Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
Establishment and Clinical Application of the Nomogram Related to Risk or Prognosis of Hepatocellular Carcinoma: A Review
Authors Wang X, Zhao M, Zhang C, Chen H, Liu X, An Y, Zhang L , Guo X
Received 13 April 2023
Accepted for publication 17 August 2023
Published 22 August 2023 Volume 2023:10 Pages 1389—1398
DOI https://doi.org/10.2147/JHC.S417123
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Jörg Trojan
Xiangze Wang,1 Minghui Zhao,1 Chensheng Zhang,1 Haobo Chen,1 Xingyu Liu,2 Yang An,1 Lu Zhang,1 Xiangqian Guo1
1Department of Preventive Medicine, Institute of Biomedical Informatics, Bioinformatics Center, Henan Provincial Engineering Center for Tumor Molecular Medicine, School of Basic Medical Sciences, Academy for Advanced Interdisciplinary Studies, Henan University, Kaifeng, 475004, People’s Republic of China; 2School of Computer and Information Engineering, Henan University, Kaifeng, 475004, People’s Republic of China
Correspondence: Lu Zhang; Xiangqian Guo, Department of Preventive Medicine, Institute of Biomedical Informatics, Bioinformatics Center, Henan Provincial Engineering Center for Tumor Molecular Medicine, School of Basic Medical Sciences, Academy for Advanced Interdisciplinary Studies, Henan University, Kaifeng, 475004, People’s Republic of China, Tel/Fax +86-371-23880585, Email [email protected]; [email protected]
Abstract: Hepatocellular carcinoma (HCC) is the most prevalent primary liver malignancy, accounting for approximately 90% of all primary liver cancers, with high mortality and a poor prognosis. A large number of predictive models have been applied that integrate multiple clinical factors and biomarkers to predict the prognosis of HCC. Nomograms, as easy-to-use prognostic predictive models, are widely used to predict the probability of clinical outcomes. We searched PubMed with the keywords “hepatocellular carcinoma” and “nomogram”, and 974 relative literatures were retrieved. According to the construction methodology and the real validity of the nomograms, in this study, 97 nomograms for HCC were selected in 77 publications. These 97 nomograms were established based on more than 100,000 patients, covering seven main prognostic outcomes. The research data of 56 articles are from hospital-based HCC patients, and 13 articles provided external validation results of the nomogram. In addition to AFP, tumor size, tumor number, stage, vascular invasion, age, and other common prognostic risk factors are included in the HCC-related nomogram, more and more biomarkers, including gene mRNA expression, gene polymorphisms, and gene signature, etc. were also included in the nomograms. The establishment, assessment and validation of these nomograms are also discussed in depth. This study would help clinicians construct and select appropriate nomograms to guide precise judgment and appropriate treatments.
Keywords: hepatocellular carcinoma, nomograms, prognosis, biomarker, precision medicine
Introduction
Hepatocellular carcinoma (HCC) is the most prevalent primary liver malignancy, accounting for approximately 90% of all primary liver cancers, with high mortality and a poor prognosis.1 80% of patients with HCC are in advanced stage at the first visit. Although some patients have received radical hepatectomy, the high recurrence rate and metastasis rate after surgery remain the challenges for the survival of patients.2,3 In recent years, targeted therapies and immune checkpoint inhibitors have achieved a satisfactory curative effect in HCC. In addition, some new therapeutic options have contributed to improved prognosis in patients with HCC, such as the combination of PD-1 inhibitors with anti-angiogenic therapy and intensity-modulated radiotherapy, as well as Gamma knife radiosurgery.4,5 However, a significant percentage of individuals still have low survival rates.6 A large number of studies have been conducted to identify potential risk factors for the diagnosis and prognosis of HCC.7 Based on universally recognized risk factors, such as the stage of American Joint Committee on Cancer Tumor-Node-Metastasis (TNM) and the stage of Barcelona Clinic Liver Cancer (BCLC),8 many predictive models have been established to stratify or score the risk associated with HCC. However, these models are not easy to apply to clinical practice as they require extensive calculations or rely on certain devices such as imaging modes or biochemical tests when evaluating risk scores. Furthermore, personalized prognostic prediction based on individual risk is more cost-effective, saves net medical costs and improves patient survival compared with current methods of prognostic risk assessment for HCC that rely only on clinical characteristics. Therefore, combined with clinical characteristics, new molecular information may improve the accuracy of predicting the prognostic risk of HCC, such as plasma alkaline phosphatase (ALP), PD-L1 expression on circulating tumor cells and plasma HSP90α level.9–11
The nomogram is an easy-to-use prognostic model for cancer patients, which can help doctors determine the possibility of specific events to make more precise clinical decisions.12 The user-friendly interface of the nomogram allows an individual patient to easily perform prognostic prediction; thus, it has been widely used in various cancers in recent years.13 In this review, we have collected 97 nomograms of HCC, deeply analyzed the establishment and verification of the nomogram, and discussed the potential clinical usage of these nomograms.
Process of Literature Selection
We searched PubMed to collect publications reporting HCC associated nomograms by November 1, 2022. The keywords “hepatocellular carcinoma” and “nomogram” were used to search the literature in PubMed. The primary search retrieved 974 publications. When looking through the titles and abstracts, 72 publications were excluded because lacking original nomograms or presenting nomograms unrelated to HCC. In addition, seven non-English publications were excluded. Finally, according to the principle of establishment of nomograms, 97 nomograms from 77 literatures were included in this study (Figure 1).
 |
Figure 1 Literature screening process. |
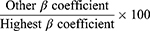
These nomograms meet the construction guidelines proposed by Iasonos A et al in 2008,8 the following inclusion criteria were applied: (i) Nomograms are established using logistic regression models or Cox proportional hazard model or other mathematical models. (ii) Hazard ratio (HR), odds ratio (OR), and regression coefficients (β) are available and accurate. (iii) A nomogram has been plotted accurately according to the weight of β coefficients of variables in the model, that is, the weight of the highest β coefficient (absolute value) is assigned 100 points on the scale, and the β coefficient of other variables are assigned a smaller number of points proportional to their effect size, following the formula
Based on the above selection criteria, 97 HCC-related nomograms in 77 articles were finally included in this review. Study characteristics including first author, PMID number, year of publication, data sources, sample size, risk factors, predictive effect, and verification method were extracted.
Characteristics of the HCC Nomogram
97 HCC-related nomograms covered more than 100,000 patients and were used for in-depth analysis. The basic characteristics of these study cohorts are summarized in Supplementary Table 1, including first author, publication date, PMID number, disease outcomes, sample size, data source, risk factors, statistical methods, etc. Most of the HCC-related nomograms were published after 2020 and were based on hospital patient data (Figure 2A and B). The nomograms of only 21 articles were built on publicly available data, including The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), Surveillance, Epidemiology, and End Results (SEER), International Cancer Genome Consortium (ICGC), and The cBio Cancer Genomics Portal (cBioPortal). In general, the nomogram based on hospital-based data collected by the researchers themselves is more representative, especially data from multiple research centers.
These nomograms focus on the prognosis of various HCC treatment methods and the risk of serious complications, including hepatectomy, immunotherapy, targeted therapy, transarterial chemoembolization, radiofrequency ablation, liver transplantation, risk of microvascular invasion, risk of deep vein thrombosis, etc. Among them, 39 studies focused on the prognosis of patients after hepatectomy, including radical hepatectomy, partial hepatectomy and laparoscopic hepatectomy.
The staging and grading system for HCC is crucial for the selection of treatment plans and prognosis evaluation of patients. AJCC TNM stage, BCLC stage and Child-Pugh grade are often used as staging criteria for HCC. Most studies have used existing HCC staging and grading systems to identify samples, with only a few studies using uncertain terms such as advanced-stage patients or patients without distant metastasis. The 97 nomograms contained seven major disease outcomes, including overall survival (OS), recurrence-free survival (RFS), disease-free survival (DFS), progression-free survival (PFS), cancer-specific survival (CSS), risk of HCC and its complications, and therapeutic response prediction (Figure 2C).
Hepatitis B virus (HBV), hepatitis C virus (HCV), exposure to aflatoxin B1, excessive consumption of alcohol, and non-alcoholic liver disease are the main risk factors for HCC.14 The geographic variability in the incidence of HCC is mainly due to the distribution of HBV and HCV infections. 80–90% of HCCs are associated with HBV or HCV of the world.15,16 Therefore, the HCC-related nomogram that provides information about the infection of patients by the hepatitis virus is more representative. In this review, 69 articles provide information on viral infection in patients with HCC. Only a few studies have provided information on alcoholism and cirrhosis in patients.
Construction Steps of the Nomogram
To establish, evaluate and validate nomograms by collecting patients’ clinical characteristics, survival information and molecular features. Therefore, the nomogram should follow certain steps before clinical application (Figure 3).
 |
Figure 3 Standard process of nomogram establishment. The dotted box indicates that this method is optional. |
Establishment
Logistic regression model builds a linear relationship between the probability of the disease outcome and risk factors. Cox proportional hazard model assesses the effect of risk factors on survival time. Logistic regression models are often used for cross-sectional studies and case-control studies, whereas Cox regression model is often used for cohort studies because Cox regression analysis allows for the presence of censored data. Thus, logistic regression model was used to establish a nomogram of the risk of HCC, while Cox regression model was used to establish a nomogram predicting the prognosis of HCC. So logistic regression model and Cox proportional hazard model are often used to select risk factors for nomograms. Odds ratio (OR) in logistic regression model and hazard ratio (HR) in Cox proportional hazard model are metrics used in epidemiological etiological studies to assess the strength of causal relationships between treatment/exposure and certain outcome. OR and HR are calculated from the regression coefficients of the variables, that is, OR or HR= exp (β). Therefore, accurate OR, HR, and β coefficients are the key to building an accurate and powerful nomogram.
In addition, because the multivariable regression model can adjust potential confounding factors, it is better to select a multivariable regression model to establish a nomogram when evaluating the relationship between risk factors and disease outcomes. Generally, multivariable logistic regression analysis is used to develop the predictive risk model, and multivariable Cox proportional hazard model is used to develop the prognostic model. Of the 97 nomograms, 84 were constructed with Cox regression models and 13 with a logistic regression model.
The least absolute shrinkage and selection operator (LASSO) method was used for data dimension reduction and covariate selection.17 Therefore, when it is necessary to screen statistically significant prognostic factors from numerous clinical variables or biomarkers, LASSO is often combined with Cox regression model or logistic regression model for the construction of nomograms.18,19
Assessment
The goal of an individualized risk prediction model is to accurately predict the disease outcome. The ability of a model to separate patients with different outcomes is called discrimination.8 The predictive accuracy (or discrimination ability) of a nomogram is usually measured by the concordance index (C-index), the area under the curve (AUC), and the decision curve analysis (DCA). In general, the logistic regression model is evaluated with AUC and the Cox regression model is evaluated with C-index and time-dependent AUC, but both models can be evaluated with DCA. It is worth noting that most studies provide multiple assessment indicators of the nomogram for mutual verification.
The C-index can measure the predictive accuracy (discrimination) of a nomogram, which quantifies the consistency between the prediction probability of the predictive model and the real probability.13 Therefore, C-index is the most extensive indicator for the overall evaluation of the prognostic model, which can characterize the prognostic ability of a model considering the occurrence and time of the results.20 The AUC of a time-dependent receiver operating characteristic curve (ROC) is another similar metric to the C-index, and researchers tend to select at least one to assess the predictive power of nomograms.21 ROC analysis is used to describe the accuracy of predictive models, and AUC can quantify the accuracy of predictive capability of the model. The C-index and AUC values are closer to 1 to indicate a more accurate prediction model.22 Most of the nomograms in this study provide exact C-index or AUC values, and most the nomograms had C-index or AUC values greater than 0.7.
The decision curve analysis calculates the clinical “net benefit” of the predictive model or diagnostic test, compared to the default strategy of treating all patients or none. Net benefit is calculated across a range of threshold probabilities, defined as the minimum probability of disease at which further intervention would be warranted, as net benefit = sensitivity × prevalence – (1 – specificity) × (1 – prevalence) × w where w is the odds at the threshold probability.23 The decision curve analysis shows the discrimination of the prediction model through the graph, rather than the exact value, so this graph is not easy to understand. But this method tries to overcome the limitations of traditional statistical indicators and can be used as a powerful supplement to the evaluation of prediction models. The nomograms of several studies provide the results of the decision curve analysis and show good discrimination of the prediction model.24–27
Validation
A nomogram needs to be evaluated to clarify the accuracy, specificity, and sensitivity of the model before translated into clinics, and this analysis process is called validation. Nomogram validation is a standard process for determining the efficacy and generalizability of prognosis models. Generally, validation includes “external” and “internal” validation. Internal validation is economical because it splits an input data set into multiple parts, some of which are used for the training set and the rest for the testing set. Common internal validation methods are k-fold cross-validation and bootstrap resampling, but cannot guarantee the quality of a nomogram because of potentially biased training data and the complexity of the validation process itself. To evaluate the nomogram comprehensively, it is best to use data sources elsewhere as validation datasets. External validation uses independently derived data sets to verify the performance of a nomogram model. Therefore, positive performance in external verification is more regarded as proof of generalizability.28 Of the 77 studies we collected, only 13 studies provided the results of external validation.
Risk Factors Included in Nomograms
Clinical Characteristics
Traditional prediction models mostly use clinicopathological and clinicoradiological factors, which are often detected in clinical diagnosis and treatment. Furthermore, some clinically relevant and important factors were also included for the construction of the nomogram, although they may not be statistically associated with the outcomes yet exhibit clinical indispensable values.12
Many important clinicopathological and clinicoradiological variables were analyzed in 97 nomograms, for example, tumor size was used in 32 nomograms, tumor number in 25 nomograms, and patient age in 15 nomograms (Figure 2D). Furthermore, platelet-to-lymphocyte ratio (PLR), γ-glutamyl transpeptidase-to-platelet ratio (GPR) and neutrophil times γ-glutamyl transpeptidase-to-lymphocyte ratio (NrLR), new clinical inflammatory indicators, were used to construct nomograms. Hepatitis virus-related variables were also included in the nomogram, including HBV DNA level, the infection by hepatitis virus, and antiviral therapy.29–31
There are many staging systems for the prognosis of HCC. There is no consensus on which staging system is the best, because these systems have different prognostic values in different populations of patient. The AJCC TNM stage system and the Barcelona-Clinic-Liver Cancer (BCLC) classification were widely used in the construction of the HCC-related nomogram. The AJCC TNM stage system determines the most important prognostic factors, the number of tumors, and the presence and extent of vascular infiltration in the tumor. However, this system cannot accurately stage patients with unresectable HCC, which limits its application in this group of patients.32 The BCLC classification defines five prognostic subclasses and assigns specific treatments for each stage, including surgical resection, liver transplantation, radiofrequency ablation, chemoembolization, and the multikinase inhibitor sorafenib. The classification provides an easy-to-use algorithm to link tumor stages with treatment allocation policies, which is endorsed by European and American clinical practice guidelines.33
With advances in computed tomography (CT) and magnetic resonance imaging (MRI), HCC can now be reliably diagnosed without biopsy.34 Therefore, nomograms based on CT or MRI features were also used in the study of prognosis of liver cancer, such as homogeneous signal, rim enhancement, peritumoral enhancement, and fusion radiomic signature.35–37
Molecular Features
In addition to clinical characteristics, the gene signature and biomarker were also selected for the development of the nomogram, although they may be difficult and costly to be measured compared to clinical variables. However, these biomarkers are related to hepatitis virus infection or HCC progression, so they are of great significance in clarifying the molecular and genetic mechanisms.
As a cheap and convenient biomarker, alpha-fetoprotein (AFP) has been widely used in the diagnosis and surveillance of HCC. Therefore, AFP was the most common risk factor in the nomogram (Figure 2D). AFP was used as a categorical variable in most nomograms, and as a continuous variable in some nomograms, even with logarithmic conversion of values. The risk factors in the nomograms can be continuous variables or categorical variables, which will affect the weight of the risk factors in the nomograms. Therefore, it must be seriously considered how to select the type of variable and cut-off value of the variable.
It should be noted that researchers are paying more attention to the clinical values of biomarkers. This study demonstrated the prognostic significance of the novel biomarkers contained in all collected nomograms, of which 11 nomograms provide the prognostic value of the novel gene signature, and 17 nomograms show the prognostic value of a single novel biomarker, including mRNA expression, protein expression, lncRNA, miRNA, ctDNA and single nucleotide polymorphism (SNP) (Figure 4). These genes are involved in cuproptosis,38 mitochondrial function,39 immune infiltration,40 pyroptosis,41 m6A methyltransferase modification,42 DNA repair,43 etc. There are well-known PD-L144 and VEGFA45 related to the prognosis of HCC, as well as MPV1739 and HSPB1146 that are less studied. Some genes are related not only to OS, but also to RFS, such as RPS3A25 and APOA4.47
Notably, the determination of diagnostic and prognostic cutoffs for biomarkers is dependent on laboratory equipment and detection techniques. Therefore, the cutoff values of biomarkers from different laboratories are not suitable for direct comparison. The cut-off range of biomarkers requires repeated validation in a large sample to be determined. However, the diagnostic and prognostic effects of these biomarkers should be consistent.
Clinical Application of Nomogram
The validity of the prognostic model is based on the correlation between the observed probability and the predictive probability of an event (calibration) and on its ability to distinguish patients with different prognoses (discrimination). An effective risk prediction model should have good discrimination and calibration. Discrimination can stratify patients into groups with different prognosis according to risk scores. There was a significant difference in recurrence and progression rates between the low-risk and high-risk groups. Calibration can accurately predict the course of an individual patient’s disease. Therefore, the choice of variables in the prognosis model is crucial.
The nomogram could transform the prognostic risk factors and complex regression equation into a simple and visual graph, making the prediction model more readable and more valuable. But the quality of the published nomograms is uneven, mainly due to the following problems. First, the nomogram should be derived from a statistical model and preferably provide explicit OR or HR values. Second, the selection of variable types in the nomogram is important, that is, continuous variables or categorical variables, which can affect the weight of variables in the model. Third, there are too few nomograms that can provide external data validation, so it is questionable whether the conclusions of these studies are reliable.
With the development of high-throughput technologies, more key prognostic biomarkers have been found. Combining clinical characteristics and biomarkers can make nomograms play a stronger predictive function. In addition, the rapid development of the Internet contributes to the visualization of nomographs and makes them more convenient to use. In this review, six studies provide available online websites.48–53 People can predict the risk scores of the specific disease by entering a limited number of variables into a website, which will greatly facilitate the application of nomograms in clinical practice.
Conclusions
This study collected published nomograms related to HCC, which provide definite computational models and validation results. This review categorizes the published nomograms and provides a detailed description of the establishment process, risk factors, application population, and advantages and disadvantages of these models. This study provides resources for clinicians and researchers to apply the established nomograms and provides more directions for developing new predictive models.
Funding
This work was supported by the supporting program for Central Plain Young Top Talents (ZYQR201912176), undergraduate teaching reform research and practice project of Henan University (HDXJJG2022-99).
Disclosure
The authors have no conflict of interests related to this publication.
References
1. Couri T, Pillai A. Goals and targets for personalized therapy for HCC. Hepatol Int. 2019;13(2):125–137.
2. Deng M, Sun S, Zhao R, et al. The pyroptosis-related gene signature predicts prognosis and indicates immune activity in hepatocellular carcinoma. Mol Med. 2022;28(1):16.
3. Anwanwan D, Singh SK, Singh S, et al. Challenges in liver cancer and possible treatment approaches. Biochim Biophys Acta Rev Cancer. 2020;1873(1):188314.
4. Su K, Guo L, Ma W, et al. PD-1 inhibitors plus anti-angiogenic therapy with or without intensity-modulated radiotherapy for advanced hepatocellular carcinoma: a propensity score matching study. Front Immunol. 2022;13:972503.
5. Su K, Gu T, Xu K, et al. Gamma knife radiosurgery versus transcatheter arterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus: a propensity score matching study. Hepatol Int. 2022;16(4):858–867.
6. Cheng AL, Hsu C, Chan SL, et al. Challenges of combination therapy with immune checkpoint inhibitors for hepatocellular carcinoma. J Hepatol. 2020;72(2):307–319.
7. Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021;18(4):223–238.
8. Iasonos A, Schrag D, Raj GV, et al. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–1370.
9. Su K, Huang W, Li X, et al. Evaluation of lactate dehydrogenase and alkaline phosphatase as predictive biomarkers in the prognosis of hepatocellular carcinoma and development of a new nomogram. J Hepatocell Carcinoma. 2023;10:69–79.
10. Su K, Guo L, He K, et al. PD-L1 expression on circulating tumor cells can be a predictive biomarker to PD-1 inhibitors combined with radiotherapy and antiangiogenic therapy in advanced hepatocellular carcinoma. Front Oncol. 2022;12:873830.
11. Su K, Liu Y, Wang P, et al. Heat-shock protein 90α is a potential prognostic and predictive biomarker in hepatocellular carcinoma: a large-scale and multicenter study. Hepatol Int. 2022;16(5):1208–1219.
12. Balachandran VP, Gonen M, Smith JJ, et al. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–180.
13. Kawai K, Sunami E, Yamaguchi H, et al. Nomograms for colorectal cancer: a systematic review. World J Gastroenterol. 2015;21(41):11877–11886.
14. Petruzziello A. Epidemiology of hepatitis B virus (HBV) and hepatitis C virus (HCV) related hepatocellular carcinoma. Open Virol J. 2018;12:26–32.
15. Xie Y. Hepatitis B virus-associated hepatocellular carcinoma. Adv Exp Med Biol. 2017;1018:11–21.
16. Khatun M, Ray R, Ray RB. Hepatitis C virus associated hepatocellular carcinoma. Adv Cancer Res. 2021;149:103–142.
17. Tang B, Zhu J, Li J, et al. The ferroptosis and iron-metabolism signature robustly predicts clinical diagnosis, prognosis and immune microenvironment for hepatocellular carcinoma. Cell Commun Signal. 2020;18(1):174.
18. Li W, Han J, Yuan K, et al. Integrated tumor stromal features of hepatocellular carcinoma reveals two distinct subtypes with prognostic/predictive significance. Aging. 2019;11(13):4478–4509.
19. Liu GM, Zeng HD, Zhang CY, et al. Identification of a six-gene signature predicting overall survival for hepatocellular carcinoma. Cancer Cell Int. 2019;19:138.
20. Longato E, Vettoretti M, Di Camillo B. A practical perspective on the concordance index for the evaluation and selection of prognostic time-to-event models. J Biomed Inform. 2020;108:103496.
21. Razdan S, Sljivich M, Pfail J, et al. Predicting morbidity and mortality after radical cystectomy using risk calculators: a comprehensive review of the literature. Urol Oncol. 2021;39(2):109–120.
22. Obuchowski NA, Bullen JA. Receiver operating characteristic (ROC) curves: review of methods with applications in diagnostic medicine. Phys Med Biol. 2018;63(7):07TR01.
23. Vickers AJ, van Calster B, Steyerberg EW. A simple, step-by-step guide to interpreting decision curve analysis. Diagn Progn Res. 2019;3:18.
24. Zeng J, Zeng J, Wu Q, et al. Novel inflammation-based prognostic nomograms for individualized prediction in hepatocellular carcinoma after radical resection. Ann Transl Med. 2020;8(17):1061.
25. Zhou C, Weng J, Liu C, et al. High RPS3A expression correlates with low tumor immune cell infiltration and unfavorable prognosis in hepatocellular carcinoma patients. Am J Cancer Res. 2020;10(9):2768–2784.
26. Zhou T, Cai Z, Ma N, et al. A novel ten-gene signature predicting prognosis in hepatocellular carcinoma. Front Cell Dev Biol. 2020;8:629.
27. Li X, Huang H, Yu X, et al. A novel prognostic nomogram based on microvascular invasion and hematological biomarkers to predict survival outcome for hepatocellular carcinoma patients. Surg Oncol. 2020;33:51–57.
28. Ho SY, Phua K, Wong L, et al. Extensions of the external validation for checking learned model interpretability and generalizability. Patterns. 2020;1(8):100129.
29. Li Y, Ruan DY, Jia CC, et al. Surgical resection versus liver transplantation for hepatocellular carcinoma within the Hangzhou criteria: a preoperative nomogram-guided treatment strategy. Hepatobiliary Pancreat Dis Int. 2017;16(5):480–486.
30. Hsu CY, Liu PH, Ho SY, et al. Impact of tumor burden on prognostic prediction for patients with terminal stage hepatocellular carcinoma: a nomogram study. PLoS One. 2017;12(11):e0188031.
31. Huang K, Liao X, Han C, et al. Genetic variants and expression of cytochrome p450 oxidoreductase predict postoperative survival in patients with hepatitis B virus-related hepatocellular carcinoma. J Cancer. 2019;10(6):1453–1465.
32. Liu CY, Chen KF, Chen PJ. Treatment of liver cancer. Cold Spring Harb Perspect Med. 2015;5(9):a021535.
33. Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–1314.
34. Li Y, Zhang R, Xu Z, et al. Advances in nanoliposomes for the diagnosis and treatment of liver cancer. Int J Nanomedicine. 2022;17:909–925.
35. Sheng R, Jin K, Sun W, et al. Prediction of therapeutic response of advanced hepatocellular carcinoma to combined targeted immunotherapy by MRI. Magn Reson Imaging. 2023;96:1–7.
36. Li W, Shen H, Han L, et al. A multiparametric fusion radiomics signature based on contrast-enhanced MRI for predicting early recurrence of hepatocellular carcinoma. J Oncol. 2022;2022:3704987.
37. Zhu HB, Zheng ZY, Zhao H, et al. Radiomics-based nomogram using CT imaging for noninvasive preoperative prediction of early recurrence in patients with hepatocellular carcinoma. Diagn Interv Radiol. 2020;26(5):411–419.
38. Jin Z, Wang M, Meng Y, et al. Prognostic implication of a cuproptosis-related miRNA signature in hepatocellular carcinoma. J Healthc Eng. 2022;2022:4694323.
39. Tao H, Wang C, Lu C, et al. Comprehensive analysis on the specific role and function of mitochondrial inner membrane protein MPV17 in liver hepatocellular carcinoma. Genet Res (Camb). 2022;2022:7236823.
40. Dai K, Liu C, Guan G, et al. Identification of immune infiltration-related genes as prognostic indicators for hepatocellular carcinoma. BMC Cancer. 2022;22(1):496.
41. Zhou T, Wang T, Zeng K, et al. A nomogram based on a three pyroptosis gene model and clinical parameters for predicting prognosis of hepatocellular carcinoma. Gene. 2022;819:146243.
42. Li L, Xie R, Lu G. Identification of m6A methyltransferase-related lncRNA signature for predicting immunotherapy and prognosis in patients with hepatocellular carcinoma. Biosci Rep. 2021;41(6):BSR20210760.
43. Zeng H, Liu C, Zhou X, et al. A new prognostic strategy based on four DNA repair-associated lncRNAs for hepatocellular carcinoma. Comb Chem High Throughput Screen. 2022;25(5):906–918.
44. Li TE, Zhang Z, Wang Y, et al. A novel immunotype-based risk stratification model predicts postoperative prognosis and adjuvant TACE benefit in Chinese patients with hepatocellular carcinoma. J Cancer. 2021;12(10):2866–2876.
45. Wang H, Lu Y, Liu R, et al. A Non-invasive nomogram for preoperative prediction of microvascular invasion risk in hepatocellular carcinoma. Front Oncol. 2021;11:745085.
46. Liu H, Yang M, Dong Z. HSPB11 is a prognostic biomarker associated with immune infiltrates in hepatocellular carcinoma. Int J Gen Med. 2022;15:4017–4027.
47. Wang X, Gong Y, Deng T, et al. Diagnostic and prognostic significance of mRNA expressions of apolipoprotein A and C family genes in hepatitis B virus-related hepatocellular carcinoma. J Cell Biochem. 2019;120(10):18246–18265.
48. Ji K, Zhu H, Wu W, et al. Tumor response and nomogram-based prognostic stratification for hepatocellular carcinoma after drug-eluting beads transarterial chemoembolization. J Hepatocell Carcinoma. 2022;9:537–551.
49. Yan H, Wang X, Zhou D, et al. Dynamic nomogram for predicting macrovascular invasion of patients with unresectable hepatocellular carcinoma after transarterial chemoembolization. J Cancer. 2022;13(6):1914–1922.
50. Chen X, Lu Y, Shi X, et al. Development and validation of a novel model to predict regional lymph node metastasis in patients with hepatocellular carcinoma. Front Oncol. 2022;12:835957.
51. Bai Y, Lian Y, Wu J, et al. A prognostic scoring system for predicting overall survival of patients with the TNM 8th edition stage I and II hepatocellular carcinoma after surgery: a population-based study. Cancer Manag Res. 2021;13:2131–2142.
52. Zhang Z, Li J, He T, et al. The competitive endogenous RNA regulatory network reveals potential prognostic biomarkers for overall survival in hepatocellular carcinoma. Cancer Sci. 2019;110(9):2905–2923.
53. Zhang Z, Ouyang Y, Huang Y, et al. Comprehensive bioinformatics analysis reveals potential lncRNA biomarkers for overall survival in patients with hepatocellular carcinoma: an on-line individual risk calculator based on TCGA cohort. Cancer Cell Int. 2019;19:174.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.