Back to Journals » Drug Design, Development and Therapy » Volume 17
Efficacy of Super-Bioavailable Itraconazole and Conventional Itraconazole at Different Dosing Regimens in Glabrous Tinea Infection - A Randomized Clinical Trial
Authors Shenoy MM, De A, Shah B, Das A, Saraswat A , Lahiri K, Yadav S, Sarda A, Chakraborty D, J D , Kamat S, Doshi Y, Gonsalves N, Choudhary A, Dhoot D , Mahadkar N, Bhushan S, Gadkari R, Barkate H
Received 30 May 2023
Accepted for publication 28 August 2023
Published 21 September 2023 Volume 2023:17 Pages 2899—2908
DOI https://doi.org/10.2147/DDDT.S421583
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Manfred Ogris
Manjunath M Shenoy,1 Abhishek De,2 Bela Shah,3 Anupam Das,4 Abir Saraswat,5 Koushik Lahiri,2 Sheetal Yadav,6 Aarti Sarda,2 Disha Chakraborty,7 Dharmender J,2 Shruti Kamat,2 Yashika Doshi,2 Nelry Gonsalves,2 Ankita Choudhary,2 Dhiraj Dhoot,8 Namrata Mahadkar,8 Sumit Bhushan,8 Rujuta Gadkari,8 Hanmant Barkate8
1Department of Dermatology, Omega Hospital, Mangalore, Karnataka, India; 2Department of Dermatology, Wizderm Specialty Skin and Hair Clinic, Kolkata, West Bengal, India; 3Department of Dermatology, BJ Medical College and Civil Hospital, Ahmedabad, Gujarat, India; 4Department of Dermatology, Iris Multispecialty Hospital, Kolkata, West Bengal, India; 5Department of Dermatology, Indushree Skin Clinic, Lucknow, Uttar Pradesh, India; 6Department of Dermatology, ABVIMS and Dr. RML Hospital, New Delhi, India; 7Department of Dermatology, Calcutta National Medical College, Kolkata, West Bengal, India; 8Department of Global Medical Affairs, Glenmark Pharmaceuticals Ltd, Mumbai, Maharashtra, India
Correspondence: Dhiraj Dhoot, Glenmark Pharmaceuticals Ltd, B D Sawant Marg, Chakala, Andheri (E), Mumbai, India, 400099, Tel +91 9619811219, Email [email protected]
Introduction: Itraconazole follows non-linear pharmacokinetics and hence is recommended once daily, but in real-world practice, is commonly prescribed as twice daily. Hence, this study aimed to evaluate the efficacy and safety of super-bioavailable-itraconazole-130 mg (SB-130) and conventional-itraconazole-200 mg (CITZ-200) once daily compared with conventional-itraconazole-100 mg (CITZ-100) twice daily in glabrous tinea.
Methods: A total of 261 eligible patients were enrolled in this prospective, randomized, clinical study from December-2021 to August-2022 at seven centers in India. Efficacy and safety assessments were done at week-3 and 6, with follow-up at week-10 for relapse. The primary objective was to assess the proportion of patients who achieved complete cure at week-6 following treatment in all itraconazole groups. The secondary outcomes were safety and clinical and mycological cure rates.
Results: Of 261 patients, 240 were included in the analysis. At week-6, 140 patients were completely cured; thus, overall cure rate was 58.33%. Fifty-five patients (69%) in SB-130 while 47/77 (61%) and 38/83 (46%) patients were completely cured in CITZ-200 and CITZ-100 groups respectively (p< 0.05; SB-130: CITZ-100, p=0.32; SB-130: CITZ-200, p=0.058; CITZ-200: CITZ-100). There was no statistical difference in the mycological cure rate and area clearance rate between any of the groups (p=0.14); however, a statistically significant difference was noted for OD dosing over BD dosing in achieving clinical cure rates (p< 0.05). A total of 13/140 patients (9%) relapsed following complete cure, with no statistically significant difference between any of the groups (p=0.50). All treatments were safe and well-tolerated, with no discontinuation.
Conclusion: In this clinical study, moderate efficacy with all doses of ITZ was reported but was better with OD dosing. Although there was no statistical difference between SB-130 and CITZ-200, SB-130 may be preferred over CITZ-200 owing to the advantage of SB over the conventional ITZ.
Keywords: itraconazole, super-bioavailable itraconazole, 130mg, efficacy, safety, India, OD, dermatophytosis, relapse
Corrigendum for this paper has been published.
Introduction
Over the past few years, a steep surge in dermatophytosis or glabrous tinea1 has been reported by many folds, especially in India, along with an increase in chronic and recurrent presentation and relapse rates of dermatophytosis.2,3 Additionally, there is an immense discrepancy between the management of dermatophytosis in the current scenario and treatment guidelines given in standard dermatology text books.4–6
Although, systemic antifungals play important role in the management, an inadequate clinical response to fluconazole, griseofulvin and terbinafine has been reported.7,8 This has led to increased use of itraconazole (ITZ) as the first-line systemic antifungal.6 Moreover, it has been reported as one the most potent antifungals in a recent article.9 But, ITZ has multiple pharmacokinetic challenges like variations in bioavailability, and requirement of food for optimal absorption, which limit its use.10 Hence, a new formulation of ITZ, super-bioavailable ITZ (SB-ITZ), was approved by the Central Drug Standard Control Organization (CDSCO, central licensing authority) in the strength of 65 mg and 130 mg.11
With the availability of this new formulation, there is a dilemma regarding the frequency of ITZ administration of ITZ. Although ITZ is recommended to be prescribed once a day because of its non-linear pharmacokinetics,1,12 it is common practice to prescribe ITZ in divided doses, and many articles have documented this.13,14 This calls for a re-evaluation of ITZ, either conventional or SB-ITZ, in the management of glabrous tinea, in terms of its dosage, administration, and efficacy.
The objective of this clinical study was to compare the cure rates with relapse and safety profiles with three commonly prescribed dosing regimens of itraconazole (ITZ 100 mg BD, ITZ 200 mg OD [2 capsules of 100 mg], and SB-ITZ 130 mg OD) in the management of glabrous tinea, over a period of 6 weeks.
Methods
Setting
This open-label, prospective, three-arm clinical study (registered with the Clinical Trials Registry India, registration number (CTRI/2021/11/038275) was carried out across seven centers in India with prior approval of the ethics committee for the respective centers from December 2021 to August 2022 and in accordance with Good Clinical Practices and the Declaration of Helsinki 1996 (Supplement 1).
Sample Size
The desired sample size of 87 patients in each group was calculated considering 90% power to reject the null hypothesis of zero effect size, with a population effect size of 0.53,15 the significance level (alpha) was 0.05, using a two-sided z-test with a dropout rate of 15%.
Inclusion and Exclusion Criteria
Adult patients (≥ 18 years and ≤ 60 years) of either sex with glabrous tinea requiring systemic antifungal therapy, with no history of intake of any oral antifungal agent in the preceding four weeks or a topical antifungal/steroid in the preceding two weeks, were recruited. Additionally, patients with chronic dermatophytosis1 with a duration of ≥6 months and no use of antifungals for the last 4 weeks were recruited. Patients who were pregnant, lactating, or had any significant medical illnesses, such as metabolic diseases or immunocompromised conditions, that would have affected the clinical outcomes were excluded from the study. Patients taking concomitant medications that interact with itraconazole were also excluded. All female patients of childbearing age were advised to avoid pregnancy during the treatment.
Study Design
Two hundred and sixty-one patients fulfilling the selection criteria were randomized into three parallel treatment groups using a computer randomization method, with 87 patients in each group (allocation ratio 1:1:1). Written informed consent was obtained in Hindi, English, or a regional language, according to the patient’s choice. Diagnosis was made on clinical examination, and the patients’ demographics and baseline clinical characteristics, including duration of current illness, extent of lesion, and clinical signs and symptom scores, were recorded at the first visit. All diagnoses were confirmed by direct microscopy under 10% potassium hydroxide (KOH mount), which was repeated at the end of the treatment period (6 weeks). KOH mounts were made from all active clinical lesions and all fields within each smear were examined at 40 × magnification. No special stains were added for microscopic examination of the skin scrapings. Liver function tests (LFTs) were performed at baseline and at the end of the treatment. Scoring of the Dermatology Life Quality Index (DLQI)16 was performed at the same visit and at the end of treatment.
The study comprised two parts: the first part, the treatment period of six weeks, and the second part of an observation period of another four weeks, thus making the entire study duration of 10 weeks. During the treatment period, patients were followed-up according to the routine protocol, and clinical assessment data were collected on visits 2 (day 1), 3 (day 22±2), and 4 (day 43±2). Following this treatment period, patients with complete cure were not prescribed any antifungal medication, whereas the remaining patients were allowed to take antifungal medication at the discretion of the treating physician. All patients with a complete cure were contacted by telephone regarding any recurrence of the disease on day 71±2.
Interventions
Group I received super-bioavailable itraconazole 130 mg (SB-130) once a day, Group II received conventional itraconazole 200 mg (CITZ-200) once a day (2 capsules of 100 mg), and Group III received CITZ 100 mg (CITZ-100) twice a day, after food. All the patients received emollients containing light liquid paraffin and white soft paraffin. Patients were asked to bring used and in-use strips of medicine at each visit for compliance. All patients received complete treatment for six weeks and were advised to use any other antifungal medication.
Measurement of Treatment Effect
The primary endpoint of the study was to compare the percentage of patients achieving a complete cure (clinical cure plus mycological cure) at the end of the treatment period from baseline in all the groups. Clinical cure was defined as the absence of any signs and symptoms (lesion severity score of 0) and complete clearance of the area involved (area severity score of 0). The Lesion Severity Score (LSS) comprises four symptoms: scaling, pruritus, erythema, and margin continuity or elevation of a representative lesion. Each symptom was scored on a four-point Likert scale of 0 to 3, where 0 denotes the absence of a symptom and 3 denotes the maximum intensity of an individual symptom. The LSS was obtained by the summation of individual signs and symptom scores at each time point (range: 0–12). The Area Severity Score (ASS) was calculated by the extent of lesions in terms of Body Surface Area (BSA), and ranged from 0 to 3, where 0 corresponds to the absence of lesions, 1 - BSA involvement of <3%, 2 - BSA involvement of 3%–10%, and 3 corresponds to BSA involvement of >10%.17 Mycological cure was defined as negative KOH at the end of 6 weeks.
Analysis Set
The Full Analysis Set (FAS) (ie, patients who received at least one dose of medication and completed at least one post-baseline follow-up visit) was used for efficacy and safety analyses.
Statistical Analysis
Baseline variables are presented as numbers and percentages, and as means with standard deviations (SDs), depending on the distribution of data. The mean difference in lesion and area severity scores was analyzed using one-way ANOVA with Tukey’s HSD test and chi-square test, with a significance level set at 0.05, as appropriate. The cure and relapse rates were compared using Fisher’s exact test. All p values were two-tailed. When appropriate, 95% confidence intervals were calculated. The denominator for the calculation of the relapse rate was the number of patients who achieved cure. All statistical analyses were performed using SPSS version 16.0 (SPSS, Armonk, NY, USA) and Microsoft Excel.
Result
Patients
Of 261 patients enrolled in this study, 240 were included in the FAS. Twenty-one patients (7 in the SB-130 group, 10 in the CITZ-200 group, and 4 in the CITZ-100 group) were lost to follow-up after enrolment. All the baseline characteristics are presented in Table 1. The patient distribution was homogeneous in all groups, and most patients presented with ≥3 lesions and a disease duration of ≥6 months.
 |
Table 1 Demographic and Baseline Clinical Characteristics of the Treatment Groups |
Treatment Response
Complete Cure Rate
At week 6, 140 of the 240 patients were completely cured, while 30 patients failed treatment (11 in SB-130, 5 in CITZ-200, and 14 in the CITZ-100 group), giving an overall cure rate of 58.33%. Seventy patients showed clinical improvement (>50% improvement in LSS and ASS) with 14 patients in SB-130 group, 25 CITZ-200 and 31 patients in CITZ-100 group, respectively. The cure rates in the SB-130, CITZ-200, and CITZ-100 mg groups thus were 69% (55 of 80 patients), 61% (47 of 77 patients), and 46% (38 of 83 patients), respectively (Figure 1). This difference was statistically significant for SB-130 compared with CITZ-100 (p<0.05), but no statistically significant difference was noted between the SB-130 and CITZ-200 (p=0.32) and CITZ-200 and CITZ-100 (p=0.058) groups.
 |
Figure 1 Consort diagram. |
In the subgroup analysis of chronic dermatophytosis, 41/61 patients (67%) in the SB-130 group, 33/57 (58%) in the CITZ-200 group, and 27/61 patients (44%) in the CITZ-100 group achieved a complete cure, whereas 9, 4, and 12 patients showed clinical failure in the SB-130, CITZ-200, and CITZ-100 groups, respectively (Table 2). This difference was statistically significant for SB-130 compared with CITZ-100 (p<0.05), but no statistical difference was noted between the SB-130 and CITZ-200 (p=0.34) and CITZ-200 and CITZ-100 (p=0.14) groups.
 |
Table 2 Complete Cure, Clinical Improvement and Clinical Failure Rates in Different Dermatophytosis Groups at Week 6 |
In obese/overweight patients with dermatophytosis (BMI ≥25), in the SB-130 group, of 22/35 (63%) patients achieved complete cure whereas 23/39 (59%) and 12/37 (32%) patients in the CITZ-200 and CITZ-100 groups achieved complete cure, respectively, which was statistically significant for the OD groups over the BD group (p<0.05). No statistically significant difference was observed between the SB-130 and CITZ-200 groups (p=0.81).
Mycological Cure
At week 6, 71/80 patients (89%) in the SB-130 group achieved mycological cure, while 73/77 (95%) in the CITZ-200 group and 71/83 (86%) in the CITZ-100 group achieved the same results. There was no statistical difference between any of the groups in achieving mycological cure (p=0.14).
Improvement in Mean Scores
At week 6, the mean LSS of 9.43±1.97 was reduced to 1.35±1.92 (85% reduction) in the SB-130 group, while it was reduced from 9.32±2.07 to 1.30±1.97 (86% reduction) and from 9.79±1.19 to 2.06±2.52 (79% reduction) in CITZ-200 and CITZ-100 groups respectively. All treatments significantly reduced the LSS at the end of the therapy (p<0.05) from the baseline. However, in the inter-group comparison, a statistically significant difference was observed at week 6 (p<0.05) between the OD groups and BD group (Table 3).
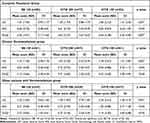 |
Table 3 Efficacy Scores in Terms of Mean LSS, ASS and DLQI at Week 6 |
Significant lesion clearance was observed in all groups at week 6. The mean ASS of 2.41±0.60, 2.42±0.62 and 2.40±0.56 was reduced to 0.65±0.76 (73% reduction), 0.61±0.75 (75% reduction) and 0.82±0.87 (65% reduction) in the SB-130 group, CITZ-200 and CITZ-100 groups respectively. All treatments were found to be statistically significant in clearing lesions from baseline at week 6 (p<0.05), but no statistical difference was noted in the inter-group comparison. For DLQI, a statistical difference was observed between the SB-130 and CITZ-100 groups (Table 3).
In the case of chronic dermatophytosis, only SB-130 was found to be statistically significant compared to CITZ-100 for LSS. No statistical differences were noted in the other mean scores between the groups. For obese patients, a statistical difference was observed between the OD and BD groups for LSS only; however, no statistical difference was noted for any of the other domains. There was no statistically significant difference between the SB-130 and CITZ-200 group (p=0.88) (Table 3).
Relapse Rates
Thirteen of the 13/140 patients (9%) relapsed following successful treatment completion. There were five relapses in the SB-130 group (9% completely cured), six in the CITZ-200 group (13% completely cured), and two in the CITZ-100 group (5% completely cured), and the difference in relapse rates among the groups was not statistically significant (p=0.50). Similarly, in the chronic group, 5/41 (12%) patients in the SB-130 group, 1/33 (3%) patient in the CITZ-200 and 1/27 (4%) patient in the CITZ-100 group relapsed, which was not statistically significant (p=0.36). In obese patients with dermatophytosis, 4/35 (11%) patients, 4/39 (10%), and 0/37 patients relapsed in the SB-130, CITZ-200, and CITZ-100 groups, respectively (p=0.1). The percentages of patients with relapse in the different dermatophytosis groups are shown in Figure 2.
 |
Figure 2 Percentage of patients with complete cure and relapse in dermatophytosis. |
Safety Outcome
All treatments were well-tolerated by the patients. In the SB-130 group, only one patient had pruritus, whereas three patients in the CITZ-200 group reported adverse events (pruritus, erythema, and burning in one patient each), and none of the patients had any adverse events (AE) in CITZ-100 group. There were no serious adverse events (SAE) or treatment discontinuations in any group. Additionally, no derangements in liver enzyme levels were noted at the end of treatment in any group.
Discussion
Multiple guidelines recommend ITZ at a dose of 200 mg/day.1,17 However, in the current scenario, multiple ITZ dosing practices have been observed by clinicians, such as ITZ 200 mg/day or two divided doses. Additionally, SB-ITZ 130 mg has proven its bioequivalence to ITZ 200 mg,18 which is commonly prescribed once daily. As the total dose of ITZ was the same in all three groups, we aimed to compare different dosing practices in the management of dermatophytosis.
Compared with the recent literature on ITZ cure rates, a slightly lower cure rate has been noted in all ITZ groups.8,13 However, the treatment duration was also lower in our study. There was a statistically significant difference in the cure rates between the SB-130 and CITZ 100 mg groups; however, no statistically significant difference was noted between the other groups. The reason for these failures may thus be inter-patient variability in itraconazole serum and sebum concentrations, as documented in some articles.18–20
Itraconazole has highly variable and complex pharmacokinetics, particularly following oral administration. Both itraconazole and hydroxy-itraconazole have non-linear kinetics in a comparison of single- versus multiple-dose administration.21,22 Multiple studies of the effect of food on itraconazole absorption documented the erratic absorption pattern of itraconazole and high inter-patient variations, with considerable variability in the area under curve (AUC) concentrations in the fed as well as fasted states.23–26 In contrast, SB-ITZ has less restrictive administration conditions, lower inter-patient variability, and subjective drug tolerability.27 In recent times, there has been influx of higher ITZ formulations like 200 mg and 400 mg, but Sardana et al, had mentioned the limitation of ITZ-200 mg capsule and raised the question on the quality of CITZ-200 mg as a single capsule in the manufacturing process.28 In our study, we used two capsules of ITZ-100 mg and not the single capsule of ITZ-200 mg in CITZ-200 group.
In terms of mean efficacy scores for LSS, significant clearance of lesions was observed in all groups, with a statistically significant difference in OD over the BD group. Notably, uncured patients in all groups had mild pruritus at the end of 6 weeks. This could be due to an alteration in barrier function by dermatophytes, as reported in a recent article.29 No statistical difference was observed for ASS, indicating that neither the dosing of ITZ nor the cure rates were considerably affected by the BSA involved, leading to the effectiveness of all regimens. Quality of life also improved significantly in the SB-130 group compared with the CITZ-100 group, thus reflecting the advantages of SB-ITZ and once-daily dosing with a single pill.
In our study, we observed a relatively low relapse rate (9%), with no statistically significant difference between any of the groups, as compared to the recently published literature.8 This could be due to persistent itraconazole levels in the stratum corneum up to 3–4 weeks even after cessation of the drug.30
In the subgroup analysis, we observed similar results in the chronic dermatophytosis group; however, in obese patients with dermatophytosis, OD dosing was found to be statistically significant compared to BD dosing. Once absorbed, ITZ is highly protein-bound and has a large volume of distribution (11 L/kg), which includes penetration into multiple organs and various other tissues.31,32 Grant et al demonstrated that approximately 17% of the plasma concentration of ITZ is distributed to adipose tissues33 and obese patients have a much higher fat mass.31,34–36 Hardin et al have already concluded the non-linear increase in AUC and Cmax of ITZ,21 thus confirming the advantage of OD dosing over BD dosing. At the time of writing this manuscript, there had been no studies on ITZ dosing in obese patients with dermatophytosis.
Of the 240 enrolled patients, infection persisted in 100 (41.67%), suggesting a significantly prolonged treatment duration. As mentioned earlier, the treatment duration in our study was only six weeks. In recently published articles, ITZ was studied for 8 weeks, thus giving a cure rate between 76%-93%.8,13 The ITART consensus also recommended individualized treatment based on clinical response.1
In our study, clinical and mycological cure did not occur concurrently, which was in accordance with a recently published article.8 Hence, it is important to evaluate both before discontinuing treatment. In this context, KOH smear examination stands out as a diagnostic tool for treatment monitoring owing to its low cost and quick turnaround time.37,38
Treatment-related adverse events (TEAEs) reported in our study were relatively low compared to those reported in the literature.8,39–41 ITZ is known to cause some mild gastrointestinal complaints, such as nausea or abdominal pain, headache, and elevation of transaminase levels, which led to treatment discontinuation. However, in the present study, there was no elevation of transaminase levels or treatment discontinuation.
Limitations
This is the first clinical comparative study of the same dose of ITZ per day in glabrous tinea, but with a different dosing pattern and formulation in Indian patients. In this study, the treatment period was only six weeks, and a long follow-up period for recurrences was not performed. The non-blinding and non-identification of isolates by fungal culture also have major limitations. Hence, a double-blind, randomized, comparative clinical study with fungal cultures for a longer duration and follow-up period is warranted.
Conclusion
In this clinical study, we report moderate efficacy with all doses of ITZ, but better efficacy with OD dosing; hence, longer treatment durations are needed to achieve a complete cure. Although there was no statistical difference between SB-130 and CITZ-200, SB-130 could be preferred over CITZ-200 owing to the advantage of SB over conventional ITZ and quality issues with a single ITZ-200 mg capsule. Additionally, SB-130 mg was safe and tolerable compared to CITZ-200 mg.
Data Sharing Statement
Data available on request due to privacy/ethical restrictions and same can be requested to [email protected].
Acknowledgment
The drugs used in this study were supplied by Glenmark Pharmaceuticals, Ltd. The company had no role in the study design and conduct, or in the collection, management, analysis, or interpretation of the data. The authors also thank Mr. Manoj Karwa (Auriga Research Pvt. Ltd., Gurgaon) for help with the clinical operations of the study and Ms. Deepal Mistry (Ascent Insights, Mumbai) for helping with statistical analysis.
Funding
The drugs used in this study were supplied by Glenmark Pharmaceuticals Ltd. The company had no role in the study design and conduct, or in the collection, management, analysis, or interpretation of the data.
Disclosure
Manjunath M Shenoy reports grants from Glenmark pharmaceuticals, India. Dhiraj Dhoot, Namrata Mahadkar, Sumit Bhushan, Rujuta Gadkari, and Hanmant Barkate are employees of Glenmark Pharmaceuticals Ltd., India. The authors declare no other conflicts of interest in this work.
References
1. Rengasamy M, Shenoy MM, Dogra S, et al. Indian Association of Dermatologists, Venereologists and Leprologists (IADVL) Task Force against Recalcitrant Tinea (ITART) Consensus on the Management of Glabrous Tinea (INTACT). Indian Dermatol Online J. 2020;11(4):502–519. doi:10.4103/idoj.IDOJ_233_20
2. Bishnoi A, Vinay K, Dogra S. Emergence of recalcitrant dermatophytosis in India. Lancet Infect Dis. 2018;18(3):250–251. doi:10.1016/S1473-3099(18)30079-3
3. Verma SB, Zouboulis C. Indian irrational skin creams and steroid-modified dermatophytosis - an unholy nexus and alarming situation. J Eur Acad Dermatol Venereol. 2018;32(11):e426–e427. doi:10.1111/jdv.15025
4. Hay RJ, Ashbee HR. Fungal infections. In: Griffiths CE, Barker J, Bleiker T, Chalmers R, Creamer D, editors. Rook’s Textbook of Dermatology.
5. Schieke SM, Garg A. Fitzpatrick’s Dermatology in General Medicine.
6. Shenoy MM, Shenoy SM. Superficial fungal infections. In: Sacchidanand S, Oberoi C, Inamdar AC, editors. IADVL Textbook of Dermatology.
7. Khurana A, Sardana K, Chowdhary A. Antifungal resistance in dermatophytes: recent trends and therapeutic implications. Fungal Genet Biol. 2019;132(132):103255. doi:10.1016/j.fgb.2019.103255
8. Khurana A, Agarwal A, Agrawal D, et al. Effect of different itraconazole dosing regimens on cure rates, treatment duration, safety, and relapse rates in adult patients with tinea corporis/cruris: a randomized clinical trial. JAMA Dermatol. 2022;158(11):1269–1278. doi:10.1001/jamadermatol.2022.3745
9. Das S, De A, Saha R, et al. The current Indian epidemic of dermatophytosis: a study on causative agents and sensitivity patterns. Indian J Dermatol. 2020;65(2):118–122. doi:10.4103/ijd.IJD_203_19
10. Lindsay J, Mudge S, Thompson GR. Effects of food and omeprazole on a novel formulation of super bioavailability itraconazole in healthy subjects. Antimicrob Agents Chemother. 2018;62(12):e01723–18. doi:10.1128/AAC.01723-18
11. Central Drugs Standard Control Organisation. Recommendations of the SEC (Antimicrobial & Antiviral) made in its 103nd meeting held on 25.08.2021 at CDSCO HQ, New Delhi. Available from: https://cdsco.gov.in/opencms/resources/UploadCDSCOWeb/2018/UploadCommitteeFiles/RecommendationSE%20Antimicrobial%20&%20Antiviral%2025.08.2021n.pdf.
12. U.S. Food and Drug Administration. SPORANOX® (itraconazole) Capsules. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020083s040s041s044lbl.pdf.
13. Singh SK, Subba N, Tilak R. Efficacy of terbinafine and itraconazole in different doses and in combination in the treatment of tinea infection: a randomized controlled parallel group open labeled trial with clinico-mycological correlation. Indian J Dermatol. 2020;65(4):284–289. doi:10.4103/ijd.IJD_548_19
14. Shenoy M, Dhoot D, Mahajan H, Barkate H. An open-label, randomized, double-arm clinical trial to compare the effectiveness and safety of super bioavailable itraconazole capsules and itraconazole capsules in the management of dermatophytosis in India. Clin Cosmet Investig Dermatol. 2021;Volume 14(14):1367–1376. doi:10.2147/CCID.S326642
15. Mahajan H, Dhoot D, Deshmukh G, Barkate H. Comparative clinical effectiveness and safety of super bioavailable itraconazole and conventional itraconazole in management of dermatophytosis: a retrospective data analysis. Int J Res Dermatol. 2021;7(7):388–394. doi:10.18203/issn.2455-4529.IntJResDermatol20211427
16. NHS Fife.DERMATOLOGY LIFE QUALITY INDEX (DLQI). Available from: https://www.nhsfife.org/media/32589/dermatology-life-quality-index-dlqi.pdf.
17. Rajagopalan M, Inamadar A, Mittal A, et al. Expert Consensus on The Management of Dermatophytosis in India (ECTODERM India). BMC Dermatol. 2018;18(1):6. doi:10.1186/s12895-018-0073-1
18. Dhoot D, Jain GK, Manjhi M, Kesharwani P, Mahadkar N, Barkate H. Pharmacokinetic and clinical comparison of super-bioavailable itraconazole and conventional itraconazole at different dosing in dermatophytosis. Drugs Context. 2023;12:1. doi:10.7573/dic.2022-8-1
19. Abuhelwa AY, Foster DJR, Mudge S, Hayes D, Upton RN. Population pharmacokinetic modeling of itraconazole and hydroxyl itraconazole for oral SUBA-itraconazole and Sporanox capsule formulations in healthy subjects in fed and fasted states. Antimicrob Agents Chemother. 2015;59(9):5681–5696. doi:10.1128/AAC.00973-15
20. Khurana A, Agarwal A, Singh A, et al. Predicting a therapeutic cut-off serum level of itraconazole in recalcitrant tinea corporis and cruris-A prospective trial. Mycoses. 2021;64(12):1480–1488. doi:10.1111/myc.13367
21. Hardin TC, Graybill JR, Fetchick R, Woestenborghs R, Rinaldi MG, Kuhn JG. Pharmacokinetics of itraconazole following oral administration to normal volunteers. Antimicrob Agents Chemother. 1988;32(9):1310–1313. doi:10.1128/AAC.32.9.1310
22. Mouton JW, van Peer A, de Beule K, Van Vliet A, Donnelly JP, Soons PA. Pharmacokinetics of itraconazole and hydroxyitraconazole in healthy subjects after single and multiple doses of a novel formulation. Antimicrob Agents Chemother. 2006;50(12):4096–4102. doi:10.1128/AAC.00630-06
23. Yun HY, Baek MS, Park IS, Choi BK, Kwon KI. Comparative analysis of the effects of rice and bread meals on bioavailability of itraconazole using NONMEM in healthy volunteers. Eur J Clin Pharmacol. 2006;62(12):1033–1039. doi:10.1007/s00228-006-0200-5
24. Zimmermann T, Yeates RA, Laufen H, Pfaff G, Wildfeuer A. Influence of concomitant food intake on the oral absorption of two triazole antifungal agents, itraconazole and fluconazole. Eur J Clin Pharmacol. 1994;46(2):147–150. doi:10.1007/BF00199879
25. Zimmermann T, Yeates RA, Albrecht M, Laufen H, Wildfeuer A. Influence of concomitant food intake on the gastrointestinal absorption of fluconazole and itraconazole in Japanese subjects. Int J Clin Pharmacol Res. 1994;14(3):87–93.
26. Bae SK, Park SJ, Shim EJ, et al. Increased oral bioavailability of itraconazole and its active metabolite, 7-hydroxyitraconazole, when coadministered with a vitamin C beverage in healthy participants. J Clin Pharmacol. 2011;51(3):444–451. doi:10.1177/0091270010365557
27. Rauseo AM, Mazi P, Lewis P, Burnett B, Mudge S, Spec A. Bioavailability of single-dose SUBA-itraconazole compared to conventional itraconazole under fasted and fed conditions. Antimicrob Agents Chemother. 2021;65(8):e0013421. doi:10.1128/AAC.00134-21
28. Sardana K, Khurana A, Singh A, Gautam RK. A pilot analysis of morphometric assessment of itraconazole brands using dermoscopy and its relevance in the current scenario. Indian Dermatol Online J. 2018;9(6):426–431. doi:10.4103/idoj.IDOJ_339_17
29. Sardana K, Gupta A, Mathachan SR. Immunopathogenesis of dermatophytoses and factors leading to recalcitrant infections. Indian Dermatol Online J. 2021;12(3):389–399. doi:10.4103/idoj.IDOJ_503_20
30. Cauwenbergh G, Degreef H, Heykants J, Woestenborghs R, Van Rooy P, Haeverans K. Pharmacokinetic profile of orally administered itraconazole in human skin. J AmAcad Dermatol. 1988;18(2):263–268. doi:10.1016/S0190-9622(88)70037-7
31. Amsden JR, Slain D. Antifungal dosing in obesity: a review of the literature. Curr Fungal Infect Rep. 2011;5(2):83–91. doi:10.1007/s12281-011-0049-7
32. De Beule K, Van Gestel J. Pharmacology of itraconazole. Drugs. 2001;61 Suppl 1:27–37. doi:10.2165/00003495-200161001-00003
33. Grant SM, Clissold SP. Itraconazole. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in superficial and systemic mycoses. Drugs. 1989;37(3):310–344. doi:10.2165/00003495-198937030-00003
34. Blouin RA, Warren GW. Pharmacokinetic considerations in obesity. J Pharm Sci. 1999;88(1):1–7. doi:10.1021/js980173a
35. Cheymol G. Effects of obesity on pharmacokinetics implications for drug therapy. Clin Pharmacokinet. 2000;39(3):215–231. doi:10.2165/00003088-200039030-00004
36. Hanley MJ, Abernethy DR, Greenblatt DJ. Effect of obesity on the pharmacokinetics of drugs in humans. Clin Pharmacokinet. 2010;49(2):71–87. doi:10.2165/11318100-000000000-00000
37. Khurana A, Agarwal A, Agrawal D, Sethia K. Re-emerging role of KOH smear examination in the era of recalcitrant dermatophytoses. Dermatol Ther. 2021;34(2):e14891. doi:10.1111/dth.14891
38. Shenoy MM, Teerthanath S, Karnaker VK, Girisha BS, Krishna Prasad MS, Pinto J. Comparison of potassium hydroxide mount and mycological culture with histopathologic examination using periodic acid-Schiff staining of the nail clippings in the diagnosis of onychomycosis. Indian J Dermatol Venereol Leprol. 2008;74(3):226–229. doi:10.4103/0378-6323.39584
39. Thompson GR, Lewis P, Mudge S, Patterson TF, Burnett BP. Open-label crossover oral bioequivalence pharmacokinetics comparison for a 3-day loading dose regimen and 15-Day Steady-State Administration of SUBA-itraconazole and conventional itraconazole capsules in healthy adults. Antimicrob Agents Chemother. 2020;64(8):e00400–20. doi:10.1128/AAC.00400-20
40. Nield B, Larsen SR, van Hal SJ. Clinical experience with new formulation SUBA®-itraconazole for prophylaxis in patients undergoing stem cell transplantation or treatment for haematological malignancies. J Antimicrob Chemother. 2019;74(10):3049–3055. doi:10.1093/jac/dkz303
41. Lindsay J, Sandaradura I, Wong K, et al. Serum levels, safety and tolerability of new formulation SUBA-itraconazole prophylaxis in patients with haematological malignancy or undergoing allogeneic stem cell transplantation. J Antimicrob Chemother. 2017;72(12):3414–3419. doi:10.1093/jac/dkx295
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
