Back to Journals » Journal of Pain Research » Volume 16
Effects of Hyperbaric and Isobaric Bupivacaine on Hemodynamic Profiles and Block Characteristics Among Parturients Undergoing Elective Cesarean Section Under Spinal Anesthesia: A Randomized Controlled Trial
Authors Besha A, Zemedkun A, Tadesse M , Hailu S , Mossie A , Shiferaw A , Angasa D, Adamu Y
Received 7 August 2023
Accepted for publication 13 October 2023
Published 20 October 2023 Volume 2023:16 Pages 3545—3558
DOI https://doi.org/10.2147/JPR.S428314
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ellen M Soffin
Aschalew Besha,1 Abebayehu Zemedkun,2 Muhiddin Tadesse,2 Seyoum Hailu,2 Addisu Mossie,1 Adanech Shiferaw,1 Dugo Angasa,1 Yayeh Adamu2
1Department of Anesthesia, College of Health Sciences and Medicine, Hawassa University, Hawassa, Ethiopia; 2Department of Anesthesiology, College of Health Sciences and Medicine, Dilla University, Dilla, Ethiopia
Correspondence: Abebayehu Zemedkun, Department of Anesthesiology, College of Health Sciences and Medicine, Dilla University, Dilla, Ethiopia, Email [email protected]
Background: Cesarean section (CS) is a surgical procedure where the baby is delivered through incisions made in the abdomen and uterus. Bupivacaine is a widely recognized local anesthetic available in different baricity and it is frequently used for spinal anesthesia. The baricity of bupivacaine impacts hemodynamic profiles and block characteristics.
Objective: To compare the effects of hyperbaric and isobaric bupivacaine on hemodynamic profiles and block characteristics among parturients undergoing elective cesarean section under spinal anesthesia at Dilla University Referral Hospital.
Methods: 64 pregnant mothers scheduled for elective cesarean section under spinal anesthesia were randomly assigned to two groups: Group A received a dose of 12.5 mg of isobaric bupivacaine (n = 32), Group B received a dose of 12.5 mg of hyperbaric bupivacaine (n = 32). Prior to conducting the study, the necessary ethical approvals were obtained. For comparing numerical variables between the two groups, the independent Sample t-test or Mann–Whitney U-test was employed as needed. Repeated measurements were analyzed using mixed ANOVA. Categorical variables were assessed using either the chi-square test or Fisher’s exact test. Statistical significance was set at P < 0.05, with a power of 90%.
Results: The mean Systolic Blood Pressure (SBP), Diastolic Blood pressure (DBP), and Mean Arterial Blood Pressure (MAP) showed significant decrement in the group receiving isobaric spinal anesthesia compared to those receiving hyperbaric bupivacaine. The decrement was observed from the 6th to 30th minute (p< 0.05). Furthermore, the hyperbaric group had a faster onset time for achieving the maximum sensory block, with a median time of 3 (1) min compared to 4 (2) mins in the isobaric group (p< 0.001).
Conclusion and Recommendation: We conclude that hyperbaric bupivacaine provides stable intraoperative hemodynamic parameters and an earlier onset of block than isobaric bupivacaine. Therefore, we recommend clinicians to use hyperbaric bupivacaine for cesarean delivery.
Keywords: block characteristics, hemodynamics, isobaric bupivacaine, hyperbaric bupivacaine, cesarean section, spinal anesthesia
Introduction
Cesarean section is a surgical procedure where the baby is delivered through incisions made in the abdomen and uterus, is the most common obstetric surgery performed worldwide.1 Despite the World Health Organization’s recommended rate, the global rate of cesarean sections is increasing.2 The most recent available data from the global health report on cesarean section rates (2010–2018) from 154 countries reported the global cesarean section rate as 21.1%. The study also revealed that the rate of rate of CS in Africa in general and Sub- Saharan Africa) was 9.2% (95% CI: 5.2 to 13.2) and 5.0 (95% CI: 3.5 −6.6), respectively.3
The demographic health survey in 2014 found that the cesarean section rate in Addis Ababa was 22%, which was higher than the WHO recommendation of 10–15%.4 A systematic review and meta-analysis study done in 2020 in Ethiopia showed that cephalopelvic disproportion was the most common indication for cesarean section, followed by non-reassuring fetal heart rate pattern and obstructed labor.5
Spinal anesthesia is a form of neuraxial regional anesthesia achieved by injecting small doses of local anesthetics into the subarachnoid space.6 Post-spinal hypotension among parturients undergoing elective cesarean section under spinal anesthesia was estimated to be 80–90%, which is higher than that of the general population (25–75%) worldwide.7 A study in New York among 919 singleton term pregnancies undergoing elective CS under spinal anesthesia showed decrements in maternal blood pressure by 30–50% from baseline.8 In Ethiopia, at Gandi Memorial Hospital, the magnitude of post-spinal hypotension among parturients who underwent cesarean section was reported as 64%.9
Due to hormonal changes, compression of the inferior vena cava by a larger uterus, increased susceptibility to the effects of sympathectomy due to decreased sensitivity to endogenous vasoconstrictors, and other factors, this condition is particularly severe in pregnant women. This physiological alteration raises the pressure of cerebrospinal fluid (CSF) in the lumbosacral region, which causes local anesthetic drugs to spread cephalad.10
Technical factors such as block level above T5, baricity of the local anesthetics (the ratio of the density of local anesthetics (LAs) and cerebrospinal fluid (CSF)and high-dose regional anesthesia were linked to an increased risk of hypotension following spinal anaesthesia in addition to physiological alterations during pregnancy.11
Bupivacaine is a well-known amide type local anesthetic in isobaric and hyperbaric forms, commonly used during spinal anesthesia for caesarean section. Dextrose-free bupivacaine is isobaric whereas dextrose-containing bupivacaine is hyperbaric. The differences in the baricity of bupivacaine are believed to affect hemodynamic parameters and block characteristics. In addition, such baricity differences affect the extent, onset, and duration of sensory and motor blockade.12,13 Delayed motor and sensory block onset increases the time that a pregnant mother is in the supine position without delivering the baby which in turn increases aortocaval compression and the risk of hypotension. Severe hypotension during CD is associated with decreased uteroplacental blood flow, which may cause fetal hypoxia and acidosis, respiratory depression, nausea and vomiting, and cardiac arrest.14
Various strategies have been implemented to reduce post-spinal induced hypotension in women undergoing cesarean section. These methods include administering a small dose of bupivacaine, decreasing the amount of local anesthetic and combining it with additives like neuraxial opioids, preloading intravenous fluids, co-loading, adopting a left lateral tilt position, elevating the legs, and using vasopressors as a preventive measure. Despite these efforts, the occurrence of post-spinal hypotension remains significant.14–16
Different randomized controlled studies have been carried out to compare the effects of hyperbaric bupivacaine and isobaric bupivacaine on hemodynamics, as well as the extent and timing of sensory and motor block, in women undergoing elective cesarean section. Some of the studies indicate that hyperbaric bupivacaine leads to reduced post-spinal hypotension and a quicker achievement of maximum sensory and motor block compared to isobaric bupivacaine.16–18 Other studies found minimal post-spinal hypotension and a faster onset of block in the isobaric bupivacaine group than in the hyperbaric bupivacaine group.18,19 This controversy calls for a well-designed study to compare the two groups in terms of their effects on hemodynamic profiles and block characteristics.
This study aids in the selection of bupivacaine with minimal hemodynamic instability during cesarean sections. It also helps to select drugs with a faster onset of maximum sensory and motor blocks, which can shorten the duration of spinal anesthesia induction to skin incision time. Therefore, the aim of this study was to compare the effects of isobaric and hyperbaric bupivacaine on hemodynamic profiles and block characteristics (specifically onset of maximum sensory block, onset of maximum motor block and level of sensory block) among parturients undergoing cesarean section.
Materials and Methods
Study Design, Area and Period
A double-blinded randomized controlled trial was conducted from February 10, 2022, to June 10, 2022 at Dilla University teaching Hospital.
Eligibility Criteria
The study included pregnant women with a singleton pregnancy, classified as American Society of Anesthesiologists (ASA) class II, aged 18–45, and with a body mass index (BMI) of 30 kg/m2 or lower and scheduled for elective cesarean delivery. Pregnant women with systemic diseases such as renal impairment, chronic liver disease, known diabetes, pre-existing neurological disease, hypothyroidism, hyperthyroidism, placental abruption, placenta previa, hypertensive disorders of pregnancy (pre-eclampsia, eclampsia), as well as those with twin pregnancies, were excluded from the study.
Ethical Approval
This study was conducted in accordance with declaration of Helsinki. To conduct the study, ethical clearance was obtained from the institutional review board of college of health sciences and medicine (Protocol Unique No: 047/22-02). Written informed consent for participation was obtained from all patients. The study was registered in a pan-African clinical trial with the unique identification number PACTR- 202205836867776. Furthermore, the study was reported following CONSORT guidelines for clinical trials (Figure 1).
 |
Figure 1 Consort flow diagram of patients enrollment. Notes: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000251Citation: Schulz KF, Altman DG, Moher D, for the CONSORT Group (2010) CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med 7(3):e1000251. https://doi.org/10.1371/journal.pmed.1000251. |
Sample Size and Sampling Procedure
The sample size was calculated based on previous studies conducted in Iran, which showed a significant reduction in mean systolic blood pressure with sustained duration for the isobaric vs hyperbaric groups.20 We use N1= 42, µ1=7.8, SD1= 1.6 for isobaric bupivacaine group and N2= 42, µ2= 12.5, SD2=7.4 for the hyperbaric group. (Where N1=total population, µ1=mean, SD2= standard deviation in the isobaric group and N2=total population, µ2= mean, SD2=standard deviation in the hyperbaric group. Using a power of 90% and alpha 0.05, the sample size was calculated using a prior power analysis with G Power 3.1.9.7 software to be 58. An additional 10% was added to the enrollment to offset potential dropouts, assuming a balanced design. The total sample size was 64, with 32 participants in each group.
One hundred thirty (130) pregnant mothers underwent elective caesarean sections under spinal anesthesia, according to a situational analysis with exclusion criteria performed at the Dilla University Referral Hospital within the previous four months. Based on our inclusion criteria, there was a 50% chance that every patient during the data collecting period would be a study subject. We used a systematic random sampling method based on the order of the elective surgery schedules to select each patient one after the other to create a sample size of 64 patients. From among the anticipated 130 or more parturients during our data collecting period, the first case was picked at random until the necessary sample size was reached.
Operational Definition
Onset of maximum sensory block: the total time from the completion of the study drug injection until the patient did not feel the pinprick.
Onset of maximum motor blockage: the time taken from injection of the study drug (0 minutes) until the patient attained bromage scale> II.
The Modified Bromage scale is a criterion used for examining skeletal muscle strength, which is rated as zero = no paralysis, one = only able to move the knee, two = only able to move feet, and three = inability to move the leg or knee.21
The level of sensory block is assessed bilaterally in the anterior axillary line or mid-clavicular line for loss of sharp sensation to pinprick or cold.
Post-spinal hypotension: a drop in systolic blood pressure of more than 20–30% from baseline after local anesthesia administration into the subarachnoid space.22
Randomization and Blinding
Prior to allocation, a clear explanation of the procedure and assessments of motor and sensory blocks were provided to the parturients. They were randomized to either the isobaric or hyperbaric bupivacaine groups. Simple randomization was conducted by drawing one of the levels from a sealed envelope containing A or B, where A represents the isobaric group and B represents the hyperbaric group. For blinding purposes, study participants and data collectors were blinded to what was given. Allocation concealment was verified by sequential labeling and sealing of the envelope.
Data Collection and Anesthesia Protocol
The data for the study was collected from patient medical charts, vital sign charts, and monitors. Information about the study’s objectives, benefits, and potential harm was prepared in English and then translated into Amharic. The information was explained to the study participants. The data collection process involved four trained data collectors and one supervisor. The primary outcome variable of the study was the effect of isobaric and hyperbaric bupivacaine on the hemodynamic profiles of the parturients. Secondary outcome variables included comparisons of the sensory block level and the onset of maximum sensory and motor block between the two groups. Informed consent was obtained from the participants the night before their surgery. The parturients followed specific fasting guidelines, refraining from solid food for eight hours and clear fluids for two hours before surgery. On the morning of surgery, the parturients received premedication through intravenous administration of cimetidine (200 mg), metoclopramide (10 mg), and dexamethasone (4 mg), 30 minutes prior to undergoing spinal anesthesia. Standard monitoring procedures, including non-invasive blood pressure (NIBP), electrocardiogram (ECG), and pulse oximetry, were applied in the operating room. Patients received a preload of isotonic fluid at a rate of 10–15 mL/kg before the administration of spinal anesthesia. The bupivacaine solution used was freshly prepared in a labeled 5cc syringe with a sterile protocol. The drugs were prepared by an anesthetist who was not involved in the study. Baseline blood pressure and heart rate measurements were taken immediately before the administration of spinal anesthesia.
The anesthetist instructed the parturient to sit after setting up the equipment. At the proposed spinal injection site, skin infiltration with 2% lidocaine solution (2 mL) was carried out after aseptic procedures involving iodine and alcohol. Using 24G spinal needles, a lumbar puncture was performed between the L3-L4 spaces while the patient was sitting. 12.5 mg of 0.5% isobaric bupivacaine was injected intrathecally into group A after the accurate needle placement had been confirmed by the free flow of CSF, and 12.5 mg of 0.5% hyperbaric bupivacaine was given to group B for 10–15 seconds. Time zero was the point at which the local anesthetic injection into the subarachnoid space was completed. A senior anesthetist participated in the administration of anesthesia to reduce bias in the rate of injection. The primary end point of the study was to compare the effect of isobaric and hyperbaric bupivacaine on maternal hemodynamic profile among parturients undergoing elective cesarean section under spinal anesthesia.
After administering spinal anesthesia, the pregnant woman was positioned on her back with a pillow supporting her shoulder. Maternal blood pressure (systolic, diastolic, mean arterial pressure) and heart rate were monitored and recorded. The level of sensory block was assessed by gently applying an alcohol swap or pricking with a pin, while degree of motor function was evaluated using a modified bromage scale. This assessment continued until both complete sensory and motor blocks were achieved. Once the sensory block reached a level above the 10th thoracic vertebrae (T10) and the bromage scale indicated a motor block of at least level 2, a surgical incision was made.
After complete sensory (>T10) and motor (Bromage score>II) block, a skin incision was made. Hemodynamic monitoring was continued. Hemodynamic parameters were made at two-minute intervals initially for the first ten minutes, then at five-minute intervals until the end of the procedure. Despite continued fluid management, if MAP is <65 mmHg or SBP < 90 MAP vasopressor treatment was considered. The protocol for the management of hypotension and other complications were prepared before the start of the study. An uterotonic agent was administered immediately after delivery based on a protocolized uterotonic administration strategy. The intraoperative estimated blood loss and fluid requirements were also documented. Parturients were transferred to the PACU with stable vital signs at the end of the procedure.
During recovery, parturients’ vital signs (BP, HR, and SPO2) were monitored. After all vital signs stabilized, the parturient was transferred to the obstetric ward.
Data Processing and Analysis Procedure
SPSS version 26 was employed to analyze the collected data. Normality checks were conducted using both histogram and Shapiro–Wilk tests, while Levene’s test was utilized to assess the homogeneity of variance for normally distributed data. To compare numerical variables between different study groups, the independent t-test and Mann–Whitney U-test were applied for symmetric and asymmetric data, respectively. Repeated measurements were analyzed using mixed ANOVA. Symmetrical data were described as mean ± standard deviation, whereas asymmetrical data were presented as median (interquartile range).
Categorical variables were described using frequency and percentage, and statistical differences between groups were evaluated through the chi-square test and Fisher’s exact test, as necessary. For repeated measures, outliers were assessed using box plots and examination of studentized residuals for values greater than ±3.
Levene’s test was employed to assess homogeneity of variance, and Box’s M test was used to evaluate covariance. Mauchly’s test was conducted to verify the assumption of sphericity, and in cases where this assumption was violated for two-way interactions, the Greenhouse-Geisser correction was applied. Pairwise comparisons were performed to determine where the differences lay. However, this is of limited interest because of the significant two-way interactions between groups and time. We used a simple contrast to compare every level of the repeated measures factor to a baseline vital sign. Statistical significance was set at P < 0.05.
Result
Sixty-four mothers who were scheduled for elective cesarean sections and met the criteria were divided into two groups, each consisting of thirty-two participants. There were no dropouts from the study. The two groups did not show any significant differences in terms of age, weight, height, BMI, baseline maternal hemoglobin, and hematocrit level (p>0.05). The estimated amount of blood loss during the surgery, baby weight, and duration of the operation were similar between the groups. Although not statistically significant, the total amount of crystalloid fluid used during the surgery was slightly higher in the isobaric group compared to the hyperbaric group. However, none of the patients in either group received vasopressor therapy. The socio-demographic data of the patient was shown in (Table 1).
 |
Table 1 Demographic Data, Some Perioperative Parameters of Parturients and Neonatal Apgar Score Between Both Groups at Dilla University Referral Hospital, Dilla, Ethiopia, 2022 |
Comparison of Hemodynamic Parameters Between the Groups
There were no significant differences in terms of baseline SBP, DBP, MAP, and HR between the two groups. However, the intraoperative mean SBP decreased from baseline in the isobaric group (98.84 ± 4.33) compared to the hyperbaric group (106.19 ± 3.31) at six minutes with a statistically significant mean difference of-3.344 (95% CI, −5.270 to-1.481, P<0.001). This was also noticed at subsequent time intervals until the 30th min. There were also significant differences in mean DBP and MAP from the sixth minute to the 30th minute (p<0.05). The difference in mean SBP, DBP, MAP and HR was comparable between both groups in all other levels (P>0.05) as shown in (Table 2 and Figure 2).
 |
Table 2 Baseline and Intraoperative Hemodynamics Parameters Between the Two Groups at Dilla University Referral Hospital, Dilla, Ethiopia, 2022 |
 |
Figure 2 Comparison of mean arterial blood pressure in parturients undergoing elective cesarean section between both groups at Dilla University Referral Hospital, Dilla, Ethiopia, 2022. |
Comparison of Repeated Measures Between /Within Groups on Mean Arterial Blood Pressure Measurements
There was a statistically significant interaction between group and time on MAP, F (4.019, 249.200) =9.449, P=0.001, partial η2 = 0.132, and ε = 0.365. The main effect of group showed that there was a statistically significant difference in mean MAP between intervention groups, F (1, 62) = 15.388, P = 0.001, and partial η2 = 0.199. The main effect of time showed a statistically significant difference in mean MAP at different time points, F (4.019, 249.200) =99.847, P = 0.001, Partial η2 = 0.617, ε = 0.365. There was no statistically significant interaction between the baseline and other levels of time on MAP for the hyperbaric bupivacaine group (p>0.05) while a statistically significant decrement of MAP was observed from the 6th minute of spinal anesthesia administration until the 30th minute for the isobaric group (p<0.05) the comparisons of MAP over repeated measures shown in Figure 3.
Onset of Sensory and Motor Blocks Between the Groups
The median (IQR) onset time of maximum sensory block in the isobaric bupivacaine group was 4(1) min compared to the hyperbaric bupivacaine group, in which the corresponding values observed were 3(2) min. The median onset time of maximum motor block in the isobaric bupivacaine group was 5(2) min, whereas for the hyperbaric bupivacaine group, it was 4(2) min. The statistical analysis showed significant differences in both maximum sensory and motor block onset times between the two groups with (P < 0.001) as shown (Figures 4 and 5).
Level of Sensory Block Between the Groups
The levels of sensory block between the groups were assessed, and the majority of parturients in both the isobaric and hyperbaric bupivacaine groups had T6 sensory block. The T10 level of sensory block was observed in 6.3% of parturients in the hyperbaric and 3.1% in the isobaric groups. There were no statistically significant differences in the level of sensory block between the groups (P>0.05) as shown (Figure 6).
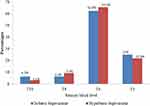 |
Figure 6 Level of sensory block after spinal anesthesia between groups in a parturients underwent elective cesarean section at Dilla University Referral Hospital, Dilla, Ethiopia, 2022. |
Discussion
Bupivacaine is an amide local anesthetic agent commonly used for spinal anesthesia, mainly in hyperbaric or isobaric form. Our study revealed that there was a statistically significant mean difference of 3.34 (−5.27 to −1.48), P< 0.001 at 6 minutes in mean systolic blood pressure between the isobaric group (98.84 4.33) and the hyperbaric group (106.19 ± 3.31). At the 8th, 10th, 15th, 20th, 25th, and 30th min, we also noticed a higher mean SBP in the hyperbaric group than in the isobaric group (P<0.05), although there was no significant difference in the mean SBP between the two groups at baseline or over the other time intervals. This result was similar to that of a study conducted in Pakistan, which indicated that the isobaric bupivacaine group had lower mean SBP (83.27 ± 12.69 mmHg) than the hyperbaric group (114.33±13.83 mmHg) with a statistically significant difference (P < 0.05).23
In contrast to the current study, a double-blind RCT study reported that the mean SBP in the hyperbaric bupivacaine group significantly decreased from five minutes to 15 min compared to the isobaric group (P<0.05). This discrepancy could be caused by the surgical process, use of adjuvant medications (15 mg of fentanyl), and dose variability of bupivacaine (15 mg of 0.5%).24 Similar to this, Critchley et al found that systolic blood pressure was significantly lower in the hyperbaric bupivacaine group than in the isobaric group (P = 0.006). The variation in results might be caused by differences in the study demographics, type of surgery, and dose volume, as well as the use of a small sample size.25
Our main finding also indicated that the mean arterial blood pressure was significantly decreased in the isobaric (70.38 ± 5.61) group at the 6th minute compared to that in the hyperbaric (78.16 ±4.17) group (P = 0.028). We also observed a significant difference in the mean MAP at subsequent time intervals until the 30th minute between the two groups (P<0.05). This is because the MAP value is related to systolic blood pressure, which is also lower in the isobaric group than in the hyperbaric group at these time intervals. There was a comparable MAP at baseline and over the remaining time intervals between the two groups. This finding was comparable with the RCT by Khalid et al on 60 parturients showed a significant decrement in mean systolic blood pressure (P = 0.010) and mean arterial blood pressure (P = 0.028) at five minutes of spinal induction in the isobaric group compared to the hyperbaric group.17 A prospective observational study conducted on 100 parturients in Ethiopia found a significant drop in MAP from the 5th to the 25th minute in the isobaric group compared to the hyperbaric group (P 0.05).26
Our results are inconsistent with those of a double-blind RCT study (Iran) that found a higher incidence of hypotension in the hyperbaric group than in the isobaric group. They found a shorter duration of hypotension in the isobaric group compared to the hyperbaric bupivacaine group (1.67 ±7.8 min vs 7.4 ± 12.5 min, P = 0.004) and lower ephedrine requirements in the isobaric bupivacaine group than in the hyperbaric bupivacaine group (2.4 mg ± 6.6 mg vs 5.3 ± 10.7 mg, P = 0.006).20 The results of our study are also inconsistent with those of a randomized controlled trial conducted at the Cantonal Hospital, which showed a greater reduction in MAP in the hyperbaric group than in the isobaric group. This difference might be due to the difference in the volume of bupivacaine used (10 mg), additive intrathecal fentanyl (15 µg), positioning, height of parturients, and differences in the study population.27
Our study showed comparable mean HR changes at all measurement time intervals in both groups, with baseline vital signs. This finding is comparable with another study conducted at the Dow University of Health Sciences on the effect of intrathecal hyperbaric and isobaric bupivacaine on elective CS that showed comparable HR variation between the groups.23
In our study, while assessing the quality of the block, a faster onset of maximum sensory and motor block was observed in the hyperbaric group than in the isobaric group. The median (IQR) onset times of maximum sensory block in the hyperbaric and isobaric groups were 3(1) and 4 (2) min, respectively (P = 0.001). The median maximum motor block onset time in the hyperbaric group was 4(2) min compared to 5 (2) min in the isobaric group (P < 0.001). However, the final block level achieved with both drugs was adequate for cesarean section without additional analgesic requirements in both groups. This was comparable to the RCT study (Pakistan) by Nadia Bano and Robina Firdous on the onset of block between both drugs among parturients who underwent elective cesarean section. They found a faster mean time onset of block in the hyperbaric bupivacaine group (3.55 ± 0.67 minutes) compared to the isobaric bupivacaine group (7.77 ± 0.77) with P=0.0005.18 Another RCT conducted in India also demonstrated that the average time it took for sensory blockade to occur was 3.11 ± 0.28 minutes in the isobaric group and 1.82 ± 0.14 minutes in the hyperbaric group, showing a statistically significant difference (p < 0.001). Additionally, the study reported that the average time for motor blockade to occur was 4.74 ± 0.51 minutes in the isobaric group and 3.81 ± 0.35 minutes in the hyperbaric group, also showing a significant difference (p < 0.001).28
In contrast to our results, a randomized controlled trial by Martin et al showed rapid sensory and motor block onset times in the isobaric group compared to the hyperbaric group (P<0.05). A possible explanation for this difference may be that they used a different dose of bupivacaine (9.75 mg of 0.75% bupivacaine both groups), or a difference in the study population and type of surgery.19 Our findings are also inconsistent with those of the study conducted by Sarvella et al. A double-blind randomized controlled trial revealed no significant difference between isobaric and hyperbaric bupivacaine at the onset of maximum sensory and motor blocks. These differences might be due to differences in the dose volume and additives (9 mg bupivacaine + 20-mcg fentanyl) used.29
Another randomized controlled trial study in India by Srivastava et al found no statistically significant difference in the onset time and level of sensory block between both groups with P> 0.05.30 Furthermore, a study in Pakistan showed no significant difference in the onset of maximum sensory and motor block between the groups (P>0.05). This difference from our results may be due to a difference in dose volume (10 mg bupivacaine with 25mcg fentanyl were used).31
During spinal anesthesia, the baricity of the local anesthetic affects the block level and blood pressure. Reports have shown that patients undergoing non-obstetric surgery experience lower blood pressure after receiving hyperbaric bupivacaine because it has a higher peak sensory block level and a greater tendency for cephalic spread than isobaric bupivacaine.27,32 However, our results showed comparable peak sensory block heights between the hyperbaric and isobaric bupivacaine groups. This might be related to torso elevation in all patients immediately after spinal anesthetic agent injection. Although we did not include a supine patient group (without pillow insertion) after spinal anesthesia administration as a control, we believe that the intervention may limit the block height resulting from hyperbaric bupivacaine caused by spinal anesthesia. In agreement with our study, other studies also revealed insignificant differences in the level of sensory block between isobaric and hyperbaric bupivacaine groups.29,30
In contrast to our study, Atashkhoei et al showed that patients in a hyperbaric group had higher sensory block levels (at T3) than those in an isobaric group. This difference from our results might be due to the different doses of bupivacaine and the additives (15 µg fentanyl).20 Another study by Helill et al revealed higher levels of sensory blockage in an isobaric bupivacaine group than in a hyperbaric bupivacaine group. A sensory block up to the T4 level was seen in three (6%) patients in the isobaric group and none in the hyperbaric group (P = 0.001). This discrepancy could be due to differences in study design.26
Overall, our study demonstrated that hyperbaric bupivacaine was more effective than isobaric bupivacaine in maintaining intraoperative hemodynamic stability and a faster onset of block in parturients undergoing elective cesarean section delivery.
Strength
There was a homogeneous population in both groups that was comparable with regard to socio-demographic characteristics, preoperative and intraoperative variables that affected the study outcomes, and the same surgical procedure.
Limitations
Our study had certain limitations, including a lack of noninvasive blood pressure measurement and a lack of control over skin incision size. The other limitation of our study was the failure to control the angle of the operating room bed at different times during the surgery and the limited availability of similar studies for the comparison of both drugs at different time intervals.
Conclusion
We conclude that both isobaric and hyperbaric bupivacaine provide an effective subarachnoid block for cesarean sections. However, hyperbaric bupivacaine has been shown to have better intraoperative hemodynamic stability than isobaric bupivacaine, with minimal changes in mean SBP, DBP, and MAP after spinal anesthesia. It also has an earlier onset of maximum sensory and motor blocks than isobaric bupivacaine.
Recommendation
We recommend the clinicians to use hyperbaric bupivacaine to achieve better hemodynamic stability and shorten the duration of the onset of block during cesarean section. We also recommend that researchers perform a multicenter trial including the duration of block with invasive blood pressure measurement between both drugs.
Abbreviations
ASA, American Society of Anesthesiologist; BSC, Bachelor of Science; CSF, Cerebrospinal Fluid; CS, Cesarean Section; DBP, Diastolic Blood Pressure; DURH, Dilla University Referral Hospital; HR, Heart Rate; MAP, Mean Arterial Pressure; MSC, Masters of Science; PACU, Post Anesthesia Care Unit; SBP, Systolic Blood Pressure.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Dilla University College of Health Science and Medicine Institutional Review Board, and written informed consent for participation was obtained from all patients.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Lyell DJ, Power M, Murtough K, et al. Surgical techniques at cesarean delivery: a US survey. Surg J. 2016;2(04):e119–e25. doi:10.1055/s-0036-1594247
2. Robson SJ, De Costa CM. Thirty years of the World Health Organization’s target caesarean section rate: time to move on. Med J Aust. 2017;206(4):181–185. doi:10.5694/mja16.00832
3. Betran AP, Ye J, Moller A-B, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Global Health. 2021;6(6):e005671. doi:10.1136/bmjgh-2021-005671
4. Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian demographic and health survey. BMC Pregnancy Childbirth. 2014;14(1):1–13. doi:10.1186/1471-2393-14-161
5. Gedefaw G, Demis A, Alemnew B, Wondmieneh A, Getie A, Waltengus F. Prevalence, indications, and outcomes of caesarean section deliveries in Ethiopia: a systematic review and meta-analysis. Patient Saf Surg. 2020;14(1):1–10. doi:10.1186/s13037-020-00236-8
6. Campbell J, Sultan P. Regional anaesthesia for caesarean section: a choice of three techniques. Br J Hosp Med. 2009;70(10):605. doi:10.12968/hmed.2009.70.10.44637
7. KlÖHR S, Roth R, Hofmann T, Rossaint R, Heesen M. Definitions of hypotension after spinal anaesthesia for caesarean section: literature search and application to parturients. Acta Anaesthesiol Scand. 2010;54(8):909–921. doi:10.1111/j.1399-6576.2010.02239.x
8. Maayan-Metzger A, Schushan-Eisen I, Todris L, Etchin A, Kuint J. Maternal hypotension during elective cesarean section and short-term neonatal outcome. Am J Obstet Gynecol. 2010;202(1):56. e1–. e5. doi:10.1016/j.ajog.2009.07.012
9. Shitemaw T, Jemal B, Mamo T, Akalu L. Incidence, and associated factors for hypotension after spinal anesthesia during cesarean section at Gandhi Memorial Hospital Addis Ababa, Ethiopia. PLoS One. 2020;15(8):e0236755. doi:10.1371/journal.pone.0236755
10. Kee WDN. Prevention of maternal hypotension after regional anaesthesia for caesarean section. Curr Opin Anesthesiol. 2010;23(3):304–309. doi:10.1097/ACO.0b013e328337ffc6
11. Fakherpour A, Ghaem H, Fattahi Z, Zaree S. Maternal and anaesthesia-related risk factors and incidence of spinal anaesthesia-induced hypotension in elective caesarean section: a multinomial logistic regression. Indian J Anaesth. 2018;62(1):36. doi:10.4103/ija.IJA_416_17
12. Paganelli MA, Popescu GK. Actions of bupivacaine, a widely used local anesthetic, on NMDA receptor responses. J Neuros. 2015;35(2):831–842. doi:10.1523/JNEUROSCI.3578-14.2015
13. Sng B, Han N, Leong W, et al. Hyperbaric vs. isobaric bupivacaine for spinal anaesthesia for elective caesarean section: a Cochrane systematic review. Anaesthesia. 2018;73(4):499–511. doi:10.1111/anae.14084
14. Pollard JB. Cardiac arrest during spinal anesthesia: common mechanisms and strategies for prevention. Anesth Analg. 2001;92(1):252–256. doi:10.1097/00000539-200101000-00050
15. Salama AK, Goma HM, Hamid BMA. Fluid preloading versus ephedrine in the management of spinal anesthesia-induced hypotension in parturients undergoing cesarean delivery: a comparative study. Ain-Shams J Anaesthesiol. 2016;9(1):72. doi:10.4103/1687-7934.178883
16. Assen S, Jemal B, Tesfaye A. Effectiveness of leg elevation to prevent spinal anesthesia-induced hypotension during cesarean delivery in the resource-limited area: open randomized controlled Trial. Anesthesiol Res Pract. 2020;2020:1–8. doi:10.1155/2020/5014916
17. Javed K, Ishrat Z, Akhtar N, Ijaz B. Comparative study of intrathecal 0.5% isobaric versus 0.5% hyperbaric bupivacaine in same volume and dose to assess the quality of spinal anaesthesia and haemodynamic changes occurring during cesarean section. Pakistan J Med Health Sci. 2014;8(2):407–410.
18. Bano N, Firdous R. Effects of intrathecal hyperbaric versus isobaric bupivacaine in elective caesarean section. J Univ Med Dent Coll. 2015;6(2):1–6.
19. Martin R, Frigon C, Chretien A, Tetrault J-P. Onset of spinal block is more rapid with isobaric than hyperbaric bupivacaine. Canad J Anesth. 2000;47(1):43–46. doi:10.1007/BF03020730
20. Atashkhoei S, Abedini N, Pourfathi H, Znoz AB, Marandi PH. Baricity of bupivacaine on maternal hemodynamics after spinal anesthesia for cesarean section: a randomized controlled trial. Iran J Med Sci. 2017;42(2):136. doi:10.1093/bja/86.3.372
21. Ousley R, Egan C, Dowling K, Cyna A. Assessment of block height for satisfactory spinal anaesthesia for caesarean section. Anaesthesia. 2012;67(12):1356–1363. doi:10.1111/anae.12034
22. Šklebar I, Bujas T, Habek D. Spinal anaesthesia-induced hypotension in obstetrics: prevention and therapy. Acta Clin Croat. 2019;58(Suppl 1):90. doi:10.20471/acc.2019.58.s1.13
23. Aftab S, Ali H, Zafar S, Sheikh M, Sultan ST. Intrathecal isobaric versus hyperbaric bupivacaine for elective Caesarean section. Surgery. 2007;154:
24. Upadya M, Neeta S, Manissery JJ, Kuriakose N, Singh RR. A randomized controlled study comparing intrathecal hyperbaric bupivacaine-fentanyl mixture and isobaric bupivacaine-fentanyl mixture in common urological procedures. Indian J Anaesth. 2016;60(1):44–49. doi:10.4103/0019-5049.174813
25. Critchley L, Morley A, Derrick J. The influence of baricity on the haemodynamic effects of intrathecal bupivacaine 0.5%. Anaesthesia. 1999;54(5):469–474. doi:10.1046/j.1365-2044.1999.00841.x
26. Helill SE, Sahile WA, Abdo RA, Wolde GD, Halil HM. The effects of isobaric and hyperbaric bupivacaine on maternal hemodynamic changes post spinal anesthesia for elective cesarean delivery: a prospective cohort study. PLoS One. 2019;14(12):e0226030. doi:10.1371/journal.pone.0226030
27. Solakovic N. Level of sensory block and baricity of bupivacaine 0.5% in spinal anesthesia. Med Arch. 2010;64(3):158.
28. Saha N, Singh R, Mittal T. Comparison of intrathecal 0.5% isobaric levobupivacaine with fentanyl and 0.5% hyperbaric bupivacaine with fentanyl in LSCS surgeries – a randomized double-blind trial. Int J Adv Integ Med Sci. 2023;8(1):19–2.
29. Sarvela PJ, Halonen PM, Korttila KT. Comparison of 9 mg of intrathecal plain and hyperbaric bupivacaine both with fentanyl for cesarean delivery. Anesth Analg. 1999;89(5):1257–1262. doi:10.1213/00000539-199911000-00033
30. Srivastava U, Kumar A, Gandhi N, et al. Hyperbaric or plain bupivacaine combined with fentanyl for spinal anaesthesia during caesarean delivery. Indian J Anaesth. 2004;48(1):44–46.
31. Punshi GD, Afshan G. Spinal anaesthesia for caesarean section: plain vs hyperbaric bupivacaine. J Pak Med Assoc. 2012;62(8):807.
32. Tetzlaff JE, O’Hara J, Bell G, Grimm K, Yoon HJ. Influence of baricity on the outcome of spinal anesthesia with bupivacaine for lumbar spine surgery. Reg Anesth Pain Med. 1995;20(6):533–537.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



