Back to Journals » Journal of Pain Research » Volume 15
Effects of Continuous Fascia Iliaca Compartment Block on Early Quality of Recovery After Total Hip Arthroplasty in Elderly Patients: A Randomized Controlled Trial
Authors Gao Y, Li H, Hu H, Xu Y , Zhou J , Liu Y
Received 5 April 2022
Accepted for publication 17 June 2022
Published 28 June 2022 Volume 2022:15 Pages 1837—1844
DOI https://doi.org/10.2147/JPR.S368285
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Ying Gao,1 He Li,2 Hongfei Hu,1 Yi Xu,1 Jun Zhou,2 Youtan Liu1
1Department of Anesthesiology, Shenzhen Hospital of Southern Medical University, Shenzhen, 518110, People’s Republic of China; 2Department of Anesthesiology, The Third Affiliated Hospital of Southern Medical University, Guangzhou, 510630, People’s Republic of China
Correspondence: Jun Zhou, Department of Anesthesiology, The Third Affiliated Hospital of Southern Medical University, Guangzhou, 510630, People’s Republic of China, Tel +86 13827771415, Email [email protected] Youtan Liu, Department of Anesthesiology, Shenzhen Hospital of Southern Medical University, Shenzhen, 518110, People’s Republic of China, Tel +86 13902448143, Email [email protected]
Purpose: In recent years, patient-centered postoperative quality of recovery has gained attention. This study aimed to assess the influence of ultrasound-guided continuous fascia iliaca compartment block (CFICB) on early quality of recovery in elderly patients after total hip arthroplasty (THA) using the QoR-15 score.
Patients and Methods: In this single-center, randomized, prospective study, 60 patients scheduled for unilateral THA were randomized to the CFICB or patient-controlled intravenous analgesia (PCIA) group. The primary outcome was the QoR-15 score. The secondary outcomes were pain score, number of patients requiring rescue analgesics, time of first postoperative ambulation, incidence of postoperative complications, Bromage score, and length of hospital stay.
Results: The QoR-15 score was significantly higher in the CFICB group than in the PCIA group at 24 h (P < 0.001) after surgery. However, the QoR-15 score was not significantly different at 48 h (P = 0.074) between the two groups. Pain scores at rest and during movement were lower in the CFICB group than in the PCIA group at 12, 24, and 48 h postoperatively (P < 0.05). There was no difference in the number of patients requiring rescue analgesics, time of first postoperative ambulation, incidence of postoperative complications apart from dizziness, or length of hospital stay between the two groups. In addition, Bromage score of 1 point was reported by four patients in the CFICB group at 24 h (P = 0.048) after THA.
Conclusion: In elderly patients following THA, CFICB improved the quality of recovery at 24 h and reduced pain scores compared with PCIA. The time of first postoperative ambulation and length of hospital stay were not significantly affected.
Keywords: total hip arthroplasty, elderly, continuous fascia iliaca compartment block, postoperative quality of recovery
Introduction
Total hip arthroplasty (THA) is one of the most common surgical procedures performed worldwide.1 It is worth noting that the procedure is most often performed in patients aged 65 years and older,1 and its incidence in this age group may increase in the future due to the aging of the population.2 THA improves the mobility of elderly patients, thus benefitting their quality of life.3 However, THA is associated with moderate-to-severe postoperative acute and chronic pain.4 In the mid-1990s, the American Pain Society proposed that pain should be considered as the fifth vital sign.5 Severe acute pain increases the incidence of the postoperative complications such as delirium, pneumonia, and cardiac events; affects early postoperative functional rehabilitation; reduces patient satisfaction; and increases the incidence of chronic postsurgical pain.6 Therefore, adequate postoperative analgesia is of utmost importance to enhance the quality of recovery in elderly patients undergoing THA.
Opioids remain the mainstream analgesics that are indispensable for treating acute and chronic pain; however, there is growing concern about the side effects of opioids, such as postoperative nausea and vomiting (PONV), dizziness, urinary retention, and respiratory depression.7,8 The regional analgesic technique is a popular method to provide effective analgesia and reduce opioid consumption, which might help avoid the opioid-related side effects.9 The ideal regional block for THA can provide effective postoperative analgesia for patients without increasing the risk of motor dysfunction and affecting early postoperative functional rehabilitation. The fascia iliaca compartment block (FICB) provides effective analgesia for THA by blocking the femoral nerve, obturator nerve, and lateral femoral cutaneous nerve.10 Previous studies have shown that a single injection of FICB results in effective analgesia without an increase in the risk of fall after surgery; however, the analgesia duration only ranges from 8 to 24 h postoperatively.11,12 Therefore, the implementation of continuous FICB (CFICB) has advantages for extending the duration of analgesia after THA.13
However, the influence of CFICB on the quality of recovery in elderly patients following THA has not yet been elucidated. Quality of recovery after surgery and anesthesia is a complex process that should be measured using a more comprehensive and patient-centered approach. The QoR-15 score has been proven to be a validated measure for assessing the quality of postoperative recovery.14 This study was designed to assess the influence of CFICB on early quality of recovery after THA using the QoR-15 score. We hypothesized that CFICB would improve the early quality of recovery in elderly patients undergoing THA.
Materials and Methods
Patient Enrollment
This trial was prospectively registered in the Chinese Clinical Trials Registry (ChiCTR2100046935) and approved by the Ethics Committee of the Third Affiliated Hospital of Southern Medical University (2021-ER-018). This study followed the ethical guidelines set forth in the Declaration of Helsinki. We enrolled patients aged ≥65 years, American Society of Anesthesiologists (ASA) physical status I–III, and scheduled for unilateral THA from August 2021 to January 2022 at the Third Affiliated Hospital of Southern Medical University. Exclusion criteria included contraindications to combined spinal-epidural or regional block, cognitive dysfunction, history of chronic opioid use, revision hip surgery, severe organ dysfunction, allergy to any drug used in the study, body mass index (BMI) ≥30 kg/m2, and refusal to participate. Informed written consent was obtained from all enrolled patients.
Randomization and Blinding
Patients were randomized into the CFICB or PCIA group equally using a computer-generated random number table. Numbered and sealed envelopes were used to conceal each patient’s allocation status. The study was conducted by three investigators. The first investigator preoperatively assessed patient eligibility and assigned a sealed envelope to each patient. When patients arrived at the post-anesthesia care unit (PACU) after surgery, the second investigator, who was experienced in these analgesia techniques, opened the prepared envelope and performed the specified analgesic technique. The outcome measures were assessed by a third investigator. As CFICB is an invasive procedure, performing a placebo block in the PCIA group would harm patients. Therefore, it was not possible to blind patients or outcome assessor.
Anesthetic Technique
On the day of the surgery, patients were transferred to the operating room, and vital signs were monitored by ECG, noninvasive or invasive blood pressure, and pulse oximetry. After intravenous access was obtained, a combined spinal-epidural block was performed in the L2–L3 or L3–L4 intervertebral space by an anesthesiologist. After a spinal injection of 2.5–3 mL of 0.5% isobaric ropivacaine was administered, the spinal needle was withdrawn, and an epidural catheter was inserted. The epidural catheter was immediately removed after surgery. All patients received intravenous tropisetron (5 mg) to prevent PONV and dexmedetomidine for sedation during the operation.
Postoperative Analgesia
After surgery, the patient was transferred to the PACU. The analgesic techniques, including CFICB and PCIA, were performed by the second investigator with extensive anesthesia experience. In the CFICB group, patients were placed in the supine position. After skin disinfection and draping, the anesthesiologist placed a high-frequency linear ultrasound transducer probe on the anterior superior iliac spine, pointing toward the xiphisternum, and then moved medially along the inguinal ligament until the hourglass pattern was recognized. Using an in-plane technique, the needle was introduced in an inferior-to-superior direction and passed through the sartorius, and then, it perforated the fascia iliaca.15 Then, 1–2 mL of normal saline solution was injected to confirm the proper positioning of the needle tip, and 40 mL of 0.25% ropivacaine was injected slowly to separate the iliac fascia space. Subsequently, the catheter was inserted, fixed properly, and then connected to the electronic infusion pump. Continuous infusion of 0.2% ropivacaine (5mL/h for basic infusion, 5 mL for a bolus, and a lockout interval of 30 min) was maintained 48 h after the surgery.
In the PCIA group, patients received a PCIA pump containing sufentanil 1 µg/mL and tropisetron 0.1 mg/mL attenuated by normal saline after surgery. The continuous infusion (2 mL/h for basic infusion, 2 mL for a bolus, and a lockout interval of 15 min) was maintained for 48 h postoperatively. When the visual analog scale (VAS) score was greater than or equal to 4, the infusion pump bolus button was pressed. If the pain was not alleviated, tramadol 100 mg was administered for rescue analgesia.
Outcome Measurements
The primary outcome was the QoR-15 score, which was reported by the patients at 24 and 48 h postoperatively. The QoR-15 score includes five dimensions: pain (two items), physical comfort (five items), physical independence (two items), psychological support (two items), and emotional state (four items) (Supplemental Table 1). Each item’s score ranged from 0 to 10, and the total score ranged from 0 to 150, with a higher QoR-15 score indicating better quality of recovery.16
Secondary outcomes included the VAS score during rest and movement at 6, 12, 24, and 48 h postoperatively; number of patients requiring rescue analgesics; adverse events related to CFICB (such as puncture site infection, nerve injury, and local anesthetic toxicity); incidence of postoperative complications (such as PONV, delirium, pneumonia, and cardiac events); time of first postoperative ambulation; length of hospital stay; and Bromage score at 24 and 48 h after surgery. Lower limb motor dysfunction was evaluated using the Bromage score, which is graded from 0 (no motor block) to 3 (complete motor block). The higher the score, the more severe is the motor block.17
Statistical Analysis
The sample size of this study was calculated using the QoR-15 score at 24 h postoperatively. Based on previous studies, the minimum clinically important difference in QoR-15 is 8.0, and the SD of QoR-15 scores after major surgery is approximately 16.18,19 With type I error=0.05 and a power of 80%, a sample size of 30 patients per group was calculated.
All data were analyzed using IBM SPSS version 26. Continuous data were tested for normality using the Kolmogorov–Smirnov test. The normally distributed data were expressed as mean ± SD, and the intergroup comparison were performed using the independent sample t-test. Non-normally distributed data were described as median (interquartile range), and inter-group comparisons were performed using the Mann–Whitney U-test. Categorical data, such as sex, ASA physical status, and type of disease, were analyzed using the chi-square test or Fisher’s exact test. Statistical significance was set at P < 0.05.
Results
Sixty patients who met the inclusion criteria were recruited. In the CFICB group, two patients were excluded because of accidental removal of the catheter, and one patient was excluded because of catheter blockage. In the PCIA group, one patient withdrew because of severe PONV. Finally, 27 and 29 patients were included in the CFICB and PCIA groups, respectively (Figure 1). The demographic and surgical characteristics were comparable between the two groups (Table 1).
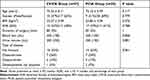 |
Table 1 Demographic and Surgical Characteristics |
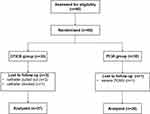 |
Figure 1 CONSORT flow diagram. Abbreviations: CFICB, continuous fascia iliaca compartment block; PCIA, patient-controlled intravenous analgesia. |
The primary outcome of the QoR-15 score is shown in Table 2. At 24 h postoperatively, QoR-15 score was significantly higher in the CFICB group than in the PCIA group (114.11 ± 10.63 vs 100.69 ± 7.65, P < 0.001). Apart from physical independence (P = 0.313), the remaining four dimensions were significantly higher in the CFICB group than in the PCIA group at 24 h. At 48 h postoperatively, there was no significant difference with respect to QoR-15 score between the two groups (117.74 ± 9.35 vs 112.90 ± 10.45, P = 0.074). Of the five dimensions of the QoR-15, only pain (P = 0.006) and emotional state (P = 0.034) were higher in the CFICB group than in the PCIA group at 48 h.
 |
Table 2 QoR-15 Scores at 24h and 48h After Surgery Between Two Groups |
Regarding secondary outcomes, the VAS scores at rest and movement were significantly lower in the CFICB group than in the PCIA group at 12, 24, and 48 h after surgery (Table 3). No intergroup differences were found in the number of patients requiring rescue analgesics, adverse events, incidence of postoperative complications except for dizziness (P = 0.042), time of first postoperative ambulation, or length of hospital stay (Table 4). In addition, Bromage score of 1 point was reported by four patients at 24 h (P = 0.048) postoperatively in the CFICB group compared with the PCIA group (Table 4).
 |
Table 3 VAS Score Between Two Groups |
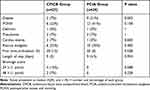 |
Table 4 Postoperative Complications, Number of Patients Requiring Rescue Analgesics, First Time of Postoperative Ambulation, Length of Hospital Stay and Bromage Score Between Two Groups |
Discussion
This is the first prospective randomized trial to evaluate the influence of CFICB on early quality of recovery in elderly patient after THA using the patient-centered outcome measure, QoR-15 score. For our primary outcome, we demonstrated that CFICB significantly improved the quality of recovery at 24 h postoperatively. Additionally, the CFICB group had a lower pain score burden than the PCIA group. However, we were unable to demonstrate a difference in time of first postoperative ambulation and length of hospital stay between the two groups.
The QoR-15 score is a simplified form of the QoR-40 score but has retained the good psychometric characteristics of the QoR-40 score and improved its clinical acceptability and feasibility, allowing its wider use in research and clinical practice.16 The QoR-15 score has been validated and has shown good content validity and internal consistency.14,20 Prior studies have shown that regional block techniques would improve postoperative quality of recovery.21,22 Similarly, we demonstrated that patients who received CFICB had a higher QoR-15 score at 24 h postoperatively than those in the PCIA group; however, the clinical difference between groups disappeared at 48 h postoperatively. Notably, the physical independence dimension was not significantly different at either 24 or 48 h postoperatively. One possible explanation for this phenomenon is that patients ambulate briefly during the first two postoperative days and remain in bed for most of the time.
Some studies have investigated the influence of other regional blocks on the quality of recovery after THA using the QoR-15 score.23–25 Lennon et al assessed the effect of the erector spinae plane block on the quality of recovery at 24 h after THA, and the results showed that the erector spinae plane block did not improve postoperative quality of recovery in THA.23 Wang et al measured the effect of lateral femoral cutaneous nerve and iliohypogastric/ilioinguinal nerve blocks on postoperative quality of recovery at 24 and 48 h after THA; however, the clinical significance was observed only at 24 h postoperatively.24 In our study, CFICB improved the quality of recovery only at 24 h after THA; however, it was surprising that we used continuous regional block to provide postoperative analgesia for patients, while Wang et al used only a single injection regional block. Therefore, which regional analgesic technique could significantly improve the postoperative quality of recovery for THA needs to be determined. Previous studies have confirmed that FICB can provide 8 to 24 h effective analgesia for patients11,12; however, none has studied the effect of FICB on the quality of recovery after THA. In the future, we could investigate the effect of FICB plus non-opioids, compared to that of PCIA, on the quality of recovery after THA.
In this study, we were unable to demonstrate a difference in the VAS score between the two groups during rest and movement at 6 h postoperatively. A combined spinal-epidural block was used as an anesthetic technique in our study, and although the epidural catheter was removed immediately after surgery, local anesthetics could be administered through the epidural catheter when the anesthetic effect was insufficient during the operation. However, supplemental local anesthetic doses were not recorded in this study, and the similar pain scores in the two groups at 6 h postoperatively may be due to the analgesia of the spinal-epidural block. In addition, patients who received CFICB had lower VAS scores at 12, 24, and 48 h after surgery than those who received PCIA. The benefit of effective analgesia with CFICB was consistent with previous studies.26,27 Nie et al evaluated the effect of CFICB on postoperative analgesia for hip fracture compared with fentanyl PCIA, and the results showed that patients in the CFICB group had less pain than those in the PCIA group with no adverse events related to nerve block.26 No adverse events such as nerve injury, anesthetic toxicity, or infection were observed in our study. Therefore, CFICB is an effective and safe analgesic technique in patients undergoing hip surgery.
In our study, we prospectively observed the influence of CFICB on complications following THA during hospitalization. We found that the incidence of postoperative complications did not appear to be clinically significant, apart from dizziness, between the two groups. Postoperative delirium, pneumonia, or cardiac events were diagnosed according to clinical and laboratory indicators and were not significantly different between the two groups. The incidence of PONV and the number of patients requiring analgesics were higher in the PCIA group than in the CFICB group; however, the difference did not appear to be clinically significant. Our results were partially consistent with those of previous studies.28–30 Loessin et al used CFICB to provide analgesia for patients undergoing hip surgery and found no difference in the incidence of opioid-related side effects, delirium, or length of stay compared with the standard analgesia.28 A retrospective study conducted by Rasappan et al showed that the rate of complications after hip surgery, including acute retention of urine, pneumonia, delirium, and deep vein thrombosis, were comparable between the CFICB and control groups during their inpatient stay.29 However, these studies were designed differently and the sample size was small. High-quality, large-sample randomized trials are needed to prospectively evaluate the influence of CFICB on postoperative systematic complications.
In the CFICB group, the four patients with a Bromage score of 1 point reported numbness in the thigh at 24 h, and in two of these, the numbness remained at 48 h after THA. This may be due to the single injection of 40 mL 0.25% ropivacaine or the excessive ropivacaine dose produced by the CFICB analgesic pump that was not calculated according to the patient’s weight. Notably, falls were not observed in either group. Future studies should investigate the optimal concentration and dose of ropivacaine for the first injection and continuous infusion.
This study had several limitations. First, this study selected elderly patients undergoing unilateral THA but did not specify the types of diseases at enrollment. The degree of pain caused by different types of diseases before surgery may affect postoperative pain scores. Second, this study assessed QoR-15 scores only at 24 and 48 h after THA; the long-term quality of recovery was not evaluated. Further studies should focus on the effect of CFICB on functional rehabilitation and the long-term quality of recovery in elderly patients after THA. Finally, CFICB was an invasive operation; considering the benefit for patients, patients and outcome assessors were not blinded in this study. Nevertheless, patients may have known their group allocation for the analgesic technique, but they did not know which analgesic technique provided better analgesia. Additionally, the QoR-15 score is a patient-centered questionnaire that is answered independently by patients expressing their subjective feelings. The results of this study provide a reference for the selection of analgesic methods for clinical use.
Conclusion
In conclusion, there was no difference in the time of first postoperative ambulation and length of hospital stay between the two groups. CFICB was effective in improving the quality of recovery at 24 h and reducing pain scores in elderly patients after THA. Furthermore, patients who underwent CFICB did not develop regional block-related complications. This study indicates that CFICB is a safe and effective analgesic technique for THA.
Data Sharing Statement
The data of this study can be obtained by contacting the corresponding author ([email protected]).
Funding
This study was funded by the National Natural Science Foundation of China (82072215) and Technology Planning Project of Shenzhen, China (JCYJ20190814111018958).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012;380(9855):1768–1777. doi:10.1016/s0140-6736(12)60607-2
2. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi:10.1016/s0140-6736(12)62167-9
3. Shan L, Shan B, Graham D, Saxena A. Total Hip replacement: a systematic review and meta-analysis on mid-term quality of life. Osteoarthritis Cartilage. 2014;22(3):389–406. doi:10.1016/j.joca.2013.12.006
4. Gerbershagen H, Pogatzki-Zahn E, Aduckathil S, et al. Procedure-specific risk factor analysis for the development of severe postoperative pain. Anesthesiology. 2014;120(5):1237–1245. doi:10.1097/aln.0000000000000108
5. Chisholm-Burns MA, Spivey CA, Sherwin E, Wheeler J, Hohmeier K. The opioid crisis: origins, trends, policies, and the roles of pharmacists. Am J Health Syst Pharm. 2019;76(7):424–435. doi:10.1093/ajhp/zxy089
6. Gaffney CJ, Pelt CE, Gililland JM, Peters CL. Perioperative pain management in Hip and Knee arthroplasty. Orthop Clin North Am. 2017;48(4):407–419. doi:10.1016/j.ocl.2017.05.001
7. Martinez V, Abalo R. Peripherally acting opioid analgesics and peripherally-induced analgesia. Behav Pharmacol. 2020;31(2&3):136–158. doi:10.1097/FBP.0000000000000558
8. Benyamin R, Trescot A, Datta S, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl):S105–S120. doi:10.36076/ppj.2008/11/S105
9. Nielsen ND. Peripheral nerve blocks for analgesia after elective total hip arthroplasty. Acta Anaesthesiol Scand. 2020;64(6):829–830. doi:10.1111/aas.13567
10. Jones MR, Novitch MB, Hall OM, et al. Fascia iliaca block, history, technique, and efficacy in clinical practice. Best Pract Res Clin Anaesthesiol. 2019;33(4):407–413. doi:10.1016/j.bpa.2019.07.011
11. Verbeek T, Adhikary S, Urman R, Liu H. The application of fascia iliaca compartment block for acute pain control of Hip fracture and surgery. Curr Pain Headache Rep. 2021;25(4):22. doi:10.1007/s11916-021-00940-9
12. Zhang XY, Ma JB. The efficacy of fascia iliaca compartment block for pain control after total Hip arthroplasty: a meta-analysis. J Orthop Surg Res. 2019;14(1):33. doi:10.1186/s13018-018-1053-1
13. Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113(4):904–925. doi:10.1213/ANE.0b013e3182285e01
14. Kleif J, Waage J, Christensen KB, Gogenur I. Systematic review of the QoR-15 score, a patient- reported outcome measure measuring quality of recovery after surgery and anaesthesia. Br J Anaesth. 2018;120(1):28–36. doi:10.1016/j.bja.2017.11.013
15. Singh H, Jones D. Hourglass-pattern recognition simplifies fascia iliaca compartment block. Reg Anesth Pain Med. 2013;38(5):467–468. doi:10.1097/AAP.0b013e3182a1f772
16. Stark PA, Myles PS, Burke JA. Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15. Anesthesiology. 2013;118(6):1332–1340. doi:10.1097/ALN.0b013e318289b84b
17. Craig D, Carli F. Bromage motor blockade score - a score that has lasted more than a lifetime. Can J Anaesth. 2018;65(7):837–838. doi:10.1007/s12630-018-1101-7
18. Myles PS, Myles DB, Galagher W, Chew C, MacDonald N, Dennis A. Minimal clinically important difference for three quality of recovery scales. Anesthesiology. 2016;125(1):39–45. doi:10.1097/ALN.0000000000001158
19. Finnerty DT, McMahon A, McNamara JR, Hartigan SD, Griffin M, Buggy DJ. Comparing erector spinae plane block with serratus anterior plane block for minimally invasive thoracic surgery: a randomised clinical trial. Br J Anaesth. 2020;125(5):802–810. doi:10.1016/j.bja.2020.06.020
20. Bu XS, Zhang J, Zuo YX. Validation of the Chinese version of the quality of recovery-15 score and its comparison with the post-operative quality recovery scale. Patient. 2016;9(3):251–259. doi:10.1007/s40271-015-0148-6
21. Nair G, Wong DJ, Chan E, Alexander T, Jeevananthan R, Pawa A. Mode of anesthesia and quality of recovery after breast surgery: a case series of 100 patients. Cureus. 2021;13(3):e13822. doi:10.7759/cureus.13822
22. Wang D, He Y, Chen X, Lin Y, Liu Y, Yu Z. Ultrasound guided lateral quadratus lumborum block enhanced recovery in patients undergoing laparoscopic colorectal surgery. Adv Med Sci. 2021;66(1):41–45. doi:10.1016/j.advms.2020.12.002
23. Lennon MJ, Isaac S, Currigan D, O’Leary S, Khan RJK, Fick DP. Erector spinae plane block combined with local infiltration analgesia for total Hip arthroplasty: a randomized, placebo controlled, clinical trial. J Clin Anesth. 2021;69:110153. doi:10.1016/j.jclinane.2020.110153
24. Wang Q, Yang Y, Yang Z, et al. Analgesic effects of ultrasound-guided iliohypogastric/ilioinguinal nerve block combined with lateral femoral cutaneous nerve block in total hip arthroplasty via direct anterior approach: a retrospective cohort study. Orthop Surg. 2021;13(3):920–931. doi:10.1111/os.12795
25. Tan NL, Gotmaker R, Barrington MJ. Impact of local infiltration analgesia on the quality of recovery after anterior total Hip arthroplasty: a randomized, triple-blind, placebo-controlled trial. Anesth Analg. 2019;129(6):1715–1722. doi:10.1213/ANE.0000000000004255
26. Nie H, Yang Y, Wang Y, Liu Y, Zhao B, Luan B. Effects of continuous fascia iliaca compartment blocks for postoperative analgesia in patients with Hip fracture. Pain Res Manag. 2015;20(4):210–212. doi:10.1155/2015/872651
27. Dulaney-Cripe E, Hadaway S, Bauman R, et al. A continuous infusion fascia iliaca compartment block in Hip fracture patients: a pilot study. J Clin Med Res. 2012;4(1):45–48. doi:10.4021/jocmr724w
28. Loessin V, ElZahabi AJ, Brownbridge B, Bajwa JS. Continuous fascia iliaca block for acute Hip fractures: a randomized-controlled pilot study. Can J Anaesth. 2019;66(10):1265–1267. doi:10.1007/s12630-019-01428-2
29. Rasappan K, Chua ITH, Tey JBL, Ho SWL. The continuous infusion fascia iliaca compartment block: a safe and effective analgesic modality in geriatric Hip fracture patients. Arch Orthop Trauma Surg. 2021;141(1):29–37. doi:10.1007/s00402-020-03450-2
30. Yamamoto N, Sakura S, Noda T, et al. Comparison of the postoperative analgesic efficacies of intravenous Acetaminophen and fascia iliaca compartment block in Hip fracture surgery: a randomised controlled trial. Injury. 2019;50(10):1689–1693. doi:10.1016/j.injury.2019.03.008
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
