Back to Journals » Journal of Pain Research » Volume 16
Effectiveness of Thoracic Wall Blocks in Video-Assisted Thoracoscopic Surgery, a Network Meta-Analysis
Authors Scorsese G , Jin Z, Greenspan S, Seiter C, Jiang Y, Huang MB , Lin J
Received 14 November 2022
Accepted for publication 3 March 2023
Published 7 March 2023 Volume 2023:16 Pages 707—724
DOI https://doi.org/10.2147/JPR.S396530
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ellen M Soffin
Giacomo Scorsese,1,* Zhaosheng Jin,1,* Seth Greenspan,1 Christopher Seiter,1 Yujie Jiang,1,2 Michael B Huang,3 Jun Lin1
1Department of Anesthesiology, Stony Brook University Health Science Center, Stony Brook, NY, 11794-8480, USA; 2Department of Anesthesiology and Pain Medicine, University of Washington, Seattle, WA, 98195-6540, USA; 3Health Sciences Library, Stony Brook University, Stony Brook, NY, 11794-8034, USA
*These authors contributed equally to this work
Correspondence: Giacomo Scorsese, Department of Anesthesiology, Stony Brook University Health Science Center, Stony Brook, NY, USA, Tel +1631637-1457, Fax +1631444-2907, Email [email protected]
Introduction: Thoracic epidural analgesia (TEA) and thoracic paravertebral blocks (PVB) are well-established techniques for pain management in thoracotomy. Here, we examine the efficacy of various thoracic fascial plane blocks vs TEA and PVB for intraoperative and postoperative analgesia for video assisted thoracoscopy surgery (VATS) with network meta-analysis.
Methods: A search for prospective randomized control studies using adult patients undergoing VATS with general anesthesia. The interventions of interest were any regional anesthesia techniques used for postoperative pain control after VATS. Primary outcomes of interest were 24-hour opioid requirement and 24-hour pain scores. A Bayesian network meta-analysis was conducted.
Results: We identified 42 studies that fulfilled our inclusion criteria. For patients who underwent VATS, TEA (MD = − 27MME, 95% CI = − 46.2 to − 9MME), ESP (MD = − 20MME, 95% CI – 33 to − 7.9MME), PVB (MD = − 15MME, 95% CI = − 26 to − 4.5MME) demonstrated significant opioid sparing efficacy, as well as reduction in cumulative 24-hour static pain scores. However, exclusion of one study due to high risk of bias revealed that TEA did not significantly reduce opioid consumption, nor did it reduce the incidence of PONV, pulmonary complications, or LOS when compared to ESP, SAP, PVB, ICN, or PECS blocks.
Conclusion: Our findings suggest that TEA did not provide superior pain relief compared to ESP, SAP, PVB, ICN, or PECS blocks following VATS. Therefore, we propose ESP as a suitable intervention for the prevention of postoperative pain after VATS.
Keywords: fascial plane blocks, thoracic epidurals, post-operative analgesia, postoperative nausea and vomiting, video assisted thoracoscopic surgery
Introduction
Managing postoperative pain after thoracic surgery is a significant challenge for the perioperative physician. Inadequate pain relief has been associated with ineffective breathing, reduced cough and difficulty clearing secretions, which increases the risk of postoperative atelectasis, pneumonia, and pulmonary embolism.1
Video-assisted thoracoscopic surgery (VATS) has been widely used to surgically manage lung disease since its introduction in the early 1990s. Unlike traditional surgical approaches involving wide surgical access via thoracotomy, VATS performs the same procedure through small port sites in the patient’s chest wall.2 Although VATS continues to emerge as the new standard surgical procedure for minor and major lung surgery, the pain related to port sites and chest tube placement can still be moderate to severely painful.3
Regional anesthesia has gained significant popularity over the last two decades by providing adjuncts and even alternatives to general anesthesia. However, while thoracic epidural analgesia (TEA) and thoracic paravertebral blocks (PVB) are well-established techniques for thoracotomy, there exists no standard of regional analgesia for the minimally invasive thoracoscopic approach.3 Conversely, a variety of regional anesthesia techniques have been studied in patients undergoing VATS, with varying degrees of success. The number regional anesthesia options, and the number of possible head-to-head comparison necessitates simultaneous comparisons of all interventions in order to identify the most effective analgesic option after VATS.
This network meta-analysis is therefore conducted to evaluate the efficacy of various regional anesthesia options and systemic analgesia for intraoperative and postoperative pain control for VATS. Regional anesthesia techniques examined included serratus anterior plane (SAP) block, erector spinae plane (ESP) block, intercostal nerve (ICN) block, pectoralis nerve block (PECS), thoracic PVB, and TEA; each technique was evaluated in terms of analgesic efficacy and safety.
Methods
Study Objectives
Our aim was to assess the analgesic efficacy of various regional anesthetic techniques for postoperative pain control following VATS. The primary outcomes are 24-hour postoperative opioid requirement, defined as the total amount of opioids administered 24-hours after emergence from anesthesia, and area under the curve (AUC) of 24-hour postoperative static pain score. The latter is a composite outcome derived from pain scores and their corresponding time points. Secondary outcomes included AUC of 24-hour dynamic pain scores (including pain with cough, deep breathing, or movement), the incidence of post-operative nausea and vomiting (PONV), pulmonary complications, length of stay (LOS), block related adverse events and patient satisfaction.
Study Selection
We included RCTs of adult patients undergoing VATS under general anesthesia, excluding conference abstracts. Screening for studies was conducted independently by at least two of the authors; discrepancies were discussed after the search process. The interventions of interest were any regional anesthesia techniques used for postoperative pain control after VATS. Comparison could be between different regional anesthesia techniques, or regional anesthesia compared to placebo/systemic analgesia. Studies were included if they reported at least one primary outcome. We only included studies which are published in English.
A preliminary search revealed limited studies investigating the efficacy of continuous blocks, with heterogeneous methodology; a decision was therefore made during the protocol design stage to exclude continuous block techniques except for TEA. Other exclusion criteria included pediatric studies and studies which compared different regional anesthesia formulations.
Search Strategy
This study conformed to the Preferred Reporting Items for Systematic reviews and Meta-analysis (PRISMA) statement.4 The study protocol is registered on PROSPERO, registration number CRD 42022313313. We used search terms related to the surgical procedure, each of the included regional anesthesia techniques and their Boolean combinations in PubMed, EMBASE (Ovid), (CENTRAL), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Web of Science citation index. The full search protocol is included in the Electronic Supplementary Material (ESM, Supplementary Table 1).
Data Extraction
Data extraction was done according to a Microsoft excel based pro-forma. All data was checked by a second author. Extracted data included bibliographical information, study design, and primary and secondary outcomes. For studies with incomplete data, we contacted the corresponding authors directly with relevant requests. In the event no replies were received, we attempted the following for data extraction. When NRS was reported as non-parametric data (with median and interquartile range), we estimated the mean and standard deviation assuming normal distribution using methods described by Cochrane (standard deviation = interquartile range/1.35).5 When study results are only displayed in graphical form, two authors independently extracted the data using WebPlot Digitizer as previously described.6,7
Statistical Analysis
A Bayesian network meta-analysis was conducted in R studios using packages “BUGSnet”, “rjags” and “netmeta”. For each outcome, a network plot was constructed to summarize the direct comparisons from the included studies. In brief, each intervention was represented by a node, and edges represented studies that compared the connected interventions weighted by the number of studies reporting said comparison. When comparing postoperative opioid requirements, opioids given in the 24-hours after surgery were standardized into intravenous milligram morphine equivalent (MME). The scores were standardized to a 0 to 100 scale when comparing the pain severity. The AUC was then calculated based on the time-weighted cumulative pain severity over the 24 hours after surgery, with a weighted mean variance of observations.8 Each point of difference in the pain score AUC represents a 1-point reduction in the pain score for an hour duration. In other words, 24 points reduction could be equated to a 1-point reduction in the pain score for 24 hours. Due to the inherent variation in the reporting of subjective pain and the variation in the efficacy of regional anesthesia procedures between practitioners, random effects models were used for all analyses. Network meta-analysis models were generated with 10,000 adaptations, a burn-in of 50,000, and 100,000 iterations.9 The findings of the network meta-analysis were reported as mean difference (MD) for continuous variables and risk ratio (RR) for dichotomous variables. The model fit was assessed using fit statistics and by inspecting the leverage plot. Consistency was assessed by comparing the NMA model with an unrelated mean effect.10 Publication bias was assessed using a comparison-adjusted funnel plot.
We performed a subgroup analysis dividing studies according to postoperative chest tube use, and a sensitivity analysis removing studies with high risk of bias. Two additional sensitivity analyses were added post hoc, these were: exclusion of patients received surgical site local anesthetic infiltration, and exclusion of patients were aware of whether they received an intervention rather than “no block”.
Potential risk of bias was evaluated at study and outcome level, with all assessments done by two authors independently and any disagreements discussed and resolved with the senior author as the adjudicator. We used the RoB 2: A revised Cochrane risk-of-bias tool for randomized trials, a 5-item questionnaire designed for assessing clinical trials. Each study is assessed on the randomization process, bias due to intervention deviations, missing outcomes, bias in outcome measurement, selective reporting and summarized as an overall grading as low, intermediate (some concerns) or high risk.11 We used GRADEpro Guideline Development Tool (GRADEpro GDT, McMaster University, 2015) to assess the certainty of the conclusion that could be drawn from the available evidence.
Results
The search was last completed on Aug 22, 2022; with active literature surveillance until October 6th, 2022. The literature search identified a total of 2307 studies. After removing duplicates, 1717 studies underwent title and abstract review; with 183 studies subsequently reviewed as full-text; 42 studies were ultimately included for analysis (Figure 1).12–53 The characteristics of the included studies were summarized in Table 1. The risk of bias evaluations of each study are summarized in Figure 2 and the justification of the gradings were listed in the Supplementary Table 2..
 |
Table 1 Characteristics of Included Studies |
 |
Figure 1 Search flowchart. |
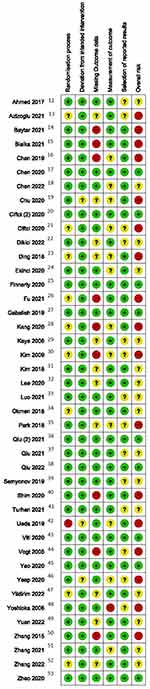 |
Figure 2 Risk of bias. |
Treatment Comparison
The following anesthesia techniques were studied among the included studies: TEA, PVB, ESP block, SAP block, PECS block, and ICN block. The approach to ESP was between T4 to T6, SAP approaches varied between T3 and T8. Multilevel approaches were taken with PVB (which varied from T3-T4 to T4-T8) and ICN (T4 to T7-9). Local anesthetics used included 0.25% to 0.5% bupivacaine and ropivacaine, adjuncts included epinephrine, dexamethasone and epidural opioids; the exact dosing in each study is reported in the Supplementary Table 3. In the study arms, which did not receive active regional anesthesia, patients were given no blocks or block with saline.
24-Hour Opioid Requirement
There were 28 studies that reported 24-hour opioid requirement. Data were available for all 6 analgesic interventions listed above, resulting in 14 unique pairwise comparisons. The most common direct comparisons were ESP vs PVB, PVB vs no block, and SAP vs no block. When compared to the “no block” arm, TEA (MD = −27MME, 95% CI = −46.2 to −9MME), ESP (MD = −20MME, 95% CI –33 to −7.9MME), PVB (MD = −15MME, 95% CI = −26 to −4.5MME) demonstrated significant opioid sparing efficacy, while SAP had no significant benefit (MD = −12MME, 95% CI = −26 to +0.4MME) (Figure 3). There were no significant differences between interventions. Exclusion of the (two) studies that employed surgical site infiltration as the “no block” arm did not result in significant changes in the findings. Subgroup analysis of 16 studies that reported using chest drains identified TEA, PVB, ESP, and ICN as effective interventions; whereas 13 studies that did not report using chest drains identified only TEA and ESP as effective interventions.
There was significant overall heterogeneity (I2=0.93, Tau=1.09), while pairwise analyses demonstrated moderate to high heterogeneities in most comparisons. Comparison-adjusted funnel plot did not demonstrate significant publication bias (Egger’s regression p = 0.89, Begg-Mazumdar p = 0.26). The unrelated mean effects model found that the posterior mean deviance contributions for most studies were close to 1 in both models; there was, however, one point that fit poorly in the consistency model (the study by Yeap et al, which is a high risk of bias study that did not report adequate participant and study personnel blinding). Exclusion of the study led to improvement in the model fit. The resultant model altered the findings for TEA and SAP; TEA was no longer opioid sparing compared to the “no block” arm, whereas SAP had significant opioid sparing efficacy (MD = −12MME, 95% CI = –23 to –2.4MME).
Sensitivity analysis was performed using only low or moderate risk of bias studies (18 studies). Notably, all TEA studies were excluded, PVB and ESP remained effective, while ICN and SAP were also noted to be effective. A second sensitivity analysis was conducted by excluding studies that did not have blinding measures for patients who received no regional anesthesia (22 studies). TEA, PVB and ESP were noted to be more effective than no block, whereas SAP and other interventions showed no difference. The evidence grades for the opioid-sparing effect of PVB, and ESP are low, and the grade of evidence for TEA is very low (Table 2). There may be very low-grade evidence for the opioid sparing efficacy of SAP from the sensitivity analyses, but the primary analysis did not support its efficacy.
 |
Table 2 GRADE Summary of the Primary Outcomes |
24-Hour Static Pain Score AUC
There were 38 studies that reported 24-hour static pain scores. Data were available for all 6 analgesic interventions. Including the no-block arm, there were 13 unique pairwise comparisons, and the most common were ESP vs PVB, PVB vs no block and SAP vs no block. When compared to the “no block” arm, ESP (MD = −29, 95% CI –43 to −16), SAP (MD = −27, 95% CI = −37 to –16), TEA (MD = −24, 95% CI = −42 to −7.6), and PVB (MD = −20, 95% CI = to −30 to −9.4) demonstrated significant reduction in the pain score AUC (Figure 4). No differences were seen between the analgesic techniques.
Exclusion of the three studies that employed surgical site infiltration as the “no block” arm did not result in significant changes in the findings. Subgroup analysis of 15 studies which reported the use of chest drains reported epidural analgesia, ESP, SAP, TEA and PVB as effective interventions for reducing postoperative pain; whereas 21 studies which did not report chest drain use identified only ESP and SAP as effective interventions.
There was significant overall heterogeneity (I2=0.92, Tau=1.00), while pairwise analyses demonstrated moderate to high heterogeneities in most comparisons. The unrelated mean effects model did not find evidence of significant inconsistency as the posterior mean deviance contributions for most studies were close to 1 in both models. One study had somewhat poor fit in both models – a moderate risk of bias study by Qui et al comparing no block to SAP.37 Comparison-adjusted funnel plot reported possible publication bias (Egger’s regression p < 0.01, Begg-Mazumdar p = 0.07).
Sensitivity analysis was performed using only low or moderate risk of bias studies (21 studies). TEA was found to no longer be effective for reducing postoperative pain; there were no significant changes to the results of the remaining interventions. A second sensitivity analysis excluded studies which did not have blinding measures for patients who received no regional anesthesia (26 studies). There were no significant changes compared to the primary analysis. The grade of evidence for the analgesic effect of chest wall blocks is very low throughout (Table 2).
Dynamic Pain Score
There were 24 studies that reported 24-hour dynamic pain scores. Data were available for ESP, PVB, SAP, PECS, and TEA, resulting in 10 unique pairwise comparisons. The most common direct comparisons were between no block vs PVB and SAP. When compared to the “no block” arm, ESP (MD = −31, 95% CI –44 to −18), TEA (MD = −27, 95% CI = −42 to −12), PVB (MD = −25, 95% CI = −35 to −16) and SAP (MD = −24, 95% CI –36 to −12) demonstrated significant opioid sparing efficacy.
The unrelated mean effects model did not demonstrate better fit compared to the study mode, as posterior mean deviance contributions for most studies were close to 1 in both models. There was significant overall heterogeneity (I2=0.92, Tau=1.03), while pairwise analyses demonstrated moderate to high heterogeneities in most comparisons. Comparison-adjusted funnel plot reported possible publication bias (Egger’s regression p = 0.02, Begg-Mazumdar p = 0.07). The grades of evidence for the chest wall blocks reducing pain on movement are low (downgraded for heterogeneity and risk of bias, Supplementary Table 2).
PONV
There were 30 studies which reported the incidence of PONV. Data were available for all 6 interventions and the no-block arm, resulting in 15 unique pairwise comparisons. The most common direct comparisons were ESP vs PVB, PVB vs no block and SAP vs no block. When compared to the “no block” arm, ESP (RR = 0.33, 95% CI = 0.21 to 0.53), PECS (RR = 0.33, 95% CI = 0.1 to 0.95), ICN (RR = 0.36, 95% CI = 0.14 to 0.89), PVB (RR = 0.38, 95% CI = 0.24 to 0.59) and SAP (RR = 0.5, 95% CI = 0.33 to 0.7), all demonstrated significant reduction in the risk of PONV. Interestingly, TEA was not associated with reduced risk of PONV compared with systemic analgesia but was associated with greater risk of PONV when compared to ESP (RR = 2.6, 95% CI = 1.3 to 5.4) and PVB (RR = 2.3, 95% CI = 1.2 to 4.6).
There was moderate overall heterogeneity (I2=0.58, Tau=0.79), while pairwise analyses demonstrated low to moderate heterogeneity in most comparisons. The unrelated mean effects model did not demonstrate a better fit compared to the study model as both had studies that were poorly fit. Those studies were a moderate risk of bias study by Qiu et al comparing no block to SAP,37 a high-risk study by Yoshioka which compared no block to TEA,48 and a high-risk study by Shim which compared ESP to no block.40 This likely represents heterogeneity in PONV risk factors and prophylactic treatment, which were inconsistently reported so further analysis is not possible. Comparison-adjusted funnel plot did not demonstrate significant publication bias (Egger’s regression p = 0.06, Begg-Mazumdar p = 0.32). The grade of evidence for the PONV reducing benefit of chest wall blocks is low (downgraded for heterogeneity and risk of bias, Supplementary Table 2).
Length of Stay
There were 16 studies which reported the length of stay, which covered all 6 interventions, resulting in 7 unique pairwise comparisons. There was no significant difference between the interventions in terms of the length of hospital stay.
Block Related Complications
Thirty-two of the 42 studies reported the incidence of block-related complications. Due to the inherent heterogeneity in diagnosing and classifying block-related complications, we did not attempt to perform quantitative analysis.
Twenty-three studies reported no block-related complications in any of the participants. Two studies by Bialka15 and Chu19 randomized a total of 62 patients to receiving ultrasound guided PVB, of which there were 8 cases of failed block. Ueda42 randomized 22 patients who underwent TEA, with two cases of block failure and 2 cases of accidental catheter removal. Kim31 reported 3 incidents of SAP partial block failures.
Chen17 randomized 24 patients each to receiving PVB or ICN block and reported that 4 patients in the PVB arm and 5 patients in the ICN arm developed a block site hematoma. No further complications were reported in relation to the hematoma; notably, there were no cases of hematoma in the ESP arm. Ding23 and Baytar14 allocated a total of 67 patients to the PVB arm and reported 6 cases of hypotension; Ding also reported 11 cases of hypotension among 32 patients who received TEA. Pruritus was reported in relation to TEA in two studies.30,48
Pulmonary Complications
There were 14 studies that examined postoperative pulmonary complications. Data were available for all six interventions, including no block. Due to the inherent heterogeneity in the type of surgery and underlying patient risk factors, we did not perform quantitative analysis on pulmonary complications. Two studies reported postoperative air-leak,42,48 and four reported no postoperative pulmonary complications.41,43,44,52 The remaining 8 studies reported incidents of pneumonia and/or atelectasis; however, there were no statistically significant differences in the incidence of these complications between groups in any of the studies.16,19,25,28,30,31,35,47
Patient Satisfaction
There were 9 studies which reported patient satisfaction. Due to the heterogeneity of scoring systems, we did not perform quantitative analysis on patient satisfaction. Two studies reported that patients had better satisfaction with PVB than without.29,50 One study reported that an opioid-sparing group that received PVB had better satisfaction than routine opioid analgesia.38 Similarly, two studies reported that SAP led to better patient satisfaction.22,35 There was one study each showing that ESP45 and PECs33 improved patient satisfaction. Kim et al reported in their study that TEA did not result in significant improvement in patient satisfaction when compared to no block.30 When comparing two different analgesic techniques (TEA vs PVB46 and PVB vs SAP14), there were no significant differences in patient satisfaction.
Discussion
Since the start of the 20th century, opioids have been the main analgesic option for severe postoperative pain control. The therapeutic goal is to titrate the lowest dose of opioids necessary to treat pain and ease suffering, while mitigating side effects such as respiratory depression, pruritus, nausea, vomiting, and sedation. Due to the limitations of opioids, perioperative multimodal anesthesia has evolved to incorporate various combinations of analgesics and regional anesthetic techniques.54
While TEA has been a popular adjuvant anesthetic technique for thoracic surgery for thoracotomy, the trend toward more minimally invasive techniques requires the physician anesthesiologist to adapt accordingly. In many situations, the risks, inefficiencies, and difficulties of epidurals versus systemic analgesia or fascial plane blocks may outweigh their potential benefits. In general, serious complications following placement of TEA are rare. In fact, the incidence seems to diverge in the literature depending on the type of patient and duration a catheter remains in situ (ie, obstetrical patient vs non-obstetrical patient). Studies conducted on laboring parturients receiving lumbar epidural analgesia have shown vanishingly low complications, likely owing to the short duration of catheterization and lack of exogenous anticoagulation.55 Conversely, when placed in non-obstetrical patients, the incidence of spinal hematoma and epidural abscess is typically higher, with a reported incidence of 18.5 per 100,000 and 7.2 per 100,000 catheterizations, respectively.56 However, the Third National Audit Project discovered that regardless of the complication, the incidence of permanent injury ranged from a pessimistic value of 4.2/100,000 to an optimistic value of 2.0/100,000.57 In contrast, clinically significant hypotension (15–33%), nausea and vomiting (30%), inadvertent dural puncture (1.5%) and even failure of epidural anesthesia (32%) were far more frequent clinical problems.15,58,59 Therefore, alternative fascial plane blocks may provide a more optimal risk benefit ratio than epidural catheters in the appropriate clinical context.
Two recent network meta-analyses by Jo et al and Lin et al have both attempted to examine the efficacy of thoracic fascial planes blocks in VATS. Jo et al found that patients undergoing VATS who received PVB, ESP, SAP, and ICN blocks had lower 24-hour opioid consumption; with PVB and ESP having the greatest analgesic effect overall based on pain scores.60 However, their study excluded epidural interventions. This provides limited perspective on the efficacy of the various blocks compared to the current standard in post-operative analgesia.61
Lin et al, who performed an analysis of 16 RCTs, found that TEA, PVB, and ESP offered better analgesia than other blocks when measured by 24-hour postoperative pain scores.62 However, their study protocol included both single-shot blocks and those with a continuous peripheral nerve catheter, which produces confounding results in relative pain scores due to the continuous infusion of analgesic medications. Furthermore, they excluded papers comparing fascial plane blocks to placebo/sham block, and their primary outcome was solely pain score rather than including postoperative opioid consumption.
Our network meta-analysis of 42 RCTs found that patients who underwent VATS and received TEA, ESP, or PVB had significantly lower 24-hour opioid requirements as well as lower cumulative pain scores. Whereas, SAP had lower cumulative pain scores without a reduction in 24-hour opioid consumption. In contrast, PECS, and ICN were not associated with significant analgesic benefits as measured by opioid requirement and pain score. In consideration of the methodological differences between our studies and the recently published network meta-analysis, we found that none of the interventions offered superior pain control over another in either 24-hour opioid consumption or cumulative pain scores. Additionally, the opioid sparing benefit of TEA in our study was primarily driven by a high-risk-of-bias study by Yeap et al, which reported significantly higher treatment effect with TEA compared to other studies.46 Furthermore, the analgesic efficacy of TEA is only supported by studies with high risk of bias. Therefore, our recommendations are consistent with the 2022 published guidelines from The PROSPECT Working Group, which support the use of PVB or ESPB for VATS and rather than TEA for post-operative analgesia.63
Despite the reduction in opioid consumption in the TEA group, there was no significant risk reduction in PONV, in comparison to no block. Conversely, all the fascial plane blocks (ESP, ICN, PEC, PVB, and SAP) reduced the risk of PONV in comparison to no block. The PONV associated with TEA is likely due to the direct consequences of sympathectomy and its effect on the cardiovascular and gastrointestinal systems. However, since opioid medication were used in combination with several epidural solutions, they are systemic effect cannot be excluded. Additionally, we found that ESP, TEA, SAP, PEC and PVB were all effective in reducing cumulative 24-hour dynamic pain scores. While these findings are theoretically associated with improved clearance of secretions and pulmonary function, notably, none of the clinical trials reported any significant differences in the incidents of pulmonary complications (ie, atelectasis or pneumonia) between any of the interventions. Ultimately, any differences observed in dynamic and static 24-hour AUC pain scores also did not contribute to decreased LOS.
Regarding the safety and efficiency of the examined interventions, we found that most studies had no block-related complications. However, of the 9 studies which reported complications the most common issue was block failure, accidental catheter removal as well as hypotension, particularly with thoracic PVB and TEA. While ICN block was associated with a rare occurrence of block site hematoma, it did not result in lasting disability.
There are several potential limitations of our study. Namely, there were only a limited number of RCTs for certain treatment modalities (ie, 2 for PEC); most of the RCTs had a low sample size (N<100) which could lead to additional variance in the results. The non-opioid post-operative analgesic regimens were inconsistent across studies (ie, non-optimized dosage and frequency of acetaminophen, ibuprofen, etc.). There were also risk of bias concerns with several included studies, 17 of the 47 included studies were graded as overall high risk of bias, the most common causes of concern included patient attrition as well as lack of study registration. Another potential source of bias is whether the epidural solutions contained opioids. While opioid regiments were all converted to MME in this study, these conversions may not represent the actual potency ratio of these medications, especially when given via the neuraxial space. A final substantial limitation our study was the examination of 24-hour AUC pain scores at rest and with activity (ie, dynamic). Whereas the acute post-operative pain following VATS can typically last for days we sought to highlight the most painful period during patients’ postoperative course, that is the 0–24 hours following surgery.64
Looking forward, there are several areas for further exploration surrounding regional analgesic modalities and thoracoscopic procedures. Future considerations worth mentioning include efficacy of pre-emptive vs post-operative nerve blocks, utilization of different medication formulations, and evaluation of regional analgesia modalities other than local anesthetics (ie, radiofrequency ablation and cryoablation).
While there is no standardized regimen for effective postoperative pain management, distinct techniques such as TEA, PVB, ESP, SAP, PECS, and ICN have become popular adjuncts for intraoperative and postoperative pain control. Our findings show that TEA did not provide superior pain relief, nor did it reduce the incidence of PONV, pulmonary complications, or LOS. Additionally, PVB and TEA were associated with a higher rate of block failure and hypotension. Collectively, these findings suggest that TEA and PVB may be unfavorable for post-operative analgesia following VATS. Based on our findings, we propose ESP as a suitable intervention for the prevention of postoperative pain after VATS.
Abbreviations
TEA, Thoracic Epidural analgesia; ESP, Erector Spinae Plane; ICN, Intercostal nerve; SAP, Serratus Anterior Plane; PVB, Paravertebral Block; LA, Local Anesthesia infiltration; PECS, Pectoralis; PONV, Post-operative Nausea and vomiting; VATS, Video Assisted Thoracoscopic Surgery; MME, Milligram Morphine Equivalent; ERAS, Enhanced Recovery After Surgery; RCT, Randomized Control Trial; AUC, Area Under the Curve; LOS, Length of Stay; ESM, Electronic Supplementary Material.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Broseta AM, Errando C, De Andrés J, Díaz-Cambronero O, Ortega-Monzó J. Serratus plane block: the regional analgesia technique for thoracoscopy? Anaesthesia. 2015;70(11):1329–1330. doi:10.1111/anae.13263
2. Mineo TC, Ambrogi V. A glance at the history of uniportal video-assisted thoracic surgery. J Vis Surg. 2017;3:157. doi:10.21037/jovs.2017.10.11
3. Steinthorsdottir KJ, Wildgaard L, Hansen HJ, Petersen RH, Wildgaard K. Regional analgesia for video-assisted thoracic surgery: a systematic review. Eur J Cardiothorac Surg. 2014;45(6):959–966. doi:10.1093/ejcts/ezt525
4. Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–784. doi:10.7326/m14-2385
5. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. Available from: https://handbook-5-1.cochrane.org/chapter_7/7_7_3_5_mediansand_interquartile_ranges.htm.
6. Morton RW, Murphy KT, McKellar SR, et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br J Sports Med. 2018;52(6):376–384. doi:10.1136/bjsports-2017-097608
7. Nielsen S, Degenhardt L, Hoban B, Gisev N. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol Drug Saf. 2016;25(6):733–737. doi:10.1002/pds.3945
8. Wolfsegger MJ. Establishing bioequivalence in serial sacrifice designs. J Pharmacokinet Pharmacodyn. 2007;34(1):103–113. doi:10.1007/s10928-006-9037-x
9. Béliveau A, Boyne DJ, Slater J, Brenner D, Arora P. BUGSnet: an R package to facilitate the conduct and reporting of Bayesian network Meta-analyses. BMC Med Res Methodol. 2019;19(1):196. doi:10.1186/s12874-019-0829-2
10. Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making. 2013;33(5):641–656. doi:10.1177/0272989x12455847
11. Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. doi:10.7326/0003-4819-158-4-201302190-00009
12. Ahmed Z, Samad K, Ullah H. Role of intercostal nerve block in reducing postoperative pain following video-assisted thoracoscopy: a randomized controlled trial. Saudi J Anaesth. 2017;11(1):54–57. doi:10.4103/1658-354x.197342
13. Azizoglu M, Yapici D, Bayulgen A, Sagun A, Ozdemir L, Rumeli S. The effect of ultrasound-guided serratus anterior plane block in addition to intrathecal morphine on early postoperative period after video-assisted thoracoscopic surgery. Turk Gogus Kalp Damar Cerrahisi Dergisi. 2021;29(4):471–479. doi:10.5606/tgkdc.dergisi.2021.20804
14. Baytar MS, Yilmaz C, Karasu D, Baytar C. Comparison of ultrasonography guided serratus anterior plane block and thoracic paravertebral block in video-assisted thoracoscopic surgery: a prospective randomized double-blind study. Korean J Pain. 2021;34(2):234–240. doi:10.3344/kjp.2021.34.2.234
15. Bialka S, Sliwczynska M, Marciniak A, Czyzewski D, Misiolek H. An assessment of the effectiveness of regional analgesia after VATS measured by an objective method for assessing testosterone, cortisol, a-Amylase, sIgA, and b-endorphin levels a randomised controlled trial. Article. Endokrynol Pol. 2021;72(2):133–142. doi:10.5603/EP.A2021.0004
16. Chen G, Li Y, Zhang Y, Fang X. Effects of serratus anterior plane block for postoperative analgesia after thoracoscopic surgery compared with local anesthetic infiltration: a randomized clinical trial. J Pain Res. 2019;12:2411–2417. doi:10.2147/jpr.S207116
17. Chen N, Qiao Q, Chen R, Xu Q, Zhang Y, Tian Y. The effect of ultrasound-guided intercostal nerve block, single-injection erector spinae plane block and multiple-injection paravertebral block on postoperative analgesia in thoracoscopic surgery: a randomized, double-blinded, clinical trial. J Clin Anesth. 2020;59:106–111. doi:10.1016/j.jclinane.2019.07.002
18. Chen Q, Liang J, Liang L, Liao Z, Yang B, Neutrophil-to-Lymphocyte QJ. Ratio as an Indicator of opioid-induced immunosuppression after thoracoscopic surgery: a randomized controlled trial. J Pain Res. 2022;15:1855–1862. doi:10.2147/jpr.S371022
19. Chu H, Dong H, Wang Y, Niu Z. Effects of ultrasound-guided paravertebral block on MMP-9 and postoperative pain in patients undergoing VATS lobectomy: a randomized, controlled clinical trial. BMC Anesthesiol. 2020;20(1):59. doi:10.1186/s12871-020-00976-1
20. Ciftci B, Ekinci M, Celik EC, Tukac IC, Bayrak Y, Atalay YO. Efficacy of an ultrasound-guided erector spinae plane block for postoperative analgesia management after video-assisted thoracic surgery: a prospective randomized study. J Cardiothorac Vasc Anesth. 2020;34(2):444–449. doi:10.1053/j.jvca.2019.04.026
21. Çiftçi B, Ekinci M, Çelik EC, et al. Ultrasound-guided erector spinae plane block and thoracic paravertebral block for postoperative analgesia management following video-assisted thoracic surgery: a prospective, randomized, controlled study. JARSS. 2020;28(3):170–178. doi:10.5222/jarss.2020.07769
22. Dikici M, Akesen S, Yavascaoglu B, Bayram AS, Kaya FN, Gurbet A. Comparison of intraoperative and post-operative effects of serratus anterior plane block performed with ultrasound and infiltration block in patients undergoing video-assisted thoracoscopic surgery. Randomized Controlled Trial. Agri Dergisi. 2022;34(1):23–32. doi:10.14744/agri.2021.22605
23. Ding W, Chen Y, Li D, et al. Investigation of single-dose thoracic paravertebral analgesia for postoperative pain control after thoracoscopic lobectomy - A randomized controlled trial. Int J Surg. 2018;57:8–14. doi:10.1016/j.ijsu.2018.07.006
24. Ekinci M, Ciftci B, Gölboyu BE, et al. Trial to compare serratus anterior plane block and erector spinae plane block for pain management following thoracoscopic surgery. Pain Med. 2020;21(6):1248–1254. doi:10.1093/pm/pnaa101
25. Finnerty DT, McMahon A, McNamara JR, Hartigan SD, Griffin M, Buggy DJ. Comparing erector spinae plane block with serratus anterior plane block for minimally invasive thoracic surgery: a randomised clinical trial. Br J Anaesth. 2020;125(5):802–810. doi:10.1016/j.bja.2020.06.020
26. Fu Z, Zhang Y, Zhou Y, et al. A comparison of paravertebral block, erector spinae plane block and the combination of erector spinae plane block and paravertebral block for post-operative analgesia after video-assisted thoracoscopic surgery: a randomised controlled trial. J Minim Access Surg. 2021;08:08.
27. Gaballah KM, Soltan WA, Bahgat NM. Ultrasound-guided serratus plane block versus erector spinae block for postoperative analgesia after video-assisted thoracoscopy: a pilot randomized controlled trial. J Cardiothorac Vasc Anesth. 2019;33(7):1946–1953. doi:10.1053/j.jvca.2019.02.028
28. Kang K, Meng X, Li B, et al. Effect of thoracic paravertebral nerve block on the early postoperative rehabilitation in patients undergoing thoracoscopic radical lung cancer surgery. World J Surg Oncol. 2020;18(1):298. doi:10.1186/s12957-020-02071-8
29. Kaya FN, Turker G, Basagan-Mogol E, Goren S, Bayram S, Gebitekin C. Preoperative multiple-injection thoracic paravertebral blocks reduce postoperative pain and analgesic requirements after video-assisted thoracic surgery. J Cardiothorac Vasc Anesth. 2006;20(5):639–643. doi:10.1053/j.jvca.2006.03.022
30. Kim JA, Kim TH, Yang M, et al. Is intravenous patient controlled analgesia enough for pain control in patients who underwent thoracoscopy? J Korean Med Sci. 2009;24(5):930–935. doi:10.3346/jkms.2009.24.5.930
31. Kim DH, Oh YJ, Lee JG, Ha D, Chang YJ, Kwak HJ. Efficacy of ultrasound-guided serratus plane block on postoperative quality of recovery and analgesia after video-assisted thoracic surgery: a randomized, triple-blind, placebo-controlled study. Anesth Analg. 2018;126(4):1353–1361. doi:10.1213/ane.0000000000002779
32. Lee J, Lee DH, Kim S. Serratus anterior plane block versus intercostal nerve block for postoperative analgesic effect after video-assisted thoracoscopic lobectomy: a randomized prospective study. Medicine. 2020;99(49):e22102. doi:10.1097/md.0000000000022102
33. Luo G, Zhu J, Ni H, et al. Pretreatment with pectoral nerve block ii is effective for reducing pain in patients undergoing thoracoscopic lobectomy: a randomized, double-blind, placebo-controlled trial. Biomed Res Int. 2021;2021:6693221. doi:10.1155/2021/6693221
34. Ökmen K, Metin ökmen B. Evaluation of the effect of serratus anterior plane block for pain treatment after video-assisted thoracoscopic surgery. Anaesth Crit Care Pain Med. 2018;37(4):349–353. doi:10.1016/j.accpm.2017.09.005
35. Park MH, Kim JA, Ahn HJ, Yang MK, Son HJ, Seong BG. A randomised trial of serratus anterior plane block for analgesia after thoracoscopic surgery. Anaesthesia. 2018;73(10):1260–1264. doi:10.1111/anae.14424
36. Qiu Y, Wu J, Huang Q, et al. Acute pain after serratus anterior plane or thoracic paravertebral blocks for video-assisted thoracoscopic surgery: a noninferiority randomised trial. Randomized controlled trial research support, Non-U.S. Gov’t. Eur J Anaesthesiol. 2021;38(Suppl 2):S97–S105. doi:10.1097/EJA.0000000000001450
37. Qiu L, Bu X, Shen J, et al. Observation of the analgesic effect of superficial or deep anterior serratus plane block on patients undergoing thoracoscopic lobectomy. Observational study randomized controlled trial research support, Non-U.S. Gov’t. Medicine. 2021;100(3):e24352. doi:10.1097/MD.0000000000024352
38. Qiu Y, Lu X, Liu Y, Chen X, Wu J. Efficacy of the intraoperative opioid-sparing anesthesia on quality of patients’ recovery in video-assisted thoracoscopic surgery: a randomized trial. J Thorac Dis. 2022;14(7):2544–2555. doi:10.21037/jtd-22-50
39. Semyonov M, Fedorina E, Grinshpun J, et al. Ultrasound-guided serratus anterior plane block for analgesia after thoracic surgery. J Pain Res. 2019;12:953–960. doi:10.2147/jpr.S191263
40. Shim JG, Ryu KH, Kim PO, et al. Evaluation of ultrasound-guided erector spinae plane block for postoperative management of video-assisted thoracoscopic surgery: a prospective, randomized, controlled clinical trial. J Thorac Dis. 2020;12(8):4174–4182. doi:10.21037/jtd-20-689
41. Turhan O, Sivrikoz N, Sungur Z, Duman S, Ozkan B, Senturk M. Thoracic paravertebral block achieves better pain control than erector spinae plane block and intercostal nerve block in thoracoscopic surgery: a randomized study. Randomized controlled trial. J Cardiothorac Vasc Anesth. 2021;35(10):2920–2927. doi:10.1053/j.jvca.2020.11.034
42. Ueda K, Hayashi M, Murakami J, Tanaka T, Utada K, Hamano K. Intercostal block vs. epidural analgesia in thoracoscopic lung cancer surgery: a randomized trial. Gen Thorac Cardiovasc Surg. 2020;68(3):254–260. doi:10.1007/s11748-019-01197-1
43. Viti A, Bertoglio P, Zamperini M, et al. Serratus plane block for video-assisted thoracoscopic surgery major lung resection: a randomized controlled trial. Interact Cardiovasc Thorac Surg. 2020;30(3):366–372. doi:10.1093/icvts/ivz289
44. Vogt A, Stieger DS, Theurillat C, Curatolo M. Single-injection thoracic paravertebral block for postoperative pain treatment after thoracoscopic surgery. Br J Anaesth. 2005;95(6):816–821. doi:10.1093/bja/aei250
45. Yao Y, Fu S, Dai S, et al. Impact of ultrasound-guided erector spinae plane block on postoperative quality of recovery in video-assisted thoracic surgery: a prospective, randomized, controlled trial. J Clin Anesth. 2020;63:109783. doi:10.1016/j.jclinane.2020.109783
46. Yeap YL, Wolfe JW, Backfish-White KM, et al. Randomized prospective study evaluating single-injection paravertebral block, paravertebral catheter, and thoracic epidural catheter for postoperative regional analgesia after video-assisted thoracoscopic surgery. J Cardiothorac Vasc Anesth. 2020;34(7):1870–1876. doi:10.1053/j.jvca.2020.01.036
47. Yildirim K, Sertcakacilar G, Hergunsel GO. Comparison of the results of ultrasound-guided thoracic paravertebral block and modified pectoral nerve block for postoperative analgesia in video-assisted thoracoscopic surgery: a prospective, randomized controlled study. Randomized controlled trial. J Cardiothorac Vasc Anesth. 2022;36(2):489–496. doi:10.1053/j.jvca.2021.08.014
48. Yoshioka M, Mori T, Kobayashi H, et al. The efficacy of epidural analgesia after video-assisted thoracoscopic surgery: a randomized control study. Ann Thorac Cardiovasc Surg. 2006;12(5):313–318.
49. Yuan B, Liu D, Zhu Z, Hao Y, He K, Deng S. Effect of thoracic paravertebral nerve block on blood coagulation in patients after thoracoscopic lobectomy: a prospective randomized controlled clinical trial. J Pain Res. 2022;15:633–641. doi:10.2147/jpr.S355227
50. Zhang X, Shu L, Lin C, et al. Comparison between intraoperative two-space injection thoracic paravertebral block and wound infiltration as a component of multimodal analgesia for postoperative pain management after video-assisted thoracoscopic lobectomy: a randomized controlled trial. J Cardiothorac Vasc Anesth. 2015;29(6):1550–1556. doi:10.1053/j.jvca.2015.06.013
51. Zhang S, Han X, Zhou D, et al. The effects of erector spinae plane block on perioperative opioid consumption and rehabilitation in video assisted thoracic surgery. Randomized Controlled Trial. BMC Anesthesiol. 2021;21(1):313. doi:10.1186/s12871-021-01536-x
52. Zhang Y, Fu Z, Fang T, et al. A comparison of the analgesic efficacy of serratus anterior plane block vs. paravertebral nerve block for video-assisted thoracic surgery: a randomized controlled trial. Wideochirurgia i Inne Techniki Maloinwazyjne. 2022;17(1):134–142. doi:10.5114/wiitm.2021.105725
53. Zhao H, Xin L, Feng Y. The effect of preoperative erector spinae plane vs. paravertebral blocks on patient-controlled oxycodone consumption after video-assisted thoracic surgery: a prospective randomized, blinded, non-inferiority study. J Clin Anesth. 2020;62:109737. doi:10.1016/j.jclinane.2020.109737
54. Beverly A, Kaye AD, Ljungqvist O, Urman RD. Essential elements of multimodal analgesia in Enhanced Recovery After Surgery (ERAS) guidelines. Anesthesiol Clin. 2017;35(2):e115–e143. doi:10.1016/j.anclin.2017.01.018
55. Ruppen W, Derry S, McQuay H, Moore RA. Incidence of epidural hematoma, infection, and neurologic injury in obstetric patients with epidural analgesia/anesthesia. Anesthesiology. 2006;105(2):394–399. doi:10.1097/00000542-200608000-00023
56. Christie IW, McCabe S. Major complications of epidural analgesia after surgery: results of a six-year survey. Anaesthesia. 2007;62(4):335–341. doi:10.1111/j.1365-2044.2007.04992.x
57. Cook TM, Counsell D, Wildsmith JAW; Project oboTRCoATNA. Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists†. Br J Anaesth. 2009;102(2):179–190. doi:10.1093/bja/aen360
58. Joshi GP, Bonnet F, Shah R, et al. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth Analg. 2008;107(3):1026–1040. doi:10.1213/01.ane.0000333274.63501.ff
59. Hartmann B, Junger A, Klasen J, et al. The incidence and risk factors for hypotension after spinal anesthesia induction: an analysis with automated data collection. Anesth Analg. 2002;94(6):1521–1529. doi:10.1097/00000539-200206000-00027
60. Jo Y, Park S, Oh C, et al. Regional analgesia techniques for video assisted thoracic surgery: a frequentist network meta-analysis. Korean J Anesthesiol. 2021;13:13.
61. Balzani E, Rosboch GL, Ceraolo E, et al. The effect of peripheral regional analgesia in thoracic surgery: a systematic review and a meta-analysis of randomized-controlled trials. Tumori. 2022:3008916221081891. doi:10.1177/03008916221081891
62. Lin J, Liao Y, Gong C, et al. Regional analgesia in video-assisted thoracic surgery: a bayesian network meta-analysis. Front Med. 2022;9:842332. doi:10.3389/fmed.2022.842332
63. Feray S, Lubach J, Joshi GP, Bonnet F, Van de Velde M. PROSPECT guidelines for video-assisted thoracoscopic surgery: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2022;77(3):311–325. doi:10.1111/anae.15609
64. Sommer M, de Rijke JM, van Kleef M, et al. The prevalence of postoperative pain in a sample of 1490 surgical inpatients. Eur J Anaesthesiol. 2008;25(4):267–274. doi:10.1017/s0265021507003031
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


