Back to Journals » The Application of Clinical Genetics » Volume 16
Donor Safety, Discrepancies Between Practice and Theory: Analysis of the Polish Supreme Audit Office’s Report
Authors Patryn R, Zagaja A, Drozd M
Received 15 June 2022
Accepted for publication 21 November 2022
Published 20 January 2023 Volume 2023:16 Pages 1—10
DOI https://doi.org/10.2147/TACG.S376251
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Martin Maurer
Rafał Patryn, Anna Zagaja, Mariola Drozd
Department of Humanities and Social Medicine, Medical University of Lublin, Lublin, Poland
Correspondence: Mariola Drozd, Department of Humanities and Social Medicine, Medical University of Lublin, 1, Raclawickie str 20-059, Lublin, Poland, Tel +48 448 68 50, Email [email protected]
Abstract: The introduction and development of genetic testing has caused the emergence of numerous dilemmas, which pertain to the performed tests, their results, and the influence they have on an individual person. To minimize potential doubts, it is crucial to ensure compliance with established procedures and to fulfill all test-associated formalities. In 2018, a report of the Polish Supreme Audit’s Office (a governmental control agency) on the quality of genetic tests revealed that there is much to be done in the field of laboratory diagnostics in Poland. The inspection of six selected laboratories performing genetic tests identified shortcomings in terms of formalities accompanying the process of performing laboratory tests, keeping patient documentation and personal data protection. Although the observed shortcomings pertained to legal aspects of genetic tests, and not the quality of the tests themselves, the aforementioned may be detrimental to the individual person and the society (eg, lack of consent undermines the concept of biological material ownership), may cause legal liability to the laboratory personnel and even undermine public trust in genetic testing.
Keywords: safety, laboratory tests, genetics, consent, quality
Introduction
In 2012, an experiment was conducted to check the quality of performed laboratory tests.1 A tea infusion imitating a urine sample was intentionally submitted to six laboratories in one of the larger Polish cities. Obtained results proved quite surprising as they revealed that the sample contained urobilinogen, leukocytes, erythrocytes and epithelia, ie, substances characteristic of urine. A question arose of how these substances, typical of the human body’s natural excretion like urine, could have been found in a tea sample.1 This experiment, apart from undermining the credibility and reliability of performed tests, also sparked a discussion on the regulations governing Polish laboratories, including laboratories performing genetic tests.
Currently, there is no single, concise regulation on the functioning of laboratories in Poland. Such a situation is dangerous and may pose a threat to patients. According to the analyzed report of the Polish Supreme Audit’s Office (NIK), the main control body of Poland, the legal formalities that are available are not always met and that the current situation of medical benefits and laboratory services is not conducive to the safety of genetic tests.2 Laboratory tests play an important role in monitoring and evaluating the effectiveness of treatment outcomes, helping clinicians in the decision-making process. The level of quality of documentation of tests performed in laboratories is of key importance for providing patients with safe, effective and efficient medical care, as the information provided by laboratories (results, analyses, tests) have a direct impact on the patient’s treatment model.3
The area of genetic testing in Poland is serviced by laboratories of research institutes and hospitals that are subjected to legal provisions regarding the standards and requirements of medical diagnostic laboratories. The remaining laboratories are various private entities (network, specialized) that carry out economic activity. In 2022, the number of diagnostic laboratories reached 2700 (an increase of slightly over 1000 laboratory points as compared to 2019); however, because there is no central register of laboratories performing genetic tests, we were unable to determine whether enumerated laboratories offered such services.4 The number of laboratories performing genetic tests (that have “genetic” in their name) reached 44 in 2015, 45 in 2016, 40 in 2017,2 63 in 2020 and 61 in 2022.5
Because information obtained from genetic tests can be sensitive, laboratories performing such tests require the introduction of processes and activities associated with the protection of patients’ health. This mainly concerns the reliability and clinical usefulness of ordered genetic tests as well as ensuring proper genetic counseling. Genetic counseling is referred to in the in-Vitro Diagnostic Medical Devices Regulation (Regulation (EU) 2017/746 of the European Parliament and of the Council of 5 April 2017 on in vitro diagnostic medical devices and repealing Directive 98/79/EC and Commission Decision 2010/227/EU) and is based on providing information on genetic predisposition to diseases or illnesses to the biological material donor. In case of questionable, unreliable, erroneous results, or results on the existence of a yet incurable disease, such counseling is hampered.
The UNESCO International Bioethics Committee calls for the introduction of special protection of genetic data concerning the intergenerational nature of such information. A series of documents has been issued to enforce such protection including the Universal Declaration on Bioethics and Human Rights in 1997 (mainly: a protocol devoted to genetic testing performed for medical purposes) and the Declaration on Human Genetic Data in 2003. Additionally, a Recommendation of the Council of Europe committee of Ministers No. R (92) 3 of the Committee of Ministers to Member States on Testing and Screening for Health Care Purposes of February 10 was also specified. Furthermore, the Recommendation of the Parliamentary Assembly of the Council of Europe 1512 (2001) on the protection of the human genome should also be mentioned. One of the most important regulations in Europe is the Convention for the Protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine: Convention on Human Rights and Biomedicine signed in 1997. This Convention defines fundamental principles of law in the field of bioethics, in particular additional Protocol IV adopted in 2008 for genetic testing for health purposes. What is more, individual countries introduced additional acts,6 eg, Germany enactedGesetz über genetische Untersuchungen bei Menschen – Gendiagnostikgesetz of June 1, 2009, in France: Loi no 2011–814 relative à la bioéthique,7 Switzerland, Loi fédérale sur l’analyse génétique humaine of October 9, 2003, and Spain, Ley 14/2007 de Investigación biomedical (2007).8 The Czech Republic introduced legal regulations on genetic testing as a chapter in the Act of November 6, 2011 on special healthcare activities.9
In case of Polish legislative solutions, there are no comprehensive regulations as to the area of genetics, including genetic testing. Lack of such regulations, and therefore also regulations concerning supervision, may lead to various shortcomings and differences between laboratory proceedings. It may also influence the quality of testing as well as data protection. The abiding regulations relate to genetic testing to a very limited extent and are included in many legal acts, often inconsistent. One of them is the Ordinance of the Minister of Health of 23 March 2006 on the quality standards for medical diagnostic and microbiological laboratories and the thematic appendix (can be viewed at the Announcement of the MInister of Health of September 13, 2016) on the quality standards for laboratories in terms of laboratory medical genetics, laboratory interpretation and authorization of test results, which was added to the regulation in 2009 and amended in 2015, 2019 and 2020. This legal act defines quality standards for laboratories in terms of medical genetics appendix. It focuses mostly on technical aspects behind the gathering of biological material and provides precise provisions associated with ordering of genetic tests, collecting human biological material, performing the test and sample transport. The appendix also provides regulations for the storage of biological material and quality assurance and provides guidelines for documentation keeping. The analyzed NIK’s report focused on fulfilling the established criteria by laboratories that perform genetic tests. The report revealed a discrepancy between established legal standards and the factual situation of inspected laboratories.
Materials and Methods
The base material for this study was a publicly available Supreme Audit Office’s (NIK)10 report on the safety of genetic research. In the fall of 2017, the Polish Supreme Audit’s Office inspected six analytical laboratories where genetic tests were performed. The laboratories inspected by NIK report included entities located at three research institutes, a stand-alone public hospital and two private entities. Only one of the inspected laboratories met the ISO 15189 standard for medical laboratories in terms of quality and competence requirements (authorized by the Polish Center for Accreditation). The remaining laboratories implemented quality management systems for providing various services, such as diagnostics, genetic testing, and genetic counseling. Currently, only seven laboratories in Poland are accredited by the PN/EN ISO 15189.
The study covered the period between 2015 and 2017, and the report in question was published in 2018.2
The legal basis to which each of the laboratory’s proceedings was compared against was the aforementioned Act on the quality standards for laboratories in terms of laboratory medical genetics, laboratory interpretation and authorization of test results to the Ordinance of the Minister of Health from 2006.
Each parameter in a diagnostic laboratory determined in accordance with legal requirements must be subjected to supervision. Failure to respect any provisions or lack of reference to it was interpreted as failure to comply with the applicable regulations in this regard. The inspections focused on the organization of the laboratory’s work, its equipment, documentation, as well as human resources and professional qualifications of employees. In each laboratory, the inspectors traced the process of patient’s genetic testing from the moment of biological sample collecting, transport of the sample to the laboratory and issuing of test results. In each laboratory, inspectors also analyzed selected documentation of previously performed genetic tests.
In this study, each of the post-inspection documents consisting of the Post-inspection Statement and Information on the inspection results was analyzed in terms of identified irregularities. Based on the Polish quality standards for laboratories in terms of laboratory medical genetics, the occurrence of errors and irregularities found during the audit carried out by the Polish Supreme Audit’s Office was analyzed. The results are summarized in bullet points.
Results
Inspected laboratories performed genetic tests in various numbers from 114 to 32,144. The number of tests performed in individual laboratories is presented in Table 1.
 |
Table 1 Profile of Inspected Laboratories Performing Genetic Tests in the Years Between 2015 and 2017 |
A total of 87,175 genetic tests was performed during the inspected period. During that time, 611 pieces of documentation form genetic tests were analyzed in total from all laboratories, which accounted for 0.7% of all genetic tests performed within them.
The audit revealed the following irregularities:
- Not all genetic laboratories are registered as such in the National Chamber of Diagnostic Laboratories;
- People without the required qualifications and experience were hired in the positions of laboratory diagnosticians and laboratory managers;
- Technical inspections of laboratory equipment were conducted off the schedule, eg, the inspection of the automatic capillary sequencer;
- Procedures required by Ordinance of the Minister of Health of 23 March 2006 on the quality standards for medical diagnostic and microbiological laboratories were not implemented or were not completed, eg, the procedure for accepting material for testing did not include the obligation to check data compliance between the referral and the consent form, the procedure for genetic material storing did not include the requirement to keep documentation on the storage of the material before and after the test;
- Quality management systems were not implemented in terms of requirements for research and calibration laboratories as well as quality and competence for medical laboratories;
- Improper labeling of collective packaging containing genetic material, including no indication of “infectious material” or no indication of the time the material was collected, was noted;
- Deficiencies and errors in the documentation were observed, including
- the absence of patient’s consent for storage of the genetic material,
- consent forms for genetic testing lacking annotation about obtaining information from the physician ordering the test, in particular regarding the nature of the suspected disease and the diagnostic significance of the planned genetic testing,
- consent forms missing space to indicate data of a statutory representative (in case of minors and those incapacitated),
- referral forms missing fields enabling the indication of
- the place where results should be sent,
- data of the person authorized to receive the results,
- patient’s address,
- method of preferable contact with the patient,
- family history, including information on genetic diseases;
- Failure to provide adequate technical and organizational measures to protect patients’ personal data during sample and results transport, eg, employees having access to patients’ personal data or performing genetic tests were not authorized to process personal data, lack of security measures in transferring referrals from the collection points to diagnostic workshops, test results in unsealed envelopes in a publicly available place;
- Performing tests based on referrals, despite the lack of attached consent for a genetic test from the patient;
- No register of stored samples of patients’ genetic material, after completion of the testing;
- Commissioning external entities to perform laboratory tests, including genetic tests, without concluding a written agreement to entrust the processing of personal.
The assessment of the documentation of genetic tests revealed that the irregularities pertained to deficiencies in the referral forms, patient’s consent to perform genetic tests and the test result document. The list of identified irregularities is presented in Table 2.
 |
Table 2 Irregularities Stated in the Inspected Documentation (N=611) (Based on Post-Inspection Reports) |
Due to the fact that in the inspected laboratories the random sample varied, the analysis was carried out after calculating the relative share of irregularities in relation to the number of documents examined. These relative shares of irregularities in the samples from individual laboratories, the results of which are presented in Table 2, were tested for compliance with the normal distribution at the significance level of α = 0.05. The H0 hypothesis is as follows: the studied population has a normal distribution. For this purpose, the Shapiro–Wilk test was used, for which the critical area was within (-∞, 0.788) for the sample size of 6 (number of laboratories). The test showed that there is no reason to reject the H0 hypothesis (on the normal distribution) only for the lack of following data: means for referring doctor–patient contact, address for sending the test results, time of sample collection, information about bone marrow transplant or transfusion, and for the number of identified irregularities in individual laboratories. Apart from lack of information on the bone marrow transplant or transfusion, normal distribution was observed for information that are not priority in terms of treatment. However, it should be emphasized that the lack of information on the possibility of transplant and transfusion may result in obtaining erroneous results and therefore trigger significant clinical consequences for the patient.
It should be concluded that in case of a normal distribution, the staffs’ approach to record keeping is similarly careless. On the other hand, where the normal distribution was not obtained in terms of compliance with documentation standards, it can be stated that the approach is somewhat irresponsible.
Moreover, for the determined parameters of the normal distribution, the probability of not making errors, which was established based on the probability function of the normal distribution for P (X))≤0, was checked.
What is more, according to the Shapiro–Wilk test for the total amount of stated irregularities found in individual laboratories, there are also no grounds to reject the H0 hypothesis (regarding the normal distribution). Taking into account the distribution function, the probability of a laboratory where all standards of keeping documentation are kept amounts to 11.4%. If laboratories in which the NIK auditors did not identify errors are left out, the probability of a laboratory in which all standards for keeping records of genetic tests are observed would amount to 5.5%. Calculated SD value was, in each case, slightly greater than the mean value except for the result of the total error shares.
In the inspected laboratories, irregularities and deviations from the applicable legal norms were detected including lack of regular technical inspections of used devices, lack of and errors in the documentation, lack or errors in procedures regarding quality standards, errors in labeling packages with genetic material, lack of protection of personal data and genetic material. The identified irregularities were related to the compliance with the standards and laboratory rules in the field of medical genetics, presented in Table 3.
 |
Table 3 Respecting Quality Standards in Terms of Laboratory Medical Genetics in the Inspected Laboratories [0 – Missing, 1 – Stated] |
When analyzing data found in Table 3, it should be noted that as a result of the assessment of compliance with 10 set standards, it was found that only 1 laboratory met all the requirements and one of the laboratories fulfilled only one of them, namely internal quality control of the tests. On the other hand, the number of standards observed in individual laboratories was characterized by a normal distribution. Taking into account the distribution function, the probability of the occurrence of a laboratory in which all standards are observed was determined and amounted to 3.88% (a value lower than the assumed significance level adopted for statistical research).
Inspected laboratories were licensed in accordance with applicable law. During the inspection period, the laboratories performed 87,175 genetic tests in total. Each of the inspected laboratories organized the process of performing genetic tests differently. However, according to the regulations, strictly defined and unified procedures must be followed. These procedures are specified in Annex 4 together with the description of the required rules and regulations.2
Discussion
Human genetic information can help identify and understand the etiology and pathophysiology of various diseases as well as confirm individual predispositions. Because such information can be obtained from performed laboratory tests, their quality and the quality of test associated formalities are of pivotal importance. This problem has been analyzed for over a dozen years and the undertaken activities and initiatives are aimed at credibility, safety and reliability of the performed tests.
A diagnostic laboratory must meet the requirements set out in regulations in order to provide high-quality medical diagnostic laboratory activities. In Poland, they have been specified in Annex 4 to the Ordinance of the Minister of Health of 23 March 2006 on the quality standards for medical diagnostic and microbiological laboratories. This document defines and describes the process of genetic testing, beginning with ordering of the laboratory test, collecting and transporting material for testing, its storage and diagnostic methods. What is more, this legal act contains a provision concerning the obligation to ensure the quality of tests performed within a laboratory. The method of keeping and the scope of the required documentation required are also specified, together with the rules for issuing reports on laboratory tests.11
Errors and mistakes regarding laboratory diagnostics and conducted research may concern various areas and happen at any stage of the diagnostic process. There may be errors related to improper preparation of the patient, wrong identification, improper collection, labeling, transport and storage of the biological material.. Errors may also concern mistakes related to the preparation of the sample during the analysis, its acceptance and the obtained results and their approval against the reference values.12,13
Another type of serious neglect is the failure to protect personal data. It should be noted that each area, which within its activity processes personal data (participant’s, patient’s, client’s) should implement and respect the principles related to the protection of such data. In the case of data obtained by laboratories in the EU such principles are found in the Regulation of the European Parliament and the EU Council 2016/679 of 27 April 2016 on the protection of individuals with regard to the processing of personal data and on the free movement of such data and the repeal of Directive 95/46/WE (General Data Protection Regulation – GDPR). In general, these principles relate to provisions ensuring protection of natural persons in relation to the processing of their personal data. Data obtained this way are subjected to special protection, as they relate to human health and may reveal information about the past, present or future physical or mental conditions of the person they concern. The context of genetic inheritance and likewise information is particularly relevant here.
In the analyzed report, infringements were noted both at the stage of processing and in terms of personal data protection. These infringements were visible at the stage of record keeping (forms with personal data), their archiving and proper labeling. Mainly reprehensible was failure to maintain appropriate protective measures (the possibility of unauthorized access), ie, careless processing (their placement in the database, providing overall safety and safety storage).
Violations of personal data security through careless handling may lead to their accidental or unlawful destruction, loss, modification, unauthorized disclosure or unauthorized access. Proper processing of personal data is possible, provided that organizational and technological measures related to their full security are guaranteed. In this case, the security of the collected personal data was questionable, as noted in the NIK report.
Approximately 70% of all errors in laboratory diagnostics that may influence final results, are most often an outcome of pre-laboratory procedures, ie, associated with the first stage of research.14 In 2006, a study was performed to discover the scale of laboratory errors in various branches of medicine (internal medicine, nephrology, surgery, intensive therapy). The authors showed that out of 51,746 analyses and laboratory tests, clinicians reported 393 questionable results, 160 of which were confirmed as laboratory errors.15 From that study, more attention was paid to procedures designed to exclude errors. It must be underlined that ordering inadequate laboratory test or implementing treatment based on false laboratory test results may influence patient’s health and comprise further treatment.16
Error reduction to a great extent correlates with adhering to appropriate guidelines and rules of conduct as well as supervision. Currently, the international standard for the accreditation of medical laboratories introduces the obligation of periodic quality checks in order to monitor and evaluate the performance and safety of a given laboratory. The ISO 15189 standard for laboratory accreditation recognizes the need to evaluate, monitor and improve all laboratory procedures. Adherence to this standard is an effective tool for quality improvement, reducing the risk of errors and thus increasing patient safety.17
Subsequently, the necessity to control and improve quality in clinical laboratories goes hand in hand with technological development, leading to a reduction in analytical errors. Introduced electronic algorithms identify potential undesirable events by detecting appropriate records.18 An important reason for improving the evaluation of research is the introduction of quality evaluation indicators. Quality assessment methods developed for this purpose allow for the identification of errors and inconsistencies that may occur at all stages of the pre-analytical phase.19
Establishing valuable indicators is a strategy for collecting data on quality, in particular for detecting any errors.20 Under this concept, all steps and activities in the test cycle should be monitored and assessed to reduce errors and improve patient safety.21 The developed indicators are an effective tool for estimating quality, identifying problems as well as monitoring laboratory errors.22 These tools enable quality assessment of selected aspects of the process by comparing them with appropriate criteria.23–25 Adoption of test quality assessment kits allows for the accreditation of clinical laboratories in accordance with the standards and ensures the implementation of guidelines for promoting the processes of improving the quality of diagnostic tests and providing patients with high-quality medical care.26 Laboratories can therefore measure, monitor and improve their analytical results through internal quality control regulations.27
Entities performing genetic tests (analyzed laboratories) do not ensure appropriate quality of tests, security of patients’ personal data nor the security of the obtained biological material. All inspected laboratories stored genetic material and patient data after the test was performed, but did not formally define any rules that should accompany its performance. Only two tested laboratories implemented and applied the required quality standards defined by law. This is an area that requires further improvement.
The condition of the equipment and periodic technical inspections also affect the quality of services. In the tested laboratories, the regulations concerning technical conditions and the requirement of technical inspections were not always followed. Quality control (external, internal), timely inspections of laboratory equipment and devices and the staff’s professionalism increase the guarantee of the reliability of tests performed in laboratories.2
Three laboratories did not respect formal provisions related to documentation keeping, eg, they used non-compliant consent forms for genetic testing. Formal obligations associated with keeping medical records also leave a lot to be desired.
Laboratories used various methods to protect patients’ personal data and their genetic material increasing the risk of their unauthorized disclosure. Only in one laboratory this process was appropriate, ie, it adequately protected patient data. The protection of personal data is at different levels and in this respect it will have to comply with the new EU law – the GDPR Regulation.28
Since comprehensive laws regulating the area of human genetics, including the performance of genetic tests, have not yet been developed, there is quite a lot of freedom in this area. The lack of a single, uniform law can also be read as favoring arbitrary interpretations. The existing regulations are located in various acts, which certainly does not facilitate their proper execution. In a letter addressed to the Ombudsman – The Polish Society of Human Genetics mentions the unfavorable report of the Supreme Audit Office as an assumptive for further work related to the introduction of a legal act concerning the field of genetics including genetic testing and biobanking. The letter refers to a ministerial draft that did not recognize the comments of the scientific community. Of course, the will and need to develop a single act normalizing these issues in the opinion (and with the cooperation) of the Polish Society of Human Genetics is vital.
Conclusion
Genetic tests are a type of research performed on a human biological material that can determine the occurrence of a disease or congenital defects. Therefore, they should be preceded by medical advice and, after receiving the result, consultation. The current stage of genetic research safety in Poland requires many urgent formal solutions.
The currently existing legal regulations are scarce and scattered in various legal and professional acts (eg, the Law on the Profession of Doctor and Dentist), what is more, the current state of Polish law interprets genetic data, as personal data, which are thus subjected to protection under EU regulations (eg, GDPR). The basic conclusion drawn from the manuscript is the need to improve and unify the area of genetic testing. First of all, it would be beneficial to gather and provide a clear interpretation of legal provision behind genetic testing. On its basis laboratories could be provided with a checklist of necessary to perform activities, which they could later implement. In order to counteract the current situation on the spot, we propose focusing solely on the post-inspection NIK report’ “areas of deficit” and sensitizing laboratory employees (eg, through regular seminars or coaching) on the necessity of fulfilling their legal obligations as well as on consequences of failing to do so.
Failure to respect relevant legal provisions may jeopardize data security and ultimately cause data leak to unauthorized entities that can use these information against patients, eg, insurance companies.
Due diligence in performing tests associated activities that are required by law will contribute to increasing the quality of performed test in the legal sense and can boost public trust in genetic testing. Currently, the society should have concerns about genetic testing because a lot of questions are still left unanswered and with medical progress the number of dilemmas behind genetic testing will increase; therefore, it is necessary to make every effort not to deepen this situation of mistrust through, eg, privacy breach. Thus, the formal and legal element of genetic testing in the current condition should be improved after the report’s conclusions.
At the current stage, legislative work is underway for an act that would normalize, among other things, the area of genetic research, as well as issues concerning the manner and scope of human biological material use.
Ethics Statement
There are three documents in the Polish law that pertain to the functioning of Bioethics Committees: The Act of the Pharmaceutical Law, The Act on the Professions of Doctor and Dentist (art 21.1) and the Regulation of the Minister for Health and Social Welfare of 11 May 1999 on the detailed rules for setting up and financing of bioethics committees and the operating procedures for bioethics committees (art 4 item 1). These documents define that the bioethics committees in Poland are legally obliged to provide an opinion only in the case of clinical studies or medical experiments. Since publically available documentation analysis is neither a clinical study nor a medical experiment, our study does not require an IRB approval.
What is more, National Supreme Audit Office (NIK) is a controlling entity
Underpinned by clearly defined principles: transparency of intentions, reliability of information, apoliticality of auditors and collegiality in taking key decisions (…)
The standards reflect NIK’s achievements to date, including recognised solutions in the area of audit methodology. These standards have been developed on the basis of the Polish law, the INTOSAI Auditing Standards, the European Implementing Guidelines for the INTOSAI Auditing Standards, the Standards of the International Federation of Accountants (IFAC) and the long experience of NIK. (https://www.nik.gov.pl/en/about-us/) As the controlling Body, NIK is legally obliged to control entities, and draft and publish rapports about the inspection’s results to maintain transparency and public trust.
According to the Polish law, public information can be a source of scientific knowledge and can be used by anyone, as long as the usage is in accordance with the Copyright and Related Right’s Act.
This is a report of an auditing body and the publically available data, under Polish laws, can be used without Bioethics Committee or Supreme’s Audit Office approval (however with proper citations). What is more, the auditing body (here NIK) does not need to obtain a bioethics committee opinion for conducting the inspections and we, as authors do not need a bioethics committee approval to use publically available data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gabińska A. Badania laboratoryjne mogą być niewiarygodne [Laboratory tests may not be reliable. We have the evidence]. Mamy dowody. Available from: https://gazetawroclawska.pl/badania-laboratoryjne-moga-byc-niewiarygodne-mamy-dowody/ar/542543.
2. Bezpieczeństwo badań genetycznych. Jednostka kontrolująca: delegatura NIK w Warszawie. Nr ewidencyjny: P/17/102/LWA [Safety of genetic testing. Inspection body. NIK’s Delegature in Warsaw. Identification number P/17/102/LWA]. Available from: https://www.nik.gov.pl/kontrole/P/17/102/LWA/.
3. Pilonis H. Po co robić badania genetyczne? [Why get genetic testing?] Available from: http://www.medonet.pl/zdrowie,po-co-robic-badania-genetyczne-,artykul,1723396.html.
4. Krajowa Izba Diagnostów Laboratoryjnych [National Chamber of Laboratory Diagnosticians]. Available from: kidl.org.pl.
5. Szczecin. International hereditary cancer center – szczecin. Available from: https://genetyka.com/?page_id=119.
6. Soini S. Genetic testing legislation in Western Europe – a fluctuating regulatory target. J Comm Genetics. 2012;3:143–153. doi:10.1007/s12687-012-0078-0
7. Kapelańska-Pręgowska J. Laws governing postnatal genetic testing for medical purposes in Germany, Switzerland, Spain and France. Comparative Law Rev. 2013;16:131–158. doi:10.12775/CLR.2013.020
8. Kapelańska-Pręgowska J Wybrane problemy prawnej regulacji testów genetycznych. Wybrane aspekty praw człowieka a bioetyka. red. Anny Białek i Mirosława Wróblewskiego [Selected challenges behind legal regulations of genetic testing. Chosen aspects of human rights and bioethics]. Avialble from: https://repozytorium.umk.pl/bitstream/handle/item/4080/Wybrane%20aspekty%20praw%20cz%C5%82owieka%20a%20bioetyka%20-%20JKP.pdf?sequence=1.
9. Zákon 373/2011 ze dne 6. listopadu 2011 o specifických zdravotních službách, Uveřejněno v č. 131/2011 Sbírky zákonů, s. 4802 [Act 373/2011 of 6 November 2011 on specific health services, Published in No. 131/2011 of the Collection of Laws, p. 4802; 2011]; 2011.
10. Article 10 ustawy z dnia 23 grudnia 1994 r. O najwyższej Izbie Kontroli [Article 10 of the Act of 23 December 1994 On the Supreme Audit Office]; 2022:623.
11. Rozporządzenie Ministra Zdrowia w sprawie standardów jakości dla medycznych laboratoriów diagnostycznych i mikrobiologicznych [Regulation of the Minister of Health on quality standards for diagnostic and microbiological laboratories; 2019]; 2019.
12. Plebani M. Exploring the iceberg of errors in laboratory medicine. Clin Chim Acta. 2009;404:16–23. doi:10.1016/j.cca.2009.03.022
13. Howanitz PJ. Errors in laboratory medicine: practical lessons to improve patient safety. Arch Pathol Lab Med. 2005;129:1252–1261. doi:10.5858/2005-129-1252-EILMPL
14. Plebani M. Errors in clinical laboratories or errors in laboratory medicine? Clin Chem and Lab Med. 2006;44(6):750–759. doi:10.1515/CCLM.2006.123
15. Carraro P, Plebani M. Errors in a stat laboratory: types and frequencies 10 years later. Clin Chem. 2007;53:1338–1342. doi:10.1373/clinchem.2007.088344
16. Epner PL, Gans JE, Graber ML. When diagnostic testing leads to harm: a new outcomes-based approach for laboratory medicine. BMJ Qual Saf. 2013;22:ii6–ii10. doi:10.1136/bmjqs-2012-001621
17. Plebani M. Diagnostic errors and laboratory medicine – causes and strategies. eJIFCC. 2015;26:7–14.
18. Plebani M. Quality in laboratory medicine: 50 years on. Clin Biochem. 2017;50:101–104. doi:10.1016/j.clinbiochem.2016.10.007
19. Plebani M, Sciacovelli L, Aita A, Padoan A, Chiozza ML. Quality indicators to detect pre-analytical errors in laboratory testing. Clin Chim Acta. 2014;432:44–48. doi:10.1016/j.cca.2013.07.033
20. Plebani M, Sciacovelli L, Aita A, Pelloso M, Chiozza ML. Performance criteria and quality indicators for the pre-analytical phase. Clin Chem Lab Med. 2015;53:943–948. doi:10.1515/cclm-2014-1124
21. Sciacovelli L, Aita A, Padoan A, et al. Performance criteria and quality indicators for the post-analytical phase. Clin Chem Lab Med. 2016;54:1169–1176. doi:10.1515/cclm-2015-0897
22. Raab SS. Improving patient safety through quality assurance. Arch Pathol Lab Med. 2006;130(5):633–637. doi:10.5858/2006-130-633-IPSTQA
23. Shahangian S, Snyder SR. Laboratory medicine quality indicators: a review of the literature. Am J Clin Pathol. 2009;131:418–431. doi:10.1309/AJCPJF8JI4ZLDQUE
24. Plebani M. The quality indicator paradox. Clin Chem Lab Med. 2016;54:1119–1122. doi:10.1515/cclm-2015-1080
25. Khullar D, Jha AK, Jena AB. Reducing diagnostic errors--why now? N Engl J Med. 2015;373:2491–2493. doi:10.1056/NEJMp1508044
26. Plebani M. Performance specifications for the extra-analytical phases of laboratory testing: why and how. Clin Biochem. 2017;50:550–554. doi:10.1016/j.clinbiochem.2017.02.002
27. Plebani M, Astion ML, Barth JH, et al. Harmonization of quality indicators in laboratory medicine. A preliminary consensus. Clin Chem Lab Med. 2014;52:951–958. doi:10.1515/cclm-2014-0142
28. Rozporządzenie Parlamentu Europejskiego i Rady. w sprawie ochrony osób fizycznych w związku z przetwarzaniem danych osobowych i w sprawie swobodnego przepływu takich danych oraz uchylenia dyrektywy 95/46/WE/ - RODO [Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation)]; 2016.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Quality by Design: Development of Safe and Efficacious Full-Thickness Acellular Dermal Matrix Based on EuroGTPII Methodologies
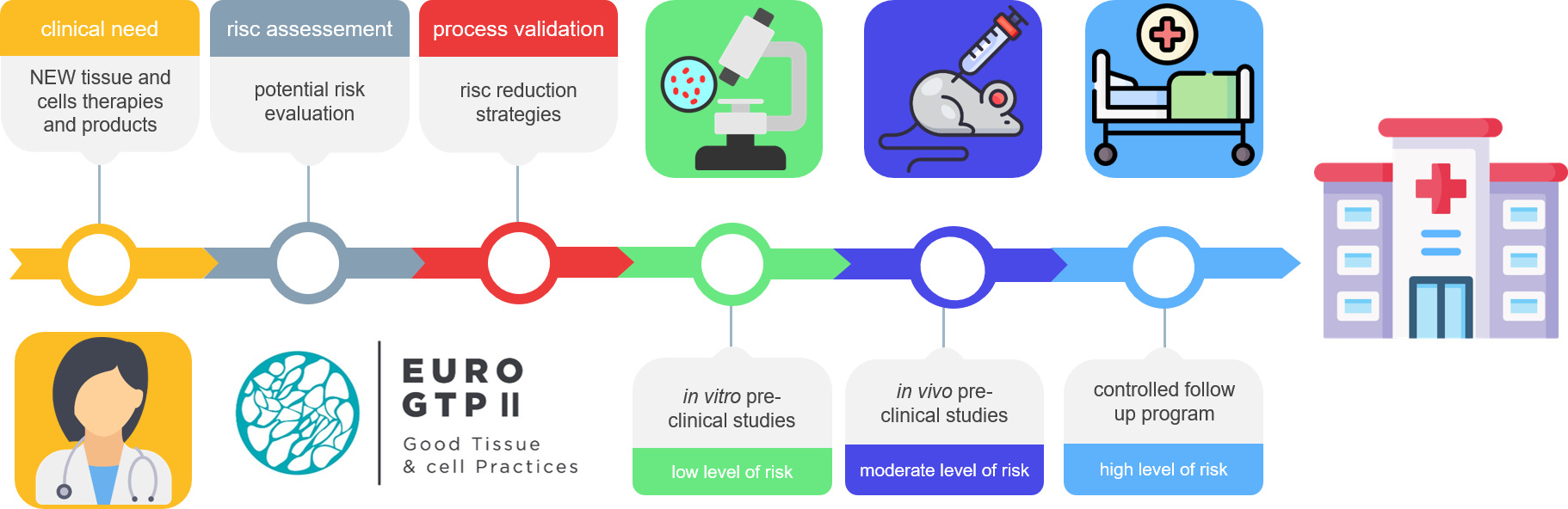
López-Chicón P, Pérez ML, Castells-Sala C, Piteira AR, Fariñas O, Tabera J, Vilarrodona A
Therapeutics and Clinical Risk Management 2023, 19:567-578
Published Date: 4 July 2023
