Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Different Case Finding Approaches to Optimise COPD Diagnosis: Evidence from the RADICALS Trial
Authors Alotaibi N , Borg BM, Abramson MJ , Paul E , Zwar N, Russell G , Wilson S, Holland AE, Bonevski B , Mahal A , George J
Received 30 April 2022
Accepted for publication 28 May 2023
Published 20 July 2023 Volume 2023:18 Pages 1543—1554
DOI https://doi.org/10.2147/COPD.S371371
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Min Zhang
Nawar Alotaibi,1 Brigitte M Borg,2,3 Michael J Abramson,3 Eldho Paul,3 Nicholas Zwar,4 Grant Russell,5 Sally Wilson,1,6 Anne E Holland,2,7 Billie Bonevski,8 Ajay Mahal,9 Johnson George1,3
1Centre for Medicine Use and Safety, Monash University, Melbourne, VIC, Australia; 2Respiratory Medicine, Alfred Health, Melbourne, VIC, Australia; 3School of Public Health & Preventive Medicine, Monash University, Melbourne, VIC, Australia; 4Faculty of Health Sciences and Medicine, Bond University, Robina, QLD, Australia; 5Department of General Practice, Monash University, Melbourne, VIC, Australia; 6Department of Infrastructure Engineering, The University of Melbourne, Melbourne, VIC, Australia; 7Central Clinical School, Monash University, Melbourne, VIC, Australia; 8College of Medicine and Public Health, Flinders University, Bedford Park, SA, Australia; 9The Nossal Institute for Global Health, The University of Melbourne, Melbourne, VIC, Australia
Correspondence: Johnson George, Centre for Medicine Use and Safety, Faculty of Pharmacy and Pharmaceutical Sciences, Monash University, 381 Royal Parade, Parkville, VIC, 3052, Australia, Email [email protected]
Aim: Diagnosis of COPD in primary care is hindered by underuse of spirometry. Case finding using validated symptom and health status questionnaires, and simple handheld devices in high-risk populations may improve diagnosis. This study aimed to determine the best combination of measures to optimise COPD diagnosis in the primary care setting.
Methods: We recruited 335 current or ex-smokers, including those with an established diagnosis of COPD from general practices. Participants’ FEV1 and FEV6 were measured using a handheld spirometry device (COPD-6®). Each completed the COPD assessment test (CAT), a modified Medical Research Council (mMRC) dyspnoea scale, St George’s Respiratory Questionnaire (SGRQ) and smoking history questionnaire. From these data we calculated the predictive validity for spirometry-confirmed diagnosis of COPD. Area under the receiver operating characteristic curve (AUROC), sensitivity, specificity, positive and negative predictive values (PPV, NPV) were calculated for each. Kappa coefficient was used to measure the agreement between the Fixed-Ratio (FR) and Lower Limit of Normal (LLN) spirometric criteria in diagnosing COPD.
Results: FEV1/FEV6 < 0.70 alone showed significant association (p< 0.0001) with COPD diagnosis and good predictive accuracy (AUROC=0.725). However, no further improvement was found after combining SGRQ, CAT and mMRC with FEV1/FEV6. FEV1/FEV6 < 0.70 using the COPD-6® handheld device had moderate sensitivity (65.7%) and high PPV (90.1%), high specificity (79.3%) and NPV (44.8%). There was good agreement between FR and LLN definitions (κ=0.70).
Conclusion: Handheld micro-spirometers can facilitate case finding of COPD in smokers and ex-smokers attending general practice. The fixed ratio criterion currently recommended by COPD-X guidelines offers the simplest method for diagnosing COPD in Australian primary care.
Keywords: case finding, COPD, diagnosis, primary care
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is characterised by persistent airflow limitation and debilitating symptoms.1 COPD is a global public health issue associated with significant mortality, morbidity, and health service utilisation.2 COPD is the fourth leading cause of death globally. The World Health Organization (WHO) has projected COPD to be contributing to 8.6% of deaths worldwide and become the third leading cause of death by 2030.3 In Australia, the overall prevalence of moderate to severe COPD in adults aged ≥40 years was 7.5%.4 The prevalence was 29.2% among those aged ≥75 years.5
Studies suggest that a significant number of cases of COPD in primary care go undiagnosed or are not adequately diagnosed, resulting in many patients only being diagnosed after they have already experienced a significant loss of lung function.6,7 Liang et al have provided an overview of the current state of spirometry usage in Australia and reported the inadequate use of spirometry in primary care.8 A large proportion of primary care facilities do not offer spirometry. The insufficient utilization of spirometry has been identified as the primary cause of COPD underdiagnosis or failure to diagnose.9
Carrying out the standard laboratory spirometry test may not be practical in the primary care setting due to the high costs associated with acquiring, storing, and maintaining the equipment, as well as a shortage of trained healthcare workers. However, referring all patients suspected of having COPD to hospitals or laboratories for spirometry testing would not only increase the cost of medical care for these patients, but also delay formal diagnosis and initiation of appropriate treatment.
The use of opportunistic screening in patients at high-risk of COPD (ie, case finding) could potentially enhance secondary prevention measures, such as smoking cessation, in the early stages.10 Case finding may also improve COPD diagnosis and management in primary healthcare.11,12 COPD could also be diagnosed using advanced machine learning algorithms.13–15 Novel computerized techniques have been shown to provide quick and robust assessment of COPD at early stages even without being dependent on expert pulmonologist clinicians.16,17 However, high costs and lack of trained personnel may be challenges for their uptake.
Handheld spirometers such as PiKo-6® (nSpire Health, Inc. Longmont, CO, USA) or COPD-6™ (Vitalograph Ltd, Ennis, Co., Clare, Ireland) are becoming increasingly popular in clinical settings because they are affordable, portable, and easy to use. Multiple studies have demonstrated that the results using handheld spirometers are highly comparable to those using traditional spirometers.18,19 Consequently, handheld spirometers have gained traction in medical practice and research and maybe a viable alternative for identifying people with COPD at an early stage in resource-constrained healthcare settings.
The ratio of forced expiratory volumes in 1 and 6 seconds (FEV1/FEV6) has been proposed as an alternative to FEV1/FVC (Forced Vital Capacity) to reliably detect airflow obstruction.20 Lung Foundation Australia COPD-X guidelines recommend a cut-off of FEV1/FEV6 <0.75 for COPD case finding, as this value could distinguish individuals with a confirmed diagnosis (through spirometry) from those who do not.21 However, the US Preventive Services Task Force did not support screening of asymptomatic persons, as it would not enhance the individual’s quality of life.22 Case finding initiatives should target adults >35 years with characteristic respiratory symptoms and a history of exposure to tobacco smoke and/or noxious particles.23
COPD remains underdiagnosed in primary care24 and utilisation of spirometry has declined further following the COVID-19 pandemic. Yet combining lung function data (eg, FEV1/FEV6) with symptom or quality of life questionnaires may improve COPD case finding in primary care.10 Vestbo and Lange have called for further research to characterise COPD using different diagnostic criteria.25 Moreover, spirometry indices are influenced by age, height, sex, and ethnicity.26 Therefore, discovering the cut-off value of FEV1/FEV6 for COPD diagnosis in a nationwide, representative population sample in Australian primary care is worthwhile.
This study aimed to optimise COPD diagnosis in primary care by finding the best combination of case finding tools, specifically lung function measured using hand-held devices along with available symptom/quality of life questionnaires. Additionally, it assessed the predictive performance of each tool individually or in a combination, aiming to identify as many COPD cases as possible in the primary care setting. This was reached by calculating the optimal cut-off of FEV1/FEV6 against 3 different criteria for COPD. Finally, it aimed to determine the level of agreement between these different diagnostic criteria.
Methods
Study Design
Data were from the Review of Airway Dysfunction and Interdisciplinary Community-based care of Adult Long-term Smokers (RADICALS), a cluster randomised controlled trial investigating COPD management in current or ex-smokers, with a history of at least 10 pack years, including those with an existing diagnosis of COPD. Details of the RADICALS trial have been published elsewhere.27 From a cohort of 1050 participants with a history of smoking only 394 individuals with FEV1/FEV6 <0.75 and/or clinical correlations were referred for further spirometric assessment.
Lung function (FEV1/FEV6) was measured using a handheld device (COPD-6®, Vitalograph, Ennis, Ireland). Smoking status (‘current smokers’ defined as participants who smoked on a daily or occasional basis; ex-smokers were considered as ‘non-smokers’), COPD assessment test (CAT), modified Medical Research Council (mMRC) Dyspnoea Scale, and St George’s Respiratory Questionnaire (SGRQ) scores were obtained. Predictive performances were tested against post-bronchodilator FEV1/FVC <0.7 ± clinical correlation and FEV1/FVC <LLN (5th percentile).
Optimal FEV1/FEV6 cut-off was determined against three diagnostic criteria: (1) RADICALS criterion: post-BD FEV1/FVC <0.7 and clinical correlation (our “gold standard”); (2) FR criterion: post-BD FEV1/FVC <0.7; and (3) LLN criterion: post-BD FEV1/FVC <LLN (5th percentile).
Statistical Methods
Baseline characteristics and clinical variables were reported as frequencies and percentages, medians and interquartile ranges [IQR] or means and standard deviations (SD), as appropriate. To determine the diagnostic accuracy of FEV1/FEV6 and the questionnaires, the area under the receiver operating characteristic curve (AUROC) was calculated. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for each measure. Logistic regression was used to determine the association between these variables and odds of having a COPD diagnosis. Odds ratios (OR) and 95% confidence intervals (CI) were estimated. The kappa coefficient (K) was used to determine the agreement beyond chance between the FR and LLN spirometric criteria in diagnosing COPD.
Results
A total of 394 participants were referred for spirometry. Of these participants, 25 did not have spirometry; 34 participants had missing data, leaving 335 participants eligible for the analyses. Their baseline and clinical characteristics are summarised in Table 1 and Table 2. The majority of participants were born in Australia, were daily smokers and had mild COPD. Majority of participants were male, and the mean (±SD) age was 63.3 (±10.9) years.
 |
Table 1 Characteristics of the Participants (n = 335) |
 |
Table 2 Participant Clinical Characteristics (n = 335) |
Optimal Cut-off for Case Finding Against RADICALS Definition of COPD
When the recommended cut-off of FEV1/FEV6 <0.75 was used, the sensitivity was 93.1%, specificity 35.6% and PPV 80.5% (see Online Supplement, Table S1) for post-BD FEV1/FVC <0.7 and clinical correlation. At FEV1/FEV6 <0.70, among candidates with confirmatory spirometry, the probability of disease (PPV) was 90.1%. Among candidates with a negative screening result, the probability of not having COPD (NPV) was 44.8%.
FEV1/FEV6 <0.70 yielded better diagnostic predictive accuracy (AUROC=0.725 (Figure 1)), than SGRQ (AUROC=0.651), CAT (AUROC=0.620) or mMRC (AUROC=0.612) (Online Supplement Figures S1A–C). The ROC curve confirmed that the discriminatory power was 72.5% with p-value <0.0001. This meant that 72.5% of the times, FEV1/FEV6 values were lower for patients with COPD compared to those without COPD.
 |
Figure 1 ROC curve for FEV1/FEV6 <0.70 against post-BD FEV1/FVC <0.7 and clinical correlation. |
Univariate analysis showed significant associations between SGRQ (OR=1.03, p-value=0.0001); CAT (OR=1.07, p=0.009); and mMRC scores (OR=1.56, p=0.016) and the odds of having COPD (Table 3). However, multivariate analysis found that only FEV1/FEV6 < 0.70 was independently associated with COPD diagnosis (OR=3.62, p=0.001).
 |
Table 3 Univariate and Multivariate Logistic Regression Analyses for COPD at Baseline, Based on the “Gold Standard” of Post-BD FEV1/FVC <0.7 and Clinical Correlation |
Optimal Cut-off for Case Finding Against Post-BD FEV1/FVC <0.7 COPD Definition
Using the FR definition for COPD, a FEV1/FEV6 <0.70 provided the best combination of sensitivity (72.6%) and PPV (90.0%), and specificity (83.3%) and NPV (59.6%) (See Online Supplement Table S2). Also, FEV1/FEV6 <0.70 gave the highest AUROC=0.780 (Figure 2) for COPD predictive accuracy, against FR, compared to SGRQ (0.641), CAT (0.605) and mMRC (0.608) (see Online Supplement Figures S2A–C).
 |
Figure 2 ROC curve for FEV1/FEV6 <0.70 against post-BD FEV1/FVC <0.7. |
Univariate analysis showed significant associations between SGRQ (OR=1.03, p-value=0.0001); CAT (OR=1.06, p=0.007); and mMRC scores (OR=1.56, p=0.004) and the odds of COPD (Table 3). Multivariate logistic regression showed that only FEV1/FEV6 <0.70 was significantly independently associated with COPD diagnosis (OR=8.88, p <0.001) (Table 4).
 |
Table 4 Univariate and Multivariate Regression Analysis for SGRQ, CAT, mMRC and Smoking Status for COPD at Baseline, Based on Post-BD FEV1/FVC < 0.7 |
Optimal Cut-off Value for Case Finding Against FEV1/FVC <LLN COPD Definition
Using the LLN definition for COPD diagnosis, the best cut-off value for FEV1/FEV6 was <0.70, which showed high sensitivity (84.3%), and specificity (80.4%) (See Online Supplement Table S3). The AUROC of FEV1/FEV6 against FEV1/FVC <LLN was 0.824 (Figure 3), which was higher than those using fixed cut-off methods (Figures 1 and 2). Other methods yielded unacceptable ROC values (below 0.70) (see Online Supplementary Figures S3A–C).
 |
Figure 3 ROC curve for FEV1/FEV6 <0.70 against post-BD FEV1/FVC <LLN. |
SGRQ, CAT and mMRC scores were significantly associated with having a diagnosis of COPD in univariate analyses (Table 5). However, multivariate analysis confirmed that only FEV1/FEV6 <0.70 was independently associated with the odds of having a COPD diagnosis (OR= 16.2, p-value <0.001) (Table 5).
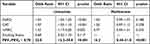 |
Table 5 Univariate and Multivariate Regression Analysis for SGRQ, CAT, mMRC and Smoking Status for COPD at Baseline, Based on Post-BD FEV1/FVC < LLN |
The results for cut-offs of FEV1/FEV6 against mild and moderate-severe COPD are presented in Table S4.
There was good agreement between the RADICALS and FR criteria, with κ=0.72 (p-value = <0.001). This analysis showed that 87.4% (215) of the cohort met the criteria for RADICALS and FR. However, agreement between the RADICALS and LLN criteria was only moderate, with κ=0.51 (p<0.001) where only 67.6% of the cohort met those criteria. Interestingly, the agreement between the FR and LLN criteria was better (κ=0.70; p<0.001), and 76.9% of the cohort met both criteria (Table 6).
 |
Table 6 The Agreement Between Alternative Definitions of COPD in RADICALS |
Discussion
This study examined the predictive performances in diagnosing COPD using different cut-off values for handheld spirometer readings alone, and in combination with symptom and quality of life scales. It also determined the level of agreement between 3 alternative diagnostic definitions for COPD. A cut-off value for FEV1/FEV6 of < 0.70 in high-risk patients (defined as patients aged ≥35 years and current or ex-smokers with a history of at least 10-pack-years) was the most efficient method for case finding of COPD in primary care.
The use of FEV1 and FEV1/FVC ratio seems to have become the primary method for COPD diagnosis. However, using the FEV1/FVC is more time-consuming and expensive than using the FEV1/FEV6 ratio. FVC based portable spirometers are generally more expensive, while FEV1/FEV6 instruments only cost one-tenth of that of traditional spirometers. Therefore, it is an effective and practical method for diagnosing and monitoring respiratory diseases in busy primary care centres. With an AUROC value of 0.802, excellent overall performance was obtained for FEV1/FEV6 <0.70 as a fixed cut-off for the detection of COPD.
Multiple studies have used FEV1/FEV6 with a variety of cut offs suggested for best yields. One study28 found FEV1/FEV6<0.73 yielded a sensitivity of 79.2% and specificity of 80.3% for FEV1/FVC<0.70 (GOLD criteria). The AUROC was 0.84, suggesting that screening with the COPD-6 device predicted COPD effectively. A second study,11 determined a cut off value of FEV1/FEV6< 0.75 produced best yields for finding COPD in primary care with sensitivity and specificity of 81% and 71%, respectively. A third study12 confirmed COPD in 487 participants using FEV1/FEV6<0.7. Our study similarly found that FEV1/FEV6<0.70 in high-risk patients was the most efficient method for case finding of COPD in primary care.
While a fixed cut-off point for FEV1/FEV6 is a useful method for the diagnosis of COPD, it is important to consider certain disadvantages. Firstly, FEV6, alike FVC, can be affected by sex and education level.29 In addition, there is potential misclassification for elderly subjects, where the age-related decline in FEV1/FVC and FEV1/FEV6 may result in over-diagnosis of COPD.30 Furthermore, smoking and exposure to ambient air pollution can also affect the accuracy of FEV1 measurements.31,32 Therefore, the fixed ratio of FEV1/FEV6 should be interpreted for in the context of the patient’s risk factors, age, and symptoms. Nonetheless, the use of a fixed cut-off value for FEV1/FEV6 instead of a reference equation, remains an important diagnostic tool for COPD, as highlighted in the GOLD COPD guidelines.1 Quality of life and symptom questionnaires are often used in research, to measure the influence of diseases on an individual’s life, especially changes over time. However, these questionnaires could not distinguish accurately between participants with or without COPD in Dutch and Belgian studies.33 Similarly, our findings suggest that they add little value to COPD diagnosis in Australian primary care, especially when not used in conjunction with lung function tests.
The Agreement Between Different Spirometric Definitions of COPD
Our study showed that there was substantial overlap between RADICALS and FR criteria with a good agreement. The agreement between the FR and LLN criteria was also similar. However, the agreement between RADICALS and LLN criteria was only moderate.
A study by Çolak et al compared different diagnostic criteria to define airflow limitation in 108,246 participants, aged between 20–100 years. They concluded that the prevalence of airflow limitation ranged from 8% to 17% depending on the reference set.34
In a Belgian study, elderly people had a lower prevalence of airflow limitation (9.2%) when using the LLN method. This contrasted with the results of the FR method (27%), and there was poor agreement between methods (κ≤0.40). The authors found that LLN independently predicted mortality and detected patients at higher risk of death and hospitalization.35
The BOLD study recommended the use of FEV1/FVC <LLN, to minimise any age-related bias that could lead to an increased prevalence of COPD in healthy non-smokers while minimising the risk of false positives.36 The Canadian Cohort of Obstructive Lung Disease (CanCOLD) found that a low value of FEV1/FVC (based on FR and/or LLN) and a low value of FEV1 were strongly related to clinical outcomes.37 As expected the prevalence of airflow limitation was higher with FR than LLN.
A number of studies have assessed the agreement between FR and LLN methods in older adults, and found poor agreement between these two criteria, which showed higher prevalence of airway obstruction with FR than LLN (p <0.001) due to increasing age.38,39 However, respiratory symptoms were more prevalent in LLN confirmed COPD compared to FR confirmed COPD (50% versus 39%, p<0.0001).40 The agreement between these two methods decreased with age. This is due to evidence that in a healthy population the predicted FEV1//FVC declines with age.41 Lastly, Güder et al found that FR yielded a higher sensitivity, but LLN a higher specificity, which is consistent with our findings.38
Strengths and Limitations
The main strength of this study was inclusion of data from a well-designed pragmatic trial in primary care. Experienced and trained healthcare practitioners (respiratory scientists, nurses and doctors) were involved in performing spirometry and assisting with the interpretation of spirometry.
However there were also some limitations. In this study, we did not examine questionnaires that have been specifically designed for COPD screening or case finding such as the COPD Diagnostic Questionnaire (CDQ), COPD Population Screener, COPD Screening Questionnaire, COPD Assessment in Primary Care to Identify Undiagnosed Respiratory Disease and Exacerbation Risk (CAPTURE), or Lung Function Questionnaire. The participating clinics might not be representative of all general practices in Australia. Almost all participants recruited had a history of smoking, thus the results may not be generalisable to non-smokers who develop COPD. Some participants (n=60) may have had co-existing asthma-COPD.42
The Implications of the Findings
This study provides reliable evidence for policy makers to recommend the use of simple devices such as handheld spirometry in the primary care setting to facilitate case finding for COPD in patients who are current or past smokers. Healthcare practitioners may use a cut-off value of FEV1/FEV6 <0.70, to refer those aged 35 years and above with a history of exposure to tobacco smoke or other noxious particles for spirometry. The cost-effectiveness of this method needs to be estimated and compared against other methods used in larger studies.
Conclusions
Case-finding using handheld spirometers with a cut-off value of FEV1/FEV6 <0.70 offers a convenient method in the primary healthcare setting to identify patients with COPD. Use of symptom and quality of life questionnaires added little value in case finding. The level of agreement between FR and LLN was good, although some patients with mild disease were missed by the LLN method, potentially delaying initiation of early interventions.
Take Home Messages
- Case finding using handheld spirometers at a cut-off of FEV1/FEV6 < 0.70 gives the best sensitivity and specificity for COPD diagnosis.
- Use of symptoms and COPD-related quality of life questionnaires add little value to FEV1/FEV6 -based case finding.
- Fixed-cut-off ratio and the lower limit of normal (LLN) definitions for characterising airflow limitation provide comparable results when used to diagnose COPD in the primary care setting.
Data Sharing Statement
The raw data on which conclusions of this manuscript rely are available upon reasonable requests. The overall results are available as part of the manuscript and Supplementary Tables, but if individual data points are needed, this could be provided in response to a reasonable request.
Ethics Approval and Informed Consent
The institutional Ethics Committee approved the RADICALS trial (Monash University CF14/1018 –2014000433). Informed written consent was obtained from each participant before the trial commencement. The study was conducted in accordance with Good Clinical Practice guidelines and the provisions of the Declaration of Helsinki. RADICALS trial registration number is ACTRN12614001155684.
Acknowledgments
We wish to thank the RADICALS Data Safety and Monitoring Board members (Ian Yang, Jennifer Alison and Julia Walters), Jenifer Liang, Denise van den Bosch, Jessica Webster, Rita Breare, Mieke Hutchinson-Kern, The Alfred Respiratory Laboratory, Eleonora Del Colle and Pulmetrics staff, Brian Meier, Eli Dabscheck, Agape Stratigis, Amanda Cross, Amanda Nichols, Andrew Clayton, Caroline Nicolson, Francesca Sgroi, Georgia Lakoumentas, Hilary Edwards, Janet Carberry, Jannette Angell, Kay Dunkley, Lisa Austin, Melanie Frodsham, Robyn Saunders, Robyn Stell, Ross de Gori, Rosemary Moore, Sandy Scholes, Sarah Rawlings, Tamara Ford, Yamuna Prashanth, research students, clinic staff and participants for their help with the RADICALS trial. Muhammad Rehan Sarwar assisted with responding to reviewer comments.
Disclosure
Mr Nawar Alotaibi reports grants from Pfizer, grants from Sanofi and GSK, during the conduct of the study; Ms Brigitte M Borg reports personal fees from Wiley Blackwell Publishing, outside the submitted work; Professor Michael J Abramson reports grants from Boehringer-Ingelheim, during the conduct of the study; grants from Pfizer, grants from Sanofi, grants from GSK, personal fees, personal fees from GSK, outside the submitted work; Professor Anne E Holland reports grants from National Health and Medical Research Council (Australia), grants from Boehringer Ingelheim Pty Ltd, non-financial support from Eastern Melbourne Primary Health Network (PHN), non-financial support from Lung Foundation Australia, during the conduct of the study; Dr Johnson George reports grants, non-financial support from Boehringer Ingelheim, during the conduct of the study; grants, grants from GSK, grants, grant from Pfizer, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. GOLD Science Committee. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease 2023 Report[OL]. GOLD Science Committee; 2023.
2. Barnes PJ. Chronic obstructive pulmonary disease: a growing but neglected global epidemic. PLoS Med. 2007;4(5):e112. doi:10.1371/journal.pmed.0040112
3. World health Organization. World Health Statistics 2008. World Health Organization; 2008.
4. McDonald CF, Glasgow N. The Burden of Obstructive Lung Disease (BOLD) Study in Australia. Australasian Medical Association; 2013.
5. Toelle BG, Xuan W, Bird TE, et al. Respiratory symptoms and illness in older Australians: the burden of obstructive lung disease (BOLD) study. Med J Aust. 2013;198(3):144–148. doi:10.5694/mja11.11640
6. Diab N, Gershon AS, Sin DD, et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(9):1130–1139. doi:10.1164/rccm.201804-0621CI
7. Calverley PM. COPD: early detection and intervention. Chest. 2000;117(5):365S–371S. doi:10.1378/chest.117.5_suppl_2.365S
8. Liang J, Abramson MJ, Zwar NA, et al. Diagnosing COPD and supporting smoking cessation in general practice: evidence–practice gaps. Med J Aust. 2018;208(1):29–34. doi:10.5694/mja17.00664
9. Ho T, Cusack RP, Chaudhary N, Satia I, Kurmi OP. Under-and over-diagnosis of COPD: a global perspective. Breathe. 2019;15(1):24–35. doi:10.1183/20734735.0346-2018
10. Haroon SM, Jordan RE, O’Beirne-Elliman J, Adab P. Effectiveness of case finding strategies for COPD in primary care: a systematic review and meta-analysis. NPJ Prim Care Respir Med. 2015;25(1):1–9. doi:10.1038/npjpcrm.2015.56
11. Frith P, Crockett A, Beilby J, et al. Simplified COPD screening: validation of the PiKo-6® in primary care. Prim Care Respir Med. 2011;20(2):190–198. doi:10.4104/pcrj.2011.00040
12. Kjeldgaard P, Lykkegaard J, Spillemose H, Ulrik CS. Multicenter study of the COPD-6 screening device: feasible for early detection of chronic obstructive pulmonary disease in primary care? Int J Chron Obstruct Pulmon Dis. 2017;12:2323–2331. doi:10.2147/COPD.S136244
13. Altan G, Kutlu Y, Allahverdi N. Deep learning on computerized analysis of chronic obstructive pulmonary disease. IEEE J Biomed Health Inform. 2019;24(5):1344–1350. doi:10.1109/JBHI.2019.2931395
14. Gökçen A. Computer-aided diagnosis system for chronic obstructive pulmonary disease using empirical wavelet transform on auscultation sounds. Comp J. 2021;64(11):1775–1783. doi:10.1093/comjnl/bxaa191
15. Altan G, Kutlu Y, Pekmezci AÖ, Nural S. Deep learning with 3D-second order difference plot on respiratory sounds. Biomed Signal Process Control. 2018;45:58–69. doi:10.1016/j.bspc.2018.05.014
16. Altan G, Kutlu Y, Pekmezci AÖ, Yayık A. Diagnosis of chronic obstructive pulmonary disease using deep extreme learning machines with LU autoencoder kernel.
17. Altan G, Kutlu Y, Gökçen A. Chronic obstructive pulmonary disease severity analysis using deep learning on multi-channel lung sounds. Turk J Electr Eng. 2020;28(5):2979–2996. doi:10.3906/elk-2004-68
18. Labor M, Vrbica Ž, Gudelj I, Labor S, Plavec D. Diagnostic accuracy of a pocket screening spirometer in diagnosing chronic obstructive pulmonary disease in general practice: a cross sectional validation study using tertiary care as a reference. BMC Fam Pract. 2016;17:1–11. doi:10.1186/s12875-016-0518-8
19. Chen G, Jiang L, Wang L, Zhang W, Castillo C, Fang X. The accuracy of a handheld “disposable pneumotachograph device” in the spirometric diagnosis of airway obstruction in a Chinese population. Int J Chron Obstruct Pulmon Dis. 2018;2351–2360. doi:10.2147/COPD.S168583
20. Bhatt SP, Y-i K, Wells JM, et al. FEV1/FEV6 to diagnose airflow obstruction. Comparisons with computed tomography and morbidity indices. Ann Am Thorac Soc. 2014;11(3):335–341. doi:10.1513/AnnalsATS.201308-251OC
21. Lung Foundation of Australia. Position Paper: COPD case finding in community settings; 2018.
22. Siu AL, Bibbins-Domingo K, Grossman DC, et al. Screening for chronic obstructive pulmonary disease: US preventive services task force recommendation statement. JAMA. 2016;315(13):1372–1377. doi:10.1001/jama.2016.2638
23. Dabscheck E, George J, Hermann K, et al. COPD‐X Australian guidelines for the diagnosis and management of chronic obstructive pulmonary disease: 2022 update. Med J Aust. 2022;217(8):415–423. doi:10.5694/mja2.51708
24. Petrie K, Toelle BG, Wood-Baker R, et al. Undiagnosed and misdiagnosed chronic obstructive pulmonary disease: data from the BOLD Australia study. Int J Chron Obstruct Pulmon Dis. 2021;16:467–475. doi:10.2147/COPD.S287172
25. Vestbo J, Lange P. Accuracy of airflow obstruction thresholds for predicting COPD-Related hospitalization and mortality: can simple diagnostic thresholds be used for a complex disease? JAMA. 2019;321(24):2412–2413. doi:10.1001/jama.2019.6584
26. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
27. Liang J, Abramson MJ, Zwar N, et al. Interdisciplinary model of care (RADICALS) for early detection and management of chronic obstructive pulmonary disease (COPD) in Australian primary care: study protocol for a cluster randomised controlled trial. BMJ open. 2017;7(9):e016985. doi:10.1136/bmjopen-2017-016985
28. Thorn J, Tilling B, Lisspers K, Jörgensen L, Stenling A, Stratelis G. Improved prediction of COPD in at-risk patients using lung function pre-screening in primary care: a real-life study and cost-effectiveness analysis. Prim Care Respir Med. 2012;21(2):159–166. doi:10.4104/pcrj.2011.00104
29. Bellia V, Sorino C, Catalano F, et al. Validation of FEV6 in the elderly: correlates of performance and repeatability. Thorax. 2008;63(1):60–66. doi:10.1136/thx.2007.080572
30. Hardie J, Buist AS, Vollmer W, Ellingsen I, Bakke P, Mørkve O. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002;20(5):1117–1122. doi:10.1183/09031936.02.00023202
31. Götschi T, Heinrich J, Sunyer J, Künzli N. Long-term effects of ambient air pollution on lung function: a review. Epidemiology. 2008;19:690–701. doi:10.1097/EDE.0b013e318181650f
32. Scanlon PD, Connett JE, Waller LA, et al. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease: the Lung Health Study. Am J Respir Crit Care Med. 2000;161(2):381–390. doi:10.1164/ajrccm.161.2.9901044
33. Kotz D, Nelemans P, Van Schayck C, Wesseling G. External validation of a COPD diagnostic questionnaire. Eur Respir J. 2008;31(2):298–303. doi:10.1183/09031936.00074307
34. Çolak Y, Nordestgaard BG, Vestbo J, Lange P, Afzal S. Comparison of five major airflow limitation criteria to identify high-risk individuals with COPD: a contemporary population-based cohort. Thorax. 2020;75(11):944–954. doi:10.1136/thoraxjnl-2020-214559
35. Turkeshi E, Vaes B, Andreeva E, et al. Airflow limitation by the Global Lungs Initiative equations in a cohort of very old adults. Eur Respir J. 2015;46(1):123–132. doi:10.1183/09031936.00217214
36. Vollmer WM, Gíslason Þ, Burney P, et al. Comparison of spirometry criteria for the diagnosis of COPD: results from the BOLD study. Eur Respir J. 2009;34(3):588–597. doi:10.1183/09031936.00164608
37. van Dijk W, Tan W, Li P, et al. Clinical relevance of fixed ratio vs lower limit of normal of FEV1/FVC in COPD: patient-reported outcomes from the CanCOLD cohort. Ann Fam Med. 2015;13(1):41–48. doi:10.1370/afm.1714
38. Güder G, Brenner S, Angermann CE, et al. GOLD or lower limit of normal definition? A comparison with expert-based diagnosis of chronic obstructive pulmonary disease in a prospective cohort-study. Respir Res. 2012;13:1–9. doi:10.1186/1465-9921-13-13
39. Mikulski MA, Gerke AK, Lourens S, et al. Agreement between fixed-ratio and lower limit of normal spirometry interpretation protocols decreases with age. J Occup Environ Med. 2013;55(7):802–808. doi:10.1097/JOM.0b013e31828b22cc
40. Meteran H, Miller MR, Thomsen SF, Christensen K, Sigsgaard T, Backer V. The impact of different spirometric definitions on the prevalence of airway obstruction and their association with respiratory symptoms. ERJ Open Res. 2017;3(4):00110–2017. doi:10.1183/23120541.00110-2017
41. Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. doi:10.1183/09031936.05.00035205
42. Izbicki G, Teo V, Liang J, et al. Clinical characteristics of patients with asthma COPD overlap (ACO) in Australian primary care. Int J Chron Obstruct Pulmon Dis. 2019;14:2745–2752. doi:10.2147/COPD.S220346
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
