Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Evaluation of miRNA Expression in Patients with Gestational Diabetes Mellitus: Investigating Diagnostic Potential and Clinical Implications
Authors Kunysz M , Cieśla M, Darmochwał-Kolarz D
Received 1 November 2023
Accepted for publication 24 January 2024
Published 23 February 2024 Volume 2024:17 Pages 881—891
DOI https://doi.org/10.2147/DMSO.S443755
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Mateusz Kunysz,1 Marek Cieśla,2 Dorota Darmochwał-Kolarz1
1Department of Obstetrics & Gynecology, Institute of Medical Sciences, College of Medical Sciences, University of Rzeszow, Rzeszow, 35-959, Poland; 2College of Medical Sciences, University of Rzeszow, Rzeszow, 35-959, Poland
Correspondence: Mateusz Kunysz, Email [email protected]
Purpose: Gestational diabetes mellitus (GDM) is common pregnancy complication (8%), characterized by hyperglycemia resulting from pathological homeostatic mechanisms. There’s a concerning trend of increasing GDM prevalence. New markers, particularly epigenetic ones, are sought for early detection and enhanced care. miRNA are small non-coding RNA molecules. The main goal was to investigate the potential role of miRNA (miR-16-5p, miR-222-3p, miR-21-5p) in GDM and their association with clinical features.
Patients and Methods: The study included 72 pregnant patients, with 42 having GDM and 30 in the control group. miRNA expression was measured using ELISA.
Results: There were no significant differences in miR-222-3p expression between GDM patients and the control group. The GDM group exhibited a positive correlation between miR-16-5p expression and miR-21-5p expression as well as between miR-16-5p expression and insulin resistance. In the GDM group, a positive correlation was observed between miR-21-5p expression and fasting glucose levels.
Conclusion: Results do not confirm the role of miR-222-3p in GDM pathogenesis or as a diagnostic marker. Additionally, a role for miR-16-5p in GDM pathogenesis was observed. Furthermore, a potential role for miR-21-5p in monitoring GDM treatment is indicated.
Keywords: gestational diabetes mellitus, miRNA, epigenetics, miR-16-5p, miR-222-3p, miR-21-5p
Introduction
Gestational diabetes mellitus (GDM) is the most commonly occurring complication in pregnancy characterized by hyperglycemia resulting from pathological homeostatic mechanisms; it is estimated to affect around 5.7% of pregnant women.1,2 The World Health Organization (WHO) recommends conducting a screening glucose tolerance test (75g) for all pregnant women between the 24th and 28th week of pregnancy. It is also recommended to perform an early glucose tolerance test for pregnant women with risk factors such as obesity (BMI over 30 kg/m2), a history of GDM, pre-diabetes, HbA1c of 5.7%, polycystic ovary syndrome, first-degree relative with diabetes, pre-existing hypertension, or a history of delivering a baby weighing over 4000g in a previous pregnancy.2,3 Known risk factors for increased occurrence of diabetes include advanced maternal age, overweight and obesity especially before pregnancy, excessive weight gain during pregnancy, lack of physical activity, poor diet, race, and family history.4 Additional risk factors include a history of intrauterine death, hypertension, and giving birth to a child with a developmental defect.
If GDM is not accurately diagnosed and properly treated, it can lead to negative consequences during pregnancy for both the mother and the developing fetus.5–8 Maternal complications may include an increased risk of cesarean section, peripartum trauma, and postpartum hemorrhage. Pregnant women with GDM also have an increased risk of developing preeclampsia or pregnancy-induced hypertension.7 Fetal complications depend on the duration of exposure. In the first trimester, hyperglycemia largely affects organogenesis and is responsible for spontaneous miscarriages and congenital malformations. In the second and third trimesters, the fetus is exposed to excessive growth and future metabolic burden, as well as systemic immaturity after birth. This can lead to peripartum trauma, chronic hypoxia, and even intrauterine death.9 Far-reaching effects are observed in adult life, where maternal programming and hyperglycemia during pregnancy influence the risk of metabolic syndrome as well as eating disorders and glucose tolerance.10,11
Epigenetic regulatory mechanisms in diabetes are divided into DNA methylation, histone modifications, and non-coding RNA (ncRNA). Non-coding RNA, which are not transcribed into proteins, constitute a significant part of RNA in cells (95–98%). Among ncRNA are molecules such as transfer RNA (tRNA) and ribosomal RNA (rRNA), as well as functionally significant RNA such as long ncRNA and microRNA (miRNA).12
miRNA are small non-coding RNA molecules, first described in the Caenorhabditis elegans organism.13 These genes encoding molecules usually occur in clusters and consist of about 20 nucleotides. Their main function is to regulate gene expression, both in terms of inhibition and stimulation. Inhibition of gene expression involves increased degradation of mRNA molecules or weakened translation, while stimulation involves an increase in the rate of translation. miRNA molecules can bind to many sites, not only within a single gene.14,15 miRNA can be found in various tissues. Together with proteins and lipids, they form complex structures, and they can also be found in vesicles in the extracellular fluid. This contributes to their exceptional stability in the body.16–20
So far, over 2000 miRNA molecules have been identified in the human body. A single circRNA molecule can simultaneously interact with multiple miRNA molecules, further emphasizing their complex regulatory functions.21,22 miRNAs have high stability in the serum due to the absence of exonucleases in this biological material. miRNA can be associated with proteins (outside vesicles) or be located inside vesicles.23 Cells use exosomes (small vesicles) to transmit important information to other cells, often over long distances.
Exosomes are small (30–100 nm), membrane-bound vesicles originating from endocytosis, which are released into the extracellular environment through the fusion of multivesicular bodies with the cell membrane. Microvesicles containing miRNA enable intercellular and intertissue communication in the body.24,25 Most miRNA in the serum associated with tumors are strongly correlated with their levels in blood cells.26 They serve as potential biomarkers for disease diagnosis, prognosis, and monitoring treatment responses. Moreover, manipulating miRNA levels through various strategies, such as miRNA mimics or inhibitors, holds promise for developing innovative therapeutic approaches for diverse diseases. There is a great interest in understanding the exact mechanism by which miRNA enters biological fluids such as serum, and whether they have biological activity or are merely biomarkers for unknown etiological factors. miRNA are ideal candidates as biomarkers because the technologies used to detect them are specific and sensitive.27 Detecting diabetes in pregnant women at an early stage is a crucial diagnostic element due to the prevention of maternal and fetal complications. Currently, new markers are still being sought to enable the rapid diagnosis of the disease and to identify a group of patients who are more prone to diabetes in order to provide them with intensive care. Profiling miRNA expression patterns in individuals can aid in adjusting therapeutic strategies specific to a patient’s unique molecular characteristics, potentially improving treatment outcomes. Epigenetics is currently one of the significant directions in the development of medicine. The real requirement of miRNA research lies in comprehending their roles in gene regulation, disease mechanisms, and their diagnostic and therapeutic potential.
The current glucose tolerance test is inconvenient for women. It involves consuming a large, unnecessary amount of sugar. Drawing blood three times is uncomfortable for the patient and time-consuming. Additionally, it is performed late in pregnancy. Taste preferences and unnecessary fetal exposure are further arguments for exploring other diagnostic methods.
The main problem of the research is if the concentration of selected miRNAs play a role in the pathogenesis, in the diagnosis and in the monitoring of the disease.
Materials and Methods
The studied patients were hospitalized in the Perinatology Subunit of the Clinic of Gynecology, Obstetrics, and Perinatology of Clinical Hospital No. 2 in Rzeszów. The study group included 42 patients with GDM, and the control group comprised 30 patients without GDM.
Each patient was extensively briefed on the purpose of the study, and written consent for participation in the study was obtained. The study was conducted with the approval of the Bioethics Committee of the University of Rzeszow (Approval No. 4/02/2020). Inclusion criteria were pregnant patients with diabetes diagnosed during pregnancy based on the oral glucose tolerance test (OGTT, 75g). The authors confirm that study complies with Declaration of Helsinki.
Peripheral blood from pregnant women was used as the research material, collected from the cubital vein. Part of the material was used to determine peripheral blood morphology. The serum was stored for later miRNA extraction, and until RNA isolation, it was kept at −80°C. The serum was used for biochemical determinations such as glucose concentration, insulin, and C-reactive protein. RNA was isolated using the miRNA/sncRNA Isolation kits from Biovendor. The isolated material was stored at −80°C until further analysis. A Biovendor kit was used to assess the concentration of miRNA in the plasma. The absorbance of each well was determined using an ELISA reader (Tecan Infinite M200 Pro reader with Magellan software version 7.1) set at 450 nm, with a reference wavelength set at 630 nm. The concentration of the tested miRNA was read based on the prepared standard curve.
The analysis was performed using Dell software called Statistica version 13.3. Results were considered statistically significant at p < 0.05.
Results
The study group consisted of 42 patients with GDM diagnosed after performing the glucose tolerance test, hospitalized in the Perinatology Subunit of the Clinic of Gynecology, Obstetrics, and Perinatology of Clinical Hospital No. 2 in Rzeszów.
The control group comprised 30 patients without GDM. A statistically significant difference in age was shown between the control group and the study group (p = 0.015). The median age for GDM was 33.5, and for the control group, it was 30. In the study group, 25 patients (59.52%) were treated with both diet and insulin, while 17 patients (40.48%) were treated only with diet. It was observed that the birth weight of newborns of patients with GDM was statistically significantly higher compared to newborns of mothers in the control group. In the study group of patients with GDM, BMI was statistically significantly higher compared to the control group. Those values are shown on Table 1.
 |
Table 1 Characteristics of Groups |
Regarding miR-16-5p, in the group of patients with GDM, a positive correlation was found with miR-21-5p (p = 0.03) and the HOMA-IR index (p<0,05) as shown in Figures 1 and 2.
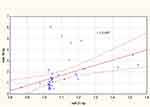 |
Figure 1 Correlation between miR-16-5p and miR-21-5p. |
 |
Figure 2 Correlation between miR-16-5p and HOMA-IR. |
The concentration of miR-222-3p did not differ significantly in both study groups (p ≥ 0.05) as shown in Figure 3.
 |
Figure 3 Box plot of miR-222-3p concentration in both groups. |
In the group of patients with GDM, a positive correlation was found between the expression of miR-21-5p and fasting glucose concentration (p<0.05) as in Figure 4.
 |
Figure 4 Correlation between miR-21-5p and glucose level. |
Discussion
Over the past few decades, the incidence of GDM has been increasing at a rapid pace, causing significant concerns both in the medical community and governmental organizations, mainly due to the lack of effective prevention strategies for diabetes.
miRNA is a type of non-coding RNA molecule composed of approximately 20–22 nucleotides. They play a crucial role in gene expression at the epigenetic level and are involved in various cellular processes. In recent years, miRNA has emerged as a promising tool for both diagnosis and therapy due to its association with GDM. Relationship between miRNA and gestational diabetes draws inspiration from previous studies that have demonstrated significant associations between miRNA and diabetes mellitus. These earlier works have unveiled the substantial role of miRNA in the development of various types of diabetes, prompting the search for similar correlations in the context of gestational diabetes. The existing body of knowledge suggests that miRNA may play a crucial role in the pathophysiological mechanisms associated with diabetes, motivating researchers to delve into this issue concerning the specific conditions present in gestational diabetes. One study concerning type 1 diabetes mellitus revealed relationship between levels of miR-146-5p, miR-155 and miR-375.28 Another one found that some miRNAs correlated with hyperglycemia and HbA1C in patients with T1DM.29
Some studies have examined the association between circulating levels of miRNAs with T2DM.30 Yang et al observed diminished levels of certain miRNAs in individuals with T2DM in contrast to the control cohorts, whereas Prabu et al identified an increase in three miRNAs and a decrease in one specific miRNA.31,32 Various miRNAs as miR-29, miR-200 and miR-30d family contribute to diabetic complications by targeting genes involved in cholesterol and glucose metabolism, and inflammation.30,33
The results of many studies suggest that miR-16-5p influences insulin sensitivity. miR-16-5p interacts with genes encoding insulin receptor substrate proteins 1 and 2. Increased miR-16-5p activity leads to reduced expression of IRS1 and IRS2, potentially causing aberrant Wnt//beta-catenin signaling, and consequently contributing to diabetes. Reduced levels of IRS1 and IRS2 also inhibit insulin signaling, leading to insulin resistance. Moreover, it mediates insulin-like growth factor-I (IGF-I).34–36
One of the proposed mechanisms of action of miR-222-3p in the pathophysiology of GDM is based on the direct activation of estrogen receptors.37 miR-222-3p is located on chromosome Xp11.3, and its upregulation may be involved in the regulation of the cell cycle through the control of cyclin-dependent kinase inhibitor expression (p27Kip1). It acts regulating the expression of estrogen receptor-α (ER-α) in estrogen-induced insulin resistance in GDM.38–40
miR-21-5p is located on chromosome 17 and shows a very high inter-species genetic similarity. Its promoter contains certain enhancer elements that are conserved and include binding sites for several specific genes, such as STAT3, p53, AP-1, Ets/PU1, C/EBPa, NFI, and SRF. miR depletion in a pancreatic cancer model led to increased apoptosis of malignant cells, inhibiting tumor growth. In pancreatic β-cells of mice with a model of T1D, NF-κB increased miR-21 levels, while miR-21 decreased the level of PDCD4, an inducer of apoptosis, indicating a role in insulin resistance.41–45
In their study, Cao et al assessed the serum concentration of miR-16-5p using a method known as quantitative reverse transcription polymerase chain reaction (qRT-PCR).46 They observed significantly increased expression of miR-16-5p and a positive correlation between insulin resistance and miR-16-5p concentration. Hocaoglu et al also examined the expression of miR-16p-5p in patients with a prior history of PCOS during the diagnosis of GDM. They examined the miRNA concentration in leukocytes.47 qRT-PCR was performed to measure microRNA expression levels. miR-16-5p was correlated with gestational age and fasting glucose levels. In the second study, miR-16-5p expression was assessed in leukocytes in patients with preeclampsia, GDM, and both PE and GDM, in comparison to healthy pregnant women.48 No significant differences in miR-16-5p expression levels were observed. Furthermore, in the GDM-PE group, a negative correlation between miR-16-5p and fasting glucose levels was observed. Zhu et al measured the concentration of miR-16-5p in serum between the 16th and 19th week of pregnancy.49 Determination was done using qRT-PCR. Significantly increased expression of miR-16-5p was observed. Juchnicka and team also found high expression of miR-16-5p in blood serum in women before the onset of GDM.50 This difference was evident between the 9th and 12th weeks of pregnancy. Furthermore, they observed a positive correlation with the HOMA-IR index. Blood serum was used for analysis. Circulating miRNAs were measured using the NanoString platform for quantitative measurements. Pheiffer et al analyzed miRNA expression in serum using quantitative real-time polymerase chain reaction (qRT-PCR).51 In this group, miR-16-5p was lower in women with GDM compared to the control group, but not statistically significant. In a study of women in the second trimester of pregnancy with singleton pregnancies, conducted by Martínez-Ibarra and their team, no significant differences in miR-16-5p expression levels in serum were observed.52 In this case, qRT-PCR was used for analysis. In the study by Balci et al, it was shown that the derivative product of miR-16-5p exhibits weaker expression, but without statistical significance. Plasma was analyzed using the qRT-PCR method.53 Tagoma and others did not find statistically significant differences in the studied group of patients.54 The expression profile of plasma miRNAs in pregnant women with GDM was determined and compared with profiles in control pregnant women using real-time PCR.
In our studies, no differences were found in the concentration of miR-16-5p in the studied group of patients compared to the control group. This result is consistent with part of the mentioned studies. However, a positive correlation was observed between the concentration of miR-16-5p and the HOMA-IR index. These results suggest a potential role of miR-16-5p expression in the pathogenesis of GDM.
In the study by Pheifer et al, the level of miR-222-3p in blood serum was assessed using the RT-PCR method.51 Levels of miR-222-3p were significantly reduced in women with GDM compared to the control group. Furthermore, miRNAs were profiled in both serum and exosomal vesicles in patients with GDM using RT-qPCR. Levels of miR-222-3p correlated with fasting glucose levels and birth weight.40 In another study conducted by Tagoma et al, a significant increase in miR-222-3p expression was observed.54 Serum samples were collected and assessed by qRT-PCR. In the study by Radojičić et al, no association was found between miR-222-3p.37 miR-222-3p was assessed in peripheral blood mononuclear cells. In the study conducted by Wander et al, no statistically significant differences were found for miR-222-3p.55 Serum of patients was examined using the qRT-PCR method.
In our work no statistically significant differences were found in both studied groups regarding the expression of miR-222-3p.
In the study by Wander et al, the authors found that elevated levels of miR-21-5p in serum were associated with a later risk of developing GDM.55 The association was observed only in women who were overweight or obese before pregnancy. Additionally, the risk of developing GDM was observed only in mothers carrying male fetuses. In the study conducted by Hocaoglu and team, a significant decrease in miR-21-5p expression levels was observed in the GDM and preeclampsia (PE) groups compared to the control group.47 Furthermore, no significant differences were observed between the expression levels in the PE-GDM group. In the control group, a significantly positive correlation was observed between the levels of miR-16-5p and miR-21-5p. This was the first study evaluating the expression of miRs in maternal blood leukocytes in patients with concurrent PE and GDM.
In our study no statistically significant differences were found in the expression of miR-21-5p in both studied groups. In the group of patients with GDM, a relationship was observed between miR-21-5p and miR-16-5p and fasting glucose levels. The above-mentioned results suggest a potential role of miR-21-5p expression in monitoring the treatment of patients with GDM. Table 2 contains studies on gestational diabetes mellitus and miRNA.
 |
Table 2 Summary of Studies on Gestational Diabetes and miRNAs |
In this study, the impact of specific miRNAs was analyzed to discover more accurate and useful predictive and prognostic markers in patients with GDM. The author’s research, as the first, evaluates the relationship between the expression of miR-21-5p, miR-16-5p, and miR-222-3p, and GDM using the enzyme-linked immunosorbent assay (ELISA) method. It is worth noting that the expression levels were assessed in plasma samples, which significantly facilitates its potential use as a marker. Additionally, the method of determining expression is shorter and easier to conduct.
The conducted studies do not indicate significant differences between the groups in terms of miR-21-5p, miR-16-5p, and miR-222-3p. The enzyme-linked immunosorbent assay (ELISA) method does not find confirmation in detecting differences between the groups. One proposed explanation could be the low expression of miRNAs in serum. For low concentrations, PCR is more sensitive method. Additionally, in the conducted studies, a highly heterogeneous selection of the study group was chosen. The ELISA method, despite its wide usefulness, may encounter certain limitations in detecting subtle differences between groups. The PCR technique allows for the amplification of even single copies of DNA, increasing its ability to detect minimal amounts of the target genetic material. This enables achieving a higher detection limit in determining miRNA concentrations and identifying potential differences between groups.
A crucial aspect of the study is the stage at which patients are included in the study. If groups of patients at different stages of the disease are included in the analysis, significant differences in miRNA expression may exist due to the dynamic nature of diabetes. Patients at different stages of the disease may have varied levels of miRNA expression, which can affect the interpretation of results.
Another factor that can significantly impact the study results is the level of diabetes control. Patients with better glycemic control may have a different miRNA profile than patients with unstable diabetes. Normalizing blood glucose levels can affect gene regulation through miRNA and influence differences between the studied groups.
Additionally, comorbidities can be a factor affecting the study results. Patients with additional conditions such as hypertension or thyroid dysfunction may have altered miRNA profiles compared to patients without these conditions. Variability in the number of blood cells can also impact the results. It is also important to note the impact of various diabetes treatment methods on the study results. Patients undergoing different therapies, such as insulin therapy or dietary interventions, may exhibit different miRNA profiles.
Nevertheless, during the analysis, some interesting correlations were found between the results and the characteristics of diabetes. This observation suggests the potential application of the ELISA method in miRNA research and indicates that it can yield significant insights. The discovery of these correlations demonstrates that the ELISA method can be a valuable tool for analyzing miRNA levels in samples from patients with different diabetes traits.
In summary, although many different miRNAs have already been identified, their exact biological functions are not yet fully understood. Due to the dynamic progress in research utilizing methods for expression analysis through next-generation sequencing and other advanced analytical techniques, the prospect of using these molecules in the field of diagnosis, therapy, and prognostic indicators for GDM is becoming increasingly feasible. Therefore, there is justification for continuing research on the biological function of miRNAs. This study may be significant in the search for new meaningful prognostic indicators that have substantial relevance for patients with GDM.
Hence, while the study may be limited by certain aspects, the discovered correlations and procedural correctness may provide arguments for further research employing the ELISA methods in miRNA studies related to diabetes. The combination of these results suggests that this method may provide valuable information about miRNA concentrations in the population of patients with diabetes.
Conclusion
In our own research, no statistically significant differences were observed regarding the concentration of miR-222-3p in the group of patients with GDM compared to the control group. The results do not confirm the role of miR-222-3p in the pathogenesis of GDM, nor its role as a potential diagnostic marker in GDM. In the group of patients with GDM, a positive correlation was found between the concentration of miR-16-5p and the insulin resistance index HOMA-IR. The positive correlation found between its concentration and the insulin resistance index (HOMA-IR) within the GDM group suggests a potential involvement in the pathogenesis of GDM, particularly in relation to insulin resistance. In the group of patients with GDM, a positive correlation was observed between the concentration of miR-21-5p and fasting glucose levels. As fasting glucose levels are a critical parameter in assessing glycemic control and treatment response in GDM, the association between miR-21-5p expression and fasting glucose levels suggests that this miRNA might be involved in regulating glucose metabolism or could serve as a biomarker for monitoring the response to GDM treatment strategies. The results suggest a potential role of miR-21-5p expression in monitoring treatment in patients with GDM. In summary, while miR-222-3p does not appear to have a significant role in GDM or as a diagnostic marker, miR-16-5p and miR-21-5p show potential implications in the context of GDM pathogenesis and monitoring of the disease, respectively. Understanding these miRNAs’ precise roles could potentially lead to the development of more targeted and effective therapeutic interventions or diagnostic approaches for GDM. Therefore, continued research into the functions and implications of these miRNAs in the context of GDM remains critical for advancing our knowledge and improving clinical outcomes for affected individuals.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Eades CE, Cameron DM, Evans JMM. Prevalence of gestational diabetes mellitus in Europe: a meta-analysis. Diabetes Res Clin Pract. 2017;129:173–181. doi:10.1016/j.diabres.2017.03
2. Hod M, Kapur A, Sacks DA, et al. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: a pragmatic guide for diagnosis, management, and care#. Int J Gynecol Obstet. 2015;131:S173. doi:10.1016/S0020-7292(15)30007-2
3. Caughey AB, Turrentine M. ACOG practice bulletin no. 190: gestational diabetes mellitus. Obstetrics Gynecol. 2018;131(2):e49. doi:10.1097/AOG.0000000000002501
4. Alejandro EU, Mamerto TP, Chung G, et al. Gestational diabetes mellitus: a harbinger of the vicious cycle of diabetes. Int J Mol Sci. 2020;21(14):5003. doi:10.3390/ijms21145003
5. Szmuilowicz ED, Josefson JL, Metzger BE. Endocrinology and METABOLISM CLInics of North America. Gestational Diabetes Mellitus. 2019;48(3):479–493. doi:10.1016/j.ecl.2019.05.001
6. Yu Y, Arah OA, Liew Z, et al. Maternal diabetes during pregnancy and early onset of cardiovascular disease in offspring: population based cohort study with 40 years of follow-up. BMJ. 2019:l6398. doi:10.1136/bmj.l6398
7. Metzger BE, Lowe LP; HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991–2002. doi:10.1056/NEJMoa0707943
8. Metzger BE, Persson B, Lowe LP, et al. Hyperglycemia and adverse pregnancy outcome study: neonatal glycemia. Pediatrics. 2010;126(6):e1545–e1552. doi:10.1542/peds.2009-2257
9. Reece EA. The fetal and maternal consequences of gestational diabetes mellitus. J Matern Fetal Neonatal Med. 2010;23(3):199–203. doi:10.3109/14767050903550659
10. Ornoy A, Becker M, Weinstein-Fudim L, Ergaz Z. Diabetes during pregnancy: a maternal disease complicating the course of pregnancy with long-term deleterious effects on the offspring. A clinical review. Int J Mol Sci. 2021;22(6):2965. doi:10.3390/ijms22062965
11. Atègbo JM, Grissa O, Yessoufou A, et al. Modulation of adipokines and cytokines in gestational diabetes and macrosomia. J Clin Endocrinol Metab. 2006;91(10):4137–4143. doi:10.1210/jc.2006-0980
12. Mattick JS, Lee JT. The genetic signatures of noncoding RNAs. PLoS Genet. 2009;5(4):e1000459. doi:10.1371/journal.pgen.1000459
13. Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75(5):843–854. doi:10.1016/0092-8674(93)90529-y
14. He L, Hannon GJ. MicroRNAs: small RNAs with a big role in gene regulation. Nat Rev Genet. 2004;5(7):522–531. doi:10.1038/nrg1379
15. Vishnoi A, Rani S. MiRNA biogenesis and regulation of diseases: an overview. In: Rani S, editor. MicroRNA Profiling. Vol 1509. Methods in Molecular Biology. New York: Springer; 2017:1–10. doi:10.1007/978-1-4939-6524-3_1
16. Cortez MA, Bueso-Ramos C, Ferdin J, Lopez-Berestein G, Sood AK, Calin GA. MicroRNAs in body fluids—the mix of hormones and biomarkers. Nat Rev Clin Oncol. 2011;8(8):467–477. doi:10.1038/nrclinonc.2011.76
17. Lu J, Clark AG. Impact of microRNA regulation on variation in human gene expression. Genome Res. 2012;22(7):1243–1254. doi:10.1101/gr.132514.111
18. Okamura K, Hagen JW, Duan H, Tyler DM, Lai EC. The mirtron pathway generates microRNA-class regulatory RNAs in Drosophila. Cell. 2007;130(1):89–100. doi:10.1016/j.cell.2007.06.028
19. Isik M, Berezikov E. Expression pattern analysis of microRNAs in Caenorhabditis elegans. Methods Mol Biol. 2013;936:129–141. doi:10.1007/978-1-62703-083-0_11
20. Selvakumar SC, Preethi KA, Tusubira D, Sekar D. MicroRNAs in the epigenetic regulation of disease progression in Parkinson’s disease. Front Cell Neurosci. 2022;16. doi:10.3389/fncel.2022.995997
21. Hsiao KY, Sun HS, Tsai SJ. Circular RNA – new member of noncoding RNA with novel functions. Exp Biol Med. 2017;242(11):1136–1141. doi:10.1177/1535370217708978
22. Zheng Q, Bao C, Guo W, et al. Circular RNA profiling reveals an abundant circHIPK3 that regulates cell growth by sponging multiple miRNAs. Nat Commun. 2016;7(1):11215. doi:10.1038/ncomms11215
23. Turchinovich A, Weiz L, Burwinkel B. Extracellular miRNAs: the mystery of their origin and function. Trends Biochem Sci. 2012;37(11):460–465. doi:10.1016/j.tibs.2012.08.003
24. Wittmann J, Jäck HM. Serum microRNAs as powerful cancer biomarkers. Biochim Biophys Acta Rev Cancer. 2010;1806(2):200–207. doi:10.1016/j.bbcan.2010.07.002
25. Jayabalan N, Nair S, Nuzhat Z, et al. Cross talk between adipose tissue and placenta in obese and gestational diabetes mellitus pregnancies via exosomes. Front Endocrinol. 2017;8:239. doi:10.3389/fendo.2017.00239
26. McDonald JS, Milosevic D, Reddi HV, Grebe SK, Algeciras-Schimnich A. Analysis of circulating microRNA: preanalytical and analytical challenges. Clin Chem. 2011;57(6):833–840. doi:10.1373/clinchem.2010.157198
27. Chen X, Ba Y, Ma L, et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 2008;18(10):997–1006. doi:10.1038/cr.2008.282
28. Assmann TS, Recamonde-Mendoza M, De Souza BM, Crispim D. MicroRNA expression profiles and type 1 diabetes mellitus: systematic review and bioinformatic analysis. Endocr Connect. 2017;6(8):773–790. doi:10.1530/EC-17-0248
29. Satake E, Pezzolesi MG, Md Dom ZI, Smiles AM, Niewczas MA, Krolewski AS. Circulating miRNA profiles associated with hyperglycemia in patients with type 1 diabetes. Diabetes. 2018;67(5):1013–1023. doi:10.2337/db17-1207
30. Zhang Y, Bai R, Liu C, et al. MicroRNA single‐nucleotide polymorphisms and diabetes mellitus: a comprehensive review. Clin Genet. 2019;95(4):451–461. doi:10.1111/cge.13491
31. Yang Z, Chen H, Si H, et al. Serum miR-23a, a potential biomarker for diagnosis of pre-diabetes and type 2 diabetes. Acta Diabetol. 2014;51(5):823–831. doi:10.1007/s00592-014-0617-8
32. Prabu P, Rome S, Sathishkumar C, et al. MicroRNAs from urinary extracellular vesicles are non-invasive early biomarkers of diabetic nephropathy in type 2 diabetes patients with the “Asian Indian phenotype”. Diabetes Metab. 2019;45(3):276–285. doi:10.1016/j.diabet.2018.08.004
33. Saliminejad K, Khorram Khorshid HR, Soleymani Fard S, Ghaffari SH. An overview of microRNAs: biology, functions, therapeutics, and analysis methods. J Cell Physiol. 2019;234(5):5451–5465. doi:10.1002/jcp.27486
34. Gao X, Zhao S. miRNA-16-5p inhibits the apoptosis of high glucose-induced pancreatic β cells via targeting of CXCL10: potential biomarkers in type 1 diabetes mellitus. Endokrynologia Polska. 2020;71(5):404–410. doi:10.5603/EP.a2020.0046
35. Chakraborty C, George Priya Doss C, Bandyopadhyay S. miRNAs in insulin resistance and diabetes-associated pancreatic cancer: the “minute and miracle” molecule moving as a monitor in the “genomic galaxy”. Curr Drug Targets. 2013;14(10):1110–1117. doi:10.2174/13894501113149990182
36. da Silva PHCM. MicroRNAs associated with the pathophysiological mechanisms of gestational diabetes mellitus: a systematic review for building a panel of miRNAs. J Pers Med. 2023;13(7):1126. doi:10.3390/jpm13071126
37. Radojičić O, Dobrijević Z, Robajac D, et al. Gestational diabetes is associated with an increased expression of miR-27a in peripheral blood mononuclear cells. Mol Diagn Ther. 2022;26(4):421–435. doi:10.1007/s40291-022-00591-5
38. Miller TE, Ghoshal K, Ramaswamy B, et al. MicroRNA-221/222 confers tamoxifen resistance in breast cancer by targeting p27Kip1. J Biol Chem. 2008;283(44):29897–29903. doi:10.1074/jbc.M804612200
39. Shi Z, Zhao C, Guo X, et al. Differential expression of microRNAs in omental adipose tissue from gestational diabetes mellitus subjects reveals miR-222 as a regulator of ERα expression in estrogen-induced insulin resistance. Endocrinology. 2014;155(5):1982–1990. doi:10.1210/en.2013-2046
40. Filardi T, Catanzaro G, Grieco GE, et al. Identification and validation of miR-222-3p and miR-409-3p as plasma biomarkers in gestational diabetes mellitus sharing validated target genes involved in metabolic homeostasis. IJMS. 2022;23(8):4276. doi:10.3390/ijms23084276
41. Chan JA, Krichevsky AM, Kosik KS. MicroRNA-21 is an antiapoptotic factor in human glioblastoma cells. Cancer Res. 2005;65(14):6029–6033. doi:10.1158/0008-5472.CAN-05-0137
42. Liu S, Wu W, Liao J, et al. MicroRNA-21: a critical pathogenic factor of diabetic nephropathy. Front Endocrinol. 2022;13:895010. doi:10.3389/fendo.2022.895010
43. Krichevsky AM, Gabriely G. miR-21: a small multi-faceted RNA. J Cell Mol Med. 2009;13(1):39–53. doi:10.1111/j.1582-4934.2008.00556.x
44. Ruan Q, Wang T, Kameswaran V, et al. The microRNA-21-PDCD4 axis prevents type 1 diabetes by blocking pancreatic beta cell death. Proc Natl Acad Sci U S A. 2011;108(29):12030–12035. doi:10.1073/pnas.1101450108
45. Sicard F, Gayral M, Lulka H, Buscail L, Cordelier P. Targeting miR-21 for the therapy of pancreatic cancer. Mol Ther. 2013;21(5):986–994. doi:10.1038/mt.2013.35
46. Cao YL, Jia YJ, Xing BH, Shi DD, Dong XJ. Plasma microRNA-16-5p, −17-5p and −20a-5p: novel diagnostic biomarkers for gestational diabetes mellitus. J Obstet Gynaecol Res. 2017;43(6):974–981. doi:10.1111/jog.13317
47. Hocaoglu M, Demirer S, Loclar Karaalp I, et al. Identification of miR-16-5p and miR-155-5p microRNAs differentially expressed in circulating leukocytes of pregnant women with polycystic ovary syndrome and gestational diabetes. Gynecol Endocrinol. 2021;37(3):216–220. doi:10.1080/09513590.2020.1843620
48. Hocaoglu M, Demirer S, Senturk H, Turgut A, Komurcu-Bayrak E. Differential expression of candidate circulating microRNAs in maternal blood leukocytes of the patients with preeclampsia and gestational diabetes mellitus. Pregnancy Hypertens. 2019;17:5–11. doi:10.1016/j.preghy.2019.04.004
49. Zhu Y, Tian F, Li H, Zhou Y, Lu J, Ge Q. Profiling maternal plasma microRNA expression in early pregnancy to predict gestational diabetes mellitus. Int J Gynaecol Obstet. 2015;130(1):49–53. doi:10.1016/j.ijgo.2015.01.010
50. Juchnicka I, Kuźmicki M, Niemira M, et al. miRNAs as predictive factors in early diagnosis of gestational diabetes mellitus. Front Endocrinol. 2022;13:839344. doi:10.3389/fendo.2022.839344
51. Pheiffer C, Dias S, Rheeder P, Adam S. Decreased expression of circulating miR-20a-5p in South African women with gestational diabetes mellitus. Mol Diagn Ther. 2018;22(3):345–352. doi:10.1007/s40291-018-0325-0
52. Martínez-Ibarra A, Martínez-Razo LD, Vázquez-Martínez ER, et al. Unhealthy levels of phthalates and bisphenol A in Mexican pregnant women with gestational diabetes and its association to altered expression of miRNAs involved with metabolic disease. IJMS. 2019;20(13):3343. doi:10.3390/ijms20133343
53. Balci S, Gorur A, Yıldırım DD, Cayan F, Tamer L. Expression level of miRNAS in patients with gestational diabetes. Turk JBiochem. 2020;45(6):825–831. doi:10.1515/tjb-2019-0157
54. Tagoma A, Alnek K, Kirss A, Uibo R, Haller-Kikkatalo K. MicroRNA profiling of second trimester maternal plasma shows upregulation of miR-195-5p in patients with gestational diabetes. Gene. 2018;672:137–142. doi:10.1016/j.gene.2018.06.004
55. Wander PL, Boyko EJ, Hevner K, et al. Circulating early- and mid-pregnancy microRNAs and risk of gestational diabetes. Diabet Res Clin Pract. 2017;132:1–9. doi:10.1016/j.diabres.2017.07.024
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
