Back to Journals » Infection and Drug Resistance » Volume 17
Epidemiological and Clinical Characteristics of Neonatal Ureaplasma urealyticum Infection
Authors Ma J , Wang Z, Luo C , Xi J , Wang X , Hu Y , Zhu C, Jin Z
Received 11 December 2023
Accepted for publication 23 March 2024
Published 3 April 2024 Volume 2024:17 Pages 1323—1332
DOI https://doi.org/10.2147/IDR.S452014
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Jun’e Ma,1,* Zhenhui Wang,1,* Chuanjin Luo,2 Jin’ou Xi,1 Xiaojing Wang,1 Yan Hu,1 Chengliang Zhu,3 Zhengjiang Jin1
1Department of Clinical Laboratory, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430070, People’s Republic of China; 2State Key Laboratory of Virology College of Life Sciences, Wuhan University, Wuhan, 430060, People’s Republic of China; 3Department of Clinical Laboratory, Institute of Translational Medicine, Renmin Hospital of Wuhan University, Wuhan, 430060, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhengjiang Jin, Department of Clinical Laboratory, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430070, People’s Republic of China, Email [email protected] Chengliang Zhu, Department of Clinical Laboratory, Institute of Translational Medicine, Renmin Hospital of Wuhan University, Wuhan, 430060, People’s Republic of China, Email [email protected]
Purpose: To understand the epidemiology and clinical features of Ureaplasma urealyticum (UU) infection in hospitalized neonates due to vertical transmission from mother to child.
Methods: Respiratory secretions were collected from neonates hospitalized in the neonatology department of the Maternal and Child Health Hospital of Hubei Province from July 2020 to June 2022, and PCR was used to detect UU-DNA in respiratory secretions. The neonates were divided into UU-positive and UU-negative groups, the epidemiological and clinical characteristics of two groups, were statistically analyzed.
Results: A total of 7257 hospitalized neonates were included in this study, of whom 561 were UU positive and 6696 were UU negative, with a UU detection rate of 7.73%. The detection rate among female neonates was higher than male neonates, and the highest detection rate was found in the period from 1– 7 days after birth; the detection rate was highest in spring and fall, and the lowest in winter, but the overall difference was not statistically significant (P> 0.05). Compared with the UU-negative group, neonates in the UU-positive group were more likely to be preterm, have a lower birth weight, be delivered vaginally, and have maternal preterm rupture of membranes. In addition, neonates in the UU-positive group were more likely to be co-infected with pathogens and to have complications related to UU infections, which were all statistically significant (P< 0.05).
Conclusion: Neonatal UU infections are detected more frequently in female infants, with the highest detection rate occurring in 1– 7 days after birth, and the most prevalent periods for infection being spring and fall. Vaginal delivery and premature rupture of membranes may lead to an increased risk of vertical UU transmission from mother to child, and UU infection is strongly associated with preterm labor, low birth weight, pathogen co-infection, and related complications.
Keywords: Ureaplasma urealyticum, neonates, infection, epidemiology, clinical characteristics, co-infection
Introduction
Ureaplasma urealyticum (UU) is the smallest prokaryotic organism between bacteria and viruses, belonging to the opportunistic pathogens, is one of the main pathogens of sexually transmitted diseases, easy to cause adult male and female urogenital tract disorders, especially in women of childbearing age.1–3 It has been reported that the UU detection rate among women during pregnancy is as high as 82%.4 In addition, the impact of UU infection in the perinatal period should not to be ignored, which can spread upward through the lower genital tract of pregnant women, causing intrauterine infections, and leading to miscarriage, preterm labor, low birth weight babies, and other adverse maternal outcomes.5–7 UU can also be transmitted vertically through the placenta or birth canal during delivery and infect the fetus, resulting in a series of complications.8,9 Currently, most studies on UU infection focus on the epidemiological characteristics of the childbearing age group, adverse perinatal outcomes, and the development of UU infection and neonatal diseases,9–13 while fewer studies have been conducted on the epidemiological investigations of neonatal infections especially co-infections of pathogens. In this study, we collected data on UU-DNA test results of 7257 hospitalized neonates from the Maternal and Child Health Hospital of Hubei Province as well as clinical data to analyze the epidemiological and clinical characteristics of neonates infected with UU. These data will be helpful for clinical improvement of screening and treatment of UU infection among pregnant women and neonates, and will provide data support for further studies of neonatal UU infections.
Materials and Methods
Patients
Neonates hospitalized in the neonatology department of the Maternal and Child Health Hospital of Hubei Province from July 2020 to June 2022 were included in this study, and according to the results of the UU-DNA tests after admission, the neonates were divided into UU-positive and UU-negative groups. Neonates in the UU-negative group were selected by a random sampling method and compared with those in the UU-positive group. (Cases of neonates with incomplete information and an unclear medical history were excluded.)
Sample Collection
The child was placed in a supine position, and a disposable sputum aspirator was used to slowly insert the sputum tube into the pharynx. The appropriate negative pressure was set, the tube was rotated to the left and right to collect sputum from the trachea, and the sterile sputum cup was sealed until examination.
Sample Detection
Samples were tested using a QuantStudioTM5 real-time fluorescence quantitative PCR instrument and the UU Nucleic Acid Detection Kit (PCR-fluorescent probe method), which was strictly operated according to the instruction manual of the kit and the standardized procedure for the detection of UU-DNA in the Laboratory of Maternal and Child Health Hospital of Hubei Province, which included four parts: reagent preparation, sample preparation, PCR amplification, and interpretation of the results.
Diagnostic Criteria for Other Pathogenic Infections
Hepatitis B surface antigen is positive for Hepatitis B virus (HBV) infection, Hepatitis C antigen is positive for Hepatitis C virus (HCV) infection, herpesvirus hominis (HSV) and respiratory syncytial virus (RSV) infection are indicated by positive serum IgM tests, cytomegalovirus (CMV) is positive for urine CMV-DNA test or positive for serum IgM test, chlamydia trachomatis (CT) infection is positive for respiratory secretion CT-DNA test; Spirochetes syphilis infection is positive for serum TRUST test; And bacterial and fungal infections such as Escherichia coli, Candida albicans, Klebsiella pneumoniae, Staphylococcus aureus, Saccharomyces cerevisiae, Candida glabrata, Streptococcus anisopliae, Acinetobacter junii, Proteus mirabilis, Streptococcus gallolyticus and Enteroaerogen infection are indicated when the pathogens are found in the blood secretion cultures.
Diagnostic Criteria for UU Infection-Related Complications
The diagnostic criteria for respiratory distress syndrome, respiratory failure, pneumonia, bronchopulmonary dysplasia, necrotizing enterocolitis, retinopathy of prematurity, and meningitis in newborns were based on the clinical diagnostic criteria of the “Practical Neonatology (4th edition)”.
Statistical Methods
The epidemiological characteristics of UU-positive neonates were analyzed by GraphPad Prism, and the related statistics were analyzed by SPSS 25. Count data were expressed as cases (rate), and the χ2 test was used for comparison between groups; measures with normal distribution were expressed as x±s, and the independent samples t-test was used for comparison between groups; measures without a normal distribution were expressed as the median and interquartile range, and the nonparametric test was used for comparison between groups. P<0.05 indicated a statistically significant difference.
Results
Epidemiological Characteristics of UU-Infected Neonates
Among the 7257 hospitalized neonates, a total of 561 neonates were determined to have UU infection, with a detection rate of 7.73%. Of the 561 UU-positive neonates, 309 were male, with a positivity rate of 7.30%, and 252 were female, with a positivity rate of 8.35%, this showed that the positivity rate among the female neonates was higher than that among the male neonates, but the difference was not statistically significant (P=0.097); Neonates were divided into four age groups (1–7 days, 8–14 days, 15–21 days, and 22–28 days), and the UU detection rates in each age group were 8.00%, 5.53%, 6.07%, and 4.89%, respectively. As shown in Table 1 and Figure 1, the detection rate among the neonates in the group aged 1–7 days was significantly higher than that of the other three age groups, and the detection rate of the neonates in the group aged 22–28 days was the lowest, but the overall difference was not statistically significant (P=0.094), The trend of the detection rate among neonates of different sexes was consistent. We also analyzed the difference in the detection rates of any two age groups, and we observed that none of the differences were statistically significant (P>0.05), and the results are shown in Supplementary Table 1. By analyzing the detection rate in different seasons, we found that there was almost no difference in the detection rate in the spring and the fall, which was higher than that in the summer and the winter, with the detection rates of 8.43% and 8.44%, while the detection rate in winter was significantly lower than in the other three seasons, with a detection rate of 6.36%, and the trend of the detection rate among neonates of different sexes was the same. The specific results are shown in Table 1 and Figure 2. By analyzing the difference in the detection rate of any two seasons, we found that the difference between spring and winter, and between fall and winter was statistically significant (P= 0.020, 0.017), and the results are shown in Supplementary Table 2. Finally, we also analyzed the changes in the detection rate in different months, and the overall detection rate showed fluctuations, with the peaks occurring in March, June, October, and November, with a detection rates of 9.64%, 9.57%, 9.23%, and 8.80%, respectively. The lowest detection rate was observed in December, which was 5.41%, except for August, when the detection rate of female neonates was high and male neonates was low, the other months showed the same trend of change in neonates of different genders, and the change in the detection rate by month was consistent with the seasonal distribution of the detection rate described in the previous section. The specific change in the trend is shown in Figure 3.
 |
Table 1 Basic Detection Rate of Neonates with Ureaplasma urealyticum Infection |
 |
Figure 1 The distribution of Ureaplasma urealyticum positive rate among neonates in different ages. |
 |
Figure 2 The distribution of Ureaplasma urealyticum positive rate among neonates in different seasons. |
 |
Figure 3 The distribution of Ureaplasma urealyticum positive rate among neonates in different months. |
Basic Clinical Characteristics of UU-Positive and UU-Negative Neonates
According to the random sampling method, 496 neonates were selected from 6696 UU-negative neonates, and their clinical data were collected to analyze the significant differences between UU-positive and UU-negative neonates. The results showed the sex difference between the two groups was not statistically significant (P>0.05). The average gestational age of the neonates in the UU-positive group and the UU-negative group was 34.9 and 36.6 weeks, and the average birth weight was 2426 and 2701.5 g. The results showed that neonates in the UU-positive group were more likely than those in the UU-negative group to be preterm and have lower birth weights, and the differences were all statistically significant. Comparison of the mode of birth and the rate of preterm rupture of membranes between the two groups showed that the proportion of vaginal delivery was higher in the UU-positive group (67.2%), and the rate of preterm rupture of membranes was higher as well (45.8%), with the difference being statistically significant. Then we further analyzed the co-infections with other pathogens and complications related to UU infections between the two groups. The results showed that 47 neonates (8.4%) in the UU-positive group had at least one pathogen infection, compared with 22 neonates (4.4%) in the UU-negative group, which suggests that neonates with UU infections may be more likely to be infected with other pathogens. The incidence of respiratory complications in the two groups was high, compared with neonates in the UU-negative group, neonates in the UU-positive group had a higher incidence of neonatal respiratory failure, neonatal respiratory distress syndrome, neonatal bronchopulmonary dysplasia, retinopathy of prematurity, and neonatal meningitis, and the difference was statistically significant, while the incidence of neonatal pneumonia and necrotizing enterocolitis of the newborn were higher in the UU-positive group, but the difference was not statistically significant. All results are shown in Table 2.
 |
Table 2 Basic Clinical Characteristics of UU-Positive and UU-Negative Neonates |
Gestational Age and Birth Weight Characteristics of Neonates with UU Infection
Previous results have shown that neonates in the UU-positive group had a younger gestational age and lower birth weight than those in the UU-negative group. We further analyzed the gestational age and birth weight of UU-positive neonates, and classified them into preterm infants (<37 weeks), normal gestational age infants (37–42 weeks), and postterm infants (≥42 weeks) according to their gestational age, and analyzed the detection rate among male infants, female infants, and all infants. The results showed that preterm infants accounted for the highest proportion of all UU-positive infants in the groups, at 56.96%, 60.71% and 58.64%, respectively. According to the birth weight of the infants, they were categorized into ultralow-birth-weight (<1000 g), very-low-birth-weight (1000 ≤ 1500 g), low-birth-weight (1500 ≤ 1500 g < 2500 g), normal-birth-weight (2500 ≤ 4000 g), and large-sized infants (>4000 g). The results showed that there were 301 neonates with a birth weight <2500g, accounting for 53.65% of all UU-positive neonates, and the results are shown in Table 3. This further indicated that neonates with UU infection were more likely to be born preterm and have a low birth weight.
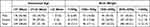 |
Table 3 Gestational Age and Weight Characteristics of Neonates with Ureaplasma urealyticum Infection |
Pathogen Co-Infections in Neonates with UU Infection
The results in Table 2 show that the incidence of pathogen co-infections was higher among neonates in the UU-positive group than in the UU-negative group, and we further tabulated the types and numbers of pathogen infections in neonates in the UU-positive group. Of the 561 UU-positive neonates, 47 neonates were co-infected with at least one pathogen infection. There were a total of 18 types of pathogen co-infections, of which there were 8 types of bacteria, with Escherichia coli accounting for the highest number of 12 cases, 3 types of fungi, with Candida albicans accounting for the highest number of infections of 4 cases, types of viruses, with respiratory syncytial virus accounting for the highest number of infections, followed by cytomegalovirus and human herpesvirus type 1 (7, 4, and 4 cases, respectively). The other pathogenic infections included Chlamydia trachomatis with 3 cases and spirochetes of syphilis with 2 cases. Most of these pathogen infections were UU infection combined with one other pathogen infection, but there were also cases of combined two and three combined pathogen infections, and there were six infants with two pathogen infections. One neonate had a combination of infections with three pathogens, and the concrete statistics are shown in Table 4.
 |
Table 4 Analysis of Ureaplasma urealyticum-Infected Neonates with Other Pathogens |
Discussion
Mycoplasma is a class of microorganisms between bacteria and viruses, with a size of 0.2–0.3 μm, and is a prokaryotic microorganism without a cell wall, that can infect the human respiratory system, genitourinary system and so on.14–16 It has been reported that there are more than ten types of Mycoplasma that infect the human genitourinary tract, which are classified as Mycoplasma hominis (Mh), Mycoplasma urealyticum (also known as Ureaplasma urealyticum (UU)), and Mycoplasma genitalium (Mg).17 UU is a colonizing organism of the genitourinary tract, that belongs to the category of conditionally pathogenic bacteria, and it is one of the main pathogens causing sexually transmitted diseases.18,19 Epidemiological studies of UU have shown that the detection rate of UU is relatively high among people of childbearing age, especially among the pregnant women.3,20 In addition to infecting adults, UU can also infect newborns through vertical transmission from mother to child.21 In this retrospective study, we analyzed the overall detection rate of UU among hospitalized UU-positive neonates, including the sex, age, and time distribution. Our results showed that the detection rate of UU among hospitalized neonates was 7.73%, which was higher among female infants, higher in spring and fall and their corresponding months, and highest from 1–7 days of life. Unlike previous studies, the lower detection rate of UU infection among the hospitalized neonates in our study may be because our study did not have any gestational age or birth weight limitations, and the detection rate of UU was also higher among preterm infants and infants with low birth weights. For example, one study have reported a 28–33% respiratory UU fixation rate in neonates with birth weights <1501 g.22 Ozdemir et al also found that the detection rate of UU infection among the respiratory tracts of neonates weighing <1250 g was 33.0% within 3 days,23 and Sung et al investigated the detection rate of UU among neonates of different gestational ages. The results showed that the UU positivity rate among preterm infants with a gestational age <26 weeks within 1 month of birth was as high as 65%, whereas among those with a gestational age >26 weeks, the positivity rate was only 31%.24 Moreover, we investigated the detection rate of UU infection among hospitalized neonates in 2016–2020, which was higher than that in 2020–2022, probably because of the gradual emphasis on screening and treatment of maternal UU infection in recent years. A large number of studies on adverse maternal outcomes caused by perinatal UU infection suggest that UU infections are closely associated with preterm delivery and low birth weight, and that the inflammatory response is considered to be the main mechanism of UU occurrence.25–27 Reproductive UU fixation can cause the pregnant mother organism to produce a series of inflammatory mediators, mainly including IL-1β, IL-8, TNF-α and TNF-β, which can affect the normal development and maturation of the fetus to the point of preterm delivery.25,28,29 Our results showed that the gestational age of the infants in the UU-positive group was on average approximately 2 weeks lower than that of infants in the UU-negative group, and that the highest percentage of preterm births was in the UU-positive group (58.64%), that the average birth weight of neonates in the UU-positive group was approximately 250 g lower than that of neonates in the UU-negative group, and that 53.65% of the UU-positive neonates had a birth weight of less than 2500 g, which is in line with the findings of Okogbule-Wonodi et al.30 A study by Gerber et al used PCR to detect UU in the amniotic fluid of 254 pregnant women at 15–17 weeks gestation and found that UU-positive pregnant women were more likely to have preterm labor than UU-negative pregnant women, and that the detection rate of UU was higher among preterm infants than term infants.31 The above results indicate that UU-infected fetuses are more likely to be born prematurely and have a lower birth weight. In addition, UU infection of neonates is affected by premature rupture of membranes and mode of delivery. In addition, our study showed a higher percentage of vaginal deliveries (67.2%) and a higher incidence of premature rupture of membranes among pregnant mothers (45.8%) in the UU-positive group compared to the UU-negative group. Fetal membranes are a natural barrier that protects the fetus, and infection by reproductive tract pathogens is the most common cause of premature rupture of membranes. Premature rupture of membranes causes the vaginal environment of the mother to become weakly alkaline, which creates a favorable environment for the survival of pathogens, that can infect the fetus through vertical transmission, and the risk of vertical transmission to the neonate is further increased by vaginal delivery.32
Furthermore, our results showed that neonates infected with UU will have an increased risk of infection with other pathogens, mainly infections caused by bacteria, viruses, fungi, chlamydia, and syphilitic spirochetes. Compared with the UU-negative group of neonates, the UU-positive group of neonates was infected with a greater types of species and number of other pathogens, of which the largest number of infections was caused by Escherichia coli, which accounted for 12 cases, and respiratory syncytial virus caused most of the viral infections. Neonates have immature immune systems and are physiologically immunocompromised, making them more susceptible to invasion by pathogens, and pathogenic infections are a major cause of neonatal morbidity and mortality.33,34 The types of pathogens vary in different countries and regions, but the prevalent strains are mainly Klebsiella pneumoniae, Escherichia coli, Staphylococcus aureus, respiratory syncytial virus, and Ureaplasma urealyticum, etc.35–37 Pathogen co-infection has more serious clinical manifestations and a poorer prognosis than the single-pathogen infections. Currently, there are few studies analyzing pathogen co-infections in UU-infected neonates, and our results indicate that early detection and treatment of UU infection is crucial for preventing neonatal infections and improving clinical outcomes.
UU infection in neonates mainly involves the respiratory system, causing neonatal pneumonia, respiratory distress syndrome, neonatal bronchopulmonary dysplasia (BPD), etc.38–40 It also has a certain effect on the digestive system and the nervous system. At present, the relationship between the occurrence of UU colonization in the body and neonatal BPD is a research hotspot, and most of the studies suggest that UU infection promotes the occurrence of BPD.22,41,42 In addition, UU infection also increases the incidence of retinopathy of prematurity, and meningitis in neonates, which is consistent with the results of our study.43 Some studies reported that UU infection increased the risk of necrotizing enterocolitis in newborns,30 but the Resch study suggested that there was no association between the two,44 and our findings were consistent with the latter conclusion. However, the specific association and mechanism still need to be further explored.
Conclusion
In conclusion, unlike previous studies on the influencing factors and clinical characteristics of neonatal UU infections, our study population was broader and not limited to preterm or low-birth-weight infants, and we statistically analyzed the status of UU infections and the clinical characteristics of hospitalized neonates in our hospital from 2020 to 2022. The detection rate of UU infection among hospitalized neonates was 7.73%, with females having a higher rate than males, the highest rate of detection was at 1–7 days of postnatal life, and the incidence of infection was high in spring and fall. In addition, the detection rate among preterm birth and low birth weight infants was significantly higher, which may indicate that UU infection is closely related to preterm birth and low birth weight. Analysis of combined pathogen infections showed that UU infection significantly increased the risk of other pathogen infections. Among them, Escherichia coli and respiratory syncytial virus were the most significant. Therefore, early screening and treatment of UU infection among women in the reproductive age group and in newborns is recommended to minimize pathogen infection, transmission and complications. However, we did not trace UU infections in mothers, which is a limitation of this study, and it is also a follow-up research direction.
Ethical Approval
In this study, we used existing data collected during the course of routine diagnostic procedures for infectious diseases of newborn and did not pose any additional risks to the patients. The patient records and information were anonymized and deidentified prior to analysis. And this study was conducted in accordance with the Declaration of Helsinki. In view of the above situation, the Ethics Committee of the Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology approved this study, and agreed to waive the right to individual informed consent from the study patients.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Waites KB, Crouse DT, Cassell GH. Systemic neonatal infection due to Ureaplasma urealyticum. Clin Infect Dis. 1993;17(Suppl 1):S131–S135. doi:10.1093/clinids/17.Supplement_1.S131
2. Plummer EL, Vodstrcil LA, Bodiyabadu K, et al. Are Mycoplasma hominis, Ureaplasma urealyticum and Ureaplasma parvum associated with specific genital symptoms and clinical signs in nonpregnant women? Clin Infect Dis. 2021;73(4):659–668. doi:10.1093/cid/ciab061
3. Leli C, Mencacci A, Latino MA, et al. Prevalence of cervical colonization by Ureaplasma parvum, Ureaplasma urealyticum, Mycoplasma hominis and Mycoplasma genitalium in childbearing age women by a commercially available multiplex real-time PCR: an Italian observational multicentre study. J Microbiol Immunol Infect. 2018;51(2):220–225. doi:10.1016/j.jmii.2017.05.004
4. Silwedel C, Speer CP, Glaser K. Ureaplasma-associated prenatal, perinatal, and neonatal morbidities. Expert Rev Clin Immunol. 2017;13(11):1073–1087. doi:10.1080/1744666X.2017.1381559
5. Yoon BH, Chang JW, Romero R. Isolation of Ureaplasma urealyticum from the amniotic cavity and adverse outcome in preterm labor. Obstet Gynecol. 1998;92(1):77–82. doi:10.1016/S0029-7844(98)00122-7
6. Rittenschober-Bohm J, Waldhoer T, Schulz SM, et al. Vaginal Ureaplasma parvum serovars and spontaneous preterm birth. Am J Obstet Gynecol. 2019;220(6):594 e591–594 e599. doi:10.1016/j.ajog.2019.01.237
7. Jeon J, Choi YS, Kim Y, et al. Maternal baseline risk factors for abnormal vaginal colonisation among high-risk pregnant women and the association with adverse pregnancy outcomes: a retrospective cohort study. J Clin Med. 2022;12(1):40. doi:10.3390/jcm12010040
8. Skevaki C, Kafetzis DA. Ureaplasma urealyticum airway colonization and pulmonary outcome in neonates. Expert Rev Anti Infect Ther. 2003;1(1):183–191. doi:10.1586/14787210.1.1.183
9. Olomu IN, Hecht JL, Onderdonk AO, Allred EN, Leviton A. Extremely Low Gestational Age Newborn Study I. Perinatal correlates of Ureaplasma urealyticum in placenta parenchyma of singleton pregnancies that end before 28 weeks of gestation. Pediatrics. 2009;123(5):1329–1336. doi:10.1542/peds.2008-1113
10. Xiao F, Qu Q, Zou M, et al. Detection of Ureaplasma urealyticum by catalytic hairpin assembly combined with a lateral flow immunoassay strip. ACS Omega. 2022;7(38):33830–33836. doi:10.1021/acsomega.2c02457
11. Pacifico L, Panero A, Roggini M, Rossi N, Bucci G, Chiesa C. Ureaplasma urealyticum and pulmonary outcome in a neonatal intensive care population. Pediatr Infect Dis J. 1997;16(6):579–586. doi:10.1097/00006454-199706000-00008
12. Aaltonen R, Vahlberg T, Lehtonen L, Alanen A. Ureaplasma urealyticum: no independent role in the pathogenesis of bronchopulmonary dysplasia. Acta Obstet Gynecol Scand. 2006;85(11):1354–1359. doi:10.1080/00016340600935987
13. Liu T, Lai SY, Zhou W, Liu YL, Chen SS, Jiang YM. Analysis of Ureaplasma urealyticum, Chlamydia trachomatis, Mycoplasma genitalium and Neisseria gonorrhoeae infections among obstetrics and gynecological outpatients in southwest China: a retrospective study. BMC Infect Dis. 2022;22(1):283. doi:10.1186/s12879-021-06966-z
14. Taglialegna A. Engineered Mycoplasma fight lung infections. Nat Rev Microbiol. 2023;21(4):218.
15. McCormack WM, Braun P, Lee YH, Klein JO, Kass EH. The genital mycoplasmas. N Engl J Med. 1973;288(2):78–89. doi:10.1056/NEJM197301112880206
16. Patel KK, Salva PS, Webley WC. Colonization of paediatric lower respiratory tract with genital Mycoplasma species. Respirology. 2011;16(7):1081–1087. doi:10.1111/j.1440-1843.2011.02016.x
17. Hjorth SV, Bjornelius E, Lidbrink P, et al. Sequence-based typing of Mycoplasma genitalium reveals sexual transmission. J Clin Microbiol. 2006;44(6):2078–2083. doi:10.1128/JCM.00003-06
18. Wang C, Wang J, Yan J, Chen F, Zhang Y, Hu X. Mycoplasma hominis, Ureaplasma parvum, and Ureaplasma urealyticum: hidden pathogens in peritoneal dialysis-associated peritonitis. Int J Infect Dis. 2023;131:13–15. doi:10.1016/j.ijid.2023.03.032
19. Pollack JD. Ureaplasma urealyticum: an opportunity for combinatorial genomics. Trends Microbiol. 2001;9(4):169–175. doi:10.1016/S0966-842X(01)01950-3
20. Tibaldi C, Cappello N, Latino MA, Masuelli G, Marini S, Benedetto C. Vaginal and endocervical microorganisms in symptomatic and asymptomatic non-pregnant females: risk factors and rates of occurrence. Clin Microbiol Infect. 2009;15(7):670–679. doi:10.1111/j.1469-0691.2009.02842.x
21. Peretz A, Tameri O, Azrad M, et al. Mycoplasma and Ureaplasma carriage in pregnant women: the prevalence of transmission from mother to newborn. BMC Pregnancy Childbirth. 2020;20(1):456. doi:10.1186/s12884-020-03147-9
22. Viscardi RM, Kallapur SG. Role of ureaplasma respiratory tract colonization in bronchopulmonary dysplasia pathogenesis: current concepts and update. Clin Perinatol. 2015;42(4):719–738. doi:10.1016/j.clp.2015.08.003
23. Ozdemir R, Sari FN, Tunay ZO, et al. The association between respiratory tract Ureaplasma urealyticum colonization and severe retinopathy of prematurity in preterm infants </=1250 g. Eye. 2012;26(7):992–996. doi:10.1038/eye.2012.77
24. Sung TJ, Xiao L, Duffy L, Waites KB, Chesko KL, Viscardi RM. Frequency of ureaplasma serovars in respiratory secretions of preterm infants at risk for bronchopulmonary dysplasia. Pediatr Infect Dis J. 2011;30(5):379–383. doi:10.1097/INF.0b013e318202ac3a
25. Li YH, Brauner A, Jonsson B, et al. Ureaplasma urealyticum-induced production of proinflammatory cytokines by macrophages. Pediatr Res. 2000;48(1):114–119. doi:10.1203/00006450-200007000-00020
26. Li J, Yin Y, Bendon R, et al. Necrotizing funisitis associated with Ureaplasma urealyticum infection: a clinicopathologic analysis of 14 cases. Placenta. 2022;126:12–16. doi:10.1016/j.placenta.2022.06.001
27. Jonduo ME, Vallely LM, Wand H, et al. Adverse pregnancy and birth outcomes associated with Mycoplasma hominis, Ureaplasma urealyticum and Ureaplasma parvum: a systematic review and meta-analysis. BMJ Open. 2022;12(8):e062990. doi:10.1136/bmjopen-2022-062990
28. Paira DA, Olivera C, Tissera AD, et al. Ureaplasma urealyticum and Mycoplasma hominis urogenital infections associate with semen inflammation and decreased sperm quality. J Leukoc Biol. 2023;113(1):18–26. doi:10.1093/jleuko/qiac006
29. Bender RA, Gundogdu C. Cytological diagnosis of genital ureaplasma urealyticum and its importance in cervical inflammation. Eur Rev Med Pharmacol Sci. 2022;26(21):7912–7917. doi:10.26355/eurrev_202211_30143
30. Okogbule-Wonodi AC, Gross GW, Sun CC, et al. Necrotizing enterocolitis is associated with ureaplasma colonization in preterm infants. Pediatr Res. 2011;69(5 Pt 1):442–447. doi:10.1203/PDR.0b013e3182111827
31. Gerber S, Vial Y, Hohlfeld P, Witkin SS. Detection of Ureaplasma urealyticum in second-trimester amniotic fluid by polymerase chain reaction correlates with subsequent preterm labor and delivery. J Infect Dis. 2003;187(3):518–521. doi:10.1086/368205
32. Sun T, Fu J. Analysis of the clinical features of intrauterine ureaplasma urealyticum infection in preterm infants: a case-control study. Front Pediatr. 2021;9:774150. doi:10.3389/fped.2021.774150
33. Ma B, McComb E, Gajer P, et al. Microbial biomarkers of intestinal barrier maturation in preterm infants. Front Microbiol. 2018;9:2755. doi:10.3389/fmicb.2018.02755
34. Chapman RL. Candida infections in the neonate. Curr Opin Pediatr. 2003;15(1):97–102. doi:10.1097/00008480-200302000-00016
35. Simonsen KA, Anderson-Berry AL, Delair SF, Davies HD. Early-onset neonatal sepsis. Clin Microbiol Rev. 2014;27(1):21–47. doi:10.1128/CMR.00031-13
36. Milton R, Gillespie D, Dyer C, et al. Neonatal sepsis and mortality in low-income and middle-income countries from a facility-based birth cohort: an international multisite prospective observational study. Lancet Glob Health. 2022;10(5):e661–e672. doi:10.1016/S2214-109X(22)00043-2
37. Stoll BJ, Puopolo KM, Hansen NI, et al. Early-onset neonatal sepsis 2015 to 2017, the rise of Escherichia coli, and the need for novel prevention strategies. JAMA Pediatr. 2020;174(7):e200593. doi:10.1001/jamapediatrics.2020.0593
38. Viscardi RM, Terrin ML, Magder LS, et al. Randomised trial of azithromycin to eradicate Ureaplasma in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2020;105(6):615–622. doi:10.1136/archdischild-2019-318122
39. Cultrera R, Seraceni S, Germani R, Contini C. Molecular evidence of Ureaplasma urealyticum and Ureaplasma parvum colonization in preterm infants during respiratory distress syndrome. BMC Infect Dis. 2006;6(1):166. doi:10.1186/1471-2334-6-166
40. Cassell GH, Waites KB, Crouse DT, et al. Association of Ureaplasma urealyticum infection of the lower respiratory tract with chronic lung disease and death in very-low-birth-weight infants. Lancet. 1988;2(8605):240–245. doi:10.1016/s0140-6736(88)92536-6
41. Ozdemir R, Erdeve O, Dizdar EA, et al. Clarithromycin in preventing bronchopulmonary dysplasia in Ureaplasma urealyticum-positive preterm infants. Pediatrics. 2011;128(6):e1496–e1501. doi:10.1542/peds.2011-1350
42. Payne MS, Goss KC, Connett GJ, Legg JP, Bruce KD, Chalker V. A quantitative analysis of Ureaplasma urealyticum and Ureaplasma parvum compared with host immune response in preterm neonates at risk of developing bronchopulmonary dysplasia. J Clin Microbiol. 2012;50(3):909–914. doi:10.1128/JCM.06625-11
43. Resch B, Gutmann C, Reiterer F, Luxner J, Urlesberger B. Neonatal Ureaplasma urealyticum colonization increases pulmonary and cerebral morbidity despite treatment with macrolide antibiotics. Infection. 2016;44(3):323–327. doi:10.1007/s15010-015-0858-7
44. Kurath-Koller S, Neumann C, Moissl-Eichinger C, et al. Hospital regimens including probiotics guide the individual development of the gut microbiome of very low birth weight infants in the first two weeks of life. Nutrients. 2020;12(5):1256. doi:10.3390/nu12051256
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
