Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Effect of Macrolide Antibiotics on In-Hospital Mortality Among Acute Exacerbation of COPD Patients: A Propensity Score-Matched Analysis
Authors Morasert T , Kriengwattanakul O, Kulalert P
Received 11 May 2022
Accepted for publication 28 August 2022
Published 13 September 2022 Volume 2022:17 Pages 2229—2239
DOI https://doi.org/10.2147/COPD.S373595
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Min Zhang
Thotsaporn Morasert,1 Orakarn Kriengwattanakul,2 Prapasri Kulalert3
1Pulmonary and Critical Care Medicine, Department of Internal Medicine, Suratthani Hospital, Surat Thani, 84000, Thailand; 2Department of Internal Medicine, Suratthani Hospital, Surat Thani, 84000, Thailand; 3Department of Clinical Epidemiology, Faculty of Medicine, Thammasat University, Pathum Thani, Thailand
Correspondence: Thotsaporn Morasert, Pulmonary and Critical Care Medicine, Department of Internal Medicine, Suratthani Hospital, Surat Thani, 84000, Thailand, Tel +66 88 753 2006 ; +66 77 915 600, Email [email protected]
Objective: This study aimed to assess whether the short-term use of macrolide antibiotics during hospitalization can reduce in-hospital all-cause mortality compared to non-macrolide treatment in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD).
Methods: A propensity score (PS) matching analysis was performed using retrospective data from the admission records of AECOPD patients in the medical general ward and medical intensive care unit of a tertiary care center between October 2015 and September 2018. The multivariable Cox proportional hazard model was performed to eliminate residual confounding after the PS analysis.
Results: The mortality rate was 11.1% of 1528 admissions in the PS matching cohort. Approximately 70% of patients had respiratory failure requiring intubation on initial admission, and 34% had pneumonia. Macrolide treatment significantly reduced in-hospital mortality among AECOPD patients (adjusted hazard ratio, 0.55; 95% confidence interval 0.32– 0.96; P=0.034). Clarithromycin was the most commonly prescribed macrolide (80%).
Conclusion: Macrolide antibiotics reduced in-hospital mortality in hospitalized AECOPD patients. The combination of antimicrobial and immunomodulatory effects of macrolide treatment could play an essential role.
Keywords: macrolides, AECOPD, mortality, propensity score-matched
Introduction
An acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is defined as an acute worsening of respiratory symptoms that may cause a progressive decline in lung function.1 The infectious agent in exacerbation can be viral or bacterial.2 The international guidelines3,4 recommend considering empiric antibiotic therapy for AECOPD patients who are most likely to have a bacterial infection and for the most ill patients who require hospitalization.5–7 In addition, many randomized controlled trials (RCTs) and cohort studies demonstrated that prompt, appropriate antibiotic treatment could improve clinical outcomes that reduced in-hospital mortality,8,9 all-cause mortality,10 and the composite outcome of treatment failure11 in selected patients with AECOPD.
However, the initial choice of empiric antibiotic therapy is not standardized and should be guided by prior antibiotic use, AECOPD severity, local bacterial resistance, and the likelihood that Pseudomonas species are present.3 The commonly used initial empirical antibiotics are aminopenicillin with clavulanic acid and macrolides.3 However, in patients with frequent exacerbations, severe airflow limitation,12 or mechanical ventilation is required,6 a culture from sputum or tracheal suction should be performed to detect resistant organisms, especially gram-negative bacteria.
Macrolides are antibiotics that are effective against gram-positive and some gram-negative bacteria. They are also active against atypical bacteria such as Mycoplasma pneumoniae and Chlamydophila pneumoniae. Although a viral infection can be involved in AECOPD, there is no significant evidence that macrolides might have a direct benefit in viral infections. However, a recent extensive literature review proposed that macrolides may improve the clinical course of viral respiratory infections through anti-inflammatory and immunomodulatory effects.13 The immunomodulatory effect of long-term use of macrolide antibiotics can decrease the rate of AECOPD recurrence.14 Long-term use of macrolides was reported in a meta-analysis to significantly reduce exacerbations due to immunomodulatory properties. The latest GOLD 2021 recommends using macrolide antibiotics in patients who continue to have exacerbations while optimizing inhaled therapy.3
A published RCT compared azithromycin to placebo taken daily for one year. Azithromycin was shown to decrease the frequency of exacerbations and improve the quality of life,15 especially in those who were not current smokers.16 However, the benefit of macrolides in the short-term mortality of AECOPD patients is still controversial. Furthermore, in a propensity score (PS)-matched study in the United States among critically ill patients with AECOPD, macrolide treatment within the first 48 hours of admission reduced 30-day hospital readmissions and time to readmission but did not reduce hospital mortality.17 Therefore, we aimed to investigate the impact of macrolide treatment at initial admission on in-hospital mortality in AECOPD patients.
Methods
Study Design and Setting
We conducted a therapeutic study based on a retrospective cohort of hospitalized AECOPD patients in Suratthani Hospital, which is a university-affiliated tertiary care and referral center located in southern Thailand. The Institutional Review Board and the Ethics Committee of Suratthani Hospital approved the study protocol (Approval ID. 87/2564, December 23, 2021). The study was performed in accordance with the declaration of Helsinki. Patient informed consent was not required because neither direct patient contact nor primary collection of individual patient data occurred.
Study Population
We included all consecutive AECOPD patients admitted to the medical general ward and medical intensive care unit (ICU) between October 2015 and September 2018. The diagnosis of AECOPD was based on the International Statistical Classification of Diseases and Related Health Problems 10 (ICD-10) codes J44.0, J44.1, and J44.9 as the principal diagnoses in the admission records. The exclusion criteria were: (1) patients aged <40 years and (2) spirometry results not consistent with COPD (FEV1/FVC ratio <0.7). Patients were separated into two groups based on whether they were treated with macrolide antibiotics (clarithromycin, erythromycin, or azithromycin) or non-macrolide antibiotics. Treatment with antibiotics and systemic steroids was defined as prescribing the medications within the first 24 hours of hospitalization and continued for at least two consecutive days. The primary outcome was all-cause in-hospital mortality.
Data Collection
Patient demographic data included age, gender, body mass index, smoking status, comorbidities, spirometry results, history of emergency department (ED) visits or hospitalization within the past year, the year of hospitalization, and COPD controller medications. We also collected data on the initial (within the first 24 hours) clinical data that included vital signs (body temperature, heart rate, respiratory rate, systolic blood pressure [SBP], diastolic blood pressure [DBP], and the presence of respiratory failure requiring intubation), initial investigations (eg, complete blood count, blood chemistries, and chest radiography), point of care glucose testing, sputum and tracheal aspiration cultures, initial antibiotic and systemic steroid prescriptions, hospital length of stay, and mortality.
Statistical Analysis
Clinical characteristics of the macrolide and non-macrolide groups were compared using Fisher’s exact test for categorical data. Continuous variables are presented as mean ± SD and compared using an independent sample t-test. Non-parametric continuous variables are presented as median with interquartile range (IQR) and compared using the Wilcoxon-Mann–Whitney rank sum test. All proportions and P values were calculated based on variables with no missing data.
PS matching was used to address the problems of selection bias and imbalanced prognostic determinants between patients who did and did not receive macrolides. The independent covariates to develop the models were the admission year and the potential variables that might affect the prescribing of antibiotics by physicians. The variables included the history of admission or ED visit in the previous year, the presence of respiratory failure (intubation), and pneumonia demonstrated by consolidation on chest radiography on initial admission. A multivariable logistic regression model was used to compute the PS values, which were split into different blocks with a similar probability of receiving macrolides. Then, we matched the patients who did and did not receive macrolides within each block with a 1:1 ratio.
A standardized difference of the entire cohort and PS-matched cohorts was performed. The absolute standardized difference value of more than 10% was considered a significant difference between the clinical characteristics, prognostic factors, and potential confounders of the macrolide and non-macrolide groups.18 Therefore, those variables in the matched cohort with a standardized difference of more than 10% were included in the final multivariable Cox proportional hazard model to eliminate the residual confounders. The impact on in-hospital mortality of macrolide treatment was demonstrated in a Kaplan–Meier survival curve and expressed as adjusted hazard ratio (aHR) with 95% confidence interval (CI). P values <0.05 were considered statistically significant in all analyses. In all analysis modeling, the clustering method adjusted the standard errors for the same patient correlation due to readmission. All statistical analyses were performed using Stata Statistical Software Release 16 (StataCorp LLC, College Station, TX, USA).
Results
Patient Characteristics
A total of 1919 admissions of AECOPD patients were screened. Thirty-seven admissions were excluded due to age <40 years, FEV1/FVC ratio ≥0.7, or the lack of a mortality outcome report (Figure 1). Finally, the entire cohort had 1882 admissions (948 patients). Of the original cohort, 1035 admissions (55%) were treated with macrolides, and 847 (45%) did not receive macrolides. Comparisons of baseline characteristics, admission parameters, years of hospitalization, antibiotic co-administrations and systemic steroids between the macrolide and non-macrolide groups by the original and PS-matched cohort are shown in Tables 1 and 2.
 |
Table 2 Macrolides and Other Antibiotic Co-Administrations and Systemic Steroids |
Propensity-Matched Cohort
The logistic modeling results to derive the confounding scores are presented in Table 3. After PS matching (1:1), the PS-matched cohort had 1528 admissions (842 patients). The mortality rate of the PS-matched cohort (11.1%) was similar to the original cohort (11.6%). In the PS-matched cohort, the patients were predominantly male (86.2%) with a mean ± SD age of 75 ± 11.1 years. Eighty-five percent of this cohort had other comorbidities of which 47.7% had hypertension. The mean ± SD ratios of FEV1/FVC and the % predicted FEV1 were 0.50 ± 0.10 and 66.4 ± 19.6%, respectively. Before the current admission, 72.3% of patients used inhaled controller medications, 54.7% had ED visits in the previous 1 year, and 43.3% were hospitalized in the previous 1 year. Approximately 70% of patients had respiratory failure requiring intubation on initial admission, and 34% had pneumonia demonstrated by radiographic consolidation. Macrolide and antibiotic co-administration treatments are shown in Table 2. Eighty-eight percent of patients received one or more antibiotics. The most common macrolide given was clarithromycin (80%). Significant differences were observed in the proportions of all other antibiotic and systemic steroid treatments between the macrolide and non-macrolide groups. Compared to the non-macrolide group, patients in the macrolide group were more likely to receive ceftriaxone (77% vs 25%) and systemic steroids (73% vs 55%). On the other hand, the macrolide group was less likely to receive other antibiotics except for ceftriaxone. Of the 1171 admissions that had sputum or tracheal aspiration culture performed, 1092 were accepted as suitable for culture (Table 4). Almost 50% of these cultures were positive for bacteria: gram-negative 40.7% and gram-positive 9.7%.
 |
Table 3 Logistic Regression Models for the Derivation of the Propensity Score |
 |
Table 4 Microbiological Results Including Sputum and Tracheal Aspiration Cultures of Hospitalized Acute Exacerbation of COPD Patients in Propensity-Matched Cohort (n = 1092 Admissions) |
In-Hospital Mortality Outcome
Finally, after PS matching, the residual variables with a standardized difference of more than 10% were bronchiectasis, SBP, DBP, blood urea nitrogen, serum creatinine, serum albumin, and hemoglobin level (Table 1). All of these variables and the post-treatment covariates, which included antibiotic co-administration and systemic steroids, were included in the final multivariable Cox’s proportional hazard regression model. Macrolide treatment significantly reduced in-hospital mortality of AECOPD (aHR, 0.55; 95% CI, 0.32–0.96; P=0.034). The Kaplan–Meier survival curve shows the impact on in-hospital mortality of macrolide treatment (Figure 2). A sensitivity analysis was performed. The multivariable logistic regression model using the PS as a covariate yielded a similar result (adjusted odds ratio, 0.58; 95% CI, 0.35–0.98; P=0.043).
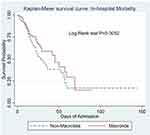 |
Figure 2 Kaplan–Meier survival curve shows the impact on in-hospital mortality of macrolide treatment. |
Discussion
Patients with AECOPD initially treated with macrolide antibiotics in addition to standard treatment showed a significantly lower rate of in-hospital mortality compared to the non-macrolide group. The patients were treated at a tertiary care and referral center, which included ICU and non-ICU settings. The presentations on admission were quite severe. Respiratory failure that required invasive mechanical ventilation was found in 70% of patients, and 33% of patients also had pneumonia. This study demonstrated the in-hospital mortality outcome of up to 11% of hospitalized AECOPD patients. This study also found that macrolides reduced all-cause mortality by 45% using the time to event analysis in the PS matching cohort. In previous studies, estimated in-hospital mortality varied from 2.5% to 25%.19–23
In line with a previous study that used PS matching in critically ill AECOPD patients, macrolide treatment on initial admission reduced 30-day hospital readmissions and time to subsequent admission but did not reduce hospital mortality.17 Our study differed from that study17 in that we recruited more respiratory failure patients who required mechanical ventilation (75% vs 20%), and we adjusted for the initial admission clinical and laboratory parameters that could affect mortality outcomes. Furthermore, in a small retrospective study in Japan, single-dose 2.0 gm azithromycin compared to intravenous antibiotics in hospitalized AECOPD patients resulted in a shorter length of hospital stay.24 A previous RCT25 demonstrated that azithromycin treatment within the first two days of infectious AECOPD admission and extended for three months compared to placebo did not reduce all-cause mortality but only tended to reduce mortality by 45% within six days of admission. This observation indicated the potential benefit of macrolide treatment on in-hospital mortality during the early admission period. The subsequent post hoc analysis of this trial showed the benefit of azithromycin in reducing hospital readmissions, especially in patients who had either high C-reactive protein (CRP) (>50 mg/L) or low blood eosinophil count (<300 cells/μL).26 Unfortunately, our study did not have CRP information to explore this issue and determine who would benefit from antibiotics.27–29
The biological plausibility of this study was the biological action of macrolides in terms of antimicrobial and immunomodulatory properties.14 The macrolide antimicrobial effect on atypical bacteria might explain the benefit in mortality reduction. A previous study in China demonstrated the important role of atypical pathogens in hospitalized AECOPD patients by the positivity rates of Mycoplasma pneumoniae (20.7%), Chlamydia pneumoniae (29.7%), and Legionella pneumophila (10.3%).30 One-third of respiratory specimens from pneumonic exacerbation patients in this study had negative culture results and were possibly infected by “atypical” pathogens, which refer to organisms that have intrinsic resistance to beta-lactams and are not visualized on gram stain or grown on culture using traditional techniques. Furthermore, in the subgroup of organisms with intrinsic macrolide resistance, especially Pseudomonas aeruginosa, the effect of macrolides on in-hospital mortality appeared to be less explicit (Figure 3). Immunomodulatory mechanisms of macrolides include anti-inflammatory effects by decreasing cytokine levels, inhibiting mucous secretion, inhibiting effects on bacterial virulence and biofilms, and inhibiting effects of viral infection, which are involved in several pathways of the AECOPD mechanism. The combination of antibiotics and systemic steroids reduced in-hospital mortality and lowered the risk of readmission within 30 days.9 The latest GOLD guideline 2022,3 British Thoracic Society guideline 2020,31 and several studies32,33 suggest using low-dose macrolide therapy in patients with COPD in the following scenarios: (1) patients with more than three exacerbations per year requiring steroid therapy and (2) patients who had at least one exacerbation requiring hospital admission per year. Low-dose macrolide therapy can also be considered for a minimum duration of six months and up to 12 months to assess the impact on exacerbation rate.15,16,31
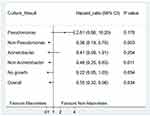 |
Figure 3 Risk of in-hospital mortality by subgroups of culture results in patients treated with macrolides vs non-macrolides. |
The limitations of this study need to be considered. First, due to the nature of a retrospective study, we could not collect some data that might affect the results, especially spirometry data, which are predictors of baseline COPD severities. Second, several health data that occurred in the primary and secondary care units were not linked to our data system. Some patients possibly received treatments during those visits or in the past that resulted in different risks of mortality. Third, macrolides have well-known adverse effects like QT prolongation, hearing impairment, bacteria developing increased drug resistance, allergic reaction, and drug interaction with many other medications.34 In this study, we did not collect data on macrolide adverse effects but assumed that short-term use of macrolides might have fewer adverse effects than long-term use. However, repeated courses of macrolide therapy might increase the risk of adverse effects, especially azithromycin with a longer elimination half-life. Thus, monitoring after macrolide therapy is warranted.35
Conclusion
Macrolide treatment at initial admission with usual care for hospitalized AECOPD patients showed promising results in reducing all-cause in-hospital mortality. Therefore, the antimicrobial and immunomodulatory effects of macrolide treatment can play an essential role.
Acknowledgments
The authors thank Dr Theerasuk Kawamatawong for his valuable advice in the discussion part. We thank Editage for English language editing. We thank Glenn Shingledecker for his assistance in editing and proofreading the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. All authors have drafted or written or substantially revised or critically reviewed the article and have agreed on the journal to which the article will be submitted. All authors reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. All authors agree to take responsibility and be accountable for the contents of the article.
Funding
This study was supported by the Medical Education Centre of Suratthani Hospital, Thailand. The research was designed, conducted, analyzed, and interpreted by the authors entirely independently of the funding sources.
Disclosure
The authors have no conflicts of interest in relation to this work.
References
1. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi:10.1016/S0140-6736(07)61382-8
2. Love ME, Proud D. Respiratory viral and bacterial exacerbations of COPD-the role of the airway epithelium. Cells. 2022;11(9):1416. doi:10.3390/cells11091416
3. Kalanuria AA, Ziai W, Mirski M. Ventilator-associated pneumonia in the ICU. Critical Care. 2014;18(2):208. doi:10.1186/cc13775
4. Koenig SM, Truwit JD. Ventilator-associated pneumonia: diagnosis, treatment, and prevention. Clin Microbiol Rev. 2006;19(4):637–657. doi:10.1128/CMR.00051-05
5. Sethi S, Murphy TF. Bacterial infection in chronic obstructive pulmonary disease in 2000: a state-of-the-art review. Clin Microbiol Rev. 2001;14(2):336–363. doi:10.1128/CMR.14.2.336-363.2001
6. Soler N, Torres A, Ewig S, et al. Bronchial microbial patterns in severe exacerbations of chronic obstructive pulmonary disease (COPD) requiring mechanical ventilation. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1498–1505. doi:10.1164/ajrccm.157.5.9711044
7. White AJ, Gompertz S, Stockley RA. Chronic obstructive pulmonary disease. 6: the aetiology of exacerbations of chronic obstructive pulmonary disease. Thorax. 2003;58(1):73–80. doi:10.1136/thorax.58.1.73
8. Nouira S, Marghli S, Belghith M, Besbes L, Elatrous S, Abroug F. Once daily oral ofloxacin in chronic obstructive pulmonary disease exacerbation requiring mechanical ventilation: a randomised placebo-controlled trial. Lancet. 2001;358(9298):2020–2025. doi:10.1016/S0140-6736(01)07097-0
9. Stefan MS, Rothberg MB, Shieh MS, Pekow PS, Lindenauer PK. Association between antibiotic treatment and outcomes in patients hospitalized with acute exacerbation of COPD treated with systemic steroids. Chest. 2013;143(1):82–90. doi:10.1378/chest.12-0649
10. Roede BM, Bresser P, Prins JM, Schellevis F, Verheij TJ, Bindels PJ. Reduced risk of next exacerbation and mortality associated with antibiotic use in COPD. Eur Respir J. 2009;33(2):282–288. doi:10.1183/09031936.00088108
11. Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303(20):2035–2042. doi:10.1001/jama.2010.672
12. Miravitlles M, Espinosa C, Fernández-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Study Group of Bacterial Infection in COPD. Chest. 1999;116(1):40–46. doi:10.1378/chest.116.1.40
13. Poddighe D, Aljofan M. Clinical evidences on the antiviral properties of macrolide antibiotics in the COVID-19 era and beyond. Antivir Chem Chemother. 2020;28:2040206620961712. doi:10.1177/2040206620961712
14. Yamaya M, Azuma A, Takizawa H, Kadota J-I, Tamaoki J, Kudoh S. Macrolide effects on the prevention of COPD exacerbations. Eur Respir J. 2012;40(2):485. doi:10.1183/09031936.00208011
15. Albert RK, Connett J, Bailey WC, et al. Azithromycin for Prevention of Exacerbations of COPD. N Engl J Med. 2011;365(8):689–698. doi:10.1056/NEJMoa1104623
16. Han MK, Tayob N, Murray S, et al. Predictors of chronic obstructive pulmonary disease exacerbation reduction in response to daily azithromycin therapy. Am J Respir Crit Care Med. 2014;189(12):1503–1508. doi:10.1164/rccm.201402-0207OC
17. Kiser TH, Reynolds PM, Moss M, Burnham EL, Ho PM, Vandivier RW. Impact of macrolide antibiotics on hospital readmissions and other clinically important outcomes in critically ill patients with acute exacerbations of chronic obstructive pulmonary disease: a propensity score-matched cohort study. Pharmacotherapy. 2019;39(3):242–252. doi:10.1002/phar.2221
18. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi:10.1080/00273171.2011.568786
19. Ai-Ping C, Lee K-H, Lim T-K. In-hospital and 5-year mortality of patients treated in the ICU for acute exacerbation of COPD: a retrospective study. Chest. 2005;128(2):518–524. doi:10.1378/chest.128.2.518
20. Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003;163(10):1180–1186. doi:10.1001/archinte.163.10.1180
21. Cao Y, Xing Z, Long H, et al. Predictors of mortality in COPD exacerbation cases presenting to the respiratory intensive care unit. Respir Res. 2021;22(1):77. doi:10.1186/s12931-021-01657-4
22. Steer J, Gibson J, Bourke SC. The DECAF Score: predicting hospital mortality in exacerbations of chronic obstructive pulmonary disease. Thorax. 2012;67(11):970. doi:10.1136/thoraxjnl-2012-202103
23. Roche N, Zureik M, Soussan D, et al. Predictors of outcomes in COPD exacerbation cases presenting to the emergency department. Eur Respir J. 2008;32(4):953. doi:10.1183/09031936.00129507
24. Asai N, Ohkuni Y, Iwasaki T, et al. Efficacy and safety of single-dose 2.0 g azithromycin in the treatment of acute exacerbation of chronic obstructive pulmonary disease. J Infect Chemother. 2011;17(6):793–798. doi:10.1007/s10156-011-0260-z
25. Vermeersch K, Gabrovska M, Aumann J, et al. Azithromycin during acute chronic obstructive pulmonary disease exacerbations requiring hospitalization (BACE). A multicenter, randomized, double-blind, placebo-controlled trial. Am J Respir Crit Care Med. 2019;200(7):857–868. doi:10.1164/rccm.201901-0094OC
26. Vermeersch K, Belmans A, Bogaerts K, et al. Treatment failure and hospital readmissions in severe COPD exacerbations treated with azithromycin versus placebo – a post-hoc analysis of the BACE randomized controlled trial. Respir Res. 2019;20(1):237. doi:10.1186/s12931-019-1208-6
27. Prins HJ, Duijkers R, van der Valk P, et al. CRP-guided antibiotic treatment in acute exacerbations of COPD in hospital admissions. Eur Respir J. 2019;53(5):1802014. doi:10.1183/13993003.02014-2018
28. Brightling CE. Biomarkers that predict and guide therapy for exacerbations of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10:S214–S219. doi:10.1513/AnnalsATS.201302-023AW
29. Bafadhel M, Clark TW, Reid C, et al. Procalcitonin and C-reactive protein in hospitalized adult patients with community-acquired pneumonia or exacerbation of asthma or COPD. Chest. 2011;139(6):1410–1418. doi:10.1378/chest.10-1747
30. Feng C, Xu M, Kang J, et al. Atypical pathogen distribution in Chinese hospitalized AECOPD patients: a multicenter cross-sectional study. Int J Chron Obstruct Pulmon Dis. 2021;16:1699–1708. doi:10.2147/COPD.S300779
31. Smith D, Du Rand IA, Addy C, et al. British Thoracic Society guideline for the use of long-term macrolides in adults with respiratory disease. BMJ Open Respir Res. 2020;7(1):e000489. doi:10.1136/bmjresp-2019-000489
32. Talman S, Uzun S, Djamin RS, et al. Long-term azithromycin maintenance treatment in patients with frequent exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2021;16:495–498. doi:10.2147/COPD.S284397
33. Uzun S, Djamin RS, Kluytmans JA, et al. Azithromycin maintenance treatment in patients with frequent exacerbations of chronic obstructive pulmonary disease (Columbus): a randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2014;2(5):361–368. doi:10.1016/S2213-2600(14)70019-0
34. Hansen MP, Scott AM, McCullough A, et al. Adverse events in people taking macrolide antibiotics versus placebo for any indication. Cochrane Database Syst Rev. 2019; 1. doi:10.1002/14651858.CD011825.pub2
35. Malhotra-Kumar S, Lammens C, Coenen S, Van Herck K, Goossens H. Effect of azithromycin and clarithromycin therapy on pharyngeal carriage of macrolide-resistant streptococci in healthy volunteers: a randomised, double-blind, placebo-controlled study. Lancet. 2007;369(9560):482–490. doi:10.1016/S0140-6736(07)60235-9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


