Back to Journals » Journal of Pain Research » Volume 15
Establishment and Validation of a Predictive Nomogram for Hallux Valgus with Pain Under the Second Metatarsal
Authors Bai Z, Cao X, Yang Y, Sun X, Dong Y, Wen J, Sun W
Received 19 August 2022
Accepted for publication 25 October 2022
Published 7 November 2022 Volume 2022:15 Pages 3523—3536
DOI https://doi.org/10.2147/JPR.S386315
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Alaa Abd-Elsayed
Zixing Bai1 *, Xuhan Cao1 *, Yanjun Yang,1 Xudong Sun,1 Yongli Dong,2 Jianmin Wen,1 Weidong Sun1
1Second Department of Orthopedics, Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing, People’s Republic of China; 2Scientific Research Department, Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Weidong Sun, Wangjing Hospital of China Academy of Chinese Medical Sciences, No. 6 Central South Road, Wangjing, Chaoyang District, Beijing, 100102, People’s Republic of China, Tel +86-84739140, Email [email protected]
Objective: To investigate the risk factors for hallux valgus complicated with pain under the second metatarsal and construct an effective model and method for predicting hallux valgus complicated with pain under the second metatarsal based on risk factors.
Methods: A total of 545 patients with hallux valgus who were admitted to our hospital were divided randomly into a training set and a validation set. The demographic characteristics, imaging indices and gait test indices of the patients were collected. The risk factors were identified by univariate and multivariate logistic regression analyses. A risk prediction model for hallux valgus with pain under the second metatarsal was established, and the area under the curve (AUC) of the receiver operating characteristic and a decision curve analysis were used for verification and identification. The value of the model was tested in the verification group.
Results: Second metatarsal length, second metatarsal peak pressure, hallux valgus angle (HVA), intermetatarsal angle 1– 2 (IMA1– 2) and weight were the risk factors for hallux valgus complicated with pain under the second metatarsal. Based on the weighting of these seven risk factors, a prediction model was established. The AUC of the prediction model was 0.84 (95% confidence interval [CI]: 0.802~0.898, P < 0.05), and the results of a Hosmer–Lemeshow test showed a good degree of calibration (χ2 = 10.62, P > 0.05). The internal validation of the AUC was 0.83 (95% CI: 0.737– 0.885, P < 0.05). The model had obvious net benefits when the threshold probability was 10%– 70%.
Conclusion: Second metatarsal length, second metatarsal peak pressure, HVA, IMA1– 2 and weight were the risk factors for hallux valgus combined with second metatarsal pain. The risk prediction model for hallux valgus complicated with pain under the second metatarsal based on these seven variables was proven effective.
Level of Evidence: Level III, retrospective comparative study.
Keywords: hallux valgus, metatarsalgia, nomogram, predictive model, risk factors
Introduction
Hallux valgus is a forefoot deformity characterised by a valgus deviation of the hallux and widening of the first/second intermetatarsal angle (IMA).1 With the opening of society, increasing numbers of women are wearing high heels, and the incidence of hallux valgus is rising. According to statistics from the Foot and Ankle Surgery Group of the Chinese Medical Association, the incidence of hallux valgus in the female population in China is about 20%.2 Often, patients with hallux valgus also have metatarsalgia.3,4 The preliminary investigation of this research group found that 61.7% (148/240) of patients with hallux valgus were complicated with metatarsal pain, the most common of which was pain in the second-lower metatarsal.5 Patients with hallux valgus often complain of pain under the metatarsal head and seek medical treatment.6 Biomechanical studies have shown that the occurrence of hallux valgus complicated with pain under the second metatarsal is closely related to the change in plantar pressure in hallux valgus, and the two are positively correlated.7,8
The main pathogenesis of hallux valgus combined with pain of the second-lower metatarsal is hallux valgus and pronation. Due to hallux valgus, the extensor and flexor tendons of the hallux play the role of bowstrings in the walking and propulsion movements of the hallux. This aggravates hallux valgus and pushes the first metatarsal head into varus, which increases the angle between the first and second metatarsal bones and moves the metatarsal head inwards.9 The change in the metatarsophalangeal angle inevitably disorders the balance system of the attached muscles (extensor hallucis longus, flexor hallucis longus, adductor hallucis and abductor hallucis), resulting in the collapse of the hallux valgus arch, the outward pressure of the forefoot upon loading and the formation of pain and callosities under the second metatarsal head.10 In addition, lateral medial cuneiform tilt is an important factor in aggravating the varus angle. Erduran et al11 demonstrated that increasing the medial cuneiform lateral tilt increases the articulation obliquity of the first metatarsocuneiform joint.
Hallux valgus is often associated with pain in the second-lower metatarsal, and metatarsalgia is often secondary to metatarsalgia after hallux valgus surgery. In cases where conservative treatment fails, surgery is the final solution. Research by Biz et al12 showed that minimally invasive surgery with Reverdin-Isham and Akin percutaneous osteotomy combined with previous exostosectomy and subsequent lateral soft-tissue release is a safe, effective and reliable procedure for the correction of mild to moderate hallux valgus. The use of a minimally invasive intramedullary nail device for the correction of moderate and severe hallux valgus has also been proven to be a feasible method.13 The ideal treatment aim is to improve and eliminate the associated metatarsalgia while dealing with hallux valgus, which helps reduce the burden on patients and avoids the need for a secondary operation.
One of the most important diagnostic and evaluation basis of hallux valgus is X-ray measurement. The change in the X-ray angle of the foot arch can indirectly reflect the degree of change in the function of plantar soft tissue, and plantar pressure measurement can evaluate the change in plantar pressure. Some studies have found that hallux valgus with second submetatarsal pain is related to socio-demographic factors (age, gender, body mass index [BMI], etc.), imaging factors, hallux valgus angle (HVA), intermetatarsal angle 1–2 (IMA1–2), medial longitudinal arch angle, relative length of the second metatarsal head and gait factors, such as subpeak pressure, impulse and ground contact area of the first and second metatarsal heads.14,15
Although previous studies have obtained relevant quantitative data, the relationship between hallux valgus and the risk of pain under the second metatarsal head has not been determined. Therefore, this study explored the risk factors affecting the occurrence of hallux valgus complicated with pain under the second metatarsal using univariate and multivariate logistic regression analyses. Our study aimed to clarify the risk factors for the occurrence of hallux valgus complicated with pain under the second metatarsal, construct an effective model for predicting hallux valgus complicated with pain under the second metatarsal and provide a valuable reference for the diagnosis and assessment of hallux valgus complicated with pain under the second metatarsal in clinical practice.
Materials and Methods
Study Design and Patient Selection
The clinical data of patients with hallux valgus who underwent surgery in our hospital from June 2019 to June 2021 were analysed retrospectively. All patients had hallux valgus deformities, and some patients were complicated with pain under the second metatarsal head or with callus. Our study was approved by the ethical review committee (approval number: WJEC-KT-2019-013-P003).
The clinical sample data were divided randomly into a training dataset (70%) and a validation dataset (30%). The training dataset was used to build the prediction model and nomogram diagram, while the verification dataset was used to evaluate the model’s prediction performance, degree of generalisation and extrapolation. The patients were divided into two groups: a second metatarsal head pain group (ie, the pain group) and a second metatarsal head pain-free group (ie the painless group).
Diagnostic Criteria
The diagnosis of hallux valgus was made via clinical evaluation and standing radiographs. The clinical evaluation criteria were as follows: (1) The second toe was a hammer toe, the second and third metatarsal heads formed a callus, and the protruding part of the first metatarsophalangeal joint formed a bunion. (2) The patient had local pain in their feet and found it difficult to walk. The X-ray diagnosis criteria were as follows: (1) X-ray shows HVA > 15° and/or IMA 1-2 > 9°. (2) The metatarsophalangeal joint of the thumb was slightly dislocated. (3) Osteophytes may have formed near the medial joint of the first metatarsophalangeal joint, which may produce osteoarthritis in severe cases. (4) The metatarsal heads were open, and the metatarsal bones of the first metatarsal head were displaced outward.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) Hallux valgus deformity with obvious pain after walking. Conservative treatment was ineffective and seriously affected the patient’s quality of life. (2) The diagnostic criteria for hallux valgus were met. (3) Age ≥ 18 years. (4) Complete case data that met the needs of the study.
The exclusion criteria were as follows: (1) Missing case data and no regular review. (2) Diabetic foot, severe rheumatoid foot and gouty arthritis. (3) Severe osteoarthritis of the first metatarsophalangeal joint requiring joint fusion or replacement. (4) Relaxation and instability of the metatarsophalangeal wedge joint and abnormal range of motion of the metatarsophalangeal and interphalangeal joints. (5) Active infection focused on the foot and a previous history of foot and ankle surgery. The screening process is shown in Figure 1.
 |
Figure 1 Participant flow chart. This figure shows participant flow chart including final enrollment patients for the investigation. |
Study Variables Predictors
The research group’s previous study found that hallux valgus combined with pain under the second metatarsal head was related to sociodemographic factors, imaging factors and gait mechanics factors. The sociodemographic factors included age, gender, height, weight and BMI. The physical indicators were the dorsal extension angle of the hallux and the plantar flexion angle of the hallux. The observation indices included HVA, IMA1–2, the position of the tibial sesamoid, the apex angle of the medial longitudinal arch, the first metatarsal relative to the second metatarsal and the length of the second metatarsal. The gait analysis indicators included the lower peak pressure of the first and second metatarsal heads, the impulse and the contact area.
Foot X-Ray Indicators
Using standing anteroposterior radiographs of the foot, we measured the HVA, IMA1–2, the position of the tibial sesamoid, the apex angle of the medial longitudinal arch, the first metatarsal relative to the second metatarsal and the length of the second metatarsal. Then, the tibial sesamoid position was measured according to Hardy’s protocol.16 The forefoot length was assessed in the first metatarsal relative to the second metatarsal, and the patients were divided into three groups according to this length: In the minus index, the first metatarsal was shorter than the second, and the following metatarsals became progressively shorter. In the plus index, the first metatarsal was longer than the second. In the plus–minus index, the first and second metatarsals were approximately the same length.
Gait Analysis Indicators
The gait analysis indicators included the pressure, impulse and touchdown area of the first and second metatarsal heads. Using a force plate measurement system (RSScan, Belgium), the patients walked barefoot along a 3-m-long test aisle at normal walking speed three times, and the average value of the three measured results was obtained.
Physical Indicators
The following method was used to measure the range of motion of the metatarsophalangeal joint of the big toe (active): The ankle joint was in a neutral position, the distal end of the first metatarsal was fixed, the toes were suspended, the metatarsophalangeal joint was actively flexed and extended, and the angles of plantar flexion and dorsiflexion were recorded, respectively.
Study Outcomes
The observation of pain under the second metatarsal head was based on the patient’s subjective pain when walking normally, and the observation was recorded in the patient’s medical record as ‘yes’ or “no”.
Sample Size
At present, there is no recognised calculation method for the sample size in logistic regression. Currently, the most widely used method is events per variable (EPV), that is, the number of events corresponding to each independent variable in which the number of events represents the one with the fewest dependent variables. Statistical simulation research has shown that the recommended empirical criterion in logistic regression is an EPV of at least 10, that is, the number of events is 10 times that of the included independent variables, to ensure the robustness of the results. Our number of samples and events exceeded the number of events found when using the EPV method to determine the sample size. Therefore, it was expected to provide robust estimates.
Statistical Analysis
A statistical analysis was performed using STATA 15.0 software for Windows (StataCorp, Texas, USA). A bivariate analysis was performed using the Mann–Whitney U-test for continuous variables and Fisher’s exact test or the Chi-squared test for categorical variables. The binary logistic regression model was used to develop a predictive model. A nomogram was constructed using the Stata nomolog package, and calibration plots were constructed to assess the accuracy of the nomogram. The discrimination of the model was evaluated using the receiver operating characteristic (ROC) curve. A decision curve analysis (DCA) was conducted to determine the clinical practicability of the nomogram’s quantification at different threshold probabilities in the validation dataset. All statistical P tests were two sided, and a value of P < 0.05 was considered significant. The goodness of fit of the model was tested by a Hosmer–Lemeshow test, and P > 0.05 indicated a good degree of calibration, which was verified by internal data.
Results
Clinical Characteristics of Patients
The researchers screened inpatients with hallux valgus from June 2019 to June 2021 in the Department of Bone and Joint 2 at Wangjing Hospital, Chinese Academy of Chinese Medical Sciences. According to the inclusion and exclusion criteria, 545 patients were enrolled. Among them were 388 patients with hallux valgus alone and 157 patients with hallux valgus combined with pain under the second metatarsal head. The clinical sample data were divided randomly into a training dataset (380 cases, 70%) and a validation dataset (165 cases, 30%). The baseline data of each group were analysed statistically, and the specific results are shown in Table 1.
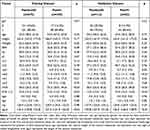 |
Table 1 Characteristics of Patients in the Training and Validation Dataset |
The training dataset revealed significant differences in weight, mp1, mp2, HVA, IMA1–2 and zgcd between the painless group and the pain group (P < 0.05). The validation dataset revealed significant differences in mp1, mp2, HVA, IMA1–2 and zgcd between the painless group and the pain group (P < 0.05).
Results of Logistic Regression Analysis
The univariate logistic analysis showed that age, mp2, cm1, HVA, IMA1–2 and the length of the second metatarsal were related to the risk factors for patients with hallux valgus with pain under the second metatarsal head (P < 0.05). The multivariate logistic regression analysis showed that the length of the second metatarsal (OR = 1.078, 95% CI [1.051, 1.105]), the peak pressure of the second metatarsal head (OR = 1.607, 95% CI [1.342, 1.925]), HVA (OR = 1.068, 95% CI [1.028, 1.109]), IMA1–2 (OR = 1.222, 95% CI [1.044, 1.43]) and weight (OR = 1.044, 95% CI [0.983, 1.108]) were the risk factors for patients with hallux valgus with pain under the second metatarsal head. The protective factors were the area under the first metatarsal head (OR = 0.806, 95% CI [0.726, 0.895]) and BMI (OR = 0.925, 95% CI [0.832, 1.029]) (see Table 2).
 |
Table 2 Logistic Regression Analysis Results of Hallux Valgus Combined with Pain Under the Second Metatarsal Head |
Development of Nomogram and Establishment of Prediction Model
Nomograms are a method of quantifying and visualising the results of a logistic regression analysis. According to the results of the multivariate logistic regression analysis in Table 2 (P < 0.2), nomograms were developed to predict the risk of hallux valgus combined with pain under the second metatarsal head, as shown in Figure 2.
In the ROC curve analysis, the area under the curve (AUC) of the prediction model constructed in this study (0.84, 95% CI: 0.802~0.898, P < 0.05) demonstrated very good discrimination, and the Hosmer–Lemeshow test results exhibited a good degree of calibration (χ2 = 10.62, P > 0.05), as shown in Figures 3 and 4.
 |
Figure 3 Receiver operating characteristic (ROC) curve developed for the prediction model of the risk of hallux valgus combined with pain under the second metatarsal head. |
 |
Figure 4 Calibration plot for the Hosmer–Lemeshow goodness of fit test for the risk prediction model. |
Internal Validation
The internal validation of the AUC (0.83, 95% CI: 0.737~0.885, P < 0.05) and the Hosmer–Lemeshow test (χ2 = 11.57, P > 0.05) indicated that the model had good prediction ability for hallux valgus complicated with pain under the second metatarsal head (Figures 3 and 4).
The clinical effectiveness of the prediction model was evaluated using a DCA. We performed a DCA on our prediction model to assess the net benefits for patients. As shown in the decision curve, the nomogram model had obvious net benefits for almost all threshold probabilities, especially when the threshold probability was 10%–70%. However, when the threshold probability was less than 10%, the net benefit of the nomogram was equivalent to predicting positive results in all patients (Figure 5).
 |
Figure 5 The decision curve analysis (DCA) analysis of predictive models. |
Discussion
Pathological Mechanism of Hallux Valgus Complicated with Pain Under the Second Metatarsal Head
The normal foot arch is divided into the medial and lateral longitudinal arch and the transverse arch. It has been reported that the five metatarsal heads of the forefoot, the two sesamoid bones and the transverse metatarsal ligament under the first metatarsal head form the top of the second and third metatarsal heads. The transverse arch of the forefoot with the base of the five metatarsal heads plays a role in absorbing shock and relieving pressure on the sole of the foot during gait.17 As the only medial supporting structures of the first metatarsophalangeal joint are the medial sesamoid and medial collateral ligaments, their failure is the early and essential lesion.18 Then, the metatarsal head can drift medially, slipping off the sesamoid apparatus. An oblique or unstable tarsometatarsal joint may encourage this movement.19 The proximal phalanx moves into a valgus position as it is tethered at its base to the sesamoids, the deep transverse ligament and the adductor hallucis tendon.20 The metatarsal head sits on the medial sesamoid and can erode the cartilage and crista. The lateral sesamoid can appear to sit in the intermetatarsal space, although it does not move. The extensor and flexor hallucis longus tendons appear to bowstring laterally, increasing the valgus displacement and occasionally acting as dorsiflexors of the proximal phalanx.21 As the metatarsal head drops off the sesamoid apparatus, it pronates because of the muscle forces acting across it.22 Normally, the abductor hallucis strongly resists the valgus of the proximal phalanx, but it becomes dysfunctional as its medial and plantar attachment rotates inferiorly. The adductor hallucis is attached to the plantar surface laterally, so it tends to pull the phalanx into pronation as well as tether its base.21 The weaker dorsal metatarsophalangeal joint capsule is not reinforced by any tendons and rotates medially with pronation, providing poor stability.21
The first ray plays a key role in maintaining the structure of the medial arch, and as the main load-bearing structure, it is subject to substantial forces during gait.23 Failure anywhere along the first ray, from the distal phalanx to the talonavicular joint, can result in hallux valgus. First-ray hypermobility (FRH) was considered a pathological entity in previous studies and was seen as a primary cause of hallux valgus.24 However, the relationship between FRH and hallux valgus remains controversial.
The collapse of the arch of the foot causes the stress on the forefoot of the hallux valgus foot to shift laterally, resulting in a painful callus under the second and third metatarsal heads.8 Forefoot alterations cause imbalances in weight-bearing distribution that may lead to mechanical overload on the affected metatarsal heads and may evolve into pain and plantar callosities.25 Initial metatarsalgia treatment is conservative; however, when these conservative measures fail and the metatarsalgia becomes recalcitrant, it requires surgical treatment with or without procedures on the first ray.26 The primary goal of surgery is to relieve pain and restore an ideal forefoot morphology with normal forefoot pressure distribution. In our study, the multivariate logistic regression results revealed that the HVA (OR = 1.068, 95% CI [1.028, 1.109]) and IMA1–2 (OR = 1.222, 95% CI [1.044, 1.43]) indirectly shows the pathological changes of the hallux valgus foot arch, which is consistent with the reports of previous studies,27 that is, with the increase in the HVA and IMA1–2, abnormal dynamic factors, such as muscle ligaments, will lead to hallux valgus foot complicated with pain under the second metatarsal head. Therefore, it is proven that HVA and IMA1–2 are risk factors for hallux valgus combined with pain under the second metatarsal head.
Analysis of Risk Factors Related to Hallux Valgus Combined with Pain Under the Second Metatarsal Head
The difference in metatarsal length is considered to be one of the important risk factors for hallux valgus complicated with pain under the second metatarsal head.28 In the gait advancement stage, the relatively long small metatarsal bone easily causes mechanical overload under the metatarsal head. The continuous compression of the metatarsal head will lead to the inflammation of plantar soft tissue, reactive keratosis of plantar skin and pain in the plantar corpus callus.9 It has been reported29,30 that the mean metatarsal length of a foot with metatarsalgia is greater than the mean metatarsal length of a normal foot, indicating that the increase in the length of the metatarsal or the shortening of the adjacent metatarsal is one of the reasons for the formation of painful submetatarsal corpus callosities. The multivariate logistic regression results of this study showed that the length of the second metatarsal bone (OR = 1.078, 95% CI [1.051, 1.105]), which was consistent with the conclusions of previous studies.
The pressure ratio of the first to the fifth metatarsal heads of a normal forefoot was 1:0.76:0.44:0.29:0.21, while the pressure ratio of the first to the fifth metatarsal heads of patients with hallux valgus combined with pain under the second metatarsal head was 1:1.20:0.74:0.40:0.29.31 Hu et al15 showed that the pressure under the second metatarsal head in a group with hallux valgus combined with pain under the second metatarsal head was the highest and was significantly greater than the pressure in a normal group and a group with hallux valgus without plantar pain. Whether static or dynamic, the pressure under the first metatarsal head of a hallux valgus foot is significantly lower than that of a normal foot, and the pressure under the second metatarsal head is significantly higher than that of a normal foot.3
The above research shows that the occurrence of hallux valgus changes the pressure balance of the forefoot, resulting in an increase in pressure under the responsible metatarsal head, which manifests as pain under the metatarsal head upon loading. The multivariate logistic regression analysis showed that the peak pressure under the second metatarsal head (OR = 1.607, 95% CI [1.342, 1.925]) was one of the important risk factors for hallux valgus complicated with pain under the second metatarsal head. In the gait cycle, the stress of a normal forefoot is concentrated in the first and fifth metatarsals, and the contact area is inversely proportional to the pressure under the metatarsal head. In the gait cycle, the front foot touchdown area is the largest in the pedal-off phase, with a specific total area. The smaller the touchdown area of the first metatarsal bone, the greater the pressure under the metatarsal head.32,33 The multivariate logistic regression analysis revealed that the touchdown area under the first metatarsal head (OR = 0.806, 95% CI [0.726, 0.895]) was the protective factor for hallux valgus complicated with pain under the second metatarsal head.
Obesity is a major public health problem. It is defined as weight gain due to the excessive accumulation of body fat and is usually assessed by BMI. Obesity changes the function and structure of the foot through different mechanisms, including changes in plantar biomechanics, decreases in muscle strength and changes in the gait cycle. Increases in body weight are positively correlated with an increase in peak plantar pressure and foot contact area.34 Arnold et al35 believed that there was a significant relationship between weight gain and the increase of the peak pressure of the heel and metatarsal head of the second to fifth metatarsal bones. Our multivariate logistic regression analysis showed that BMI (OR = 0.925, 95% CI (0.832, 1.029]) was a protective factor for hallux valgus complicated with pain under the second metatarsal head, while body weight (OR = 1.044, 95% CI [0.983, 1.108]) was a risk factor. These results are consistent with those of previous studies.
Application of Prediction Model of Hallux Valgus Combined with Second Metatarsal Head Pain
When a medical model develops from empirical medicine to evidence-based medicine and then to precision medicine, the value of the data receives unprecedented attention. The rapid development of data acquisition, storage, analysis and prediction technology in the era of big data increases the prospect of personalised medicine.36,37 Clinical prediction models use mathematical formulae to estimate the probability of a specific individual currently suffering from a disease or a certain outcome in the future. As a quantitative tool for risk and benefit assessment, it can provide intuitive and rational information for decision making by doctors, patients and healthcare personnel.38 In the prevention and treatment of hallux valgus foot combined with pain under the second metatarsal head, the forefoot metatarsal pad can be used to alleviate the change in the arch of the hallux valgus foot through changes in imaging and plantar pressure in the early stage to indirectly reduce the load of the second metatarsal head and delay the aggravation of the HVA through the use of a hallux valgus correction belt or a split toe pad. Of course, it is very important to avoid soft tissue factors, such as the strain on internal and external muscles and ligaments, through internal and external muscle training.
Limitations
This study was a retrospective study and had some limitations. The clinical data came from the orthopaedic department of our hospital, so it lacked comparisons with data from different centres. Although the sample size was large, the verification of the model was internal; therefore, it needs further external verification to confirm the model’s practicability. Additionally, as a retrospective study, there may have been a certain degree of selection bias. Based on the risk factors and prediction model for hallux valgus combined with pain under the second metatarsal head identified in this study, it is necessary to expand the sample size and deal with covariates. Furthermore, a future multicentre study is required to verify the validity of the prediction model for hallux valgus combined with pain under the second metatarsal head to expand the predictive model for clinical application.
Conclusion
The length of the second metatarsal bone, the peak pressure under the second metatarsal head, the HVA, IMA1–2 and weight are risk factors for hallux valgus combined with pain under the second metatarsal head, while BMI and the touchdown area under the first metatarsal head are protective factors. The risk prediction model based on these seven variables is expected to be used for preoperative risk prediction and intervention in high-risk groups. With the emergence of the prediction model for hallux valgus combined with pain under the second metatarsal head, the accuracy of interventions will be enhanced, and the clinical effect will be more significant in the future.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Wangjing Hospital of China Academy of Chinese Medical Sciences (WJEC-KT-2019-013-P003), and all subjects signed the informed consent.
Funding
This research was supported by the Beijing Municipal Science and Technology Project (Z191100006619024) and the Beijing Municipal Natural Science Foundation of China (7172244).
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately.
References
1. Arbab D, Schneider LM, Schnurr C, et al. Treatment of hallux valgus: current diagnostic testing and surgical treatment performed by German foot and ankle surgeons. Z Orthop Unfall. 2018;156(2):193–199. doi:10.1055/s-0043-120352
2. Wang ZY, Jiang BG, Tang KL. Expert consensus on the surgical treatment of hallux valgus. Chin J Bone Joint Surg. 2018;11(2):87–95. doi:10.3969/j.issn.2095-9958.2018.02.002
3. VVerdu Roman C, Martinez Gimenez E, Bustamante Suarez de Puga D, et al. Hallux valgus with and without metatarsalgia in women: a matched-cohort study of plantar pressure measurements. Indian J Orthop. 2021;55(Suppl 2):436–444. doi:10.1007/s43465-021-00416-3
4. Cooke R, Manning C, Palihawadana D, et al. Metatarsalgia: anatomy, pathology and management. Br J Hosp Med. 2021;82(9):1–8. doi:10.12968/hmed.2021.0348.
5. Gong H, Sang ZC, Wen JM, et al. Correlative analysis on metatarsalgia and the X-ray measurement indexes under weight-bearing and non-weight-bearing of hallux valgus. Zhongguo Gu Shang. 2014;27(4):303–307.
6. Hofmann UK, Götze M, Wiesenreiter K, et al. Transfer of plantar pressure from the medial to the central forefoot in patients with hallux valgus. BMC Musculoskelet Disord. 2019;20(1):149. doi:10.1186/s12891-019-2531-2
7. Hida T, Okuda R, Yasuda T, et al. Comparison of plantar pressure distribution in patients with hallux valgus and healthy matched controls. J Orthop Sci. 2017;22(6):1054–1059. doi:10.1016/j.jos.2017.08.008
8. Zeidan H, Ryo E, Suzuki Y, et al. Detailed analysis of the transverse arch of hallux valgus feet with and without pain using weightbearing ultrasound imaging and precise force sensors. PLoS One. 2020;15(1):e0226914. doi:10.1371/journal.pone.0226914
9. Walker AK, Harris TG. The role of first ray insufficiency in the development of metatarsalgia. Foot Ankle Clin. 2019;24(4):641–648. doi:10.1016/j.fcl.2019.07.001
10. Chang C, Wang QF, Guo JC, et al. The biomechanical relationship between hallux valgus deformity and metatarsal pain. J Healthc Eng. 2020;2020:8929153. doi:10.1155/2020/8929153
11. Erduran M, Acar N, Demirkiran ND, Atalay K. The impact of medial cuneiform bone variant measures on the severity of hallux valgus: a radiological study. J Orthop Surg. 2017;25(3):2309499017727921. doi:10.1177/2309499017727921
12. Biz C, Fosser M, Dalmau-Pastor M, et al. Functional and radiographic outcomes of hallux valgus correction by mini-invasive surgery with Reverdin-Isham and Akin percutaneous osteotomies: a longitudinal prospective study with a 48-month follow-up. J Orthop Surg Res. 2016;11(1):157. doi:10.1186/s13018-016-0491-x
13. Biz C, Crimì A, Fantoni I, Tagliapietra J, Ruggieri P. Functional and radiographic outcomes of Minimally Invasive Intramedullary Nail Device (MIIND) for moderate to severe hallux valgus. Foot Ankle Int. 2021;42(4):409–424. doi:10.1177/1071100720969676
14. Zuo JG, Sang ZC, Wen JM, et al. Study on the correlative factors of the pain under the second metatarsal in patients with hallux valgus. Zhongguo Gu Shang. 2017;30(1):51–56. doi:10.3969/j.issn.1003-0034.2017.01.012
15. Hu HW, Sun WD, Jiang KW, et al. A Logistic regression analysis on hazards of transfer metatarsalgia for surgery patient after treatment integrated TCM, west medicine and minimally invasive technique. Chin Med Pharm. 2012;2(24):9–11.
16. Iliou K, Paraskevas GK, Kanavaros P, et al. Correlation of the hallux sesamoids’ orientation with various anatomical parameters in patients with hallux valgus deformity. Cureus. 2019;11(5):e4643. doi:10.7759/cureus.4643
17. Dantas G, Sacco ICN, Dos Santos AF, et al. Effects of a foot-ankle strengthening programme on clinical aspects and gait biomechanics in people with knee osteoarthritis: protocol for a randomised controlled trial. BMJ Open. 2020;10(9):e039279. doi:10.1136/bmjopen-2020-039279
18. Wong DW, Wang Y, Chen TL, et al. Finite element analysis of generalized ligament laxity on the deterioration of hallux valgus deformity (bunion). Front Bioeng Biotechnol. 2020;8:571192. doi:10.3389/fbioe.2020.571192
19. Schneider W. Distal soft tissue procedure in hallux valgus surgery: biomechanical background and technique. Int Orthop. 2013;37(9):1669–1675. doi:10.1007/s00264-013-1959-5
20. Dalmau-Pastor M, Vega J, Malagelada F, Peña F, Manzanares-Céspedes MC. An anatomical study of nerves at risk during minimally invasive hallux valgus surgery. J Vis Exp. 2018;132:56232. doi:10.3791/56232
21. Van Elst C, Van Riet A, Vandeputte G. Tendon balancing in hallux valgus surgery. Acta Orthop Belg. 2016;82(3):627–631.
22. Vanhegan IS, Alva A, Shaerf D, Baghla D. Intraoperative assessment of flexor hallucis longus tendon integrity following hallux valgus correction. Ann R Coll Surg Engl. 2016;98(7):520. doi:10.1308/rcsann.2016.0157
23. Ota T, Nagura T, Kokubo T, et al. Etiological factors in hallux valgus, a three-dimensional analysis of the first metatarsal. J Foot Ankle Res. 2017;10:43. doi:10.1186/s13047-017-0226-1
24. Biz C, Maso G, Malgarini E, Tagliapietra J, Ruggieri P. Hypermobility of the first ray: the Cinderella of the measurements conventionally assessed for correction of hallux valgus. Acta Biomed. 2020;91(4–S):47–59. doi:10.23750/abm.v91i4-S.9769
25. Biz C, Corradin M, Kuete Kanah WT, et al. Medium-long-term clinical and radiographic outcomes of minimally invasive Distal Metatarsal Metaphyseal Osteotomy (DMMO) for central primary metatarsalgia: do maestro criteria have a predictive value in the preoperative planning for this percutaneous technique? Biomed Res Int. 2018;2018:1947024. doi:10.1155/2018/1947024
26. Nakagawa S, Fukushi J, Nakagawa T, Mizu-Uchi H, Iwamoto Y. Association of metatarsalgia after hallux valgus correction with relative first metatarsal length. Foot Ankle Int. 2016;37(6):582–588. doi:10.1177/1071100716634792
27. Okuda R, Kinoshita M, Yasuda T, et al. Hallux valgus angle as a predictor of recurrence following proximal metatarsal osteotomy. J Orthop Sci. 2011;16(6):760–764. doi:10.1007/s00776-011-0136-1
28. Justiniano P, Mac-Iver PEM, López M, et al. Relative first metatarsal length variation following hallux valgus surgery and association with postoperative metatarsalgia. Foot Ankle Orthop. 2022;7(1):2473011421S0026. doi:10.1177/2473011421S00267
29. Sovilj M, Baljozović A, Baščarević Z. Influence of the length of the first and second metatarsal bone measured distal from Maestro line upon severity of hallux valgus deformity. Sci Rep. 2021;11(1):11539. doi:10.1038/s41598-021-91085-7
30. Fleischer AE, Hshieh S, Crews RT, et al. Association between second metatarsal length and forefoot loading under the second metatarsophalangeal joint. Foot Ankle Int. 2018;39(5):560–567. doi:10.1177/1071100717753829
31. Tsujinaka S, Shima H, Yasuda T, et al. Comparison of plantar pressure distribution between postoperative hallux valgus feet and healthy feet. Foot Ankle Int. 2019;40(5):578–585. doi:10.1177/1071100718821631
32. Yoshida T, Tanino Y, Nakao T, et al. Examination of gait characteristics and related factors in elderly subjects with and without hallux valgus. Prog Rehabil Med. 2021;6:20210028. doi:10.2490/prm.20210028
33. Geng X, Huang D, Wang X, et al. Loading pattern of postoperative hallux valgus feet with and without transfer metatarsalgia: a case control study. J Orthop Surg Res. 2017;12(1):120. doi:10.1186/s13018-017-0622-z
34. Taş S, Bek N, Ruhi Onur M, et al. Effects of body mass index on mechanical properties of the plantar fascia and heel pad in asymptomatic participants. Foot Ankle Int. 2017;38(7):779–784. doi:10.1177/1071100717702463
35. Arnold JB, Causby R, Pod GD, et al. The impact of increasing body mass on peak and mean plantar pressure in asymptomatic adult subjects during walking. Diabet Foot Ankle. 2010;1(1):5518. doi:10.3402/dfa.v1i0.5518
36. Manchia M, Pisanu C, Squassina A, et al. Challenges and future prospects of precision medicine in psychiatry. Pharmgenomics Pers Med. 2020;13:127–140. doi:10.2147/PGPM.S198225
37. Ibrahim A, Primakov S, Beuque M, et al. Radiomics for precision medicine: current challenges, future prospects, and the proposal of a new framework. Methods. 2021;188:20–29. doi:10.1016/j.ymeth.2020.05.022
38. Staffa SJ, Zurakowski D. Statistical development and validation of clinical prediction models. Anesthesiology. 2021;135(3):396–405. doi:10.1097/ALN.0000000000003871
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

