as follows: one moderate exacerbation with prior COPD maintenance therapy, two moderate exacerbations, or one severe exacerbation. The index date was the earliest exacerbation event occurring prior to BGF initiation but after the approval of BGF (July 24, 2020). In addition, the included patients were required to be age ≥40 at the index date, have ≥12 months of continuous enrolment preceding the index date, and have ≥90 days of continuous enrollment following the index date. Individuals were followed from their index to the end of the study. Individuals using closed triple therapy during the baseline period or had a severe exacerbation prior to BGF approval were excluded.
Three study cohorts were created based on the timing of BGF initiation following the index exacerbation event (Figure 1). Patients initiating within 30 days of the index date were included in the prompt initiation group. Those initiating between 31 and 180 days and 181 and 365 days after index were included in the delayed and very delayed groups, respectively.
Study Outcomes
Patient demographics and clinical characteristics were collected for each cohort at baseline. The Elixhauser Comorbidity Index (ECI) was calculated.26,27 Outcomes of interest included COPD exacerbations, COPD-related healthcare resource utilization (HCRU), and COPD-related healthcare costs, each measured during the follow-up period. COPD exacerbations were measured by calculating the rates of moderate and severe exacerbations during the post-index follow-up. As individual follow-up time varied by patient, rates were annualized and reported as per-patient-per-year (PPPY), along with 95% confidence interval (CI).
The operational definitions of moderate and severe exacerbations were adapted from analyses previously conducted by the study teams.24 Moderate exacerbations were defined as an outpatient visit with a COPD diagnosis followed by a filled prescription for a short-course of oral corticosteroids (OCS) or antibiotic (≤14 days) within (±) 7 days of the outpatient visit, or any outpatient visit with a diagnosis of COPD and a corticosteroid injection. Severe exacerbations were defined as an inpatient hospitalization with a primary diagnosis of COPD or a primary diagnosis of respiratory failure with a secondary diagnosis of COPD. Additional exploratory analyses were conducted that examined sub-groups by type of maintenance therapy used in the 30 days prior to BGF initiation and in the 30-day period following the index exacerbation.
COPD-related HCRU and expenditures were collected during the 12-month baseline and during the variable-length follow-up period. During the post-index period, HCRU and costs were reported as average PPPY. HCRU included the average number of emergency department (ED), urgent care (UC) visits, and inpatient stays, while costs included total medical costs, pharmacy costs, inpatient costs, ED costs, and UC costs. COPD-related HCRU and costs were based on inpatient claims with a COPD diagnosis in the primary position, and outpatient claims with a COPD diagnosis in any position. All costs were adjusted for inflation using the medical care component of the Consumer Price Index obtained from the US Bureau of Labor Statistics and standardized to 2022 USD.28
Statistical Analysis
Demographics and clinical characteristics were presented via means, medians, and standard deviations (SD) for continuous variables, and frequencies and proportions for categorical variables. Statistically significant differences across study groups were determined via analysis of variance (ANOVA) for normally distributed continuous variables, Kruskal-Wallis test for skewed variables, and chi-square tests of equality of proportions for categorical variables. A multivariable negative binomial regression model was constructed to estimate the effect of each 30-day delay in initiation of BGF on the average number of subsequent disease exacerbations (either moderate or severe) during the follow-up period, while a gamma model with a log-link was constructed to estimate the effect of each 30-day delay in initiation of BGF on the incremental increase in COPD-related costs. The critical alpha level was set at 0.05 for all analyses.
Results
Characteristics of Study Sample
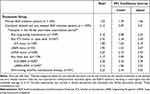
A total of 2409 COPD patients met all sample selection criteria: 434 prompt, 1187 delayed, and 788 very delayed (Figure 2). A total of 835 (34.7%) patients indexed with one moderate exacerbation with prior COPD maintenance therapy, 1337 (55.5%) indexed with two moderate exacerbations and 237 (9.8%) indexed with a severe exacerbation. The overall study cohort was 63.4% female. There were no differences in patient demographics by group, and baseline comorbidities were similar with a few exceptions (Table 1, see Table S1 for the full set of demographics collected). Notably, there were no differences in reported rates of allergic rhinitis, asthma, or smoking between groups. Managed Medicaid was the most common insurance type (42.6–47.7% within groups). Patients had an average follow-up of 331 days, with each cohort consisting of over 70% of individuals with at least 180 days of follow-up time.
 |
Table 1 Demographic and Clinical Characteristics, Among COPD Patients Initiating Budesonide/Glycopyrrolate/Formoterol Fumarate (BGF) Following a COPD Exacerbation, by Delay in BGF Initiation |
Compared with patients who promptly started BGF, patients who delayed BGF trended toward higher ECI scores 4.7 ± 6.3 (prompt), 5.6 ± 7.2 (delayed) and 5.8 ± 7.6 (very delayed) and were more likely to have pulmonary/respiratory failure: 6.5% (prompt), 9.9% (delayed) and 12.0% (very delayed). Most patients were indexed on a moderate exacerbation (90.2%), and patients among the delayed and very delayed cohort were about twice as likely to index from a severe exacerbation (5.8% for the prompt group vs 9.3% and 12.9% for the delayed and very delayed groups, respectively). During the baseline period, 97.7% had some maintenance medication of any type, with 85.1% having some long-acting inhaled medication, and overall 62.7% had fixed combination of ICS/LABA and 19.1% had fixed LABA/LAMA combination.
Baseline and Follow-Up Exacerbation Rates
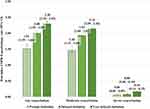
The rates of post-index exacerbation events were compared among the cohorts (Figure 3). The rate (95% CI) of total exacerbations increased as the time from index exacerbation to BGF administration increased: prompt 1.52 (1.39–1.66); delayed 2.00 (1.92–2.09); and very delayed 2.30 (2.20–2.40), p<0.01. Relative rates of total exacerbations for prompt were 0.76, 95% CI: (0.72 – 0.79) and 0.66, 95% CI: (0.63 – 0.69) versus delayed and very delayed. The trend persisted for severe exacerbations: prompt 0.06 (0.04–0.09); delayed 0.08 (0.06–0.10); and very delayed 0.16 (0.14–0.19), p<0.01. Relative rates of severe exacerbations for prompt were 0.75 (95% CI: 0.67-0.90) and 0.38 (95% CI: 0.29-0.47) versus delayed and very delayed. Additional exploratory analyses revealed that the rate of exacerbation remained higher for all maintenance COPD therapy classes prescribed compared to the prompt BGF group, including annualized rates of 2.14 (LAMA/LABA) and 2.20 (ICS/LABA) based on treatment received 30 days post index (Table 2). A similar trend was observed when examining the 30-day period preceding BGF initiation, with the highest rate observed in the group receiving short acting only or no maintenance (Table S2)
Results of a multivariable negative binomial regression model adjusting for patient characteristics and baseline exacerbation history revealed that each 30-day delay in receiving BGF was associated with a 5% increase in average number of subsequent exacerbations during the follow-up period, compared to individuals who initiated BGF < 30 days after the post-index exacerbation, rate ratio (95% CI): 1.05 (1.01–1.08), p<0.05 (Figure 4). Other statistically significant factors associated with post-index exacerbations were severe index exacerbation (1.45 (1.04–2.01), p<0.05; ref. moderate index exacerbation), presence of any short-acting treatment during baseline (1.06 (1.02–2.12), p<0.05), number of pulmonologist visits during baseline (0.72 (0.54–0.96), p<0.05), number of baseline COPD visits during baseline (1.02 (1.00–1.03), p<0.05), and number of baseline exacerbations (2.27 (1.88–2.73), p<0.05). Figure 5 displays the estimated increase in post-index COPD exacerbations for each 90-day delay in BGF initiation, by lower-bound, average, and upper-bound adjusted rate ratios, which provides a visualization of the cumulative exacerbation risk from delay of BGF initiation. After 12-months delay, those that initiated BGF were estimated to have a 60% increase in exacerbations, on average. Similarly, among who had a severe index exacerbation, the multivariable negative binomial regression model indicated that every 30-day delay in initiation was associated with a 10% increase in subsequent exacerbations during follow-up, rate ratio (95% CI): 1.10 (1.00–1.20), p<0.05.
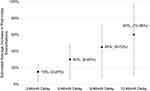 |
Figure 5 Estimated increase in post-index COPD exacerbations for each 3-month delay in BGF initiation, by average, (lower-bound-upper-bound) adjusted rate ratios. These estimates are extrapolated from the negative binomial regression model presented in Figure 4. Abbreviations: BGF, budesonide/glycopyrrolate/formoterol fumarate; COPD, chronic obstructive pulmonary disease. |
Healthcare Utilization and Cost Outcomes
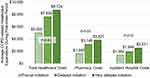
Full HCRU and costs results are shown in Table S3 which displays annualized (PPPY) follow-up COPD-related HCRU and COPD-related costs. Follow-up average COPD-related inpatient hospitalization visits increased as time to BGF initiation increased (mean (SD)): 0.17 (0.55), 0.26 (0.82), and 0.31 (0.80) for the three groups, p<0.05. Figure 6 visualizes the primary expenditure outcomes. Similarly to post-index hospitalizations, post-index COPD-related healthcare costs increased as time to BGF increased for each of the three groups: $5002, $7639, and $8724 for the prompt, delayed, and very delayed groups, p<0.01 (Figure 6), an increase of 74% for the very delayed group, compared to the prompt group. Results of a gamma regression model with a log link adjusting for patient characteristics and baseline exacerbation history revealed that each 30-day delay in receiving BGF was associated with an increase in average COPD-related costs of $256 PPPY during the follow-up period, compared to individuals who initiated BGF < 30 days after the post-index exacerbation (estimate = 1.03 (95% CI): 1.02–1.05, p<0.05). On average, the delayed group delayed BGF by 100 days, resulting in an estimated increased cost of $853, while the very delayed group delayed BGF by 256 days, resulting in an estimated increased cost of $2185.
Discussion
This retrospective, observational database study was conducted to describe patient characteristics, outcomes, healthcare resource utilization, and costs of COPD patients initiating BGF following a COPD exacerbation. The patient characteristics were very similar to the study population of the PRIMUS study, which utilized data from the MarketScan research databases to examine COPD patients initiating triple therapy following a COPD exacerbation.24 Despite a similar demographic profile, the distribution of individuals among the prompt, delayed, and very delayed cohorts differed from PRIMUS. There were fewer individuals initiating BGF promptly, possibly due to the uptake of the newly available medication, BGF. Additionally, patients in the PRIMUS study had index years ranging from 2010 to 2019, before the start of the 2020 COVID-19 pandemic. Conversely, patients in the current study were indexed after the beginning of the pandemic which may have had a significant impact on healthcare utilization and access to care in the US.29
The present sample demonstrated particularly high ECI scores. As co-morbidities are common in COPD and frequently lead to mortality from non-COPD causes, it is important to further understand why escalation to triple therapy was often delayed in patients with greater presence of comorbidities. It is possible that providers and patients are prioritizing the management of other conditions at the expense of COPD, which is associated with the higher exacerbation rates observed here and elsewhere.24 The current study suggests that patients with comorbidities, who are more prone to severe exacerbations, are those in which triple therapy should be promptly initiated, rather than delayed. A hesitancy or delay in BGF uptake within hospitals likely adds to the disease and economic burden.
The primary finding of the present study is that delay in BGF initiation was associated with increased rates of COPD exacerbations, as the prompt group presented an average of 1.5 subsequent exacerbations compared to 2.0 for the delayed group and 2.3 for the very delayed group. Promptly initiating BGF following a moderate or severe exacerbation was associated with a 24.0% and 33.9% reduction in subsequent exacerbations among COPD patients appearing in the delayed and very delayed BGF initiation groups, respectively. This reduction in subsequent exacerbations for the prompt initiation group shows a similar trend to the same set of measures in the PRIMUS study.24 These benefits were present regardless of the type of maintenance therapy that patients remained on beyond the initial 30-days period following the index exacerbation.
The trend of increased exacerbation rates with increased delayed initiation of BGF persisted when controlling for patient characteristics and baseline exacerbations. For every 30-day delay in BGF, the average number of post-index exacerbations in the year following the initial exacerbation increased by 5%. Compared to those that initiated BGF within the first 30 days, a patient who delays initiation by a full year could face approximately 60% increase in average number of subsequent exacerbations. Similar to the trend observed in post-index exacerbations, delay in initiation of BGF was also associated with increases in post-index HCRU and costs. Patients within the prompt cohort, compared to the very delayed cohort, had less COPD-related HCRU in most places of service, including ED visits, urgent care visits, and inpatient hospitalizations.
When examining post-index costs, compared to the prompt group, the very delayed group incurred greater post-index COPD-related healthcare expenditure in each metric assessed, including hospital costs, total healthcare costs, and pharmacy costs.
Implications of Study Results and Future Research Direction
Taken together, the results indicate a strong pattern of increased exacerbations, healthcare utilization, and expenditure associated with delays in BGF initiation and remaining on existing standard of care beyond 30-days following a moderate or severe COPD exacerbation. Promptly initiating BGF following an exacerbation was associated with a reduction in subsequent exacerbations, healthcare utilization, and costs. Ultimately, as time to BGF administration increased, COPD-related healthcare costs increased, and every 30-day delay in BGF initiation was shown to increase exacerbation risk. Recently, Mannino et al published results of a retrospective analysis in the US of delayed treatment for another fixed triple and arrived at similar conclusions that prompt initiation of triple following a moderate or severe COPD exacerbation was associated with significant reductions in exacerbations and healthcare costs relative to delayed initiation.23 The results from these studies, EROS and Mannino, further support that proactive COPD management is both clinically and economically effective for patients, providers, and payers.
Study Limitations
As with all real-world data-based studies, there are a few limitations that should be considered when interpreting results. First, despite quality assurance processes, administrative claims data are subject to data coding limitations and data entry errors by providers, which may result in missing or erroneous data and may result in misclassification bias. It is also important to note that medication usage was based on filled outpatient prescriptions, and patients were assumed to take the medications as prescribed, though this cannot be confirmed. In addition, medications received as samples from physicians, inpatient medications, and prescriptions paid for exclusively out-of-pocket by patients are not captured, which could result in an underestimation of pharmacy and medical expenditure. Although multivariable modeling was used to control for baseline differences between cohorts, residual misbalancing may remain, and this adjustment was limited to variables that are able to be measured within administrative claims. It is also important to note that immortal time bias is built into the design, as only those patients who present continuous enrollment and an absence of death following the index exacerbation are eligible for inclusion of the study. Lastly, while the sample size is robust for this analysis, there may be populations (eg, uninsured, Medicare FFS) where these results may not be generalizable and require additional analyses.
Conclusion
Promptly initiating BGF following a moderate or severe exacerbation was associated with a reduction in subsequent exacerbations and costs among COPD patients compared to “delayed” and “very delayed” BGF initiation groups. Patients with a greater number of comorbidities were associated with higher rates of delayed initiation of BGF, suggesting those who are in the poorest overall health are those who are most delayed in receiving triple therapies. Proactive disease management, including the use of triple therapies, may be warranted to prevent future exacerbations among patients with COPD.
Abbreviations
ANOVA, analysis of variance; BGF, Budesonide/glycopyrrolate/formoterol; CI, confidence interval; COPD, Chronic obstructive pulmonary disease; ECI, Elixhauser Comorbidity Index; ED, emergency department; FDA, Food and Drug Administration; GOLD, Global Initiative for Chronic Obstructive Lung Disease; HCRU, healthcare resource utilization; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; OCS, oral corticosteroids; PPPY, per-patient-per-year; SD, standard deviation; UC, urgent care.
Ethics Approval and Informed Consent
As this was an analysis of de-identified claims data compliant with guidance related to the Health Insurance Portability and Accountability Act (HIPAA) privacy rule, institutional review board (IRB) approval was not required. Per Title 45 of CFR, Part 46, the administrative claims data analysis of our study was exempt from the IRB review as it was a retrospective analysis of existing data (hence no patient intervention or interaction), and no patient-identifiable information was included in the claims dataset.
Acknowledgments
Interim partial results for this paper were presented at American Thoracic Society conference 2023 and have been accepted for presentation at the American College of Chest Physicians conference 2023. The poster abstract was published in the American Journal of Respiratory and Critical Care Medicine, https://doi.org/10.1164/ajrccm-conference.2023.207.1_MeetingAbstracts.A6019.
Author Contributions
All authors had access to the data, had a role in writing this manuscript, including critically reviewing the manuscript, and made significant contributions to this work. All authors agreed on the journal submission choice, have agreed on all revisions, gave final approval for the version to be published, and agreed to be accountable for all aspects of the work.
Funding
This study was sponsored by AstraZeneca.
Disclosure
SS, SP, DE, NF, and MP are employees of AstraZeneca and hold AstraZeneca stock. JT, JS, BL, and BA are employees of Inovalon, who received funding from AstraZeneca to conduct this study. DRT, EP, and CS are paid consultants of AstraZeneca. DRT reports personal fees from Stage Analytics, eMax Health, Horizon Pharmaceuticals, Monument Analytics; grants from Takeda Pharmaceuticals, outside the submitted work. CS reports personal fees from AlphaNet, Adverum, CSL Behring, Morair, UpToDate, GlaxoSmithKline; grants from Arrowhead, OCI, Pandorum, Pulmanage, Takeda, Vertex, NuVaira, CSA Medical, Grifols, Pulmonx, and AstraZeneca, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Biener AI, Decker SL, Rohde F. Prevalence and treatment of Chronic Obstructive Pulmonary Disease (COPD) in the United States. JAMA. 2019;322(7):602. doi:10.1001/jama.2019.10241
2. Ford ES, Murphy LB, Khavjou O, Giles WH, Holt JB, Croft JB. Total and state-specific medical and absenteeism costs of COPD among adults aged >/= 18 years in the United States for 2010 and projections through 2020. Chest. 2015;147(1):31–45. doi:10.1378/chest.14-0972
3. Dieleman KID, Maxwell B, David HA, Laura JS, Laura CF, Joseph L. Health Care spending on respiratory diseases in the United States, 1996–2016. Am J Respir Crit Care Med. 2023. doi:10.1164/rccm.202202-0294OC
4. Mannino RM, Mapel D, Zhang Q, et al. Publications list. JMCP. 2023;29:1.
5. Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi:10.1164/rccm.201204-0596PP
6. Foster TS, Miller JD, Marton JP, Caloyeras JP, Russell MW, Menzin J. Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD. 2006;3(4):211–218. doi:10.1080/15412550601009396
7. Schwab P, Dhamane AD, Hopson SD, et al. Impact of comorbid conditions in COPD patients on health care resource utilization and costs in a predominantly medicare population. Int J Chron Obstruct Pulmon Dis. 2017;12:735–744. doi:10.2147/copd.s112256
8. Dalal AA, Christensen L, Liu F, Riedel AA. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chron Obstruct Pulmon Dis. 2010;5:341–349. doi:10.2147/COPD.S13771
9. Global Initiative for Chronic Obstructive Lung Disease Inc. Global initiative for chronic obstructive lung disease: global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease; 2021. Available from: https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf.
10. Sin DD, Singh D, Stockley R, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Eur Respir J. 2023;61(4). doi:10.1183/13993003.00239-2023
11. Vanfleteren L, Fabbri LM, Papi A, Petruzzelli S, Celli B. Triple therapy (ICS/LABA/LAMA) in COPD: time for a reappraisal. Int J Chron Obstruct Pulmon Dis. 2018;13:3971–3981. doi:10.2147/COPD.S185975
12. Zheng Y, Zhu J, Liu Y, et al. Triple therapy in the management of chronic obstructive pulmonary disease: systematic review and meta-analysis. BMJ. 2018;363:k4388. doi:10.1136/bmj.k4388
13. Bourdin A, Molinari N, Ferguson GT, et al. Efficacy and safety of budesonide/glycopyrronium/formoterol fumarate versus other triple combinations in COPD: a systematic literature review and network meta-analysis. Adv Ther. 2021;38(6):3089–3112. doi:10.1007/s12325-021-01703-z
14. Martinez FJ, Rabe KF, Ferguson GT, et al. Reduced all-cause mortality in the ETHOS trial of budesonide/glycopyrrolate/formoterol for chronic obstructive pulmonary disease. a randomized, double-blind, multicenter, parallel-group study. Am J Respir Crit Care Med. 2021;203(5):553–564. doi:10.1164/rccm.202006-2618OC
15. Rabe KF, Martinez FJ, Ferguson GT, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383(1):35–48. doi:10.1056/NEJMoa1916046
16. Baker CL, Zou KH, Su J. Long-acting bronchodilator use after hospitalization for COPD: an observational study of health insurance claims data. Int J Chron Obstruct Pulmon Dis. 2014;9:431–439. doi:10.2147/COPD.S59322
17. Buikema AR, Brekke L, Anderson A, et al. The effect of delaying initiation with umeclidinium/vilanterol in patients with COPD: an observational administrative claims database analysis using marginal structural models. Multidiscip Respir Med. 2018;13:38. doi:10.1186/s40248-018-0151-6
18. Coutinho AD, Lokhandwala T, Boggs RL, et al. Prompt initiation of maintenance treatment following a COPD exacerbation: outcomes in a large insured population. Int J Chron Obstruct Pulmon Dis. 2016;11:1223–1231. doi:10.2147/COPD.S102570
19. Dalal AA, Shah M, D’Souza AO, Crater GD. Rehospitalization risks and outcomes in COPD patients receiving maintenance pharmacotherapy. Respir Med. 2012;106(6):829–837. doi:10.1016/j.rmed.2011.11.012
20. Dalal AA, Shah MB, D’Souza AO, Dhamane AD, Crater GD. Outcomes associated with timing of maintenance treatment for COPD exacerbation. Am J Manag Care. 2012;18(9):e338–45.
21. Dalal AA, Shah MB, D’Souza AO, Lunacsek OE, Nagar SP, Crater GD. Observational study of the outcomes and costs of initiating maintenance therapies in patients with moderate exacerbations of COPD. Respir Res. 2012;13:41. doi:10.1186/1465-9921-13-41
22. Sicras Mainar A, Huerta A, Navarro Artieda R, Monso E, Landis SH, Ismaila AS. Economic impact of delaying initiation with multiple-inhaler maintenance triple therapy in Spanish patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2019;14:2121–2129. doi:10.2147/COPD.S211854
23. Mannino D, Bogart M, Germain G, et al. Benefit of Prompt versus delayed use of single-inhaler fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) following a COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2022;17:491–504. doi:10.2147/COPD.S337668
24. Tkacz J, Evans KA, Touchette DR, et al. PRIMUS - prompt initiation of maintenance therapy in the US: a real-world analysis of clinical and economic outcomes among patients initiating triple therapy following a COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2022;17:329–342. doi:10.2147/COPD.S347735
25. Evans A, Pollack M, Portillo E, et al. Prompt initiation of triple therapy following hospitalization for a chronic obstructive pulmonary disease exacerbation in the United States: an analysis of the PRIMUS study. J Manag Care Spec Pharm. 2022;28(12):1366–1377. doi:10.18553/jmcp.2022.28.12.1366
26. Agency for Healthcare Research and Quality. Elixhauser Comorbidity Software, Version 3.7. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp.
27. Agency for Healthcare Research and Quality. Elixhauser comorbidity software refined for ICD-10-CM. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp.
28. Statistics UBoL Consumer Price Index: Medical Care. Medical care in U.S. city average, all urban consumers, not seasonally adjusted. Available from: https://www.bls.gov/cpi/factsheets/medical-care.htm.
29. Xu S, Glenn S, Sy L, et al. Impact of the COVID-19 pandemic on health care utilization in a large integrated health care system: retrospective cohort study. J Med Internet Res. 2021;23(4). doi:10.2196/26558
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.