Back to Journals » Journal of Pain Research » Volume 15
Effectiveness of Ultrasound-Guided Retrolaminar Block and Erector Spinae Plane Block in Retroperitoneal Laparoscopic Surgery: A Randomized Controlled Trial
Authors Liu D, Zhang G, Zhu Y, Liu X , Xu S, He M , Chen S, An K, Liang G, Zhu Z
Received 11 November 2021
Accepted for publication 24 February 2022
Published 28 March 2022 Volume 2022:15 Pages 815—826
DOI https://doi.org/10.2147/JPR.S349028
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Dexing Liu,1,2 Guangting Zhang,2 Yuhang Zhu,2 Xingxing Liu,1,2 Shan Xu,1,2 Miao He,1,2 Shulian Chen,3 Ke An,2 Guobiao Liang,1,3 Zhaoqiong Zhu1,2
1Medical College of Soochow University, Soochow University, Suzhou, People’s Republic of China; 2Department of Anesthesiology, Affiliated Hospital of Zunyi Medical University, Zunyi, People’s Republic of China; 3Department of Urology, Affiliated Hospital of Zunyi Medical University, Zunyi, People’s Republic of China
Correspondence: Zhaoqiong Zhu, Tel +86-851-28609145, Fax +86-851-28609145, Email [email protected]
Purpose: Retrolaminar block (RLB) and erector spine plane block (ESPB) share a similar block site, but their analgesia principle may differ. This study compared the postoperative analgesic effects of ultrasound-guided RLB and ESPB for retroperitoneal laparoscopic surgery.
Patients and Methods: The study included patients who scheduled for laparoscopic nephrectomy from July 2020 to January 2021. Patients in RLB group received a three-point block at the posterior surface of T8-T10 lamina, and those in ESPB group received at the T9 level. The primary result was the score of visual analogue scale (VAS). Secondary results included information on intraoperative and postoperative analgesia consumption and rescue analgesia usage, skin temperature, serum interleukin (IL)-1β, prostaglandin E2 (PGE2) level and the occurrence of safety events.
Results: There was no significant difference between the two groups in the postoperative VAS scores at both the rest and cough state (All P> 0.05). The skin surface temperature of the affected side and the healthy side in ESPB group was higher than that in the RLB group at the end of the surgery (P=0.002) and after surgery (P=0.016). The RLB group had a higher ephedrine usage than the ESPB group (P=0.027). Compared with the ESPB group, the RLB group had a shorter time to exhaust (P=0.045) and lower serum IL-1β level (P=0.049). Patients in neither group developed severe adverse event.
Conclusion: Ultrasound-guided RLB and ESPB can provide safe and effective postoperative analgesia for retroperitoneal laparoscopic surgery. ESPB has more stable intraoperative hemodynamics, while RLB has more potential research value for patients’ rapid recovery.
Keywords: nerve block, perioperative care, anesthetics, laparoscopy
Introduction
Laparoscopic nephrectomy was first reported by Clayman et al.1 Although it can be well completed by transperitoneal or retroperitoneal approach,2 the latter can achieve better perioperative outcomes.3 Therefore, retroperitoneal laparoscopic surgery is the most common clinical surgical method of treating kidney-related diseases.4–6 With the continuous advancement of visual anesthesia technology, nerve block technology has shown great values in applying abdominal surgery, and regional nerve block has become an essential component of postoperative multimodal analgesia.7 Due to the postoperative analgesic ability of “opioid-free”,8–10 multimodal analgesia involved by nerve block is expected to be the protagonist of contemporary clinical analgesia management. However, retroperitoneal laparoscopic surgery has an incision in the lateral abdomen, which presents new challenges to the rational selection of nerve block sites.
Several studies have reported the effectiveness of quadratus lumborum block (QLB) and paravertebral block (PVB) in postoperative analgesia, showing the availability of ultrasound technology guided trunk nerve block in postoperative analgesia management for retroperitoneal laparoscopic surgery.11–13 PVB has complex procedures and exhibits no breakthrough progress compared with traditional epidural analgesia,13 not to mention the possibility of serious complications such as pneumothorax. QLB also belongs to deep block and has its puncture site very close to the surgical incision, limiting the timing of its block to some extent. Therefore, appropriate options for the surgical approach of trunk nerve block for such surgery are still far from satisfaction.
Newer approaches to PVB and QLB have been the focus of many studies in recent years. Retrolaminar block (RLB)14 and erector spine plane block (ESPB)15 are considered to be compartment blocks or interfacial plane blocks. In these approaches, local anesthetics are assumed to penetrate the superior costotransverse ligament and reach the paravertebral space, although the needle tip is not advanced into the paravertebral space. In such instances, our research group were highly interested in the clinical application of RLB and ESPB for retroperitoneal laparoscopic surgery. However, existing reports only used RLB as postoperative analgesia in thoracic and lumbar surgery. Studies on ESPB also stayed in cadaveric and imaging levels.16–18 We previously conducted the RLB by using a three-point injection and demonstrated its value in retroperitoneal laparoscopic surgery.19 Based on the previous studies and clinical experience, ESPB shares a similar and novel injection point with the RLB, and could further resolve the disadvantage of limited diffusion in the block range of RLB. And according to the existing literature,20–22 both the ultrasound-guided RLB and ESPB15 are expected to provide excellent postoperative analgesia. However, specific differences may exist between the two methods regarding the management in perioperative anesthesia. Considering no randomized controlled trial has directly compared the RLB and the ESPB, we designed this study to investigate if the RLB and the ESPB would differed in postoperative analgesia for patients who underwent retroperitoneal laparoscopic surgery.
Materials and Methods
Study Design
This study was a randomized, double-blind controlled study. With the approval of the Ethics Committee of the Affiliated Hospital of Zunyi Medical College (ethical review No.: KLL-2019-007), the study protocol was registered in the China Clinical Trials Registration Center (http://www.chictr.org.cn, Project No. ChiCTR2000034485). The study complies with the Declaration of Helsinki. The participants and their family members were all informed and signed the informed consent forms before the initiation of this study. Finally, patients who underwent the elective operation of retroperitoneal laparoscopic surgery in the Affiliated Hospital of Zunyi Medical University from July 2020 to January 2021 were recruited.
Inclusion criteria: 1) Aged 18–65 years; 2) body mass index (BMI): 18–28kg/m2; 3) American Standards Association (ASA) grade I–III; 4) elective operation of retroperitoneal laparoscopic surgery; and 5) the investigator considered that the patient needed invasive arterial monitoring during the surgery. Exclusion criteria: 1) severe heart, liver and lung dysfunction; 2) abnormal blood coagulation; 3) history of allergy to anesthetic drugs; 4) history or family history of high malignant fever; 5) history of long-term drinking, chronic pain or long-term use of psychotropic drugs; 6) scar, infection and tumor of puncture site; 7) pregnancy and lactation; 8) patients with diabetes; 9) patients with severe visual and auditory disorders; and 10) patients with endocrine system diseases; 11) transferred to intensive care unit (ICU) after surgery; 12) intraoperative alteration of operation method; and 13) patients withdrew for any reason.
Blinding and Grouping
When the patients entered the operating room, an opaque envelope containing a computer-generated allocation sequence was open to determine the random grouping. Two groups of researchers with different responsibilities completed the study (Figure S1). RLB group: after the induction of general anesthesia, the patients were placed in the lateral position to specify the T7 body that located at inferior angle of the scapula, and then successively marked the T8, T9, T10 (Figure 1A). After preparing the skin and completing draping, an ultrasonography convex array probe (1–5Hz, M9, Mindray Ltd, Shenzhen, China) was placed at the median transverse section of the centrum to identify the lamina corresponding to T8, T9 and T10 through the short spinal axis (Figure 1B), and to introduce the puncture needle (21G x100mm, USG-Type CCR, Hakko Co. Ltd. Nagano, Japan) to contact lamina. The puncture needle opened 1 cm beside the mark side of the probe by the in-plane technique, and the needle was inserted at a 45° angle to the skin. Then we retracted the tip of needle to the lamina about 1 mm and withdrew to make sure that there was no blood or cerebrospinal fluid. 10mL ropivacaine (0.4%) was injected posterior to the lamina of T8, T9, and T10, respectively, with 30mL in total (Figure 1C). ESPB group: Similarly, after the induction of general anesthesia, the patients were placed in a lateral position (Figure 1D). After preparing the skin and completing draping, an ultrasonography convex array probe (1–5Hz, M9, Mindray Ltd, Shenzhen, China) was placed at the sagittal plane of the paravertebral region to identify the transverse process corresponding to T8, T9, and T10 through the long spinal axis (Figure 1E). 30mL ropivacaine (0.4%) was injected in the plane of the erector spinae at the T9 level (Figure 1F). The two groups were covered with the same dressings at the puncture point and incision, and dressings were retained until the end of the last follow-up in 48 hours to ensure the blind method.
Procedure
After entering the operating room, patients were given peripheral venous passage routinely and an electrocardiogram monitor (Benvision-T8, Mindray Ltd., Shenzhen, China) for monitoring electrocardiogram (ECG), blood pressure (BP), and oxygen saturation (SpO2). A portable color Doppler ultrasound (M9, Mindray Ltd, Shenzhen, China) was used to monitor the maximum width and the variation rate of the inferior vena cava under the xiphoid process. Before anesthesia induction, if a patient had the width of the inferior vena cava ≤ 1.0cm, or the variation rate of the inferior vena cava ≥ 50%, then he or she would quickly be supplied with 5mL/kg normal saline until the above two indicators reached the standard. All patients were treated with general anesthesia under tracheal intubation. 0.04mg/kg midazolam, 0.3mg/kg etomidate, 0.4μg/kg sufentanil, and 1.5mg/kg cisatracurium besylate were used for the induced anesthesia. Mechanical ventilation: VT 6–8mL/kg, respiratory rate (RR) 12–16bpm, and keeping end-tidal carbon dioxide partial pressure (PETCO2) of 35–45mmHg. Propofol of 4–10mg·kg−1·h−1 and remifentanil of 6–10μg·kg−1·h−1 were injected intravenously. Bispectral index (BIS) (186–0106, COVIDIEN, Massachusetts, the United States) was used to monitor the depth of anesthesia and adjust the use of anesthetics, and cisatracurium besylate was supplied to maintain anesthesia according to the surgical needs. After induction, radial artery puncture was performed and connected to Vigileo (MHD8, Edwards Lifesciences, California, the United States) to monitor the mean arterial blood pressure (MAP) and detect the stroke volume variation (SVV) and cardiac output (CO). The goal of SVV was not higher than 13% to guide perioperative fluid rehydration. Patients who had an intraoperative systolic BP less than 80mmHg would be given 6mg of ephedrine. Moreover, norepinephrine pump injection was used if the additional ephedrine was not effective. All the patients were sent back to the post-anesthesia care unit (PACU) after surgery. After their breathing recovered, neostigmine of 0.05 mg·kg-1 and atropine of 0.02 mg·kg-1 were injected intravenously for neuromuscular reversal therapy. Patients with a Steward score > 4 were sent back to the general ward.
Post-Operative Analgesia Scheme
All general anesthetics were stopped immediately after the surgery. Then, patients received the intramuscular injection of tramadol with loading analgesic dose (1 mg/kg), and intravenous injection of parecoxib sodium (40mg), and another 40mg of parecoxib sodium 24 hours after the surgery. All patients started patient-controlled intravenous analgesia (PCIA) before leaving PACU: 5 mg/kg tramadol, 0.5 mg/kg metoclopramide, and 100mL normal saline was injected at a speed of 2 mL/h, with 0.5mL single compression, and 15min locking time. If patients had insufficient analgesia after the surgery, doctors would be informed to perform the bedside evaluation. Whenever the patients reported a VAS score >4 or demonstrated a compulsively requisite for additional analgesia, he or she would be given a single intravenous injection of 0.1ug/kg sufentanil as the first rescue analgesia. A single intramuscular injection of 2mg morphine would be administered as the secondary rescue analgesia upon patient request.
Monitoring the Skin Temperature of Operation Areas
The body surface temperature at the T7 and T11 level of bilateral mid-axillary line, and at the T9 level of the bilateral mid-clavicular line were measured by an infrared thermometer (YHW-2, Yuwell Ltd., Jiangsu, China) when patients entered the operating room, received induction, entered PACU, and left PACU, respectively. The average value at the above three sites was calculated for analysis. A temperature probe of a monitor (MR403B, Mindray Ltd., Shenzhen, China) was placed at the intersection of the bilateral midclavicular line and at the costal margin during the surgery to record the body surface temperature at 1 hour after blocking and at 1 hour after the surgery started.
Follow-Up
Patients’ characteristics were recorded: Age, gender, BMI, ASA classification, cortical thickness (sum of the cortical thickness in biceps, triceps, scapula, and anterior superior iliac spine), time of operation, type of surgery and incision, perioperative drug usage, inferior vena cava diameter (IVC), inferior vena cava dilatation index (dIVC), SVV, CO, intraoperative heart rate (HR)/MAP, and perioperative body surface temperature of the surgical site. The primary outcomes were postoperative VAS scores. The secondary outcomes included the postoperative PCIA usage, the proportion of rescue analgesia during 48h, the skin surface temperature of the surgical site, the amount of ephedrine used during the surgery, the incidence of postoperative nausea and vomiting, time to exhaust, time to regular diet, time to the first bed-leaving, the length of hospital stay, and the serum concentration of IL-1β, PGE2 30 minutes after surgery.
Statistical Analysis
The postoperative VAS scores at difference visits were used to calculate the sample size in this study. We previously conducted a pilot trial consisting of 18 cases in the RLB group and 19 cases in the ESPB group. The average VAS scores at both the rest (2.11±1.41 vs 2.00±1.20) and at cough state (3.77±1.55 vs 3.89±1.24) in the previous trial were used for sample size calculation under the non-infertility test with a power of 80% and a two-sided significance level of 5%. Finally, The VAS score at the cough state at the 6th hour after surgery had the largest sample demand and were selected. In such instances, thirty-three cases in each group were deemed sufficient for the detection of difference. By referring to the calculation scheme of abnormal distribution data in Page et al,23 we calculated N=33*1.053=35 cases per group. We anticipated a 20% drop-out rate and thus expected that a total of 88 patients with 44 patients in each group would be necessary. Numerical data with normal distribution were presented by mean ± standard deviation (SD), and the group differences were compared by independent sample t-test. Data with abnormal distribution were presented by median (interquartile range), and compared by nonparametric rank-sum test. Counting data were presented by the number of cases and percentages, and the group difference were compared by χ2 test. A P<0.05 was considered statistically significant. SPSS 17.0 software (SPSS Inc, Chicago, IL) was performed for statistical analysis.
Results
106 patients who needed retroperitoneal laparoscopic surgery were initially included to assess for eligibility. Of whom, there were 18 patients who changed the operation method, and delayed or canceled the surgery were excluded from this study. Eventually, we recruited a total of 88 patients in this study and randomized them into RLB group (N=44) and ESPB group (N=44). During the treatment, two patients in the ESPB group who deviated the study protocol were excluded from further analysis. The remaining 86 patients including 44 in the RLB group and 42 in the ESPB group completed the follow-up assessment (Figure 2). No statistically significant differences were observed in baseline characteristics between the two groups (Age, gender, BMI, ASA classification, time of operation, the type of surgery, the type of incision, All P>0.05, Table 1). In addition, perioperative anesthesia management and usage of anesthetic drugs were not significantly different between the two groups (All P>0.05, Table 2).
 |
Table 1 Patient Characteristics and Clinical Data in the Study |
 |
Table 2 Perioperative Anesthesia Management and Consumption of Anesthetic Drugs |
 |
Figure 2 A flow chart illustrating patient inclusion. Abbreviations: RLB, retrolaminar block. ESPB, erector spine plane block. |
There was no significant difference in the IVC diameter and dIVC between the two groups after patients entered the operating room and at the beginning of induction (Figure 3A and B). The level of SVV and CO were comparable in the two groups at each time points during follow-up. Despite a slightly rising trend were presented in both groups after conducting the induction, the level of SVV at the end of the surgery was lower than that at other time points, with no significant differences been observed between the two groups (Figure 3C). The CO level of both groups showed a slightly descending trend after the induction but restored at the end of the surgery. The CO level of both groups after the induction and at the end of surgery was higher than that at other time points (Figure 3D). No significant differences were found in the intraoperative HR (Figure 4A). In terms of the MAP level, only the MAP at 10 min after the surgery start was found to be lower in the RLB group (87.20±12.42mmHg) compared to the ESPB group (95.47±12.65mmHgm, P=0.003, Figure 4B).
During the follow-up period, the differences in the VAS scores at rest state and cough state at each visit between the two groups were not significant (Figure 5A and B). After summarizing the scores at all six-time points, there was still no significant differences in the mean VAS scores and maximum VAS scores at rest state and cough state between groups (Figure 5C and D). The postoperative statistics of PCIA and analgesic drug consumption were not significantly different between the two groups (Table 3). No additional morphine was used in both groups.
 |
Table 3 PCIA and Analgesic Drug Consumption During Follow-Up |
Regarding the comparison of skin temperature at body surface, the temperature difference (TD) between the affected and healthy sides was calculated. After the surgery ended, the TD was higher in the ESPB group (−0.93±0.59 °C) compared to the RLB group (−0.53±0.31, P=0.002). And after the patients entered the PACU, the TD in the ESPB group (−0.50±0.64) was higher compared to that in the RLB group (−0.39±0.23, P=0.016, Figure S2).
Patients in neither group developed severe adverse events such as death, allergic or toxic reactions to local anesthetics, or pneumothorax, as well as severe hypotension that was difficult to reverse with ephedrine. The percentage of patients who used ephedrine was higher in the RLB group compared to the ESPB group (40.9% vs 19.0%, P=0.027). Particularly, there were 17 patients (38.6%) in the RLB group and 7 patients (16.6%) in the ESPB group used ephedrine after nerve block implementation (P=0.023). During the follow-up period, no significant difference was found in the cumulative incidence of nausea and vomiting between the two groups at each time point. Patients in the RLB group had an average shorter time to intestine exhaust than those in the ESPB group (26.53±11.21h, vs 31.99±13.57h, P=0.045). While other rehabilitation data were not significantly different (Table 4).
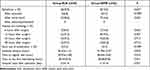 |
Table 4 Adverse Events and Postoperative Rehabilitation Data |
For the detection of plasma inflammatory factor, the RLB group (169.0, IQR: 96.5 to 407.0 pg/mL) had lower IL-1β than the ESPB group (301.0, IQR: 142.5 to 797.0 pg/mL, P=0.049) after surgery (Figure S3A), while the two groups showed no statistical significance in PGE2 at the end of surgery (Figure S3B). White blood cell count and neutrophil percentage at 24 hours after surgery were not significantly different between the two groups (Figure S3C and S3D).
Discussion
To the best of our knowledge, this is the first randomized controlled trial to investigate the analgesic efficacy of ESPB compared to RLB in retroperitoneal laparoscopic surgery. The results of this study showed that at each follow-up time point after surgery, there were no significant differences in VAS scores at rest state or cough state between two groups. The differences in mean VAS scores and maximum VAS scores were also not significant. We also demonstrated that ESPB is equivalent to RLB in terms of the consumption of anesthetic drugs during the operation and followed-up. Less than 10% of patients (4.54% vs 9.53%) in both groups proposed the needs for remedial analgesia, demonstrating that both methods provide promising postoperative analgesia during retroperitoneal laparoscopic surgery.
In terms of the postoperative patient-reported pain control, our study demonstrated that both ESPB and RLB presented a stable and sustained analgesic effect within the 48 hours after surgery either at rest or cough state. Existing reports on RLB and ESPB as the methods for postoperative analgesia were mostly discussed in thoracic and lumbar surgery24–28 and there was no study reported the direct comparison between ESPB and RLB in retroperitoneal laparoscopic surgery. Until now, the mechanism of the drug effect of RLB and ESPB has not yet been clarified. Even though the injection sites of ESPB and RLB differ only a few centimeters anatomically, RLB may prefer to take effect through the approach of PVB, that is, “deep” penetration, while ESPB mainly affects the lateral cutaneous branch and some small branches of the intercostal nerve through “transverse” penetration to produces analgesic effect.24–26 Recently, several clinical trials have demonstrated the non-inferior anesthetic effect of ESPB and RLB irrespectively compared to other nerve block methods,25,29,30 and the VAS scores were not significantly different between the two groups at any time points after surgery in our study, which was rather consistent with the results in a previous clinical trial that comparing the anesthetic effect between RLB and ESPB in breast surgery.31 It was still worth noted that previous study reported an average lower score in verbal rating scale (VRS) with the interquartile range from 1- to 2-points at rest for 24 hours postoperative among patients in both ESPB and RLB groups.
Inspired by earlier literature,32 sympathetic blockade causes increased skin temperature in the innervated area. So, after implementing unilateral nerve block, the comparison of TD between the two sides in the same patient may be used to speculate which method has more anesthetic drugs penetrate the paravertebral or even epidural space. Since the affected side is constantly exposed to air and the healthy side is always in contact with a large amount of dressing, most patients had significantly lower body temperature than the health side during the whole surgery. However, in the comparison of TD between the two sides, the decrease of affected side body temperature regarding the healthy side in the RLB group was significantly lower than that in the ESPB group at the end of surgery (P=0.002) and the time of delivery to PACU (P=0.016), indicating that more sympathetic nerve block effects reverse the decrease in the affected side body temperature in RLB group. Unfortunately, there were no existing trial focusing on the TD difference in this filed, thus the results in our study might not be conclusive enough for the comparison of anesthetic effect between RLB and ESPB.
Furthermore, the effect on hemodynamics may distinguish the analgesic difference between nerve block methods. RLB and ESPB are currently the most debating subject on which of them has the greater possibility of allowing local anesthetics to penetrate the paravertebral space. Consequently, the block at the same site and observation of its effect on hemodynamics has become strong evidence to compare which of the two methods facilitates more local anesthetics into the paravertebral space. In the present study, we concentrated on all the approaches that our institution can guide fluid rehydration, including balancing the dIVC of the two groups before induction and guiding fluid rehydration with SVV after the anesthesia induction patients in the two groups achieve consistent volume status. The results showed that compared with the ESPB group, the RLB group had a significantly higher total number of patients who used ephedrine (40.9% vs 19.0%) and the number of patients who used ephedrine after block implementation (38.6% vs 16.6%). Therefore, the MAP was lower in the RLB group than in the ESPB group after the surgery started (P=0.003), presumably owing to the better visceral analgesic effect of RLB and a more severe hemodynamics compared to ESPB after block completion.
Cadaveric studies have shown that local anesthetics can penetrate the paravertebral or even epidural space,33 and although the view has been suspected earlier, human imaging studies have found direct evidence of drug diffusion into the epidural space after RLB.16 This means that RLB as an ideal alternative to epidural block has the effect of incision analgesia, and may produce visceral analgesia and reduce neuroinflammatory response. In this analysis, we found that patients in the RLB group had an average shorter time to exhaust than those in the ESPB group (26.53±11.21 h vs 31.99±13.57 h), but unfortunately this difference does not effectively improve the prognosis of patients as there was no difference in diet, activity, or time to discharge from hospital between the two groups. Meanwhile, our results suggested a significantly lower level of IL-1β in RLB group compared to the ESPB group (P=0.049), yet the differences on postoperative PGE-2, white blood cell and neutrophil were not observed. This might be related to our inclusion of multiple surgery types. Therefore, we need more studies with a large sample size to identify whether RLB provides more value for rapid recovery of patients beyond postoperative analgesia.
There were limitations in our study. Firstly, the nerve block was performed after induction to improve the patients’ anesthesia experience, which made it difficult to assess the extent of skin paresthesia at each follow-up time point in both groups. At the same time, our study calculated the sample size based on the speculation that postoperative analgesia of ESPB were non-inferior than RLB, which might undermine the statistically power to detect the differences. Moreover, despite the study was designed to observe whether RLB and ESPB with the use of weak opioid analgesia (tramadol) would both have a satisfactory effect in the clinic practice, it might still be inappropriate to compare a single high-volume injection with multiple injections since injection area is very close in RLB and ESPB, and volume administered highly effects the drug spread. Further study investigating the differences in analgesic mechanisms between RLB and ESPB will be conducted. In addition, we included various surgeries completed by retroperitoneal laparoscopic surgery, which greatly reduced the reliability of the comparative results of postoperative inflammation levels. Therefore, the value of secondary measures needs to be further verified by more clinical randomized controlled trials.
Conclusion
Ultrasound-guided three-point RLB and single-point ESPB can provide safe and effective postoperative analgesia for retroperitoneal laparoscopic surgery. ESPB is more hemodynamically stable during surgery, and RLB can shorten the postoperative recovery time of gastrointestinal function, which has more excellent potential research value for patients’ rapid recovery.
Abbreviations
BIS, bispectral index; BMI, body mass index; BP, blood pressure; CO, cardiac output; dIVC, inferior vena cava dilatation index; ECG, electrocardiogram; ESPB, erector spine plane block; HR, heart rate; ICU, intensive care unit; IL, interleukin; IVC, inferior vena cava diameter; MAP, mean arterial blood pressure; PACU, post-anesthesia care unit; PCIA, patient-controlled intravenous analgesia; PETCO2, end-tidal carbon dioxide partial pressure; PGE2, prostaglandin E2; PVB, paravertebral block; RLB, retrolaminar block; RR, respiratory rate; SD, standard deviation; SVV, stroke volume variation; VAS, visual analogue scale; VRS, verbal rating scale.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Ethics Committee of the Affiliated Hospital of Zunyi Medical College (KLL-2019-007). Written informed consent was obtained from participants.
Consent for Publication
Written informed consent was obtained for publication.
Funding
This work was supported by Joint fund of Zunyi Science and Technology Bureau [grant number ZUNSHIKEHE.HZ (2019)97], the Department of Education Fund of Guizhou Province [grant No.KY 045-2017], and Guizhou Province Scientific and Technological Achievements Application and Industrialization Plan (Clinical Special) [grant number QianKeHe-chengguo-LC[2022]020].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Clayman RV, Kavoussi LR, Soper NJ, et al. Laparoscopic nephrectomy. N Engl J Med. 1991;324(19):1370–1371.
2. Wang B, Tian Y, Peng Y, et al. Comparative study of retroperitoneal laparoscopic versus open ipsilateral nephrectomy after percutaneous nephrostomy: a multicenter analysis. J Laparoendosc Adv Surg Tech A. 2020;30(5):520–524. doi:10.1089/lap.2019.0746
3. Jiang YL, Qian LJ, Li Z, et al. Comparison of the retroperitoneal versus transperitoneal laparoscopic adrenalectomy perioperative outcomes and safety for pheochromocytoma: a meta-analysis. BMC Surg. 2020;20(1):12. doi:10.1186/s12893-020-0676-4
4. Cho SJ, Moon HW, Kang SM, et al. Evolution of laparoscopic donor nephrectomy techniques and outcomes: a single-center experience with more than 1000 cases. Ann Transplant. 2020;25:e918189. doi:10.12659/AOT.918189
5. Flores P, Cadario M, Lenz Y, et al. Laparoscopic total nephrectomy for Wilms tumor: towards new standards of care. J Pediatr Urol. 2018;14(5):388–393. doi:10.1016/j.jpurol.2018.06.015
6. Yucel C, Ulker V, Kisa E, Koc G, Ilbey YO. Laparoscopic transperitoneal nephrectomy in non-functioning severe hydronephrotic kidneys with or without renal stone. Cureus. 2018;10(12):e3729. doi:10.7759/cureus.3729
7. Chou R, Gordon DB, de Leon-casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, And Administrative Council. J Pain. 2016;17(2):131–157. doi:10.1016/j.jpain.2015.12.008
8. Brown EN, Pavone KJ, Naranjo M. Multimodal general anesthesia: theory and Practice. Anesth Analg. 2018;127(5):1246–1258. doi:10.1213/ANE.0000000000003668
9. Richebé P, Capdevila X, Rivat C. Persistent postsurgical pain: pathophysiology and preventative pharmacologic considerations. Anesthesiology. 2018;129(3):590–607. doi:10.1097/ALN.0000000000002238
10. Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, Albrecht E. Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia. 2019;74(5):651–662. doi:10.1111/anae.14582
11. Aditianingsih D, Anasy N, Tantri AR, Mochtar CA, Mochtar CA. A randomized controlled trial on analgesic effect of repeated Quadratus Lumborum block versus continuous epidural analgesia following laparoscopic nephrectomy. BMC Anesthesiol. 2019;19(1):221. doi:10.1186/s12871-019-0891-7
12. Yuan Q, Cui X, Fei Y, Xu Z, Huang Y. Transmuscular quadratus lumborum block versus thoracic paravertebral block for acute pain and quality of recovery after laparoscopic renal surgery: study protocol for a randomized controlled trial. Trials. 2019;20(1):276. doi:10.1186/s13063-019-3359-7
13. El Shora HA, El Beleehy AA, Abdelwahab AA, et al. Bilateral paravertebral block versus thoracic epidural analgesia for pain control post-cardiac surgery: a randomized controlled trial. Thorac Cardiovasc Surg. 2020;68(5):410–416. doi:10.1055/s-0038-1668496
14. Voscopoulos C, Palaniappan D, Zeballos J, Ko H, Janfaza D, Vlassakov K. The ultrasound-guided retrolaminar block. Can J Anesth. 2013;60(9):888–895. doi:10.1007/s12630-013-9983-x
15. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–627. doi:10.1097/AAP.0000000000000451
16. Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector spinae plane block versus retrolaminar block: a magnetic resonance imaging and anatomical study. Reg Anesth Pain Med. 2018;43(7):756–762. doi:10.1097/AAP.0000000000000798
17. Yang HM, Choi YJ, Kwon HJOJ, Cho TH, Kim SH, Kim SH. Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: a cadaveric study. Anaesthesia. 2018;73(10):1244–1250. doi:10.1111/anae.14408
18. Schwartzmann A, Peng P, Maciel MA, Forero M. Mechanism of the erector spinae plane block: insights from a magnetic resonance imaging study. Can J Anaesth. 2018;65(10):1165–1166. doi:10.1007/s12630-018-1187-y
19. Liu D, Xu X, Zhu Y, et al. Safety and efficacy of ultrasound-guided retrolaminar block of multiple injections in retroperitoneal laparoscopic nephrectomy: a prospective randomized controlled study. J Pain Res. 2021;14:333–342. doi:10.2147/JPR.S282500
20. Rispoli M, Tamburri R, Nespoli MR, et al. Erector spine plane block as postoperative rescue analgesia in thoracic surgery. Tumori. 2020;106(5):388–391. doi:10.1177/0300891620915783
21. Singh S, Choudhary NK, Lalin D, Verma VK. Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: a randomized control trial. J Neurosurg Anesthesiol. 2020;32(4):330–334. doi:10.1097/ANA.0000000000000603
22. Saadawi M, Layera S, Aliste J, Bravo D, Leurcharusmee P, Tran Q. Erector spinae plane block: a narrative review with systematic analysis of the evidence pertaining to clinical indications and alternative truncal blocks. J Clin Anesth. 2021;68:110063. doi:10.1016/j.jclinane.2020.110063
23. Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515–523. doi:10.1016/S2213-2600(13)70166-8
24. Onishi E, Murakami M, Nishino R, Ohba R, Yamauchi M. Analgesic effect of double-level retrolaminar paravertebral block for breast cancer surgery in the early postoperative period: a placebo-controlled, randomized clinical trial. Tohoku J Exp Med. 2018;245(3):179–185. doi:10.1620/tjem.245.179
25. Murouchi T, Yamakage M. Retrolaminar block: analgesic efficacy and safety evaluation. J Anesth. 2016;30(6):1003–1007. doi:10.1007/s00540-016-2230-1
26. Onishi E, Toda N, Kameyama Y, Yamauchi M. Comparison of clinical efficacy and anatomical investigation between retrolaminar block and erector spinae plane block. Biomed Res Int. 2019;2019:2578396. doi:10.1155/2019/2578396
27. Tsui BCH, Fonseca A, Munshey F, McFadyen G, Caruso TJ. The erector spinae plane (ESP) block: a pooled review of 242 cases. J Clin Anesth. 2019;53:29–34. doi:10.1016/j.jclinane.2018.09.036
28. Chen N, Qiao Q, Chen R, Xu Q, Zhang Y, Tian Y. The effect of ultrasound-guided intercostal nerve block, single-injection erector spinae plane block and multiple-injection paravertebral block on postoperative analgesia in thoracoscopic surgery: a randomized, double-blinded, clinical trial. J Clin Anesth. 2020;59:106–111. doi:10.1016/j.jclinane.2019.07.002
29. Aksu C, Şen MC, Akay MA, Baydemir C, Gürkan Y. Erector spinae plane block vs quadratus lumborum block for pediatric lower abdominal surgery: a double blinded, prospective, and randomized trial. J Clin Anesth. 2019;57:24–28. doi:10.1016/j.jclinane.2019.03.006
30. Gürkan Y, Aksu C, Kuş A, Yörükoğlu UH. Erector spinae plane block and thoracic paravertebral block for breast surgery compared to IV-morphine: a randomized controlled trial. J Clin Anesth. 2020;59:84–88. doi:10.1016/j.jclinane.2019.06.036
31. Sotome S, Sawada A, Wada A, Shima H, Kutomi G, Yamakage M. Erector spinae plane block versus retrolaminar block for postoperative analgesia after breast surgery: a randomized controlled trial. J Anesth. 2021;35(1):27–34. doi:10.1007/s00540-020-02855-y
32. Di Filippo A, Natale V, Del Po F, Ciapetti M, Bressan F, Falchi S. Skin temperature during sympathetic block: a clinical comparison of bupivacaine 0.5% and ropivacaine 0.5% or 0.75%. Anaesth Intensive Care. 2006;34(3):334–337. doi:10.1177/0310057X0603400311
33. Sabouri AS, Crawford L, Bick SK, Nozari A, Anderson TA. Is a retrolaminar approach to the thoracic paravertebral space possible?: a human cadaveric study. Reg Anesth Pain Med. 2018;43(8):864–868. doi:10.1097/AAP.0000000000000828
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




