Back to Journals » Drug Design, Development and Therapy » Volume 17
Evaluation of the Effect of New Multimodal Analgesia Regimen for Cardiac Surgery: A Prospective, Randomized Controlled, Single-Center Clinical Study [Response to Letter]
Received 9 August 2023
Accepted for publication 16 August 2023
Published 22 August 2023 Volume 2023:17 Pages 2457—2460
Lin Jin, Kefang Guo
Department of Anesthesia, Zhongshan Hospital, Fudan University, Shanghai, People’s Republic of China
Correspondence: Kefang Guo, Department of Anesthesia, Zhongshan Hospital, Fudan University, No. 180, Fenglin Road, Xuhui District, Shanghai, People’s Republic of China, Email [email protected]
View the original paper by Dr Jin and colleagues
This is in response to the Letter to the Editor
Dear editor
Our previous study “Evaluation of the Effect of New Multimodal Analgesia Regimen for Cardiac Surgery: A Prospective, Randomized Controlled, Single Center Clinical Study” published in the June 2023 of Drug Design Development and Therapy.1 On behalf of our study team members, we want to share our appreciation for the comments from Chen PS, Xue FS and Li CW.2
Three important items mentioned by Chen et al2 were as follows: 1) How to calculate sample size based on preliminary study results; 2) The pain severity may affect the early mobilization; 3) Why we do not perform nerve block during the study.
In our study, sample size was calculated based on the findings of our preliminary study with the same protocol, in which incidence of moderate-to-severe pain was 64% and 35% in the control and multimodal groups, respectively.
44 patients were enrolled for eligibility review and randomization process, 2 cases of group M were excluded from our study due to procedure changed to lateral thoracic minimally invasive incisions. There was no significant difference in the demographic characteristics, ASA status and New York Heart Association (NYHA) grade. The main types of surgery were valvuloplasty or valve replacement. The difference was not statistically significant between groups of surgical types, cardiopulmonary bypass (CPB) time and aortic cross-clamp time (Table 1).
 |
Table 1 Demographic and Surgical Data of Patients in Preliminary Study |
Pain assessment was performed by a 100-millimeter visual analog scale (VAS). Patients were evaluated twice a day (7am-9am and 7pm-9pm) to record the VAS at rest and on coughing until discharge. The incidences of daily moderate-to-severe pain were defined as the proportion of patients with daily VAS score ≥4 at least once. The incidence of moderate-to-severe pain at rest during hospitalization was 32% and 20% in Group T and Group M, and on coughing was 64% and 35%, respectively, with no statistical significance (Table 2).
 |
Table 2 Evaluation of Patients’ Opioid Dosage and Analgesic Effect in Preliminary Study |
There was no significant difference in the average mechanical ventilation time, ICU and hospital length of stay. The incidences of complications in-hospital of the two groups were similar (Table 3).
 |
Table 3 Comparison of Patients’ Prognosis Indicators in Preliminary Study |
We calculated the sample size based on the incidence of moderate-to-severe pain on coughing during hospitalization of our preliminary study, with a power of 80% and significance level of 5%.
Our multimodal analgesic regimen design is reasonable to control the pain after cardiac surgery, which did not affect early postoperative mobilization. The incidence of chronic pain is also within the reasonable range.
Firstly, most of our patients experienced mild-to-moderate pain rather than severe pain. Pain severity can be classified as mild or no pain (VAS score, 0–3), moderate pain (VAS score, 4–6), severe pain (VAS score, 7–8) and extreme pain (VAS score, 9–10) according to the VAS score. It was reported that pulmonary, cardiovascular and psychological complications increased in patients suffered moderate above pain.3–5 Therefore, we combined moderate pain with severe pain as moderate-to-severe pain. There were no patients suffered from extreme pain, no patients suffered from severe pain at rest and very few suffered from severe pain on coughing in our study (Table 4).
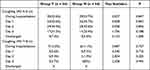 |
Table 4 Evaluation of Patients’ Analgesic Effect on Coughing (According to Our Published Data) |
Secondly, even if the patient had moderate-to-severe pain, the frequency of pain was low. We used a very strict definition of the incidences of daily moderate-to-severe pain after surgery. The daily incidence was the proportion of patients with daily VAS score ≥4 at least once, and the incidence during hospitalization was defined as the proportion of patients with VAS score on coughing ≥4 at least once during hospitalization. Patients were assessed twice a day (7am-9am and 7pm-9pm). The recorded VAS score was not the instant score at the follow-up time point, but the highest VAS score during the period from the last to the current follow-up time point. While the VAS score was greater than or equal to 4, even if only once after surgery, we considered the patient had moderate-to-severe pain.
Finally, for most patients, even if moderate-to-severe pain occurred, early postoperative mobilization was not affected by timely analgesic treatment. Patient controlled intravenous analgesia (PCIA) pump with sufentanil was used for all patients. The training of using PCIA pumps was carried out twice, during preoperative visit and after tracheal extubation. When suffered from moderate-to-severe pain, patients might use PCIA to relieve pain. If pain could not be relieved after 3 PCIA consecutive bolus or the patient could not tolerate the side effects, rescue analgesia was provided immediately. So, the pain was quickly controlled and should not last long time. This might also be the reason for the high rate of remedial analgesia.
Early activity strategy after cardiac surgery in our hospital includes: moving legs and feet, turning over and sitting up in bed with the help of medical staffs or relatives before drainage tube removal; getting out of bed as soon as possible, standing and adapting physical activity by the bed, and walking in the ward every day after the drainage tube is pulled out.
In terms of chronic pain in our study, the incidence of chronic pain at 3 months and 12 months was consistent with previous reports.6,7 The reason for the high incidence might be related to our telephone follow-up. The patients were more likely to express pain and discomfort when they aimed to get more attention with telephone follow-up, which we had explained in the discussion section.1 We discussed with the surgical follow-up specialists, who reported that the incidence of chronic pain was lower than 50%. We would design more scientific questionnaires for more realistic data in the future.
Nerve block is recommended to constitute multimodal analgesia,8,9 that reduce the stress response and opioid consumption. However, the purpose of our study was to explore the feasibility of multimodal regimen by paracetamol, gabapentin, ketamine, lidocaine, dexmedetomidine and sufentanil among cardiac surgery, and compare the analgesia efficacy with conventional sufentanil-based regimen. Our study did not involve nerve blocks nor other components of ERACS. One multicenter study of the application of ERAS protocols including nerve block in cardiac surgery is led by our department and will be finished soon (Ethics approval number: B2020-246, Clinical trial registry number: NCT04642274).
Disclosure
The authors report no conflicts of interest in this communication.
References
1. Jin L, Liang Y, Yu Y, et al. Evaluation of the effect of new multimodal analgesia regimen for cardiac surgery: a prospective, randomized controlled, single-center clinical study. Drug Des Devel Ther. 2023;17:1665–1677. doi:10.2147/DDDT.S406929
2. Chen PS, Xue FS, Li CW. Evaluation of the effect of new multimodal analgesia regimen for cardiac surgery: a prospective, randomized controlled, single-center clinical study [letter]. Drug Des Devel Ther. 2023;17:2353–2354. doi:10.2147/DDDT.S429365
3. Ballantyne JC, Carr DB, deFerranti S, et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. Anesth Analg. 1998;86(3):
4. Gousheh SM, Nesioonpour S, Javaher Foroosh F, et al. Intravenous paracetamol for postoperative analgesia in laparoscopic cholecystectomy. Anesth Pain Med. 2013;3(1):214–218. doi:10.5812/aapm.9880
5. Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–157. doi:10.1016/j.jpain.2015.12.008
6. Yu H, Xu Z, Dai SH, et al. The effect of propofol versus volatile anesthetics on persistent pain after cardiac surgery: a randomized controlled trial. J Cardiothorac Vasc Anesth. 2021;35(8):2438–2446. doi:10.1053/j.jvca.2020.10.025
7. Subramaniam K, Ibarra A, Ruppert K, et al. Intraoperative remifentanil infusion and postoperative pain outcomes after cardiac surgery-results from secondary analysis of a randomized, open-label clinical trial. J Cardiothorac Vasc Anesth. 2021;35(2):458–466. doi:10.1053/j.jvca.2020.08.064
8. Small C, Laycock H. Acute postoperative pain management. Br J Surg. 2020;107(2):e70–e80. doi:10.1002/bjs.11477
9. King M, Stambulic T, Hassan SMA, et al. Median sternotomy pain after cardiac surgery: to block, or not? A systematic review and meta-analysis. J Card Surg. 2022;37(11):3729–3742. doi:10.1111/jocs.16882
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
