Back to Journals » Veterinary Medicine: Research and Reports » Volume 13
Epidemiology and Antimicrobial Susceptibility Pattern of E. coli O157:H7 Along Dairy Milk Supply Chain in Central Ethiopia
Authors Dejene H , Abunna F, Tuffa AC, Gebresenbet G
Received 17 March 2022
Accepted for publication 2 June 2022
Published 9 June 2022 Volume 2022:13 Pages 131—142
DOI https://doi.org/10.2147/VMRR.S366888
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Young Lyoo
Haileyesus Dejene,1 Fufa Abunna,2 Ashenafi Chaka Tuffa,3 Girma Gebresenbet4
1Department of Veterinary Epidemiology and Public Health, College of Veterinary Medicine and Animal Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Clinical Studies, College of Veterinary Medicine and Agriculture, Addis Ababa University, Bishoftu, Ethiopia; 3Department of Horticulture, College of Agriculture and Veterinary Science, Ambo University, Ambo, Ethiopia; 4Department of Energy and Technology, Swedish University of Agricultural Sciences, Uppsala, Sweden
Correspondence: Haileyesus Dejene, Email [email protected]
Background: Enterohemorrhagic Escherichia coli (O157:H7) is the primary cause of bloody diarrhea or hemorrhagic colitis. The study was carried out with to determine the epidemiology and antimicrobial resistance pattern of E. coli O157:H7 along the dairy supply chains in Akaki Kaliti sub-city of Addis Ababa, Bishoftu and Sululta towns of central Ethiopia.
Methods: A cross-sectional study design with random sampling methods was employed. Thus, a total of 450 raw cow milk (294), milker hand swab (65) and water (91) samples were collected from dairy farms, milk collection centers and Cafeterias and processed according to the standards to isolate and identify E. coli O157:H7. The samples were initially enriched in buffered peptone water, then plated onto Sorbitol MacConkey agar. Consequently, the suspected non-sorbitol fermenting colonies were confirmed as E. coli biochemically and serological test using latex agglutination tests.
Results: Out of the total 450 samples examined, 6.0% were found to be contaminated by E. coli O157:H7. Accordingly, 9.89% of water, 9.23% of milker hand swab and 4.08% of raw milk samples were contaminated by the pathogen. Furthermore, the prevalence of E. coli O157:H7 was 7.79%, 6.21% and 3.97% in Akaki kaliti sub-city, Sululta and Bishoftu towns, respectively. The result of Fisher exact analysis revealed a significant difference observed (p < 0.05) between the occurrence of the pathogen and the source of sample, sources of water used, sampled material and type of containers. The study also revealed that varying level of resistance of E. coli O157:H7 isolates against nine antimicrobial discs tested and 100% (n = 27) of the isolates showed multidrug-resistance comprising from two up to seven antimicrobial drugs.
Conclusion: In conclusion, this study has indicated the occurrence of E. coli O157:H7 and its multiple drug-resistant profiles in milk samples along the dairy supply chains and its risk to public health and food safety. Therefore, proper hygienic practices from dairy farms to fork and rational drug usage are recommended.
Keywords: antimicrobial resistance, critical control points, Escherichia coli O157:H7, Ethiopia, milk
Introduction
Food-borne pathogens are the leading cause of illness, despite the substantial scientific research and technical improvements in developed countries in recent years, and death in developing countries costs billions of dollars in medical care and medical and social costs.1 Occasional cases and outbreaks of human diseases caused by food-borne pathogens have been linked to ground beef, raw milk, meat and dairy products, vegetables, unpasteurized fruit juices, and water. One of the most common causes of food-borne disease is contaminated raw milk.2,3 In addition, it is an ideal medium for the growth of various bacteria.4 Escherichia coli is one of the many microorganisms that can get access to milk and milk byproducts.5 Moreover, many E. coli strains are harmless or beneficial to the host. Some strains of E. coli, however, are harmful to humans and are found in food animals. Among them, E. coli O157:H7 is the best-known pathogenic strain.6,7
Enterohemorrhagic Escherichia coli (O157:H7) is the primary cause of bloody diarrhea or hemorrhagic colitis. Thus, the synthesis of verocytotoxins,8 commonly known as Shiga toxins, is a distinguishing trait of this group (Stx).9 Moreover, cattle are the primary reservoir of E. coli O157:H7 and an important source of human infection10 and undercooked ground beef and unpasteurized milk being common vehicles of the pathogen transmission.11 The food-borne E. coli O157:H7 is estimated to cause 2.8 million acute illnesses each year worldwide.12 In addition, an estimated 73,480 infections caused by E. coli O157:H7 infection occur in the United States each year, resulting in an estimated 2168 hospitalizations and 61 deaths13,14 and a 607 million US dollar economic burden.15 It has emerged as an important global zoonotic food and water-borne pathogen.16,17
International food management organizations, particularly the World Health Organization (WHO), the Food and Agriculture Organization (FAO), and the International Hazard Analysis Critical Control Point (HACCP) alliance, have already provided guidelines to member countries on safe handling procedures such as HACCP and Good Manufacturing Practices (GMP) to reduce the risk of zoonotic infection transmission associated with contaminated food.1,18,19 Furthermore, antibiotic resistance in E. coli has been found globally, and rising resistance rates in E. coli are a significant issue in both developed and developing countries. As a result, an increase in bacterial resistance to antibiotics complicates infection therapy.20 A few studies have been carried out in Ethiopia to examine the prevalence and antibiotic resistance patterns of E. coli from various clinical sources.21 Recent research findings22–27 have proven that E. coli O157:H7 has developed resistance to a variety of routinely used medicines, including erythromycin, amoxicillin-clavulanic acid, sulfonamides, ampicillin, and tetracycline, and those certain strains have gained multidrug resistance.
Furthermore, little is known about the frequency, distribution, and related virulent genes of E. coli O157:H7 in humans, animals, or animal-derived foods in Ethiopia.22,23,28 Also, it is unclear to what extent milk producers’ and retailers’ homes serve as a source of E. coli O157:H7 contamination for dairy products. As a result, research into this pathogenic organism contributes to a better understanding of its epidemiology by identifying transmission routes, vehicles, and sources of milk contamination. Therefore, the aims of the present study were to assess the prevalence of E. coli O157:H7 in raw cow milk, milker hand swabs, and water samples, as well as to determine the pattern of antimicrobial resistance along the dairy supply chain.
Methods
Description of the Study Areas
The study was carried out at Akaki Kaliti sub-city of Addis Ababa, Bishoftu and Sululta towns of central Ethiopia. Samples were collected from dairy farms, milk collection centres and cafeterias located at the aforementioned towns. The study areas are known for their high potential for dairy production and located in the central highlands of Ethiopia. Bishoftu and Sululta towns are located in Oromia National Regional State located at a distance of 47 km southeast and 23 km northwest of the capital Addis Ababa, respectively. Bishoftu town is situated between 8°44′4.74′′ North latitude and 39°0′30.72′′ East longitude. The altitude of the town ranges from 1900 to 1995 meters above sea level. Sululta is situated between 9°11′00′′ North latitude and 38°44′59.99′′ East longitude. It lies at an altitude of 2500 meters above sea level.29 Akaki Kaliti sub-city is one of the ten sub-cities of Addis Ababa. It is situated at a latitude of 8°53′40.92′′ North and 38°46′23.52′′ longitude of East. It lies at an altitude of 2140 meters above sea level.30
Study Design
A cross-sectional study design was carried out to determine the epidemiology and antimicrobial sensitivity pattern of E. coli O157:H7 from farm to fork along the dairy supply chains in central Ethiopia.
Sample Size Determination
The required sample size was calculated by considering a previously published prevalence estimate of 6.9% by31 reported from a study on the bacterial isolates from raw cow milk in Holeta district. Therefore, the required sample size was calculated as 98 based on the prevalence estimate described above (6.9%). Accordingly, a total of 294 (226 from farmers, 42 from milk collection centers and 26 from cafeterias) raw cow milk samples were collected from the study areas.
Sampling Strategy
First, a baseline survey was done in the research areas to determine the total number of farms, farm size, farming system, and the status and number of milk collection centers and cafeterias. According to the survey results, dairy farms were divided into three categories based on herd size (small, medium, and large-scale commercial dairy farms) for the collection of raw cow milk samples from dairy farms. Furthermore, as explained by Dohoo et al,32 the proportionate stratified random sampling method was used to allocate the number of samples to be gathered from each stratum in proportion to the total number in the stratum. A simple random sampling technique was employed to collect milk from dairy farms, collection centers and cafeterias. Furthermore, water and swab samples were collected from each dairy farm, milk collection centers and cafeterias.
Sample Collection and Transportation
A sterile syringe was used to collect 5 mL of milk samples aseptically from bulk milk buckets and tanks on dairy farms, as well as tanks in milk collecting centers and cafeterias, into a sterile screw-capped falcon tube. Similarly, 5 mL of water was collected from a water tank for routine cleanliness of equipment and staff in dairy farms, milk collection centers, and cafeterias. For sampling and transferring the milker hand swab samples, sterile cotton swabs with breakable sticks were immersed in a tube containing 10 mL of dilution fluid, buffered peptone water.33 Following that, the samples were maintained in a refrigerator at 4°C until analysis, and culturing was completed within 24 hours as stated by.34
Laboratory Investigation
Isolation and Identification of E. coli O157:H7
Each raw milk and water sample (1 mL) was supplemented with 9 mL of buffered peptone and incubated for 18–24 hours at 37°C. Similarly, a swab sample in 10 mL BPW was incubated for 18–24 hours at 37°C. After carefully mixing the enrichment, ten microliters (10 µL) of the enriched samples were placed onto Sorbitol MacConkey agar and incubated at 37°C for 24 hours. Following that, typical colonies on SMAC agar (pale, unable to ferment sorbitol) were moved to nutrient agar for further confirmatory biochemical tests (indole and KIA tests) and serological tests, as reported by.34
Serological Test
The serological confirmation of E. coli-sorbitol-negative colonies was performed using an E. coli 57:H7 latex agglutination assay using latex particles coated with antibodies specific for the E. coli O157 and E. coli H7 antigens. Identification of E. coli O157:H7 was carried out following the manufacturer’s instructions, colonies that agglutinated were assumed to be E. coli O157:H7.
Antimicrobial Susceptibility Testing
The Clinical and Laboratory Standards Institute’s Kirby Bauer disc diffusion method on Mueller Hinton agar was used to determine the antimicrobial susceptibility pattern of E. coli O157:H7 isolates.35 The isolates of E. coli O157:H7 were evaluated for sensitivity to the most commonly used antimicrobials, including ampicillin (AMP/10 μg), cefoxitin (FOX/30 μg), streptomycin (S/10 μg), tetracycline (TE/30 μg), ciprofloxacin (CIP/5 μg), gentamicin (GEN/10 μg), sulfamethoxazole (RL/100 μg), trimethoprim (TR/25 μg) and doxycycline (DO/30 μg). Furthermore, isolates that showed resistance to two or more antimicrobials were labeled as multidrug-resistant.36
Data Management and Statistical Analysis
The data obtained was classified, filtered and coded using Microsoft Excel® 2010. The data was then be exported to STATA version 14 (Stata Corp., Texas, USA) for appropriate statistical analysis. Then, the Fisher’s exact test was used to measure the association of E. coli O157:H7 occurrence with incriminated categorical risk factors. Also, logistic regression analysis was utilized to measure the degree of association between the risk factors and E. coli O157:H7 occurrence. The data were interpreted as significant when the p-value is less than 0.05. Meanwhile, for antimicrobial susceptibility test, the results were interpreted according to Clinical and Laboratory Standards Institute35 interpretive criteria for Enterobacteriaceae.
Results
Overall Prevalence of Escherichia coli O157:H7
Out of the total of 450 samples examined in the present study, Escherichia coli O157:H7 was isolated from 27 (6.0%) of the samples based on latex agglutination assay. Accordingly, 12 (7.79%), 9 (6.0%) and 6 (3.97%) of the samples were found to be contaminated by the pathogen in Akaki kaliti sub-city, Sululta and Bishoftu towns, respectively. On the other hand, from the total 294 milk samples examined at the different sampling point, E. coli O157:H7 was contaminates 9 (34.62%) of the milk samples from cafeterias and 3 (1.33%) of the milk samples from dairy farms (Table 1).
 |
Table 1 Prevalence of E. coli O157:H7 from Different Sample Types in Dairy Supply Chains, Central Ethiopia |
Association of Risk Factors with Escherichia coli O157:H7 Occurrence
There was statistically significant difference observed (p < 0.05) between the occurrences of E. coli O157:H7 with the source of sample, sources of water used, sampled material and type of containers. However, there was no statistically significant difference observed (p > 0.05) between the occurrence of the pathogen with the study area, type of sample and scales of dairy farms (Table 2).
 |
Table 2 Association of Risk Factors with E. coli O157:H7 Occurrence Along Dairy Supply Chains |
Association Escherichia coli O157:H7 Occurrence in Milk Sample
Out of the total 294 milk samples examined, 4.08% (n = 12) of the samples were contaminated by E. coli O157:H7. Also, it indicated that there was no statistically significant difference observed (p > 0.05) between the occurrences of E. coli O157:H7 with the study area and dairy farm scales. There was statistically significant difference observed (p < 0.05) between the occurrence of the pathogen with the source of samples, sampled materials and source of water used (Table 3).
 |
Table 3 Univariable Logistic Regression Analysis Based on Prevalence of E. coli O157:H7 in the Milk Samples and Associated Risk Factors |
Association Escherichia coli O157:H7 Occurrence in Water Sample
On the other hand, out of the total 91 water samples examined, 9.89% (n = 9) of the samples were found to be contaminated by E. coli O157:H7. There was no statistically significant difference observed (p > 0.05) between the occurrence of the pathogen with the study areas and type of containers used. However, there was statistically significant difference observed (p < 0.05) between the occurrence of the pathogen with the sources of samples and sources of water used. Also, the occurrence of E. coli O157:H7 was significantly (p = 0.004) higher (27.59%) in the well water with 23.2 (95% CI 2.74, 196.9) times more likely to occur than pipe water sources (Table 4).
 |
Table 4 Univariable Logistic Regression Analysis Based on Prevalence of E. coli O157:H7 in the Water Samples and Associated Risk Factors |
Association of Escherichia coli O157:H7 Occurrence in Swab Sample
Out of the total 65 milker hand swab samples examined, 9.23% (n = 6) of the samples were positive for E. coli O157:H7. There was no statistically significant difference observed (p > 0.05) between the occurrences of E. coli O157:H7 in the study areas, dairy farm scales, and water sources. However, the occurrence of the pathogen was 1.94 (95% CI 0.29, 12.95) times more likely to occur in the milker’s hand from dairy farm in Sululta than dairy farms in Akaki Kaliti sub-city dairy (Table 5).
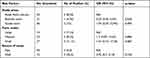 |
Table 5 Univariable Logistic Regression Analysis Based on Prevalence of E. coli O157:H7 in the Milker’s Hand Swab Samples and Associated Risk Factors |
Antimicrobial Susceptibility Profile of E. coli O157:H7
The study of antimicrobial sensitivity of E. coli O157:H7 recovered from different sample types revealed that, of the total 27, all isolates were resistant to ampicillin and cefoxitin. On the other hand, 70.37% (n = 19), 59.26% (n = 16), 37.04% (n = 10), 25.93% (n = 7), 22.22% (n = 6) and 14.81% (n = 4) were found to be resistant to streptomycin, tetracycline, doxycycline, gentamicin, sulfamethoxazole and trimethoprim, respectively. None of the isolates was resistant to ciprofloxacin (Table 6). In addition, multidrug resistance analysis showed that 27/27 (100%) of tested E. coli O157:H7 isolates were resistant to different combinations of two or more antimicrobials. A multidrug-resistance pattern consisting of seven drugs was seen in 3/27 (11.11%) isolates (Table 7).
 |
Table 6 Overall Antimicrobial Susceptibility Profile of E. coli O157:H7 |
 |
Table 7 The Fortitude Demonstration of Multidrug-Resistance Pattern of E. coli O157:H7 Isolates |
Discussion
Food-borne diseases are one of the most serious public health issues in developing countries, including Ethiopia. Human infections with E. coli O157:H7 have largely been linked to animal-sourced meals.37 Therefore, information on the incidence of these infections and their susceptibility to antimicrobials help the policy makers to develop appropriate strategies regarding prevention, treatment and control protocols.
Upon this study, from the different sample types examined the prevalence of E. coli O157:H7 was higher in the water samples (9.89%) when compared with milkers’ hand swab (9.23%) and raw cow milk (4.08%) samples. Also, there were no statistically significant differences observed (p = 0.057) between the occurrence of the pathogen and source of samples.38 This study showed a slightly higher rate of raw milk contamination by E. coli O157:H7 compared with the reports of26 in and around Asosa western Ethiopia who have reported as 2.90%. Similarly, the current finding from raw cow milk was higher when compared with the reports from abroad by39 in Libya (3.5%),40 in Nigeria (2%),41 in Greece (0.74%),42 in Egypt (0.5%),43 in Turkey (0.0%),44 in Tanzania (0.0%) and45 in Ghana (0.0%). The greater finding in this study could be attributed to variations in dairy farming type, such as the emphasis on livestock systems in other countries, geographic location, and the level of sanitary precautions.
Meanwhile, the current finding from raw cow milk was lower when compared with the reports of46 in Iraq,31 in Holeta and27 in Bishoftu towns who have reported prevalence estimates of 4.67%, 6.9% and 12%, respectively. The variation in E. coli O157:H7 contamination frequency reported in different research could be attributed to differences in sample size, dairy farming system, milking techniques, location, and sanitary procedures applied across different regions and study areas. As a result, the presence of E. coli O157:H7 does not necessarily indicate direct faecal contamination of milk, but it is an indicator of poor hygiene and unclean practices during milking and subsequent milk handling, and it poses a potential risk to people who consume such products.47
On the other hand, in this study, E. coli O157:H7 was isolated from 9.89% of the water samples. Also, from the different sampling points, a relatively higher contamination frequency of water by the pathogen was observed in water samples collected from cafeterias (23.10%) when compared with water collected from dairy farms (5.20%) and the variation was not statistically significant (p = 0.198).38 However, this study showed a higher rate of water contamination (9.89%) by the pathogen compared with the reports of28 in Modjo and48 in Batu towns who have reported 4.3% and 3.3% contamination frequency, respectively. The discrepancies seen could be attributed to variances in methodologies used, the absence of well water treatment or disinfection, carelessness in water usage, sample size, and geographical regions where the investigations were done. Consequently, the bacteriological quality of water destined for sanitation and domestic uses is affected by quality status at the source and water handling practices during collection, transportation, and storage; comparable thoughts were reflected by.49
Similarly, in the current study, E. coli O157:H7 was isolated from 9.23% of the milkers’ hand swab in the dairy farms. In addition, a higher contamination frequency of the pathogen was observed from dairy farms in Sululta town (15%) when compared with dairy farms in Akaki Kaliti sub-city (8.33%) and Bishoftu town (4.76%), by which the variation was not statistically significant (p > 0.05).38 However, compared to this study,50 Msolo et al in South Africa have reported 7% isolation frequency and this was lower than the present finding. The observed variation could be attributed to differences in hygiene procedures, sample size, geographical location, and water supply used between the various locations and study sites. In the course of the study, from the total 27 isolates tested ≥50% susceptibility to the antimicrobials was found to be ciprofloxacin (92.5%), trimethoprim (85.19%), gentamicin (59.26%) and sulfamethoxazole (55.56%). The current finding was in line with the reports of51 in Nigeria,52 in Bangladesh and27 in Bishoftu town who have reported 89.5% and 78.9%; 50% and 66.67%, and 100% and 85.7% susceptibility of E. coli O157:H7 isolates to gentamicin and ciprofloxacin, respectively. However, the current finding was in contrast to the reports of26 in and around Asosa town who have reported 36.4% to gentamicin. The observed variance could be attributed to the pathogen’s expression of resistant gene code, which is related with emerging and re-emerging characteristics of the isolates in terms of diverse agro-ecology.51
On the other hand, the finding revealed that ≥50% of E. coli O157:H7 isolates were found to be resistant to ampicillin, cefoxitin, streptomycin and tetracycline. This was in agreement with the findings of26 in and around Asosa and27 in Bishoftu towns who have reported ≥50% of resistance rate to ampicillin, streptomycin and cefoxitin. Similarly,26,51,52 Disassa et al, Reuben et al and Alam et al have reported ≥50% resistance rate to tetracycline. As a result, the emergence of resistance could be attributed to the inappropriate or indiscriminate use of antibiotics for therapeutic and preventive purposes in both E. coli and other illnesses. In the present study, 27/27 (100%) of E. coli O157:H7 isolates exhibited resistance to at least two or more of the nine antimicrobial agents tested. Compared to this finding,27 in Bishoftu town has reported 100% resistance of all the isolates to more than two drugs from milk. Also,53 and54 have also reported 100% and 73.3% resistance rate of the isolates to two or more drugs, respectively, in an abattoir-based study conducted in Ethiopia and this was in agreement with this finding. Likewise, in this study, the higher rate of multidrug-resistance was observed for four drugs (29.63%) followed by six (18.52%), three (18.52%) and two (14.81%) drugs. In contrast to this, the resistance of (57.1%) to two (28.6%) to three and (14.3%) to four drugs were reported by Bedasa et al.27 Also, the resistance of 71.4% and 28.6%, and 40% and 13.3% for three and four drugs were also reported by Bekele et al24 and Atnafie et al,54 respectively, from an abattoir-based investigation, Ethiopia. As a result, the emergence of antibiotic resistance in bacteria such as E. coli is a major public health concern. The variation in multidrug resistance development for bacteria may be due to variations in dose, route of administration, regimen, and continuous and indiscriminate use of antimicrobials for treatment and feed additive in various study areas, as well as level of awareness and geographic location for studies abroad. Because of the rapid development of multidrug resistance, the efficiency of treatments and the ability to manage infectious diseases in both animals and people may be significantly limited.5
Conclusion
In conclusion, the presence of E. coli O157:H7 in raw cow milk, milker hand swabs, and water samples collected along the dairy supply chain indicates a possible concern to public health and food safety. The pathogen was more prevalent in samples collected from the Akaki Kaliti sub-city. The presence of several antibiotic-resistant E. coli O157:H7 strains poses a risk to public health and food safety, as well as animal health and production. In general, this study provided an initial baseline of E. coli O157:H7 occurrence in dairy supply chains. Dairy farms should therefore undertake hygienic methods like as hand cleaning between milking, udder washing before and after milking, and the application of teat dip with iodine tincture.
Abbreviations
BPW, Buffered peptone water; SMAC, Sorbitol MacConkey agar.
Data Sharing Statement
All data generated during this study are available upon request of the correspondence author.
Ethical Approval and Consent to Participate
Before any attempt to collect sample, the protocol was approved by Addis Ababa University College of Veterinary Medicine and Agriculture animal research ethical committee with reference number VM/ERC/21/05/10/2018.
Acknowledgments
The researchers would like to thank Addis Ababa University office of the Vice President for Research and technology Transfer for Financial and other supports. We also acknowledge the priceless support given by the dairy farm owners.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Addis Ababa University office of the Vice President for Research and technology Transfer.
Disclosure
The authors have no conflicts of interest to declare. This manuscript is a part of an MVSc thesis entitled as “Epidemiology and assessment of critical control points of E. coli O157:H7 along dairy supply chains in central Ethiopia” and you can get online access to the full thesis paper in the repository directorate of Addis Ababa University.
References
1. Rahimi E, Momtaz H, Anari M, Alimoradi M, Momen M, Riahi M. Isolation and genomic characterization of Escherichia coli O157: NM and Escherichia coli O157: H7 in minced meat and some traditional dairy products in Iran. African J Biotechnol. 2012;11:2328–2332. doi:10.5897/AJB11.2167
2. Ali N, Farooqui A, Khan A, Khan A, Kazmi S. Microbial contamination of raw meat and its environment in retail shops in Karachi, Pakistan. J Infect Dev Countries. 2010;4:382–388. doi:10.3855/jidc.599
3. Javaid S, Gadahi J, Khaskeli M, Bhutto M, Kumbher B, Panhwar A. Physical and chemical quality of market milk sold at Tandojam, Pakistan. Pak Vet J. 2009;29:27–31.
4. Popescu A, Angel E. Analysis of milk quality and its importance for milk processors. Lucrãri Tiinþifice Zootehnie Biotechnol. 2009;42:501–506.
5. Thaker H, Brahmbhatt M, Nayak J. Study on occurrence and antibiogram pattern of E. coli from raw milk samples in Anand, Gujarat, India. Vet World. 2012;5:556–559. doi:10.5455/vetworld.2012.556-559
6. Riemann P, Cliver O. Foodborne Infection and Intoxication.
7. Oliver S, Boor K, Murphy S, Murinda S. Food safety hazards associated with consumption of raw milk. J Foodborne Pathogens Dis. 2009;6:793–806. doi:10.1089/fpd.2009.0302
8. Bandyopadhyay S, Lodh C, Rahaman H, et al. Characterization of shiga toxin-producing (STEC) and enteropathogenic Escherichia coli (EPEC) in raw yak (Poephagus grunniens) milk and milk products. J Res Vet Sci. 2012;93:604–610. doi:10.1016/j.rvsc.2011.12.011
9. Gordillo R, Cardoba J, Andrade M, Luque M, Rodriguez M. Development of PCR assays for detection of Escherichia coli O157: H7 in meat products. J Meat Sci. 2011;88:767–773. doi:10.1016/j.meatsci.2011.03.011
10. Varela-Herníndez J, Cabrera-Diaz E, Cardona-Lopez M, et al. Isolation and characterization of Shiga toxin-producing Escherichia coli O157: H7 and non-O157 from beef carcasses at a slaughter plant in Mexico. Int J Food Microbiol. 2007;113:237–241. doi:10.1016/j.ijfoodmicro.2006.06.028
11. Su H, Ma Q, Shang K, Liu T, Yin H, Ai S. Gold nanoparticles as colorimetric sensor: a case study on E. coli O157: H7 as a model for Gram-negative bacteria. Sensors Actuators B Chem J. 2012;161:298–303. doi:10.1016/j.snb.2011.10.035
12. Majowicz S, Scallan E, Jones-Bitton A, et al. Global incidence of human Shiga toxin-producing Escherichia coli infections and deaths: a systematic review and knowledge synthesis. J Foodborne Pathogens Dis. 2014;11:447–455. doi:10.1089/fpd.2013.1704
13. Rangel J, Sparling P, Crowe C, Griffin P, Swerdlow D. Epidemiology of Escherichia coli O157: H7 outbreaks in United States, 1982–2002. Emerg Infect Dis J. 2005;11:603–609. doi:10.3201/eid1104.040739
14. Scallan E, Hoekstra R, Angulo F, et al. Foodborne illness acquired in the United States-major pathogens. Emerg Infect Dis J. 2011;17:7–15. doi:10.3201/eid1701.P11101
15. Scharff R. Economic burden from health losses due to foodborne illness in the United States. J Food Prot. 2012;75:123–131. doi:10.4315/0362-028X.JFP-11-058
16. Chekabab S, Paquin-Veillette J, Dozois C, Harel J. The ecological habitat and transmission of Escherichia coli O157: H7. FEMS Microbiol Lett. 2013;341:1–12. doi:10.1111/1574-6968.12078
17. Pal M, Mulu S, Tekle M, Pintoo S, Prajapati J. Bacterial contamination of dairy products. J Beverage Food World. 2016;43:40–43.
18. Sikora T, Niewczas M, Prusak A. Ethics and Trust in Quality Assurance. In:
19. Bruno A, Carolissen-Mackay V. Antimicrobial resistance and the activities of the Codex Alimentarius Commission. Revue Scientifique Et Technique OIE. 2012;31:317–323. doi:10.20506/rst.31.1.2122
20. Erb A, Sturmer T, Marre R, Brenner H. Prevalence of antibiotic resistance in Escherichia coli: overview of geographical, temporal and methodological variations. Eur J Clin Microbiol Infect Dis. 2007;26:83–90. doi:10.1007/s10096-006-0248-2
21. Gebre-Sealsssie S. Antimicrobial resistance patterns of clinical bacterial isolates in southwestern Ethiopia. Ethiop Med J. 2007;45:363–370.
22. Hiko A, Asrat D, Zewde G. Occurrence of Escherichia coli O157: H7 in retail raw meat products in Ethiopia. J Infect Dev Countries. 2008;2:389–393. doi:10.3855/jidc.203
23. Taye M, Berhanu T, Berhanu Y, Tamiru F, Terefe D. Study on carcass contaminating Escherichia coli in apparently healthy slaughtered cattle in Haramaya University slaughter house with special emphasis on Escherichia coli O157: H7, Ethiopia. J Vet Sci Technol. 2013;4:1–4.
24. Bekele T, Zewde G, Tefera G, Feleke A, Zerom K. Escherichia coli O157: H7 in raw meat in Addis Ababa, Ethiopia: prevalence at an abattoir and retailers and antimicrobial susceptibility. Int J Food Contamin. 2014;1:4–9. doi:10.1186/s40550-014-0004-9
25. Mohammed O, Shimelis D, Admasu P, Feyera T. Prevalence and antimicrobial susceptibility pattern of E. coli isolates from raw meat samples obtained from abattoirs in Dire Dawa city, eastern Ethiopia. Int J Microbiol Res. 2014;5:35–39.
26. Disassa N, Sibhat B, Mengistu S, Muktar Y, Belina D. Prevalence and antimicrobial susceptibility pattern of E. coli O157: H7 isolated from traditionally marketed raw cow milk in and around Asosa town, western Ethiopia. J Vet Med Int. 2017;2017:1–7.
27. Bedasa S, Shiferaw D, Abraha A, Moges T. Occurrence and antimicrobial susceptibility profile of Escherichia coli O157: H7 from food of animal origin in Bishoftu town, central Ethiopia. Int J Food Contamin. 2018;5:1–8. doi:10.1186/s40550-018-0064-3
28. Mersha G, Asrat D, Zewde B, Kyule M. Occurrence of Escherichia coli O157: H7 in faeces, skin and carcasses from sheep and goats in Ethiopia. Lett Appl Microbiol. 2010;50:71–76. doi:10.1111/j.1472-765X.2009.02757.x
29. CSA (Central Statistical Agency). Central Statistical Agency of the Federal Democratic Republic of Ethiopia: Agricultural Samples Enumeration Statistical Abstract. Addis Ababa, Ethiopia: CSA (Central Statistical Agency); 2015:446–539.
30. NMSA (National Meteorological Service Agency). Rainfall and Temperature Data. Addis Ababa, Ethiopia: NMSA (National Meteorological Service Agency); 2017.
31. Ayano A, Hiriko F, Simyalew A, Yohannes A. Prevalence of subclinical mastitis in lactating cows in selected commercial dairy farms of Holeta district. J Vet Med Animal Health. 2013;5:67–72.
32. Dohoo I, Martin W, Stryhn H. Veterinary Epidemiologic Research. Charlotte town, Prince Edward Island, Canada: AVC Inc; 2003:27–52.
33. ISO (International Organization for Standardization) 18593. Microbiology of Food and Animal Feeding Stuffs: Horizontal Methods for Sampling Techniques from Surfaces Using Contact Plates and Swabs.
34. Quinn P, Carter M, Markey B, Carter G. Clinical Veterinary Microbiology. London, UK: Mosby Ltd; 2004:95–101.
35. CLSI (Clinical and Laboratory Standards Institute). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fifth Informational Supplement. CLSI Document M100-S25. Vol. 35 No. 3. Wayne, PA: CLSI (Clinical and Laboratory Standards Institute); 2015:32–194.
36. Hill D, Rose B, Pajkos A, et al. Antibiotic susceptibilities of Pseudomonas aeruginosa isolates derived from patients with cystic fibrosis under aerobic, anaerobic, and biofilm conditions. J Clin Microbiol. 2005;43:5085–5090. doi:10.1128/JCM.43.10.5085-5090.2005
37. Jo M, Kim J, Lim J, et al. Prevalence and characteristics of Escherichia coli O157 from major food animals in Korea. Int J Food Microbiol. 2004;95:41–49. doi:10.1016/j.ijfoodmicro.2004.01.016
38. Dejene H. Epidemiology and Assessment of Critical Control Points of E. coli O157: H7 Along Dairy Supply Chains in Central Ethiopia. MVSc thesis. Addis Ababa University College of Veterinary Medicine and Agriculture. Bishofu, Ethiopia. 2018. Available from: http://etd.aau.edu.et/handle/123456789/12299.
39. Garbaj A, Awad E, Azwai S, et al. Enterohemorrhagic Escherichia coli O157 in milk and dairy products from Libya: isolation and molecular identification by partial sequencing of 16S rDNA. Vet World. 2016;9:1184–1189. doi:10.14202/vetworld.2016.1184-1189
40. Ivbade A, Ojo O, Dipeolu M. Shiga toxin-producing Escherichia coli O157: H7 in milk and milk products in Ogun state, Nigeria. Vet Ital. 2014;50:185–191. doi:10.12834/VetIt.129.2187.1
41. Solomakos N, Govaris A, Angelidis A, et al. Occurrence, virulence genes and antibiotic resistance of Escherichia coli O157 isolated from raw bovine, caprine and ovine milk in Greece. Int J Food Microbiol. 2009;26:865–871. doi:10.1016/j.fm.2009.06.002
42. Ahmed A, Shimamoto T. Isolation and molecular characterization of Salmonella enterica, Escherichia coli O157: H7 and Shigella spp. from meat and dairy products in Egypt. Int J Food Microbiol. 2014;168:57–62. doi:10.1016/j.ijfoodmicro.2013.10.014
43. Sancak Y, Sancak H, Isleyici O. Presence of E. coli O157 and O157: H7 in raw milk and van herby cheese. Bull Vet Inst Pulawy. 2015;59:511–514. doi:10.1515/bvip-2015-0076
44. Swai E, Schoonman L. Microbial quality and associated health risks of raw milk marketed in the Tanga region of Tanzania. Asian Pac J Trop Biomed. 2011;1:217–222. doi:10.1016/S2221-1691(11)60030-0
45. Addo K, Mensah G, Aning K, et al. Microbiological quality and antibiotic residues in informally marketed raw cow milk within the coastal Savannah zone of Ghana. J Trop Med Int Health. 2011;16:227–232. doi:10.1111/j.1365-3156.2010.02666.x
46. Basil A, Khudor M, Abid-Smeasem O. Detection of verotoxigenic E. coli O157: H7 in raw milk using duplex PCR in Basra city, Iraq. Mirror Res Vet Sci Animals. 2012;1:25–33.
47. Arafa M. Bacteriological quality and safety of raw cow’s milk and fresh cream. Slovenian Vet Res. 2013;50:21–30.
48. Mekonnen M, Assefa F, Lemma B, Von-haaren C, Haaren P. Assessing the occurrence of waterborne pathogens in Lake Ziway and drinking water system of Batu (Ziway) town, Ethiopia. Ethiop J Health Dev. 2014;28:116–125.
49. Rufener S, Mausezahl D, Mosler H, Weingartner R. Quality of drinking water at source and point of consumption drinking cup as a high potential recontamination risk: a field study in Bolivia. J Health Popul Nutr. 2010;28:34–41. doi:10.3329/jhpn.v28i1.4521
50. Msolo L, Igbinosa E, Okoh A. Prevalence and antibiogram profiles of Escherichia coli O157: H7 isolates recovered from three selected dairy farms in the Eastern Cape Province, South Africa. Asian Pacific J Trop Dis. 2016;6:990–995. doi:10.1016/S2222-1808(16)61170-2
51. Reuben R, Owuna G. Antimicrobial resistance patterns of Escherichia coli O157: H7 from Nigerian fermented milk samples in Nasarawa state, Nigeria. Int J Pharm Sci Invent. 2013;2:38–44.
52. Alam M, Akther S, Sarwar N, Morshed S, Debnath G. Prevalence and antimicrobial susceptibility of E. coli O157 isolated from raw milk marketed in Chittagong, Bangladesh. Turk J Agric Food Sci Technol. 2017;5:214–220. doi:10.24925/turjaf.v5i3.214-220.976
53. Dulo F, Feleke A, Szonyi B, Fries R, Baumann M, Grace D. Isolation of multidrug-resistant Escherichia coli O157 from goats in the Somali region of Ethiopia: a cross-sectional, Abattoir-based study. PLoS One. 2015;10:e0142905. doi:10.1371/journal.pone.0142905
54. Atnafie B, Paulos D, Abera M, et al. Occurrence of Escherichia coli O157: H7 in cattle faeces and contamination of carcass and various contact surfaces in abattoir and butcher shops of Hawassa, Ethiopia. J BMC Microbiol. 2017;17:24–30. doi:10.1186/s12866-017-0938-1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
