Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Evaluating Inventory Management Practice of Antiretroviral Drugs in Public Health Facilities of Addis Ababa, Ethiopia
Authors Gemechu F, Ayalew M , Tefera BB , Mulugeta T , Bekele A
Received 3 September 2021
Accepted for publication 10 December 2021
Published 21 December 2021 Volume 2021:13 Pages 1091—1099
DOI https://doi.org/10.2147/HIV.S337479
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Bassel Sawaya
Fenet Gemechu,1 Mihret Ayalew,2 Bereket Bahiru Tefera,3 Temesgen Mulugeta,4 Azmeraw Bekele5
1Department of Pharmacy, Adama Hospital Medical College, Adama, Ethiopia; 2Department of Pharmacology, Institute of Health Science, Jimma University, Jimma, Ethiopia; 3Department of Pharmacy, Debre Markos University, College of Health Science, Debre Markos, Ethiopia; 4Department of Clinical Pharmacy, Institute of Health Science, Jimma University, Jimma, Ethiopia; 5Department of Social and Administrative Pharmacy, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Azmeraw Bekele
Department of Social and Administrative Pharmacy, Institute of Health, Jimma University, Jimma, Ethiopia
Email [email protected]
Background: The right to safe and effective treatment is an exclusive right that depends on the robustness of the domestic health care system.
Methods: A facility-based cross-sectional study was conducted from January 01 to February 01, 2020. Ten eligible hospitals and 12 randomly selected health centers were parts of this study. A total of 66 RRFs and 308 bin cards were reviewed. Data were collected through observation, record and report review, and physical count using an observational checklist. In addition, 44 semi structured interviews were conducted. The collected data were entered to MS Excel sheet and analysed using SPSS (version 20) software. The correlation test result was determined statistically significant at p< 0.05.
Results: Twenty-two public health facilities were included in the study of which 16 (72.72%) health facilities had at least one stock out. Availability of ARVs had very strong positive correlation ship with bin card updating practice (r=0.9 1, P< 0.01), inventory accuracy rate (r=0.912, P< 0.015) and very strong negative correlation ship with wastage rate (r = − 0.66, P< 0.001). The wastage rate due to expiration and loss was 3.9%. The mean bin card accuracy was 90.6%. RRF reports were accurate 17 (77.3%), complete 7(32%) and reported on time 14 (63.64%). Only 8 (36.36%) health facilities met acceptable storage conditions.
Conclusion: The availability of bin cards and reports and resupply forms was promising, but the data quality remains low. The majority of health facilities did not meet acceptable storage conditions and had frequent stock-outs.
Keywords: inventory management, antiretroviral, Addis Ababa
Background
The right to get safe and effective treatment is exclusive. Accordingly, the massive global expansion of access to human immunodeficiency virus (HIV) treatment realizes the right to health but it is not a striated forward effort. Globally, only 35.4% of the people living with HIV have received antiretroviral (ARV) treatment in 2019.1 This is most common in sub-Saharan African countries accounted for two-thirds of global HIV cases, and clients in need of treatment are lost initiating treatment.1–5 In HIV prevention and care programs, drugs should be managed well to secure access to treatment and to maintain the trust of clients. Successful implementation of public health programs requires an uninterrupted supply chain management of inventories.6 Unfortunately, supply chain management of ARV in low- and middle-income countries becomes increasingly difficult with an increasing number of antiretroviral treatments (ART), increasing number of ART sites, diverse nature of treatment regimen, and a limited capacity.7 Persistent access to treatment essentially depends on the robustness of the domestic health care systems to ensure the right product, in the right quantity, in the right condition, is delivered to the right place, at the right time, and for the right cost.6 Without proper inventory management, healthcare facilities are limited to making tactical decisions and run the risk of not being able to supply the most appropriate medication.8 Inadequate staffing and training, lack of adequate storage, lack of adequate resource and unreliable supplies are the main challenges of ARV inventory management practices.9 Similarly, in Nigeria, there was poor reporting of practice, stock out, and poor storage conditions of about HIV program.10 In Tanzania and Côte d’Ivoire, clients changed their treatment plans subordinate to improper inventory management.11,12
Likewise, Ethiopia is one of the most affected sub-Saharan African countries and has implemented an integrated pharmaceutical logistics system to create a robust healthcare system, synthesize the large volume of data, connect all levels of the supply chain and make accurate and timely decisions.13 Despite this effort, most of the health facilities in Addis Ababa have provided inadequate inventory management services, where nearly three-quarters of the health facilities faced stock out of one or more drugs and could not start antiretroviral treatment if patients were positive.14,15 Indeed, evaluating the existing practices helps to save undemanding costs following mismanagement of information.16,17 Therefore, this study is intended to evaluate the inventory management practice of antiretroviral drugs in public health facilities of Addis Ababa, Ethiopia.
Methods
Study Design and Settings
A facility-based cross-sectional descriptive study was conducted from January 1 to February 1, 2020, in Addis Ababa, the capital of Ethiopia. At the time of this study, Addis Ababa has 4,794,00018 resident populations living in 11 sub-cities. Among 110 public health facilities that provided health care services in the city, 93 health facilities were providing ART services for 94,693 (98%)19 clients.
Study Population
Public health facilities providing ART services, pharmacy professionals working in ART units, ARV drugs, bin card records and reporting and resupply forms (RRFs) in health facilities were the study subjects.
Eligibility Criteria
This study included first and second-line ARV drugs commonly managed in selected health facilities. Health posts were excluded because they are used as dispensing units of health centers and their inventory management practices could not be consistent with hospitals and health centers.
Sample Size and Sampling Procedures
The sample size of health facilities was determined based on the logistics indicators assessment tool (LIAT) that recommends taking at least 15% of the total health facilities to increase the generalizability of the study findings.20 At the time of the study, 93 health facilities were providing ART services (11 hospitals and 82 health centers). As the calculated sample size, 93 × 15% = 13.95 ≈ 14 was small to generalize the results. Consequently, the sample size was increased to 25% (93 × 25% = 23.25≈23). Thus, 12 randomly selected health centers and 11 hospitals were included in the study. Unfortunately, 22 health facilities were included in the actual study that one of the hospitals was selected as coronavirus disease-19 treatment center behind the data collection. According to Ethiopia’s integrated pharmaceutical logistics system, each hospital and health center is expected to submit one RRF report every 2 months to the pharmaceutical supply agency hub.21 The LIAT mentions a minimum of six-month logistic reports for service assessment20 and considered by the current study. This entails, each health facility is required to submit three RRF reports (1RRF report every 2 months in 6 months). Therefore, 66 RRF reports were submitted to hubs by a total of 22 health facilities (3 × 22 = 66). In addition, 308 bin card records (14 bin card records of 14 drugs) were reviewed (Figure 1).
 |
Figure 1 Flow diagram showing document and health facility selection in public health facilities of Addis Ababa, January 2020. |
Data Collection Tools and Process
The questionnaire was adapted from the United States Agency for International Development (USAID)/Deliver Project guidelines.20,22 Three data collectors were recruited from health facilities excluded in the actual study. The data collectors were pharmacists and they have attained 4 hours of training provided by one of the researchers. Data collectors collected required data through observation, record and report review, and physical count using an observational checklist. Forty-four interviewer administered interviews were conducted using a semi-structured instrument adapted from the national guidelines.24
Data Quality Assurance
A pilot study was conducted in 5% of health facilities omitted from the actual study and certain contents were modified towards the objectives. Data collectors were trained pharmacists, and the data collection was closely monitored during the data collection process.
Statistical Analysis
After being checked for completeness and consistency, the collected data were entered into MS Excel spreadsheet|2016| and exported to Social Science Statistics Package (SPSS, version-20) Software for statistical analysis. Descriptive statistical analysis was used to determine the frequency, average, and percentage values. The correlation test was computed in which the correlation coefficient (r) was determined statistically significant at p<0.05. Finally, results were presented using texts, tables, and graphs.
Variables and Their Measurements
The target variables, intended to respond to the study objectives, were measured using standardized indicators adapted from various the USAID/ Deliver Project22, (Appendix). Yet, it is difficult to determine the overall performance using a single unit of measurement rather than measuring individual indicators.23,24
- Completeness of reports: a report is considered complete if all the columns for each product listed in the report are filled unless the facility does not manage the product.20
- Timelines of reports: as per the standard operating procedure of the integrated pharmaceutical logistics system of Ethiopia21
- Hospitals and health centers should submit their RRF report to the Ethiopian pharmaceutical agency or zone health department until the 10th day of the month.
- Health centers that send their RRF report via the district health office should submit their RRF to the district health office until the fifth day of the month of the reporting period.
Operational Definitions
Acceptable storage condition: Storage facilities are expected to meet at least 80% of 13 predetermined criteria.24
Bin card update: It had to be updated within the previous 30 days. If the bin card was last updated with a balance of zero and the facility has not received any of that product25; if drugs had no transaction more than 30 days, it was not updated.
Data quality: This indicator represents the data quality of bin card records and RRF reports measured using timeliness, completeness, and accuracy including reporting rate.26
Data accuracy: A data is accurate when there is no discrepancy between stock balances on the bin card record (manual, electronic) compared with the physical count and the balance on the RRF report towards selected items. Inventory accuracy is said to be good if (≥80%).24
Stock-out: the product is stocked out if unavailable in place during facility visit or a balance of zero on the bin card within the last 6 months.
Results
Socio-Demographic Characteristics of Participants
A total of 44 pharmacy professionals participated in this study. Twenty participants were working in hospitals and the rest were from the health centers. The majority, 31 (46.96%), of the participants were pharmacists. Five (25%) of the hospital participants were second-degree holders and most of the participants among health facilities had 3–5 years of service experience (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Study Participants in Public Health Facilities of Addis Ababa, January 2020 |
Availability of Bin Card Records and RRF Reports
This study revealed that bin card records and RRF reports were available in 20 (91%) and 22 (100%), respectively. Bin card records of TDF + 3TC + DTG (300 + 300 + 50) mg; TDF + 3TC + EFV (300 + 300 + 600) mg, EFV 600 mg and AZT + 3TC (300 + 150) mg were fully available (Supplementary Table). Out of updated bin card records, hospitals did the most (Table 2).
 |
Table 2 Availability and Updating Practice of Bin Cards in Public Health Facilities of Addis Ababa, January 2020 (N=22) |
Availability of Antiretroviral Drugs
The availability of ARVs was different among health facilities. For instance, TDF+3TC (300+300) mg, EFV 600mg, LPV/R (200+50) mg, and LPV/R (80mL+20mL) were available among all hospitals. On the other hand, TDF+3TC (300+300) mg, AZT+3TC (300+150) mg, LPV/R (200+50) mg, AZT+3TC (60+30) mg, EFV200 mg, EFV50 mg, LPV/R (80mL+20mL found available in all health centers. Furthermore, TDF+3TC (300+300) mg was the most available drug, while ATV/R (100+25) mg was the most stock out (Table 3). Availability of ARVs had a very strong positive correlation ship with bin card updating practice (r=0.9 1, P<0.01) and the inventory accuracy rate (r=0.912, P<0.015) but there was a very strong negative correlation ship with wastage rate (r = −0.66, P<0.001).
 |
Table 3 Availability of Antiretroviral Drugs in Public Health Facilities of Addis Ababa, January 2020 (N=22) |
Stock Out of Antiretroviral Drugs
The study found that 16 (72.72%) health facilities had at least one drug stock-out lasting in an average of 80 days; varying from 1.43 to 47.4 days. Longer duration of stock out (163 days) recorded for ATV/R (300+100) mg. Indeed, AZT+3TC+NVP (60+30+50) mg and TDF+ 3TC+EFV (300+300+600) mg stocked-outs only in the health centers and LPV/R (80mL+20mL) stocked out only in hospitals (Figure 2).
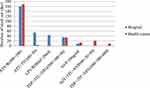 |
Figure 2 Stock out duration of antiretroviral drugs in public health facilities of Addis Ababa, January 2020. |
Data Quality of Bin Card Records
The current study indicated that the data accuracy of bin card records was 90.6. The data accuracy of bin card records reviewed in hospitals ranged from 10 (100%) to 7 (70%) with an average accuracy of 83.6%. On the other hand, the data accuracy of bin card records in the health centers was between 12 (100%) and 10 (83.3%) with an average accuracy of 96.4%. Bin card records of TDF+3TC+EFV (300+300+600) mg were found to be accurate in all health facilities (Supplementary Table). Furthermore, data accuracy of bin card records was varying among drug and facility types (Figure 3).
 |
Figure 3 Bin card accuracy of health facilities by drug type in public health facilities of Addis Ababa, January 2020. |
Data Quality of RRF Reports
The data quality of RRF reports was accurate 17 (77.3%), complete 7(32%), and reported on time 14 (63.64%) with a facility reporting rate of 81.8%. Hospitals and health centers had closely similar trends of reporting on time and accurate RRF reports (Figure 4).
 |
Figure 4 Data quality of RRF reports in public health facilities of Addis Ababa, January 2020. |
Emergency Order and Order Fill Rate
An emergency order is the last resort and falls short to maintain a minimum stock level. The current study, therefore, revealed that 19 (86.4%) health facilities made at least one emergency order within 6 months. The majority of health facilities reported emergency orders in which only 3 (13.6%) health facilities did not have emergency orders. Eleven (57.89%) health facilities made one to three emergency orders and 8(42.1%) health facilities made more than three emergency orders. Hospitals made more frequent emergency orders than the health centers. Furthermore, the order fill rate was 83.3%.
Wasted Stocks and Storage Conditions
Out of 14 ARV drugs, 3.9% were wasted due to expiration and damage; resulting from a cost of $27,839.59 among hospitals, $6555.56, and health centers $21,284.03. The stock value of unused ARVs was less than the usable stock value by 4%. Among the total drugs, TDF+3TC (300+300) mg was the most wasted drug. On the other hand, merely 8(36.36%) health facilities met acceptable storage conditions in only three-fifths of hospitals and two health centers.
Discussion
This study aimed to evaluate inventory management practices of antiretroviral drugs in public health facilities. Inventory data is evaluated to measure if it is recorded and reported in the right quantity, with the right quality, and in the right place at the right time. The present study revealed that an average of 279 (90.6%) bin card records were accurate, which is good and higher than the minimum expected target value (≥80%).24 Accordingly, transferring the exact stock on hand data to bin card record found tolerable but remains unsolved compared to the maximum target value (100%)22 of accurate stock record. Alongside this, transferring accurate stock on hand data to bin card records remains different among hospitals 83.6% and health centers 96.4%. Such inconsistencies could promote stock-outs that cannot be tolerated. The average bin card accuracy of the present study is higher than the finding in East Gojjam (63.8%),27 East Wollega (9.1%),28 and Southern Ethiopia (77%),29 while remaining below a study finding in Kenya (92.31%).9 Possible reasons for the disparity could be due to differences in sample sizes with diverse coverage of ART services as the chances of incorporating poorly performing health facilities may vary between locations. Study in which the larger the sample size, the greater the chance of incorporating underperforming facilities and vice versa. Reliable logistic data reporting is critical for an integrated pharmaceutical logistics system to function well. The present study, however, showed that data quality of RRF reports measured in terms of accuracy 17 (77.3%), timeliness 14 (63.64%), and completeness 7(32%) was low with a low reporting rate of 81.8%, which indicate the poor practice. Poor data quality of RRF reports is implicit of quantification errors and uninformed delivery of pharmaceuticals to health facilities that brings to over or under stocks. In similar studies, RRF reports were found to be accurate 89 (64.6%),28 1089 (61.9%),27 23 (76.7%),29 complete 135 (97.8%),28 49 (89%)27 and on time 16 (69.4%),28 51 (92.7%),27 17 (56.7%)29 with reporting rates of 97%,28 70.84%9 and 91.7%.27 These differences might be due to differences in practice between rural–urban mixed settings and the capital city of the state with different levels of ART service. Without adequate inventory management practices, healthcare facilities run the risk of not being able to provide patients with the most appropriate medications when they need them most so that emergency order is a last resort and stock out of ARV drugs is intolerable. In the current study, however, 16 (72.72%) health facilities had at least one stock out and 19 (86.4%) health facilities had at least one emergency order. This study found that stock out of ARVs decreased when the bin card record is updated and inventory accuracy is improved. Furthermore, only 8(36.36%) health facilities met acceptable storage conditions and 3.9% of ARV drugs were wasted. Other similar studies have also experienced stock-outs 52.12%,9 16 (80%),30 16 (53.3%),29 emergency orders 56.52%,9 wastages 43.2%9 and had acceptable storage conditions of ARV drugs 25 (83.3%),31 55%,25,32 25 (83.3%),29 6 (60%).33 The presence of rush orders, wastage of drugs, and poor storage conditions can result from irrational use, wastage of limited resources, distrust in the healthcare system, and risk client’s life. According to the present study, it requires improving efforts to achieve the goal of initiating treat for 90% of the people infected with HIV towards the 90-90-90 target.34 This study is limited to descriptive statistics that the nature of the data is not allowed to carry out further inferential statistical analysis.
Conclusion
The availability of bin card records and RRF reports was promising, while the data quality needs to be improved and all values are below the maximum target. Most health facilities had at least one stock-out of antiretroviral drugs for a mean of 80 days with a least one emergency order. Stock out of antiretroviral can be decreased when the bin card record is updated and inventory accuracy is improved but increased with an increased wastage rate. Only a third of the hospitals and two health centers met the acceptable storage conditions. It is indispensable to improve inventory management practices using user-friendly approaches. Further study is important to assess variables affecting inventory management practices including private health facilities.
Data Sharing Statement
All the necessary data were included in the manuscript.
Ethical Declarations
Ethical and research approval was obtained by the Ethics Review Board of Jimma University of the institute of health (reference number: IRB 000241/2012). All respondents received verbal informed consent approved by the Ethics Review Board of Jimma University. The participants were also convinced of the confidentiality of the information obtained during the study.
Acknowledgments
All authors would like to thank the facility directors and health facilities staff for providing relevant information. We also thank Jimma University for facilitating the study.
Disclosure
The authors declared that they have no competing interest in this work.
References
1. UNAIDS. Fact sheet-latest statistics on the status of the AIDS epidemic; 2019. Available from: https://www.unaids.org/en/resources/fact-sheet.
2. HIV/AIDS JUNPo. Global report: UNAIDS report on the global AIDS epidemic 2010. UNAIDS; 2013 Available from: https://www.unaids.org/globalreport/Global_report.htm.
3. UNAIDS. Fast-Tracking HIV Treatment: Parliamentary Action and Policy Options. The Hague/Berlin: UNAIDS; 2015.
4. UNAIDS. Communities at the Centre. Defending Rights Breaking Barriers Reaching People with HIV Services. Global AIDS Update. UNAIDS; 2019.
5. Allers C, Chandani Y. USAID/DELIVER. Guide for quantifying ARV drugs; 2006. Available from: www.pdf.usaid.gov.
6. Amenyah J. Supply chain management of antiretrovirals for oral pre-exposure prophylaxis - a program guide. In: Strengthening High Impact Interventions for an AIDS-Free Generation (Aidsfree) Project. Arlington, VA: USAID; 2020.
7. Erik JS, Andreas J, Anne BS, et al. Antiretroviral drug supply challenges in the era of scaling up ART in Malawi. J Int AIDS Soc. 2011;14(suppl 1):S4.
8. World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Appia, 1211 Geneva 27, Switzerland; 2016. Available from: https://www.who.int/publications/i/item/9789241549684?__cf_chl_captcha_tk__.
9. Johnson A, Peter K, Shital M. Inventory management practices and supply chain performance of antiretroviral medicines in public hospitals in Nyamira County, Kenya. Rwanda J MedHealth Sci. 2021;4(2):257–268. doi:10.4314/rjmhs.v4i2.5
10. Faruna T, Folinas D. Evaluating a humanitarian supply chain network: empirical findings from the HIV/AIDS program in Nigeria. MIBES Transactions. 2018;12(1):65–78.
11. Mori AT, Owenya J. Stock-outs of antiretroviral drugs and coping strategies used to prevent changes in treatment regimens in Kinondoni District, Tanzania: a cross-sectional study. J Pharma Policy Pract. 2014;7(1). doi:10.1186/2052-3211-7-3
12. Pasquet A, Messou E, Gabillard D, et al. Impact of drug stock-outs on death and retention to care among HIV-infected patients on combination antiretroviral therapy in Abidjan, Côte d’Ivoire. PLoS One. 2010;5(10):e13414. doi:10.1371/journal.pone.0013414
13. Abiy S, Dowling P, Necho W, Tewfik S, Yiegezu Y. DELIVER PROJECT, Task Order 4, and Pharmaceuticals Fund and Supply Agency (PFSA). Arlington, Va.: USAID; 2015.
14. GVP+, UKAID. Assessment of needs of women living with HIV in Amhara and Somali region of Ethiopia. Advancing the sexual and reproductive health and human rights of people living with HIV. NEP+; 2011. Available from: www.nepplus.org.
15. Berhanemeskel E, Beedemariam G, Fenta T. HIV/AIDS related commodities supply chain management in public health facilities of Addis Ababa, Ethiopia: a cross-sectional survey. J Pharma Policy Pract. 2016;9(1). doi:10.1186/s40545-016-0060-z
16. Clinicalinfo.hiv.gov. Initiation of antiretroviral therapy. NIH; 2021. Available from: https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv/initiation-antiretroviral-therapy.
17. Leung N, Chen A, Yadav P, Gallien J. The impact of inventory management on stock-outs of essential drugs in Sub-Saharan Africa: secondary analysis of a field experiment in Zambia. Ploa One. 2016;11(5):e0156026. doi:10.1371/journal.pone.0156026
18. Addis Ababa, Ethiopia metro area population 1950–2020. Available from: https://www.macrotrends.net/cities/20921/addis-ababa/population.
19. Ethiopia country operational plan (COP/ROP) strategic direction summary; 2019. Available from: https://www.state.gov/wp-content/uploads/2019/09/Ethiopia_COP19-Strategic-Directional-Summary_public.pdf.
20. USAID. DELIVER PROJECT, Task Order 1. Logistics Indicators Assessment Tool (LIAT). USAID; 2008.
21. PFSA. Standard operating procedures (SOP) manual for the integrated pharmaceuticals logistics system in health facilities of Ethiopia. Addis Ababa, Ethiopia. Addis Ababa, Ethiopia; 2015. Available from: www.pfsa.gov.et/webadmin/./IPLS.
22. World Health Organization. Harmonized Monitoring and Evaluation Indicators for Procurement and Supply Management Systems: Early-Warning Indicators to Prevent Stock-Outs and Overstocking of Antiretroviral, Antituberculosis and Antimalaria Medicines. 20 Avenue Appia, 1211 Geneva 27, Switzerland: World Health Organization; 2011:9–33.
23. USAID. Monitoring and Evaluation Indicators for Assessing Logistics Systems Performance. Arlington, Va.: DELIVER, for the U.S. Agency for International Development; 2006:29–36.
24. Federal Ministry of Health. National Pharmacy Service, Pharmaceuticals Supply Chain and Medical Equipment Monitoring and Evaluation Frame Work. Addis Ababa: Federal Ministry of Health; 2019.
25. Shewarega A, Dowling P, Necho W, et al. Ethiopia: National Survey of the Integrated Pharmaceutical Logistics System. Arlington, VA.: USAID | DELIVER PROJECT, Task Order 4, and Pharmaceuticals Fund and Supply Agency (PFSA); 2015.
26. John Snow, Inc. The Supply Chain Manager’s Handbook, a Practical Guide to the Management of Health Commodities. Arlington, VA 22209 USA: John Snow, Inc; 2019.
27. Bekele A, Anbessa G. Logistics management information system performance of program medicines in public health facilities of East Gojjam Zone, Northwest Ethiopia: a cross-sectional study. J Multidiscip Healthc. 2021;14:81–89. doi:10.2147/JMDH.S286981
28. Tiye K, Gudeta T. Logistics management information system performance for program drugs in public health facilities of East Wollega Zone, Oromia regional state, Ethiopia. BMC Med Inform Decis Mak. 2018;18(1). doi:10.1186/s12911-018-0720-9
29. Damtie T, Ibrahim A, Yikna B. Supply chain management performance of HIV/ AIDS commodities and factors affecting it at health facilities of SNNPRS of Ethiopia; from the perspective of achieving 90-90-90 Strategies. Integr Pharm Res Pract. 2020;9(11):11–21. doi:10.2147/IPRP.S228162
30. Mori A, Owenya J. Stock-outs of antiretroviral drugs and coping strategies used to prevent changes in treatment regimens in Kinondoni District, Tanzania: a cross-sectional study. J Pharma Policy Pract. 2014;7(1):1–6.
31. Damtie TA, Ibrahim AJ, Yikna BB. Supply chain management performance of HIV/AIDS commodities and factors affecting it at health facilities of SNNPRS of Ethiopia; from the perspective of achieving 90-90-90 strategies. Integr Pharm Res Pract. 2020;9:11.
32. Damtie TA, Ibrahim AJ, Yikna BB. Supply Chain Management Performance of HIV/AIDS Commodities in Public Health Facilities; the Case of Benishangul-Gumuz Region, Ethiopia. Addis Ababa, Ethiopia: Dove Press; 2018.
33. Boche B, Mulugeta T, Gudeta T. Assessment of inventory management practices at the Ethiopian Pharmaceuticals Supply Agency, Addis Ababa, Ethiopia. Integr Pharm Res Pract. 2020;Volume 9(9):175–183. doi:10.2147/IPRP.S269421
34. MoH. National Guidelines for Comprehensive HIV Prevention, Care and Treatment. Addis Ababa: MoH; 2018.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
