Back to Journals » Nature and Science of Sleep » Volume 14
Emotional and Environmental Factors Aggravating Dream Enactment Behaviors in Patients with Isolated REM Sleep Behavior Disorder
Authors Jun JS, Sunwoo JS, Byun JI, Shin JW , Kim TJ, Schenck CH, Jung KY
Received 29 April 2022
Accepted for publication 14 September 2022
Published 24 September 2022 Volume 2022:14 Pages 1713—1720
DOI https://doi.org/10.2147/NSS.S372823
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sarah L Appleton
Jin-Sun Jun1 *, Jun-Sang Sunwoo2 *, Jung-Ick Byun,3 Jung-Won Shin,4 Tae-Joon Kim,5 Carlos H Schenck,6 Ki-Young Jung7
1Department of Neurology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Republic of Korea; 2Department of Neurology, Kangbuk Samsung Hospital, Seoul, Republic of Korea; 3Department of Neurology, Kyung Hee University Hospital at Gangdong, Seoul, Republic of Korea; 4Department of Neurology, CHA Bundang Medical Center, CHA University, Seongnam, Republic of Korea; 5Department of Neurology, Ajou University School of Medicine, Suwon, Republic of Korea; 6Minnesota Regional Sleep Disorders Center, and Department of Psychiatry, Hennepin County Medical Center and University of Minnesota Medical School, Minneapolis, MN, USA; 7Department of Neurology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea
*These authors contributed equally to this work
Correspondence: Ki-Young Jung, Department of Neurology, Seoul National University Hospital, Neuroscience Research Institute, Seoul National University College of Medicine, 101 Daehak-ro, Jongno-gu, Seoul, 03080, Korea, Tel +82-2-2072-4988, Fax +82-2-3672-7553, Email [email protected]
Objective: To identify emotional and environmental factors that aggravate dream enactment behaviors (DEBs) in isolated rapid eye movement (REM) sleep behavior disorder (iRBD).
Methods: In this cross-sectional study, a total of 96 polysomnography-confirmed iRBD patients (mean age, 68.5 years; men, 68%) and their caregivers completed questionnaires regarding potential aggravating factors related to DEBs, including emotion/feelings (stress, anger, anxiety, depressive mood, fatigue, pain), food (alcohol, caffeine, overeating in the evening, fasting/hunger), activities and sleep patterns (strenuous exercise, sex before bed, conflict/fighting, sleep deprivation, oversleeping, sleeping away from home, watching TV before bed), weather/environmental factors (cloudy or rainy weather, heat, cold, noise) and medication (skipping medication, taking hypnotics).
Results: The patients reported that stress (61%) was the most aggravating factor for DEBs, followed by anxiety (56%), anger (51%), fatigue (49%), and watching TV before bed (46%). Similarly, the caregivers reported that these factors were most relevant to the aggravation of DEBs in the patients, although some factors were ranked differently. In the subgroup analyses, aggravating factors for DEBs did not differ by RBD symptom severity. Interestingly, the proportion of patients experiencing DEB aggravation by stress, anxiety and depressive mood was significantly higher in women than in men. Furthermore, depressed patients reported that stress and cloudy or rainy weather made DEBs worse than nondepressed patients.
Conclusion: Our results suggest that DEBs in iRBD patients may be mainly aggravated by emotional factors. These negative effects appeared to be more prominent in female and depressed patients.
Keywords: REM sleep behavior disorder, dream enactment behavior, precipitating factors
Introduction
Rapid eye movement (REM) sleep behavior disorder (RBD) is a parasomnia characterized by dream enactment behaviors (DEBs) due to a loss of muscle atonia during REM sleep.1 A growing body of evidence suggests that patients with isolated RBD (iRBD) eventually develop a neurodegenerative disease, including Parkinson’s disease (PD), dementia with Lewy bodies, and, less frequently, multiple system atrophy, with a conversion risk of over 80% in a decade or more.2
DEBs in patients with RBD range from simple motions such as limb jerking and sleep talking to complex and violent movements such as punching and kicking.3,4 Previous studies have shown that DEBs can result in sleep disruption and life-threatening injuries for both patients and their bed partners.5 Accordingly, appropriate treatment should be considered depending on the symptoms in patients with RBD. The current treatment guidelines for DEBs in RBD include pharmacological agents, mainly clonazepam and melatonin.6,7 However, definitive conclusions cannot be drawn from recent randomized controlled trials, in which both drugs failed to show effectiveness in patients with iRBD and PD patients with RBD.8–10
Bedroom environmental modifications are also recommended to prevent injurious behaviors for all patients with RBD. Recommended measures include removing dangerous objects from the bedroom, placing a mattress on the floor, and sleeping in separate bedrooms. However, these recommendations focus only on modifying the bedroom environment. In our experience, some patients with RBD complained of aggravation of DEBs after emotional stress or alcohol consumption. Furthermore, it has been reported that the worsening of DEBs was related to traumatic stress following a disturbing event1,11,12 or chocolate ingestion.13 These observations suggest that it is necessary for patients with RBD to avoid DEB precipitating factors, but there have been no studies to comprehensively explore such factors. Therefore, in this study, we aimed to identify the emotional and environmental factors that potentially aggravate DEBs in iRBD patients.
Methods
Study Design and Participants
We prospectively recruited consecutive patients with iRBD from the Department of Neurology at Seoul National University Hospital between 1 March 2020 and 31 August 2021. All participants underwent overnight video-polysomnography (PSG), and a diagnosis of RBD was confirmed based on the third edition of the International Classification of Sleep Disorders.14 The participants were excluded if they had any sign suggestive of neurodegenerative disease, such as parkinsonism and dementia, confirmed by a neurologist. This study was approved by the Review Board of the Seoul National University Hospital and written informed consent for research was obtained from all individuals who participated in the study (IRB No. 2007-189-1144). The study followed the principles of the Declaration of Helsinki.
Variables
Twenty-three potential precipitating factors related to DEBs were selected by seven RBD experts based on their clinical experience, including emotion/feelings (stress, anger, anxiety, depressive mood, fatigue, pain), food (alcohol, caffeine, overeating in the evening, fasting/hunger), activities and sleep patterns (strenuous exercise, sex before bed, conflict/fighting, sleep deprivation, oversleeping, sleeping away from home, watching TV before bed), weather/environmental factors (cloudy or rainy weather, heat, cold, noise) and medication (skipping medication, taking hypnotics). Patients and their caregivers were independently asked to respond either “yes” or “no” to the questions about whether the above factors aggravated DEBs in the past.
In addition, the clinical severity of RBD was assessed using the Korean version of the RBD Questionnaire-Hong Kong (RBDQ-KR).15,16 Depression was assessed using the Korean version of the Geriatric Depression Scale (GDS-K),17 and the cutoff value for the presence of depression was defined as ≥18. Cognitive function was assessed using the Korean version of the Montreal Cognitive Assessment (MoCA-K).18
Statistical Analysis
All data are presented as the mean±standard deviation. Data distribution and normality were assessed using the Shapiro–Wilk test. Demographic and clinical characteristics were compared using the chi-square test for categorical variables and Student’s t-test or the Mann–Whitney U-test for continuous variables, as appropriate. We investigated the relationship between aggravation of DEBs by emotional and environmental factors and clinical variables, including age, RBD duration, and scores on the RBDQ-KR, GDS-K, and MoCA-K using point-biserial correlations for binary outcomes (aggravation yes/no). Furthermore, subgroup analyses were performed using the chi-square test or Fisher’s exact test to explore whether the association between DEB aggravation and emotional and environmental factors differs by sex, RBD symptom severity, the presence of depression, or severity of obstructive sleep apnea (OSA). Because this is an exploratory study, no adjustments were made to control type I error. All P values were two-sided, and a P value of less than 0.05 was considered statistically significant. Calculations were performed with SPSS (IBM) version 27.
Results
A total of 96 iRBD patients and 84 caregivers were included in this study. The demographic and clinical characteristics of all patients are shown in Table 1. The mean age of the iRBD patients was 68.5±6.7 years, and 65 (67.7%) were men. The patients had a mean RBD symptom duration of 7.0±5.4 years. The male group had a higher education level than the female group (P=0.006). The scores on the GDS-K, MoCA-K and RBDQ-KR did not significantly differ between men and women. All patients were receiving clonazepam and/or melatonin for RBD at the time of the study.
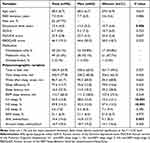 |
Table 1 Demographic and Clinical Characteristics |
The results for potential DEB aggravating factors are shown in Figure 1. Fifty-five patients (61%) and 56 (67%) caregivers answered that stress was the primary factor that aggravated DEBs. The other top 5 precipitating factors for DEBs were anxiety (56%), anger (51%), fatigue (49%) and watching TV before going to bed (46%) (Figure 1A). According to caregivers, the top 5 precipitating factors for DEBs were fatigue (62%), watching TV before going to bed (57%), anxiety (56%), and anger (50%), which was roughly similar to the responses according to the patients (Figure 1B). The results for potential DEB aggravating factors were not significantly different between the patients and their caregivers (Supplementary Table 1). Next, we examined which clinical parameters were associated with the top 5 precipitating factors for DEBs, and these results are summarized in Supplementary Table 2. We found that the aggravation of DEBs by stress was correlated with higher GDS-K scores (r=0.230, P=0.024), whereas there were no significant correlations with the other clinical variables.
 |
Figure 1 Dream enactment behavior aggravating factors, colored by category, according to isolated REM sleep behavior disorder patients (A) and their caregivers (B). |
In the subgroup analyses, the female group had a higher proportion of DEB aggravation by stress (P=0.026), anxiety (P=0.045), and depressive mood (P=0.022) than the male group (Table 2). The proportion of DEB aggravation by alcohol was significantly higher in men than in women (P=0.002). A comparison between depressed and nondepressed patients, depressed patients reported that stress (P=0.026) and cloudy or rainy weather (P=0.05) made DEBs worse than nondepressed patients (Table 3). Aggravating factors did not differ by RBD symptom severity or OSA severity (Supplementary Tables 3 and 4).
 |
Table 2 Comparison of Precipitating Factors on Dream Enactment Behaviors Between Men and Women |
 |
Table 3 Comparison of Precipitating Factors on Dream Enactment Behaviors Between Depressed and Nondepressed Groups |
Discussion
In this study, we investigated which emotional and environmental factors aggravate DEBs in iRBD patients. Our results showed that iRBD patients reported that emotional factors such as stress, anxiety, and anger were the factors that aggravated DEBs most frequently, which is roughly consistent with the results reported by their caregivers. In the subgroup analyses, the proportion of patients experiencing DEB aggravation by stress, anxiety and depressive mood was significantly higher in women than in men. Furthermore, depressed patients reported that stress and cloudy or rainy weather made DEBs worse than nondepressed patients. To the best of our knowledge, this is the first study to systematically investigate precipitating factors for DEBs in iRBD patients.
Previous studies found that post-traumatic stress disease (PTSD) is related to DEBs in patients with RBD as well as those with non-REM parasomnias,11,12 which is in line with our findings. While the precise mechanism of RBD in patients with PTSD remains largely unknown, it is suggested that the increased turnover of noradrenaline by PTSD results in its depletion in the peri-locus coeruleus, which causes dysfunction in the regulation of REM sleep atonia.19 Furthermore, there is also evidence showing that psychological stress itself, regardless of PTSD, provokes disturbances of noradrenergic function in various brain regions.20 Given the potential role of noradrenaline in the occurrence of RBD,21 one can postulate that noradrenergic pathway alterations due to emotional stress contribute to the aggravation of DEBs in iRBD patients. Although stress has also been reported to increase serotonin turnover in the brain,22 it remains debatable whether the serotonergic system is directly involved in RBD pathogenesis.21,23 Alternatively, a recent animal study revealed that chronic stress provokes enhanced REM sleep,24 which may partially explain our findings.
On the other hand, stressful events can result in highly traumatic or violent dreams.25,26 Considering the fact that verbal or motor components of dreaming are enacted behaviorally in iRBD patients,1 changes in dream contents by stressful events may not only increase the occurrence of DEBs per se but also provoke more aggressive DEBs. In support of this hypothesis, a recent study showed that aggressiveness was more frequent in dreams related to DEBs in iRBD patients, although the frequency of aggressive dream contents did not differ between the patients and healthy controls.27
Our results showed that the proportion of patients experiencing DEB aggravation by emotional factors was significantly higher in females than males, indicating sex-specific effects of precipitating factors for DEBs in iRBD patients. In general, females tend to have a higher prevalence and greater severity of mental disorders, including PTSD, panic disorder, and major depressive disorder.28 Accordingly, it is plausible that the absolute proportion of patients experiencing emotional factors is higher in females, which may contribute to disparities between the sexes in factors aggravating DEBs. However, this possibility cannot be explained by our finding that there was no significant difference in depressive symptoms between men and women. On the other hand, sex differences in responses to the stress neuropeptide, which is a corticotropin-releasing factor, are thought to increase female vulnerability to stress in mental disorders.29 In this context, increased stress sensitivity in females may be linked to sex differences in the emotional factors aggravating DEBs in iRBD patients.
Similarly, the impact of stress on DEB aggravation was more prominent in depressed patients than in nondepressed patients, which may be associated with emotion dysregulation.30 Emotion regulation is a complex process that involves adjusting emotional responses to cope with difficult situations, and its impairment is regarded as a potential mechanism in the development of depression.31 Accordingly, we speculate that depressed patients have more severe emotion dysregulation, increasing vulnerability to stress.
In addition to emotional factors, “watching TV before bed” was one of the major factors aggravating DEBs in iRBD patients. It is well known that watching TV at night is associated with sleep problems, mainly due to exposure to bright light.32 However, considering the current finding of a potential association between emotional factors and DEBs, TV content may be more important than the act of watching TV itself in determining the extent of aggravation by watching TV. One patient had repetitively experienced DEBs more frequently and violently when he watched action movies or martial sports before going to bed. Unfortunately, our study did not include an analysis of the contents or duration of watching TV before bed, which needs to be performed in future studies.
A recent review suggests that patients with RBD should avoid alcohol consumption, as this factor can aggravate RBD-related symptoms.33 Based on our experience, we also hypothesized that alcohol intake would be associated with the worsening of DEBs in iRBD patients. However, only approximately one-quarter of our patients answered that alcohol intake aggravated DEBs, and alcohol intake was ranked 12th among 23 potential precipitating factors. This weak relationship may be due to the low frequency of alcohol consumption in this study sample. In the current study, the proportion of patients who consumed alcohol more than 2 times per week was just less than 10%. Consistent with this assumption, our results showed that the negative impact of alcohol intake on DEBs seemed prominent only in men, and not surprisingly, men (68%) were more likely to drink alcohol than women (10%).
The present study has several limitations. First, the assessment of DEBs or its aggravating factors was based on self-report and therefore may have the risk of introducing recall bias. However, given the night-to-night variability in DEBs, patient-reported outcome measures may be more reliable than objective outcome measures using PSG. Moreover, to minimize bias, we also included each caregiver’s assessment, and the results were similar to those of patients. Second, because this study focused on the frequency of DEBs as an outcome measure, it still remains unclear whether exposure to emotional and environmental factors affect the severity of DEBs. Third, the sample size in subgroup analyses was modest in some cases, which may hamper the detection of significant associations. Additionally, our sample size was limited to the power to determine differences according to sex or the presence of depression in precipitating factors for DEBs. Fourth, the proportion of patients consuming alcohol in our dataset was relatively small. Furthermore, we did not obtain data on the quantity of alcohol consumption. For these reasons, a reliable conclusion about the association between alcohol intake and DEBs cannot be drawn from our results. Further studies with a larger sample size of regular alcohol-drinkers and detailed information on alcohol consumption, such as the frequency and intensity of alcohol consumption and the type of alcohol consumed, should be considered to clarify this issue. Fifth, although dream content changes may be one of the plausible mechanisms by which emotional factors were associated with DEB aggravation in our findings, we could not perform a dream content analysis due to lack of data. Last, the cross-sectional design of the current study prevented us from drawing conclusions about causality.
In summary, our results suggest that DEBs in iRBD patients may be mainly aggravated by emotional factors such as stress, anxiety, and anger. These effects were more prominent in females and depressed patients. Our results may emphasize the potential importance of emotional control as well as lifestyle modification to manage DEBs in iRBD patients. However, because this study design has potential biases from self-reported subjective data, further studies using objective measures of emotional factors and DEBs should be performed to clarify this issue.
Funding
This study was supported by a research grant of National Research Foundation funded by the Ministry of Science and ICT (MSIT) in Korea (NRF-2020R1C1C1013382), the Brain Research Program through the National Research Foundation of Korea funded by the Ministry of Science, ICT & Future Planning (2017M3C7A1029688) and the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIP) (2017R1A2B2012280).
Disclosure
Dr Carlos H Schenck reports personal fees from Eisai, Inc., outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Schenck CH, Mahowald MW. REM sleep behavior disorder: clinical, developmental, and neuroscience perspectives 16 years after its formal identification in SLEEP. Sleep. 2002;25(2):120–138. doi:10.1093/sleep/25.2.120
2. Cesari M, Heidbreder A, St Louis EK, et al. Video-polysomnography procedures for diagnosis of rapid eye movement sleep behavior disorder (RBD) and the identification of its prodromal stages: guidelines from the International RBD Study Group. Sleep. 2022;45(3):zsab257. doi:10.1093/sleep/zsab257
3. Iranzo A, Santamaria J, Tolosa E. Idiopathic rapid eye movement sleep behaviour disorder: diagnosis, management, and the need for neuroprotective interventions. Lancet Neurol. 2016;15(4):405–419. doi:10.1016/S1474-4422(16)00057-0
4. Olson EJ, Boeve BF, Silber MH. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain. 2000;123(Pt 2):331–339. doi:10.1093/brain/123.2.331
5. McCarter SJ, St Louis EK, Boswell CL, et al. Factors associated with injury in REM sleep behavior disorder. Sleep Med. 2014;15(11):1332–1338. doi:10.1016/j.sleep.2014.06.002
6. Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med. 2010;6(1):85–95. doi:10.5664/jcsm.27717
7. Gilat M, Marshall NS, Testelmans D, Buyse B, Lewis SJG. A critical review of the pharmacological treatment of REM sleep behavior disorder in adults: time for more and larger randomized placebo-controlled trials. J Neurol. 2022;269(1):125–148. doi:10.1007/s00415-020-10353-0
8. Shin C, Park H, Lee WW, Kim HJ, Kim HJ, Jeon B. Clonazepam for probable REM sleep behavior disorder in Parkinson’s disease: a randomized placebo-controlled trial. J Neurol Sci. 2019;401:81–86. doi:10.1016/j.jns.2019.04.029
9. Jun JS, Kim R, Byun JI, et al. Prolonged-release melatonin in patients with idiopathic REM sleep behavior disorder. Ann Clin Transl Neurol. 2019;6(4):716–722. doi:10.1002/acn3.753
10. Gilat M, Coeytaux jackson A, Marshall NS, et al. Melatonin for rapid eye movement sleep behavior disorder in Parkinson’s disease: a randomised controlled trial. Mov Disord. 2020;35(2):344–349. doi:10.1002/mds.27886
11. Jones MB, Jeevan S, Wang J, et al. Clinical correlates of dream enactment behaviors in previously deployed OEF/OIF/OND Veterans: an exploratory analysis. J Neuropsychiatry Clin Neurosci. 2020;32(2):147–153. doi:10.1176/appi.neuropsych.19010009
12. Elliott JE, Opel RA, Pleshakov D, et al. Posttraumatic stress disorder increases the odds of REM sleep behavior disorder and other parasomnias in Veterans with and without comorbid traumatic brain injury. Sleep. 2020;43(3). doi:10.1093/sleep/zsz237
13. Vorona RD, Ware JC. Exacerbation of REM sleep behavior disorder by chocolate ingestion: a case report. Sleep Med. 2002;3(4):365–367. doi:10.1016/S1389-9457(02)00008-4
14. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–1394. doi:10.1378/chest.14-0970
15. Li SX, Wing YK, Lam SP, et al. Validation of a new REM sleep behavior disorder questionnaire (RBDQ-HK). Sleep Med. 2010;11(1):43–48. doi:10.1016/j.sleep.2009.06.008
16. You S, Moon HJ, Do SY, et al. The REM sleep behavior disorder screening questionnaire: validation study of the Korean version (RBDQ-KR). J Clin Sleep Med. 2017;13(12):1429–1433. doi:10.5664/jcsm.6840
17. Bae JN, Cho MJ. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J Psychosom Res. 2004;57(3):297–305. doi:10.1016/j.jpsychores.2004.01.004
18. Lee JY, Dong Woo L, Cho SJ, et al. Brief screening for mild cognitive impairment in elderly outpatient clinic: validation of the Korean version of the Montreal Cognitive Assessment. J Geriatr Psychiatry Neurol. 2008;21(2):104–110. doi:10.1177/0891988708316855
19. Husain AM, Miller PP, Carwile ST. Rem sleep behavior disorder: potential relationship to post-traumatic stress disorder. J Clin Neurophysiol. 2001;18(2):148–157. doi:10.1097/00004691-200103000-00005
20. Pacák K, Palkovits M. Stressor specificity of central neuroendocrine responses: implications for stress-related disorders. Endocr Rev. 2001;22(4):502–548. doi:10.1210/edrv.22.4.0436
21. Jiménez-Jiménez FJ, Alonso-Navarro H, García-Martín E, Agúndez JAG. Neurochemical features of rem sleep behaviour disorder. J Pers Med. 2021;11(9):880. doi:10.3390/jpm11090880
22. Chaouloff F, Berton O, Mormède P. Serotonin and stress. Neuropsychopharmacology. 1999;21(2 Suppl):28s–32s. doi:10.1016/S0893-133X(99)00008-1
23. Arnaldi D, Fama F, De Carli F, et al. The role of the serotonergic system in REM sleep behavior disorder. Sleep. 2015;38(9):1505–1509. doi:10.5665/sleep.5000
24. Nollet M, Hicks H, McCarthy AP, et al. REM sleep’s unique associations with corticosterone regulation, apoptotic pathways, and behavior in chronic stress in mice. Proc Natl Acad Sci U S A. 2019;116(7):2733–2742. doi:10.1073/pnas.1816456116
25. Pillar G, Malhotra A, Lavie P. Post-traumatic stress disorder and sleep—what a nightmare Sleep Med Rev. 2000;4(2):183–200. doi:10.1053/smrv.1999.0095
26. Nielsen T, Levin R. Nightmares: a new neurocognitive model. Sleep Med Rev. 2007;11(4):295–310. doi:10.1016/j.smrv.2007.03.004
27. Cavallotti S, Stein HC, Savarese M, Terzaghi M, D’Agostino A. Aggressiveness in the dreams of drug-naïve and clonazepam-treated patients with isolated REM sleep behavior disorder. Sleep Med. 2022;92:19–23. doi:10.1016/j.sleep.2022.02.022
28. Breslau N, Davis GC, Peterson EL, Schultz L. Psychiatric sequelae of posttraumatic stress disorder in women. Arch Gen Psychiatry. 1997;54(1):81–87. doi:10.1001/archpsyc.1997.01830130087016
29. Bangasser DA, Curtis A, Reyes BA, et al. Sex differences in corticotropin-releasing factor receptor signaling and trafficking: potential role in female vulnerability to stress-related psychopathology. Mol Psychiatry. 2010;15(9):896–904. doi:10.1038/mp.2010.66
30. Jun JS, Kim R, Jung HM, et al. Emotion dysregulation in idiopathic rapid eye movement sleep behavior disorder. Sleep. 2020;43(2):zsz224. doi:10.1093/sleep/zsz224
31. Gross JJ. Emotion regulation: current status and future prospects. Psychol Inq. 2015;26(1):1–26. doi:10.1080/1047840X.2014.940781
32. Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, Czeisler CA. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. J Clin Sleep Med. 2013;9(12):1291–1299. doi:10.5664/jcsm.3272
33. Dauvilliers Y, Schenck CH, Postuma RB, et al. REM sleep behaviour disorder. Nat Rev Dis Primers. 2018;4(1):19. doi:10.1038/s41572-018-0016-5
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
