Back to Journals » ImmunoTargets and Therapy » Volume 13
Efficacy and Safety Profile of Tuberculin Protein Purified Derivative Injection As Immunotherapy For the Treatment of Cutaneous and Anogenital Warts: A Review Article
Authors Achdiat PA , Suwarsa O , Hidayat YM , Shafiee MN, Dwiyana RF , Hindritiani R , Sutedja E, Pudjiati SR, Hilmanto D , Dhamayanti M , Parwati I, Maharani RH , Sutedja EK , Avriyanti E, Yunitasari
Received 28 October 2023
Accepted for publication 22 February 2024
Published 5 March 2024 Volume 2024:13 Pages 123—150
DOI https://doi.org/10.2147/ITT.S446938
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Michael Shurin
Pati Aji Achdiat,1,2 Oki Suwarsa,1,2 Yudi Mulyana Hidayat,2,3 Mohamad Nasir Shafiee,4 Reiva Farah Dwiyana,1,2 Reti Hindritiani,1 Endang Sutedja,1 Satiti Retno Pudjiati,5 Dany Hilmanto,2,6 Meita Dhamayanti,2,6 Ida Parwati,2,7 Retno Hesty Maharani,1 Eva Krishna Sutedja,1 Erda Avriyanti,1 Yunitasari1
1Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia; 2Doctoral Study Program Faculty of Medicine Universitas Padjadjaran, Bandung, West Java, Indonesia; 3Department of Obstetrics and Gynecology, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia; 4Department of Obstetrics and Gynecology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia; 5Department of Dermatology and Venereology, Faculty of Medicine Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia; 6Department of Pediatric, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia; 7Department of Clinical Pathology, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia
Correspondence: Pati Aji Achdiat, Email [email protected]
Introduction: Various treatments available today for anogenital and cutaneous warts have limitations, including time-consuming, challenging to perform, and the risk of scarring. A new treatment using tuberculin purified protein derivative (PPD) has been developed, which is expected to generate cellular immunity against HPV.
Objective: To assess the evidence for the efficacy and safety of PPD treatment for cutaneous and anogenital warts.
Materials and methods: A literature search was performed with the keyword-based search on digital libraries, including the National Library of Medicine, Cochrane Controlled Register of Trial, and Google Scholar, using the following terms: anogenital warts, condyloma acuminata, cutaneous warts, human papillomavirus, immunotherapy, and tuberculin purified protein derivative. Original studies on treating cutaneous or anogenital warts with PPD were included. The results were 47 clinical trials and 4 case reports. Most of the research was done in countries with common Mycobacterium tuberculosis infection. The treatment showed good efficacy. Comparative studies showed that the treatment has similar efficacy with other immunotherapies. No significant side effects were reported, with evidence of the safety use on the pregnant population.
Conclusion: Based on good efficacy and safety, PPD can be considered an alternative therapy, especially in countries where tuberculosis is frequent.
Keywords: anogenital warts, condyloma acuminata, cutaneous warts, human papillomavirus, immunotherapy, tuberculin purified protein derivative
Introduction
Cutaneous and anogenital warts (AGWs) are manifestations of infection caused by human papillomavirus (HPV) on the skin and mucous membranes.1–3 It has been estimated that 7–10% of the population were affected by HPV infection.4 Furthermore, HPV is also the most frequent sexually transmitted infection worldwide, with an estimated global incidence of 160–289 cases per 100.000 persons per year.2,5 Warts can significantly impair a patient’s quality of life due to physical discomfort and cosmetic disfigurement.2,3 In two-thirds of patients, warts can undergo spontaneous resolution within two years; however, they can also resolve slowly and persist for many years with a high recurrence rate.6 Various modalities are available and being used in the treatment of warts, including destructive treatments (eg, cryotherapy, electrosurgery, ablative laser, or surgical removal), pharmacological treatments (eg, salicylic acid, trichloroacetic acid, podophyllin, 5-fluorouracil, bleomycin, imiquimod),2,3,7,8 and photodynamic therapy.7 Topical treatments are more tolerable to patients but require frequent applications.2 Meanwhile, destructive modalities require fewer treatment sessions, but they are destructive, frequently cause pain, and may lead to scarring. Furthermore, treatment modalities available to date showed variable effectiveness and are often associated with recurrence.3 Conventional treatment approaches are limited to local application and lack systemic effect; therefore, they are unfavorable for patients with multiple lesions and difficult-to-reach locations.2,9 Cell-mediated immunity (CMI) is paramount in the clearance of HPV infection and subsequent wart resolution.3 Virus-induced CMI has been shown to cause warts to regress spontaneously.4 Immunotherapeutic agents increase recognition of HPV by the patient’s immune system by stimulating CMI at the site of the wart,1 therefore helping to eradicate the virus rather than only removing visible skin lesions.1,3 Cytokines released from T helper 1 cells, such as interleukin (IL)-2 and interferon (IFN)-γ are predominantly increased in response to immunotherapeutic agent injection.2 Through the induction of delayed-type hypersensitivity and activation of cytotoxic and natural killer cells against the virus, intralesional immunotherapy can increase the host immunity to HPV.4 Due to its non-destructive action and low recurrence rates, immunotherapy has recently received growing interest in the treatment of warts.3 Various immunotherapeutic agents have been studied to stimulate the host immune response, including Candida albicans; measles, mumps, and rubella (MMR); Trichophyton; purified protein derivative (PPD); Mycobacterium w (Mw), and Bacillus Calmette-Guerin (BCG) with variable outcome.2,3
Purified protein derivative contained extract of Mycobacterium tuberculosis, routinely used to test for tuberculin protein, either acquired from previous vaccination or environmental exposure.4 The first standardized preparation of PPD was produced in 1944, known as PPD-Standard (PPD-S). This was later adopted as the international standard of tuberculin by the World Health Organization (WHO). All formulations of PPD produced after that must show potency equivalent to PPD-S. One tuberculin unit (TU) equals the biological activity contained in 0.02 μg of PPD-S. PPD-RT23 is the most widely used PPD product globally. It is stated that 2.5TU of PPD-RT23 containing Tween 80 had similar potency to 5TU of PPD-S.10 PPD is a ubiquitously available antigen and has shown promising results for treating warts in different studies.11,12 It was first introduced by Kus et al13 in 2005 to eighteen patients with recalcitrant cutaneous warts in Turkey, where tuberculosis vaccination is routinely performed. PPD was chosen for this reason. The study protocol involved intralesional injection of PPD RT23-5TU with 3-week intervals into each target wart. Complete clearance was reported in 29.4% of patients, and overall improvement (>50% reduction in wart size) was achieved in 58%. Additionally, two patients underwent complete clearance of distant untreated warts. This study demonstrated a promising result of PPD injection in treating warts, particularly in countries where tuberculosis vaccination is performed routinely.13 Based on this finding, numerous studies have increasingly developed ever since.
Injection of antigen to which the patient was previously sensitized induces the elicitation phase of the immune response to recognize HPV antigens.14 Intralesional PPD is known to stimulate the production of T helper 1 cytokines, such as interleukin IL-4, 5, 8, 12, IFN-γ and tumor necrosis factor (TNF)-α which drive cytotoxic and natural killer cells to develop an immune response against HPV. A study by Azab et al15 documented an increase in the serum level of IL-17 after PPD injection. Abd-Elazeim et al16 reported that wart clearance was related to the relative increase of IL-12, another Th1 cytokine. In addition to IL-12, Shaheen et al17 also reported a higher level of serum IL-4 after PPD injection compared to baseline level. Interferon-γ was found to be increased after PPD injection in a study by Abou-Taleb et al.
Furthermore, this study compared cytokine levels after PPD and vitamin D3 injection. The PPD group demonstrated an increase of both IL-12 and IFN-γ, while the latter only showed an increase of serum IFN-γ level. These findings suggested that PPD induces a higher Th1 immune response than vitamin D3.18 Conversely, Sil et al19 reported that IL-10, a Th2 cytokine, was downregulated after immunotherapy with PPD, Mw vaccine, Measles, and MMR vaccine. In this study, a decline in IL-10 was associated with a decrease in size and warts. Its level was found to be significantly low in complete responders of the PPD group compared to the partial responders at the end of the study period, indicating its essential role in the total clearance of lesions. The production pattern of the abovementioned cytokines might explain the mechanism of action of PPD in inducing wart clearance.
This study aims to evaluate the evidence regarding the efficacy and safety of PPD for treating cutaneous and anogenital warts.
Methods
We performed a literature search on digital libraries, including the National Library of Medicine, Cochrane Controlled Register of Trial, and Google Scholar. Original studies on the treatment of cutaneous or anogenital warts using purified protein derivatives from 2011 (2022) were included, as well as comparative studies and case reports. The search used the following terms: warts, verruca, condyloma, anogenital warts, cutaneous warts, purified protein derivative, and immunotherapy. Only English-language articles involving human subjects were included. After performing this initial filtering process, we further reviewed the remaining articles for relevance to our subject.
Results
We initially discovered 279 articles through a literature search of the abovementioned platforms. After reviewing the full-text articles for relevance to our subject, 228 were excluded. A total of 47 clinical trials, including 26 comparative studies and 4 case reports, were included in the final analysis (Figure 1). The selected articles should at least report the efficacy of the treatment. These studies were distributed over countries where Mycobacterium tuberculosis infection is common and BCG vaccination is mandatory, namely Egypt, India, Nepal, Iran, Iraq, Saudi Arabia, Pakistan, Malaysia, Philippines, and Indonesia. The intervention applied in each study is detailed in Tables 1 and 2 below. Most studies evaluated treatment outcomes on the size and number of lesions. Complete clearance was defined as total resolution of lesion(s) and return of the typical skin markings, partial if the clearance occurred in some of the lesions (varied between studies, ranging from 25–99%), and no response. Treatment outcome was primarily assessed on the injected lesion, and several studies also evaluated the outcome on distant-site lesions.
 |
Table 1 Clinical Trials Using PPD Immunotherapy in Cutaneous and Anogenital Warts |
 |
Table 2 Case Reports Using PPD Immunotherapy in Cutaneous and Anogenital Warts |
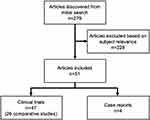 |
Figure 1 Flowchart of the article selection process. |
Discussion
Efficacy
We assessed the efficacy based on the complete clearance rate in each study. Immunotherapy showed variable efficacy across these studies, ranging from 13.3% to 96%. Figure 2 shows the complete clearance rate reported in all studies in the present work. Twelve studies (25.6%) reported an efficacy rate of 70–79%, followed by 60–69% in 11 studies (23.4%). There were nine studies (19.1%) that reported an efficacy of 50–59%, while a similar number of other studies (9; 19.1%) had an efficacy below 50%. The efficacy in 5 studies (10.6%) was 80–89%, and in 1 study (2.2%), it had efficacy >90%. The overall mean complete clearance rate is 61.5%.
 |
Figure 2 Efficacy of Purified Protein Derivative in all studies. |
The highest complete clearance rate (96%) was reported in a comparative study by Elela et al. This randomized-controlled trial, involving 110 patients with different cutaneous warts, was conducted in Egypt. Patients were divided into three groups: the first group received 0.1 mL intralesional PPD, the second group received 0.1 mL PPD given intradermally on the right forearm, and the third group (control) received 0.1 mL intralesional saline. A complete clearance rate was achieved in 96% of patients in group 2, compared to 94.1% in group 1. However, this difference was not statistically significant. The clearance in the control group was 15%. Treatment was done every two weeks for a maximum of 10 sessions. The longer treatment duration might explain the high clearance rate observed in this study.31 Meanwhile, the lowest complete clearance (13.3%) was reported by Moubasher et al, in which 15 patients with anogenital warts were given PPD-5TU intralesional injection into the largest wart and evaluated at two weeks. The injection volume was determined by the size of skin test reactivity conducted prior to treatment, ie, 0.3, 0.2, and 0.1 mL of PPD if the size of induration was 5–20 mm, 21–40 mm, and >40 mm, respectively. This study was performed in Egypt. This finding might be related to the shorter treatment duration and the fewer participants in this study.43
In addition, we included four case reports which also evaluated the efficacy of PPD. Achdiat et al used 0.2 mL PPD-2TU given weekly for three sessions as an intralesional injection in a case of AGWs in a 30-year-old homosexual man. Clinical improvement was observed starting on day 18th and complete resolution on day 46th.58 Despite the various treatment modalities available for AGWs, large recalcitrant lesions tend to be more resistant to treatments and carry a high risk of pain, scarring, and recurrence. Alhashmi et al reported a case of giant condyloma acuminata successfully treated with intralesional PPD in a dose of 0.2–0.3 mL, injected on 2 or 3 different lesions at least 2 cm apart, given at 2-week intervals. After seven sessions, more than 98% of the lesions were cleared. Then, four sessions of cryotherapy and topical podophyllin were added to clear the remaining small lesions. Ten months of follow-up revealed no recurrence.59 Manoj et al further reported the efficacy of PPD in a case series involving five patients with multiple cutaneous warts. Significant improvement was noticed in 80% of patients at the end of 3 months.60 Moreover, Nofal et al evaluated the effect of switching between intralesional antigens in 2 cases of multiple recalcitrant cutaneous warts that demonstrated complete clearance with intralesional Candida antigen after failure of treatment with five sessions of MMR and PPD. Differences in the injected antigens’ processing, presentation, and cytokine production may affect the variable responses observed in these cases.61
As depicted in Figure 2, most studies (25%) reported an efficacy rate of 70–79%. The efficacy of PPD was further confirmed in placebo-controlled studies. A statistically significant difference was constantly demonstrated between the PPD and placebo group, implying its significant role in inducing wart clearance.15,16,22,54
Furthermore, Abd-Elazeim et al16 and Azab et al15 evaluated the effect of PPD on the clearance of distant non-injected warts. In the former study, complete clearance of distant wart(s) was observed in 25% of patients in the PPD group compared to 0 in the placebo group.16 Azab et al15 reported an even higher complete clearance rate (66.7%) in the PPD group. This further adds to another beneficial effect of PPD, which is not seen with conventional treatments, suggesting its preferable use for multiple and difficult-to-reach lesions.15–17
Regarding time to resolution, complete clearance was achieved as early as two weeks after PPD injection in several studies.50,53,55 Pundir et al used intralesional injection of PPD-2TU on 40 patients with plane warts on the face. Injection was done on each wart, with a maximum of 10TU in each session. Treatment was performed every two weeks for a total of 4 sessions. Complete clearance was observed in 3 patients after two weeks. The mean age of patients in this study was 25.3 years old (range 15–40). The number of lesions ranged from 15–to 40, with an average of 25.85 lesions. Disease duration ranged from 6 to 24 months, with a mean duration of 7.05 months.50 The higher dose of PPD used in this study might contribute to the faster resolution of lesions. Nevertheless, Nimbalkar et al reported that complete clearance of lesions was first observed at the end of 6 weeks. This study involved 45 patients with single or multiple warts of different types, treated with intralesional injection of PPD-10TU on the largest wart, every two weeks for a maximum of 6 sessions.45
Safety
Adverse events (AEs) related to PPD injections were most frequently reported in the form of local reactions. Figure 3 shows the variable local AEs following PPD injection.
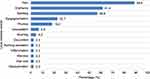 |
Figure 3 Local adverse events following Purified Protein Derivative injection. |
Among the 44 studies reporting AEs of PPD, pain at the injection site was the most frequently reported local AEs. However, it was mild and tolerable. Significant local AEs were reported by Mishra et al in which intense swelling, pain, and edema requiring discontinuation of therapy occurred in 2 cases. The characteristics of patients experiencing these AEs were not mentioned in detail. In this study, patients received an intralesional injection of 0.1 mL PPD into the most prominent wart every two weeks, with a maximum of 6 sessions.14 In a study by Nimbalkar et al, abscess and localized hair loss at the injection site were noted in 1 patient each. Patients in this study received PPD-10TU injected intralesionally into the most prominent wart every two weeks for a maximum of 6 sessions.45
A few patients experienced systemic AEs in the form of fever, flu-like symptoms, myalgia, acute urticaria, and malaise, as depicted in Figure 4. Rare AEs in the form of acute urticaria were reported in 3 studies.8,24,45 The mechanisms underlying such events are still unknown.
 |
Figure 4 Systemic adverse events following Purified Protein Derivative injection. |
In several studies, the study participants included a pediatric age group as young as four.22,30,34,45,50 There was no dose-adjustment according to age in these studies, and all study participants received similar interventions. Unfortunately, the outcomes of this particular population were also not explicitly reported, and the data was presented along with that of the other study participants. One study compared the efficacy and safety of PPD and zinc sulfate 2%, specifically in pediatric warts, and no serious AEs were reported in any of the study participants.45
Pregnant Population
During pregnancy, due to altered immunity and increased blood flow, genital warts may multiply quickly. They can present in either clinical or subclinical form. The risk of transmission from mother to child with subsequent disease development has been estimated to be around 1:80 and 1:1500, respectively. It is worthwhile to consider giving this modality of treatment to pregnant women because AGWs in this population are frequently challenging to treat, and this type of treatment is classified as category C in pregnancy. Despite lacking animal studies, the Advisory Council for the Elimination of Tuberculosis states that tuberculin skin testing is considered valid and safe throughout pregnancy. Eassa et al conducted a randomized clinical trial involving 40 pregnant Egyptian women with recalcitrant AGWs. Twenty patients received intradermal injection of 0.1 mL PPD repeated weekly for 12 weeks, while another 20 patients received intradermal injection of 0.1 mL distilled water (placebo) for four weeks and then shifted to 0.1 mL PPD weekly for 12 weeks. At the end of 12 weeks, 50% of patients in the PPD group achieved complete resolution.
Meanwhile, in the placebo group, none of the patients experienced any improvement in the first four weeks; nonetheless, 45% of patients reported complete resolution after treatment shifted to PPD injections for 12 weeks. All patients showing complete resolution were followed up for over six months, and no recurrence was reported. Adverse effects were mild and manifested locally at the injection site as pain, erythema, and tenderness. No systemic AEs were noted. In this study, PPD showed good efficacy and safety profile in the treatment of AGWs in pregnant women.30
Influencing Factors
Dosage
The dose of PPD used in these studies was variable. Some studies administered a fixed dose for all patients. In contrast, in some others, the dose was based on the size of skin test reactivity conducted before treatment. Among the fixed-dose studies using single injection, the administered dose ranged from 2–15TU. Of 32 studies, the most frequently administered dose in a single injection was 5TU. Figure 5 shows the variable doses used in fixed-dose studies using single injection. The mean complete clearance rate among studies using 5TU was 59.9%. Meanwhile, studies using 10TU reported a higher mean complete clearance rate (67.25%). One study using 2TU reported a complete clearance of 50%;39 another study using 2.5 TU achieved an 86.7% clearance rate.57 A dosage of 4TU was reported in one study by Achdiat et al58 in a case of AGWs, and complete clearance was achieved on day 46th. Two studies by Alhashimi et al59 and Nofal et al61 using 15TU demonstrated a 98% clearance rate after seven sessions and 100% complete clearance after two sessions, respectively.
 |
Figure 5 Purified Protein Derivative dosage among fixed-dose studies using single injection. |
It has been hypothesized that response to PPD may be dose-dependent. Therefore, multiple injections are thought to be more effective and potentially require less time to clear warts. Among the fixed-dose studies using multiple injections, the maximum administered dose ranged from 10–25TU. Twenty-five TU was determined as the maximum dose of injection per session in 3 studies, followed by 10 TU in 2 studies and 12.5 TU in one study. A study by Milante et al comparing single versus multiple intralesional injections of PPD in 58 patients with common warts showed a superior clearance rate in the multiple injection group (79.3%) compared to the single injection group (58.6%). This difference was statistically significant (p=0.0236). PPD 5TU was injected into the most prominent wart in the single injection group. The injection volume was determined by the size of tuberculin skin test reactivity conducted before treatment. Meanwhile, in the multiple injection group, PPD-5TU was injected into all lesions with a maximum of 88TU or 1.76 mL. Injection was done every two weeks until clearance for a maximum of 6 sessions. The highest clearance was observed in week 12 for the single injection group and week 10 for the multiple injection group. However, multiple injections were reported to be significantly more painful than single injections. Late AEs, including constitutional symptoms and vesiculation, also occurred more frequently in the multiple injection group. There was no recurrence reported in both groups.40 One study by Sharquie et al54 performed multiple injections using PPD-2TU on multiple warts until the lesions blanched but did not specify the maximum volume administered in each session. The highest dose of PPD administered among these studies was 88TU. However, the related article did not mention in detail the number of patients who received this dose and whether there were associated AEs.
Nine studies determined the volume of PPD injection based on the size of skin test reactivity conducted before treatment. Five studies administered the dose according to Johnson et al20 in which 0.3; 0.2; and 0.1 mL of PPD were injected if the size of induration was 5–20; 21–40; and >40 mm, respectively. In four studies, the dose administered was determined based on Kus et al,13 in which 0.3; 0.2; and 0.1 mL of PPD was injected if the induration size was 5–9; 10–15; and >15 mm, respectively. The treatment outcome varied between the two groups. The prior sensitization status will be discussed more in the following section.
Interval
Regarding treatment interval, the shortest interval used in these studies was weekly, while the longest was four weeks. Thirty-seven out of 50 studies (74%) determined two weeks as the minimum interval between treatments, as shown in Figure 6. This interval was chosen as this is the usual time for an induration to heal following a Mantoux test (7–12 days).12 Among these studies using a 2-week interval, the mean complete clearance rate was 61.8%. This rate was lower than studies using weekly (64.6%) and 3-week intervals (74.3%). The lowest mean complete clearance rate was demonstrated in studies using a 4-week interval (18.5%).
 |
Figure 6 Different treatment intervals between studies. |
Routes of Administration
In the present work, 43 studies applied an intralesional injection. In comparison, five studies used intradermal injection either on the forearm or deltoid region. The remaining studies did not mention the method of injection. Elela et al evaluated the effect of intradermal versus intralesional injection of PPD in 110 patients with various cutaneous warts. Patients were divided into three groups: group 1 included 40 patients treated with intralesional injection of 0.1 mL PPD, group 2 included 50 patients treated with intradermal injection of 0.1 mL PPD in the right forearm, and group 3 included 20 patients as control group treated with intralesional injection of 0.1 mL normal saline. Treatment was given every two weeks, with a maximum of 10 injections for the whole treatment duration. Complete cure was comparable between the two groups receiving PPD injection (94.1% in group 1 and 96% in group 2), and the difference was not statistically significant. These findings suggest that PPD can provide an excellent clinical outcome for wart treatment through any approach. However, local site reaction should be considered when intradermal injection is performed on healthy, uninvolved skin.31
Prior Sensitization Status
All of the studies included in the present work were conducted in countries where BCG vaccination is mandatory: Egypt (22), India (20), Nepal (2), Iran (1), Iraq (1), Saudi Arabia (1), Pakistan (1), Malaysia (1), Philippines (1), and Indonesia (1); hence, these populations were expected to have developed immunity against M. tuberculosis. Considering this, several studies straightly proceed to treatment with PPD in the intervention group. In contrast, some others performed a PPD sensitization test prior to intervention.11,20,22,24,30,39,40,44,45,50,53–55,57
A study by Alajlan involving 82 patients with multiple common warts divided patients in the intervention group into two further different groups, namely those with positive and negative PPD skin tests. A skin test was done by injecting 0.1 mL PPD-5TU intradermally. The result was read 48 hours after injection, and induration of ≥5 mm was considered positive. This study revealed that 76% of patients who were PPD-positive and 82% of patients who were PPD-negative in the intervention group achieved clearance of one or more warts. Moreover, among the responders in the positive-PPD group, distant wart clearance was observed in 38% of patients, compared to 78% in the negative-PPD group. The result of this study suggested that a positive PPD skin test is not required to induce PPD efficacy.22
On the other hand, Sharquie et al reported that 10 out of the 14 responders in the intervention group were tuberculin-positive, and 13 out of 16 non-responders in the intervention group were tuberculin-negative, with a statistically significant difference. An intradermal injection of 0.1 mL PPD-2TU was used for the sensitization test. In this study, patients who tested positive for tuberculin skin test demonstrated better responses to PPD treatment. Furthermore, a better outcome was observed in patients with previous BCG vaccination, suggesting prior sensitization to M. tuberculosis bacilli.54 These variable findings called for further study regarding the effect of prior sensitization status on the treatment outcome of PPD.
Other Factors
Most studies found no statistically significant relationship between baseline characteristics of the study participants, such as age, duration, number, and type of warts, with the therapeutic response to PPD. However, Awad et al23 and Jaiswal et al38 reported younger age of patients among the good responders compared to the minimal or non-responders. The weaker immunological response with increasing age might cause this.11 Abd-Elazeim et al,16 Elela et al31 and Nada et al44 observed that longer-duration warts were less responsive to treatment. Abd Elazeim et al16 also reported that the mean size of warts was significantly higher in minimal and non-responders than in complete and partial responders. Mohta et al8 reported a negative correlation between the number of warts and treatment outcomes in which patients showing complete clearance had a mean of 9.13 lesions compared to 17.26 lesions in patients with moderate to no clearance. Jain et al37 reported that plane warts showed the optimal response to PPD, compared to palmoplantar and periungual warts, which best responded to MMR.
Comparative Studies
Comparison to Destructive Treatments
Cryotherapy is a commonly used destructive treatment option for warts. A study by Amirnia et al compared intralesional PPD to cryotherapy using liquid nitrogen spray in 3 freeze-thaw cycles with 2-week intervals and a maximum of 6 sessions. Complete clearance was achieved in 77.1% of participants in the PPD group compared to 18.2% in the cryotherapy group. Furthermore, the PPD group revealed less recurrence after six months of follow-up than the cryotherapy group (8.6% versus 24.2%, respectively).11 Studies by Fatima et al33 on 60 cutaneous warts patients, of which 30 patients were under treatment with cryotherapy (6 sessions), also reported comparable results with a clearance rate of 70% in the PPD group versus 30% in the cryotherapy group. Wan Ahmad et al57 reported a higher clearance rate in the PPD group than in the cryotherapy group (86.7% versus 73.3%, respectively) compared to other comparative studies. However, this study involved fewer participants. Awad et al compared the combination of PPD and cryotherapy to PPD only. In the cryo-immunotherapy group, a single freezing cycle of cryotherapy for four sessions was followed by intralesional injection of PPD on the most prominent wart. While the clearance rate was comparable between the two groups, combination treatment showed less recurrence than PPD monotherapy (0 versus 20%, respectively).23 Meanwhile, Moubasher et al43 compared a combination of PPD and cryotherapy to each treatment alone for AGWs. Cryotherapy was given in 3 freeze-thaw cycles for four sessions. The cryo-immunotherapy group showed the highest clearance rate compared to PPD or cryotherapy alone (46.7% versus 13.3% and 26.7%, respectively). However, higher AEs were also observed in this group, with blistering and hypopigmentation as the most significant AEs.43 Ibrahim et al36 reported an even higher complete clearance rate in patients receiving combination therapy of intralesional PPD and cryotherapy (84%) than both monotherapy alone (24% in the cryotherapy group and 48% in the PPD group), with only a single freeze-thaw cycle.
Comparison to Other Immunotherapies
Mycobacterium w Vaccine
Mycobacterium w vaccine contained killed nonpathogenic atypical mycobacterium belonging to Runyon Group IV, currently known as Mycobacterium indicus pranii.27 Mohta et al compared the efficacy of PPD to the Mw vaccine given intralesionally in 102 patients with extragenital warts. This study achieved complete clearance in 76.3% of patients in the Mw group and 65.9% of patients in the PPD group. No recurrence was observed during the six-month follow-up period. Besides a faster clearance rate, the Mw group demonstrates a better safety profile. Significant AEs like injection site granuloma, atypical mycobacterial infection, and generalized urticarial rash were reported in the PPD group.8 In contrast, similar research by Chandra et al, which compared PPD to the Mw vaccine injected intradermally on a deltoid region for extragenital warts, reported that 32 patients in the Mw group experienced indurated nodules following every injection that later healed with scarring. Of these, 12 patients reported significant pain requiring analgetic treatment with paracetamol 650 mg, given twice daily until resolution; 11 patients developed ulceration in the nodule, and four patients reported discharge leaking from the nodule.27 Another study by Mohta et al reported similar findings, with higher AEs in the Mw group compared to the PPD group. Severe AEs, including painful nodules, nodule site ulceration, and scarring, were observed only in the Mw group.42
Measles, Mumps, Rubella
A study by Shaheen et al compared PPD, MMR vaccine, and normal saline injected intralesionally on 30 patients with cutaneous and anogenital warts, given in 3-week intervals and a maximum of 3 sessions. Before treatment, sensitization tests were performed in both groups by intradermal injection of each antigen. Only responders were later included in the study.17 For the MMR group, treatment dose was determined based on criteria by Johnson et al.20 In contrast, in the PPD group, dosing was given according to criteria by Kus et al.13 This study reported the highest clearance rate in the MMR group compared to PPD and placebo (80% versus 60% and 0, respectively). No severe side effects nor recurrence were reported during the three-month follow-up in either group.17 Studies by Fawzy et al.34 Bhalala et al.25 Jain et al37 and Nofal et al47 reported similar results. However, the difference was not statistically significant in these studies.25,34,47 In contrast, a study by Ahmed et al21 reported a higher complete clearance rate in the PPD compared to the measles and rubella (MR) group (23.2% versus 9.3%, respectively). This finding follows a study by Sil et al19 in which the clearance rate was reported as 44.4% in the PPD group and 41.66% in the MMR group. Being composed of more than one antigen might explain the higher clearance rate observed in former studies in the MMR group. However, regarding the effect on distant warts, Shaheen et al17 and Mohammed et al41 reported a higher clearance rate in the PPD compared to the MMR group (60% versus 40%, respectively, in both studies). This might reflect the less systemic effect of MMR compared to PPD, implying that MMR might be better used to treat single warts or to be injected in each wart.17
Candida
Fawzy et al compared intralesional PPD to Candida antigen and MMR in 120 patients with multiple plane warts. Forty patients received 0.1 mL PPD, while another 40 patients were given 0.1 mL of 1/1000 solution of Candida antigen, both injected intralesionally on the most prominent wart, two weeks apart and continued until a maximum of 5 sessions. Seventy percent of patients in the Candida antigen group achieved complete clearance, compared to 55% in the PPD group. Adverse events were comparable between the Candida antigen and PPD group, with edema and erythema reported more frequently in the former.34 This finding aligns with Tawfik et al, in which complete clearance was observed in 85% of patients in the Candida antigen group compared to 72.5% in the PPD group. In this study, PPD-5TU and 1/1000 solution of Candida antigen were used. However, skin test results conducted previously determined the volume of solution injected.56 Similarly, Nofal et al compared intralesional PPD to Candida antigen and MMR in 150 patients with periungual warts. Before treatment, a sensitization test was done by injecting 0.1 mL of each antigen intradermally. Only responders were later included in the study. Unlike the former, this study used 0.1 mL of 1/100 solution of Candida antigen given to 50 patients. In comparison, another 50 patients were given 0.1 mL PPD. Both injections were given intralesionally on the most prominent wart, with 2-week intervals and a maximum of 5 sessions. Complete clearance was achieved in 80% of participants of the Candida antigen group, compared to 70% in the PPD group. Moreover, complete clearance of distant warts was also higher in the Candida antigen than in the PPD group (86.7% versus 70%, respectively).47 The ability to induce stronger local inflammatory reactions might explain Candida antigen’s relative superiority over PPD. Another explanation could be the higher sensitivity to Candida antigen brought on by the widespread exposure to candidal infection, particularly in the early years of life.34 Furthermore, Nofal et al46 conducted a randomized placebo-controlled clinical trial comparing intralesional PPD and Candida antigen alternatingly versus either agent alone towards 160 patients presenting with multiple common warts. Patients were assigned to 4 groups: group 1 received 0.1 mL of intralesional PPD, group 2 received 0.1 mL of 1/1000 solution of Candida antigen, group 3 received alternating therapy of PPD and Candida antigen, and group 4 received 0.1 mL normal saline (control group). Injections were given into the most prominent wart every two weeks for six group sessions. Complete clearance was observed in 70.6% of participants in the alternating therapy group, 61.1% in the PPD group, 36.8% in the Candida antigen group, and 8.6% in the regular saline group, with a statistically significant difference. The synergistic effect of both agents might explain the better outcome observed in the alternating therapy group. Each antigen may trigger the cell-mediated immune response through a separate pathway, therefore augmenting one another.46
Bacillus Calmette-Guerin
Bacillus Calmette-Guerin contained a live attenuated form of Mycobacterium bovis introduced as a prophylactic agent against tuberculosis and other mycobacterial infections.49,62 Podder et al conducted a double-blind, randomized controlled-trial comparing PPD to BCG in 60 patients with cutaneous warts. Thirty-three patients in the BCG group received 0.1 mL of BCG, while 27 patients in the PPD group received 0.1 mL of PPD-5TU. Both antigens were injected intradermally on the right arm. Treatment was given at a 4-week interval and a maximum of 3 sessions. In this study, both immunotherapies showed significant responses after four weeks onward.
Nonetheless, at the end of the study, complete clearance was achieved in 48.5% of patients in the BCG group compared to 18.5% of patients in the PPD group. This outcome might be explained by the more significant number of cross-reacting epitopes existing on the whole bacterial antigen of M. bovis than in PPD. However, AEs were also observed more frequently in the BCG group, including pain and abscess on the injection site, scar formation.49
Combination Antigen
Nofal et al compared the efficacy and safety of triple intralesional immunotherapy composed of PPD, Candida antigen, and MMR versus each agent alone in 160 patients with multiple cutaneous recalcitrant warts. Patients were randomly assigned into four groups: group A received 0.3 mL PPD, group B received 0.3 mL of 1/100 solution of Candida antigen, group C received 0.3 mL MMR, while group D received 0.3 mL combination of the three antigens (0.1 mL each, combined in the same syringe), injections were done intralesionally into the most prominent wart every two weeks, for a maximum of 5 sessions. Although both target and distant warts’ complete clearance was reported to be highest in the triple immunotherapy (77.5% and 65%, respectively), this effectiveness was not significantly different compared to other groups that received mono immunotherapy. There was also a statistically significant difference in AEs observed between all groups; the most common AE was pain during injection, which was observed in all groups. Although it is expected that triple immunotherapy activates different immune pathways induced by various microbial antigens and different vaccine natures, each of which acts on a certain arm of the immune response, resulting in robust stimulation of CMI. However, in this study, triple immunotherapy produced nonsignificant difference in effectiveness compared to monotherapy. It also has disadvantages, such as difficulty obtaining all three antigens simultaneously.48
Comparison to Other Treatments
Vitamin D3
Although the mechanism of action of vitamin D3 in the treatment of warts has not yet been fully understood, some have suggested that in addition to regulating cell proliferation and proliferation, it also exhibits immunoregulatory properties.63 It has been proposed that vitamin D3 can activate toll-like receptors on human macrophages, leading to increased expression and production of antimicrobial peptides and alteration of innate immunity.32,63 In a study by Farhana et al comparing PPD to vitamin D3 in 20 patients with cutaneous warts, the complete clearance rate was higher in the PPD compared to the vitamin D3 group (80% versus 70%, respectively). This study used 0.2 mL of 15 mg/mL (600.000) vitamin D3 and 0.2 mL of PPD-5TU, given intralesionally into each wart every two weeks until complete clearance was achieved. The number of sessions required to achieve complete clearance in the PPD group was 3–4 sessions compared to 6 sessions in the vitamin D3 group.32 Study by Jain et al37 also reported similar findings in which complete clearance was achieved in 85% of patients in the PPD group compared to 80% in the vitamin D3 group. In addition to complete clearance of injected warts, distant warts clearance was also higher in the PPD group, supporting its superiority in inducing systemic effects.17,37 On the contrary, Ahmed et al.21 Ghaly et al35 and Raveendra et al52 reported a higher complete clearance rate in the vitamin D3 group. However, a study by Ghaly et al35 demonstrated the more favourable effect of PPD in the clearance of distant warts compared to vitamin D3 (37.5% versus 25%, respectively).
Zinc
Zinc sulfate is hypothesized to work by modulating macrophage and neutrophil functions, NK cell/phagocyte activity, and different types of inflammatory cytokines. When injected intradermally, it causes significant infiltration of inflammatory cells, consisting of eosinophils followed by lymphocytes and fibroblasts, into the injection site. Awad et al compared the efficacy of PPD to zinc sulfate 2% in 120 pediatric warts patients. Patients were randomized into two groups; one group received 0.1 mL of PPD, while another received zinc sulfate 2%; treatment was given as an intralesional injection on the most prominent wart with two-week intervals and a maximum of 5 sessions. Despite the higher complete clearance rate in the zinc sulfate group, the PPD group demonstrated a better safety profile. Significant AEs were common in the zinc sulfate group, including pain (70%), inflammation (26.7%), ulceration (8.3%), and scars (16.7%), compared to only injection site itching (13.3%) in the PPD group. Furthermore, after six months of follow-up, recurrence was observed more frequently in the zinc sulfate group (10%) compared to the PPD group (1.7%).24
5-Fluorouracil
5-fluorouracil (5-FU) is an antimetabolite, a pyrimidine analogue that enhances the production of Th1 cytokines, activating the natural killer and cytotoxic cells to eliminate HPV. Durgadevi et al compared the efficacy of intralesional PPD using PPD-1TU and topical 5% 5-FU in 50 patients with periungual warts. The volume of PPD injected was determined by the size of the skin test reactivity conducted before treatment. In the PPD group, treatment was given in 3-week intervals with a maximum of 6 sessions. In contrast, topical 5% 5-FU was given under occlusion daily at night and left for 12 hours for three months. Complete clearance was significantly higher in the PPD group (88%) compared to the 5-FU group (20%). The different treatment approaches in each group may explain this finding. Patients in the PPD group received intralesional injections exclusively delivered by an investigator. In contrast, treatment in the 5-FU group was self-applied. Therefore, the results highly depended on the patient’s motivation and adherence to the treatment protocol. Moreover, faster time to resolution was observed in the PPD group compared to the 5-FU group (6.6 weeks versus 9.8 weeks, respectively). No AE was reported in the PPD group, while 8% of patients in the 5-FU group reported paronychia, erythema, and itching.29
Isotretinoin
Retinoids are known to promote the proliferation of basal cells and the number of cells expressing differentiation markers like involucrin, loricrin, filaggrin, and epidermal transglutaminase, which results in increased epidermal desquamation. Oral retinoids also demonstrate an anti-angiogenic mechanism by inhibiting vascular endothelial growth factor synthesis by keratinocytes, causing clearance of angiogenesis-dependent warts. Furthermore, it is also known as a potent immunomodulator capable of inducing apoptosis and suppressing viral transcription in the affected keratinocytes. Diab et al conducted a randomized clinical trial in which low-dose oral tretinoin combined with intralesional PPD was compared to PPD monotherapy for treating multiple common warts. Forty patients were equally divided into two groups. One group received 0.1 mL of intralesional PPD and an oral placebo given to the most prominent wart every two weeks for a maximum of 6 sessions. In contrast, another group received intralesional PPD, as previously mentioned, plus low-dose isotretinoin (0.2–0.4 mg/kg/day) for three months. Complete clearance was achieved in 35% of patients in the PPD monotherapy group and 55% in the combination group. Nevertheless, the difference was statistically insignificant. This finding might be explained by the dose of isotretinoin in this study, which may not have been high enough to create a potent synergistic effect and preserve the immune response after PPD injection. Beside cheilitis and dry skin, which was more pronounced in the combination group, other side effects were comparable between both groups. In this study, the low-dose isotretinoin did not add a therapeutic value for treating common warts.28
Conclusion
PPD immunotherapy demonstrated promising efficacy and safety in treating cutaneous and anogenital warts, including in the pediatric population. Although previous research on PPD showed good efficacy and safety profile in treating AGWs in pregnant women, a comparison study with other modalities has not been done, which needs to be confirmed in future research. Clearance of distant, uninjected warts provides an additional benefit of PPD, particularly in cases involving multiple lesions and challenging locations. These studies were performed in countries with prevalent tuberculosis infection, and BCG vaccination is obligatory. Therefore, it sensitized such population to M. tuberculosis, and the subsequent wart treatment with PPD injection may result in easier stimulation of CMI responses. However, for this reason, the result of our study is not yet applicable to the general population.
Furthermore, trials studying the effect of prior sensitization status on treatment response still demonstrated inconsistent results. Intralesional and injection from distant sites showed comparable results. Variable treatment outcomes demonstrated in these studies may be related to the difference in dosing, interval, and frequency of treatments. Therefore, clinical trials with larger sample sizes are needed to determine the optimal dosing and frequency of treatment to standardize the treatment protocols, also adding into consideration countries in which the prevalence of tuberculosis is low. Studies with longer follow-up duration are also necessary to further evaluate recurrences and long-term AEs. Comparative studies showed comparable results with other immunotherapies. Future research on combination therapy of currently available procedural therapy such as electrocautery with PPD injection and both the effectiveness and safety on special populations such as the elderly, immunocompromised individuals, those on immunosuppressants, and patients with HIV or autoimmune diseases can be considered.
Acknowledgments
Part of this paper was presented at the 25th World Congress of Dermatology 2023 as a conference talk with interim findings. The abstract was published in “Free Communication Abstracts” in the sexually transmitted infections and HIV section of the conference abstract book, which can be accessed online via https://www.wcd2023singapore-abs.org/abstract_details.php?aid=2050.
The authors would like to thank the Dermatology and Venereology Department staff, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fields JR, Saikaly SK, Schoch JJ. Intralesional immunotherapy for pediatric warts: a review. Pediatr Dermatol. 2020;37(2):265–271. doi:10.1111/pde.14094
2. Aldahan AS, Mlacker S, Shah VV, Kamath P, Alsaidan M, Samarkandy S. Efficacy of intralesional immunotherapy for treating warts: a review of the literature. Dermatol Ther. 2016;29(3):197–207. doi:10.1111/dth.12352
3. Ju HJ, Park HR, Kim JY, Kim GM, Bae JM, Lee JH. Intralesional immunotherapy for non-genital warts: a systematic review and meta-analysis. Indian J Dermatol Venereol Leprol. 2022;88(6):724–737. doi:10.25259/IJDVL_1369_20
4. Diab N, Atef H, Salah E. Intralesional injection of purified protein derivative in the treatment of viral warts: a pilot study. Egypt J Hosp Med. 2021;85(1):3198–3201. doi:10.21608/ejhm.2021.195432
5. Gilson R, Nugent D, Werner RN, Ballesteros J, Ross J. 2019 IUSTI-Europe guideline for the management of anogenital warts. J Eur Acad Dermatol Venereol. 2020;34(8):1644–1653. doi:10.1111/jdv.16522
6. Kanchana L, Thammarucha S, Suchinwanitnit P, Rutnin S. A comprehensive review of treatment options for recalcitrant nongenital cutaneous warts. J Dermatol Treat. 2022;33(1):23–40. doi:10.1080/09546634.2020.1737635
7. Sindhuja T, Bhari N, Gupta S. Asian guidelines for condyloma acuminatum. J Infect Chemother. 2022;28(7):845–852. doi:10.1016/j.jiac.2022.03.004
8. Mohta A, Sharma MK, Kumari P, Ghiya BC, Mehta RD. An intention-to-treat-analysis of the efficacy of immunotherapy using Mycobacterium w vaccine and purified protein derivative of tuberculin for warts with assessment of improvement in quality of life. Dermatol Pract Con. 2022;12(2):1–7.
9. Obbus SFV, Barit JJG, Yap-silva C. Efficacy of intralesional purified protein derivative for cutaneous warts: a meta-analysis. Acta Med Philipp. 2019;53(4):360–368. doi:10.47895/amp.v53i4.37
10. Yang H, Kruh-Garcia N, Dobos K. Purified protein derivatives of tuberculin - past, present, and future. FEMS Immunol Med Microbiol. 2012;66(3):273–280. doi:10.1111/j.1574-695X.2012.01002.x
11. Amirnia M, Khodaeiani E, Fouladi DF, Masoudnia S. Intralesional immunotherapy with tuberculin purified protein derivative (PPD) in recalcitrant wart: a randomized, placebo-controlled, double-blind clinical trial including an extra group of candidates for cryotherapy. J DermatolTreat. 2016;27(2):173–178. doi:10.3109/09546634.2015.1078871
12. Choudhary D, Piya S. Treatment of warts by immunotherapy using purified protein derivative. Birat J Heal Sci. 2018;3(2):463–467. doi:10.3126/bjhs.v3i2.20961
13. Kus S, Ergun T, Gun D, Akin O. Intralesional tuberculin for treatment of refractory warts. J Eur Acad Dermatol Venereol. 2005;19(4):515–516. doi:10.1111/j.1468-3083.2004.01176.x
14. Mishra A, Shrestha S, K.c. S, Karn D. A prospective clinical study for safety and efficacy of intralesional tuberculin purified protein derivative in treatment of palmoplantar verruca. J Nobel Med Coll. 2022;11(1):12–16. doi:10.3126/jonmc.v11i1.45720
15. Azab M, El-shabrawy MM, Nafea ER, Nada HA. Measurement of serum interleukin 17 level in patients with genital warts before and after intralesional tuberculin injection. J Men’s Health. 2021;18(1):1.
16. Abd-Elazeim FMA, Mohammed GFA, Fathy A, Mohamed RW. Evaluation of IL-12 serum level in patients with recalcitrant multiple common warts, treated by intralesional tuberculin antigen. J DermatolTreat. 2014;25(3):264–267. doi:10.3109/09546634.2013.768760
17. Shaheen MA, Salem SAM, Fouad DA, El-Fatah AAA. Intralesional tuberculin (PPD) versus measles, mumps, rubella (MMR) vaccine in treatment of multiple warts: a comparative clinical and immunological study. Dermatol Ther. 2015;28(4):194–200. doi:10.1111/dth.12230
18. Abou-Taleb DAE, Abou-Taleb HA, El-Badawy O, Ahmed AO, Hassan AET, Awad SM. Intralesional vitamin D3 versus intralesional purified protein derivative in treatment of multiple warts: a comparative clinical and immunological study. Dermatol Ther. 2019;32(5):1–6. doi:10.1111/dth.13034
19. Sil A, Dasgupta S, Chandra S, Datta A, Banerjee A, Das NK. Changes in cytokine profile with immunotherapy in viral warts using purified protein derivative, mumps measles rubella vaccine, and Mycobacterium w vaccine. Indian J Dermatol. 2021;66(1):67–73. doi:10.4103/ijd.IJD_206_20
20. Johnson S, Roberson P, Horn T. Intralesional injection of mumps or Candida skin test antigens: a novel immunotherapy for warts. Arch Dermatol. 2001;137(4):451–455.
21. Ahmed R, Bhadbhade SP, Noojibail B, Shetty SM, Varghese A. Comparative study in efficacy and safety of intralesional injections of vitamin D3, measles rubella (MR) vaccine, and purified protein derivative (PPD) in the management of cutaneous warts. J Cutan Aesthet Surg. 2020;13(4):326–332. doi:10.4103/JCAS.JCAS_39_20
22. Alajlan A. Intra-lesional injection of tuberculin skin test antigens as an immunotherapy for warts: open label placebo controlled clinical trial. Medical Science. 2020;24:105.
23. Awad SM, Gomaa AS, Hassan HA, Tawfik YM. Efficacy of cryotherapy combined with intralesional tuberculin purified protein derivative (PPD) versus intralesional tuberculin PPD monotherapy in the treatment of multiple common warts. Dermatol Ther. 2022;35(4):1–14.
24. Awad A, Ismael AF, Sallam M, Abdelgaber S. Intralesional purified protein derivative versus zinc sulfate 2% in the treatment of pediatric warts: clinical and dermoscopic evaluation. J Cosmet Dermatol. 2022;21(10):4637–4645. doi:10.1111/jocd.14876
25. Bhalala K, Poojary S, Shah K. Comparative study of efficacy of intralesional purified protein derivative (PPD) versus intralesional measles, mumps, and rubella (MMR) vaccine in management of multiple viral warts. J Cutan Aesthet Surg. 2021;14(4):397. doi:10.4103/JCAS.JCAS_166_19
26. Bhargava S, Kumar U. Purified protein derivative (PPD) as immunotherapy for warts: how effective is it? Australas J Dermatol. 2019;2019:1.
27. Chandra S, Sil A, Datta A, Pal S, Das NK. A double-blind, randomized controlled trial to compare the effectiveness and safety of purified protein derivative of tuberculin antigen with Mycobacterium w vaccine in the treatment of multiple viral warts. Indian J Dermatol Venereol Leprol. 2019;85:355–366. doi:10.4103/ijdvl.IJDVL_549_18
28. Diab N, Atef H. Comparative efficacy of using a combination of intralesional purified protein derivative with low dose isotretinoin in the treatment of recalcitrant common warts. Dermatologic Therapy. 2022;2022:1–8.
29. Durgadevi S, Shridharan P. Treatment of periungual warts: comparison of topical 5 % 5-fluorouracil and intralesional purified protein derivative in a South Indian teaching hospital. Int J Res Dermatol. 2018;4(4):574–578. doi:10.18203/issn.2455-4529.IntJResDermatol20184464
30. Eassa BI, Abou-Bakr AA, El-Khalawany MA. Intradermal injection of PPD as a novel approach of immunotherapy in anogenital warts in pregnant women. Dermatol Ther. 2011;24(1):137–143. doi:10.1111/j.1529-8019.2010.01388.x
31. Elela IMA, Elshahid AR, Mosbeh A. Intradermal vs intralesional purified protein derivatives in treatment of warts. Golf J Deramatol Venereol. 2011;18(2):21–26.
32. Farhana K, Asia AJ. Comparative study of therapeutic efficacy of intralesional vitamin D3 versus intralesional purified protein derivative in the treatment of warts. Int J Sci Res. 2020;4(3):226–231.
33. Fatima SM, Ejaz A, Anwar A. Comparison of efficacy of intralesional purified protein derivative (PPD) with cryotherapy in the treatment of cutaneous warts. Pakistan Armed Forces Med J. 2019;69(5):965–970.
34. Fawzy MM, Nofal A, Alakad R. Intralesional antigen immunotherapy for the treatment of plane warts: a comparative study. Dermatol Ther. 2020;33(6). doi:10.1111/dth.13807
35. Ghaly NE, El-Ashmawy AA, Abou Zeid M, Shaker ESE. Efficacy and safety of intralesional injection of vitamin D3 versus tuberculin PPD in the treatment of plantar warts: a comparative controlled study. J Cosmet Dermatol. 2021;20(4):1231–1240. doi:10.1111/jocd.13712
36. Ibrahim H, El Taieb M, Nada E, Kamal E. Combined intralesional injection of tuberculin purified protein derivative plus cryotherapy versus each alone in the treatment of multiple common warts. Dermatologic Therapy. 2022;2022:1–6.
37. Jain S, Marfatia YS. A comparative study of intralesional vitamin D3, measles mumps rubella vaccine, and tuberculin purified protein derivative in the treatment of recalcitrant warts: an approach to solve a therapeutic conundrum. J Clin Aesthet Dermatol. 2021;14(11):26–34.
38. Jaiswal A, Gupta K, Sharma RP, Bedi G. Immunotherapy with PPD in treatment of warts: an open labelled study from western Uttar Pradesh. Indian J Clin Exp Dermatol. 2019;5(1):41–45. doi:10.18231/2581-4729.2019.0010
39. Kaimal S, Gopinath H, Premalatha V. Intralesional immunotherapy with purified protein derivative (PPD) for cryotherapy-resistant warts. Int J Dermatol. 2020;59(6):726–729. doi:10.1111/ijd.14839
40. Milante RR, Venida-Tablizo A, King-Ismael D. Efficacy and safety of single versus multiple intralesional immunotherapy with purified protein derivative (PPD) in the treatment of multiple verruca vulgaris. Int J Dermatol. 2019;58(12):1477–1482. doi:10.1111/ijd.14652
41. Mohammed YF, Ibrahim HS, Elbarbary MA, Elsaie ML. Comparative study of intralesional tuberculin protein purified derivative (PPD) and intralesional measles, mumps, rubella (MMR) vaccine for multiple resistant warts. J Cosmet Dermatol. 2020;2020:1–7.
42. Mohta A, Jain SK, Mehta RD, Arora A. Intralesional purified protein derivative of tuberculin versus intralesional Mycobacterium w vaccine in treatment of recalcitrant extragenital warts: a randomized, single-blinded, comparative study. Indian J Dermatol. 2018;63(2):125–130. doi:10.4103/ijd.IJD_585_17
43. Moubasher AA, Kolta M, Gaber H. Tuberculin purified protein derivative and cryotherapy in the treatment of genital warts: a randomized controlled trial. Hum Androl. 2021;11(11):1–6. doi:10.21608/ha.2021.61492.1075
44. Nada HA, El-Shabrawy MM, Ibrahim SH, Azab M. Measurement of serum glutathione peroxidase, catalase and superoxide dismutase concentration in patients with external anogenital warts before and after treatment with intralesional tuberculin purified protein derivative. Andrologia. 2020;52(9):1–6. doi:10.1111/and.13661
45. Nimbalkar A, Pande S, Sharma R, Borkar M. Tuberculin purified protein derivative immunotherapy in the treatment of viral warts. Indian J Drugs Dermatol. 2016;2(1):19. doi:10.4103/2455-3972.184103
46. Nofal A, Yehia E, Khater E, Bessar H. Alternating intralesional purified protein derivative and Candida antigen versus either agent alone in the treatment of multiple common warts. J Am Acad Dermatol. 2020;83(1):208–210. doi:10.1016/j.jaad.2020.01.054
47. Nofal A, Alakad R, Fouda I, Fawzy MM. Intralesional antigen immunotherapy in the treatment of periungual warts. J Cutan Med Surg. 2021;25(3):286–292. doi:10.1177/1203475420988859
48. Nofal AA, Elkholy BM, Abd-Elmonsef ER, Nofal HO. Triple intralesional antigen immunotherapy versus monoantigen in the treatment of multiple recalcitrant warts. Dermatol Ther. 2022;12(5):1225–1237. doi:10.1007/s13555-022-00725-x
49. Podder I, Bhattacharya S, Mishra V, Sarkar TK, Chandra S, Sil A. Immunotherapy in viral warts with intradermal Bacillus Calmette-Guerin vaccine versus intradermal tuberculin purified protein derivative: a double-blind, randomized controlled trial comparing effectiveness and safety in a tertiary care center in Eastern India. Indian J Dermatol Venereol Leprol. 2017;83(3):411. doi:10.4103/0378-6323.193623
50. Pundir M, Singh K, Kanodia S. Efficacy of tuberculin purified protein derivative (PPD) in the treatment of plane warts on face. Medpulse Int Med J. 2018;9(1):71–75. doi:10.26611/10219117
51. Puri N. A study on the efficacy of immunotherapy with purified protein derivative for the treatment of recalcitrant warts. Int J Curr Res. 2019;2019:3–5.
52. Raveendra L, Raju B, Dharam KKC, Mohan V, Yadav K. Comparison of purified protein derivative and vitamin D in the treatment of recalcitrant warts. Clin Dermatology Rev. 2021;5(1):54. doi:10.4103/CDR.CDR_51_20
53. Saoji V, Lade NR, Gadegone R, Bhat A. Immunotherapy using purified protein derivative in the treatment of warts: an open uncontrolled trial. Indian J Dermatol Venereol Leprol. 2016;82(1):42–46. doi:10.4103/0378-6323.171650
54. Sharquie KE, Al-Rawi JR, Noaimi AA, Majly WH. Tuberculin as intralesional therapy for viral warts—single-blind, split, placebo, controlled study. J Cosmet Dermatological Sci Appl. 2016;06(05):191–198.
55. S G, Kumar A. Intralesional immunotherapy with purified protein derivative antigen in the treatment of multiple cutaneous warts: an open label study in an urban teaching hospital. Int J Res Dermatology. 2020;6(6):739. doi:10.18203/issn.2455-4529.IntJResDermatol20204436
56. Tawfik NZ, Eyada MM, El Hamid REA, Halim HM. Intralesional injection of purified protein derivative versus Candida antigen in treatment of genital warts. Dermatol Ther. 2022;35(10):e15762. doi:10.1111/dth.15762
57. Wan Ahmad Kammal W, Jamil A, Md Nor N. Efficacy and safety of intralesional tuberculin purified protein derivative versus cryotherapy in the treatment of warts: an assessor-blinded, randomized controlled trial. Dermatologic Therapy. 2021;2021:10–15.
58. Achdiat PA, Antariksa NC, Rowawi R, Suwarsa O, Hidayat YM, Dwiyana RF. The success of intralesional purified protein derivative immunotherapy in the treatment of anogenital warts: a case report. J Exp Pharmacol. 2022;14:131–135. doi:10.2147/JEP.S347241
59. Alhashmi S, Sadek A. Case report: successful treatment of giant condyloma acuminata with intralesional injection of purified protein derivative. Open Dermatol J. 2021;15(1):36–38. doi:10.2174/1874372202115010036
60. Manoj S, Manjunath P, Mallikarjun M. A study to assess the efficacy of intradermal purified protein derivative (PPD) in treatment of multiple warts. Paper Presented in 24th World Congress of Dermatology, Milan, Italy. 2019. https://www.wcd2019milan-dl.org/abstract-book/documents/late-breaking-abstracts/26-medical-therapies-pharmacology/a-study-to-assess-the-55.pdf.
61. Nofal A, Fouda I. Switching between intralesional antigens: a promising therapeutic approach for recalcitrant warts. JAAD Case Rep. 2020;6(10):1032–1035. doi:10.1016/j.jdcr.2020.07.045
62. Al Hamzawi NK, Abdallah MH. Managing recalcitrant warts: facts about Bacillus Calmette-Guerin (BCG), Mycobacterium indicus pranii (Mw vaccine), and purified protein derivative (PPD) as immunotherapy. J cosmet dermatol sci appl. 2018;2018:218–235.
63. Aktaş H, Ergin C, Demir B, Ekiz Ö. Intralesional vitamin D injection may be an effective treatment option for warts. J Cutan Med Surg. 2016;20(2):118–122. doi:10.1177/1203475415602841
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
A Case of Genital and Extragenital Warts Unresponsive to Immunotherapy Using Measles, Mumps, Rubella Vaccine
Achdiat PA, Yunitasari, Usman HA, Maharani RH
International Medical Case Reports Journal 2023, 16:739-746
Published Date: 15 November 2023
